Copyright
©The Author(s) 2020.
World J Radiol. Jun 28, 2020; 12(6): 101-129
Published online Jun 28, 2020. doi: 10.4329/wjr.v12.i6.101
Published online Jun 28, 2020. doi: 10.4329/wjr.v12.i6.101
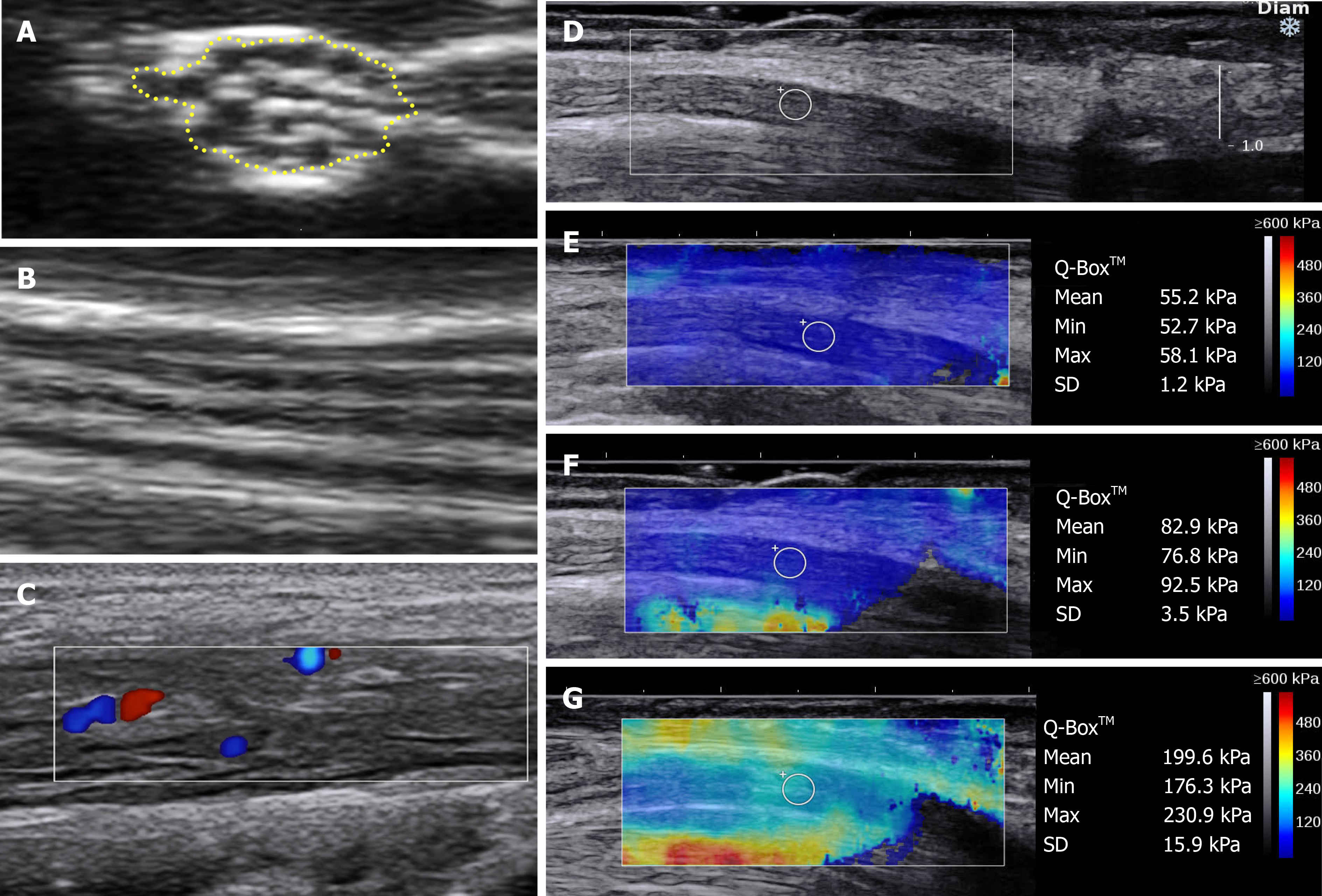
Figure 1 Approaches and techniques used in neuromuscular ultrasound.
A and B: Normal nerve ultrasound appearances of the median nerve in the forearm in B-mode. A: Cross-sectional area traced within the hyperechoic rim; B: Longitudinal view demonstrating the normal linear fascicular pattern; C: Doppler signal in the tibial nerve of a patient with hypertrophic perineuritis; D-G: Sheer wave elastography in carpal tunnel syndrome; D: Longitudinal B-mode image of the median nerve at the carpal tunnel above the lunate bone, a typical location for elastography measurements; E: Elastography values in a normal wrist; F: Increased median nerve stiffness in mild carpal tunnel syndrome; G: Further increased median nerve stiffness in severe carpal tunnel syndrome. D-G: Citation: Wee TC, Simon NG. Ultrasound elastography for the evaluation of peripheral nerves: A systematic review. Muscle Nerve 2019; 60: 501-512. Copyright© The Authors 2020. Published by John Wiley and Sons.
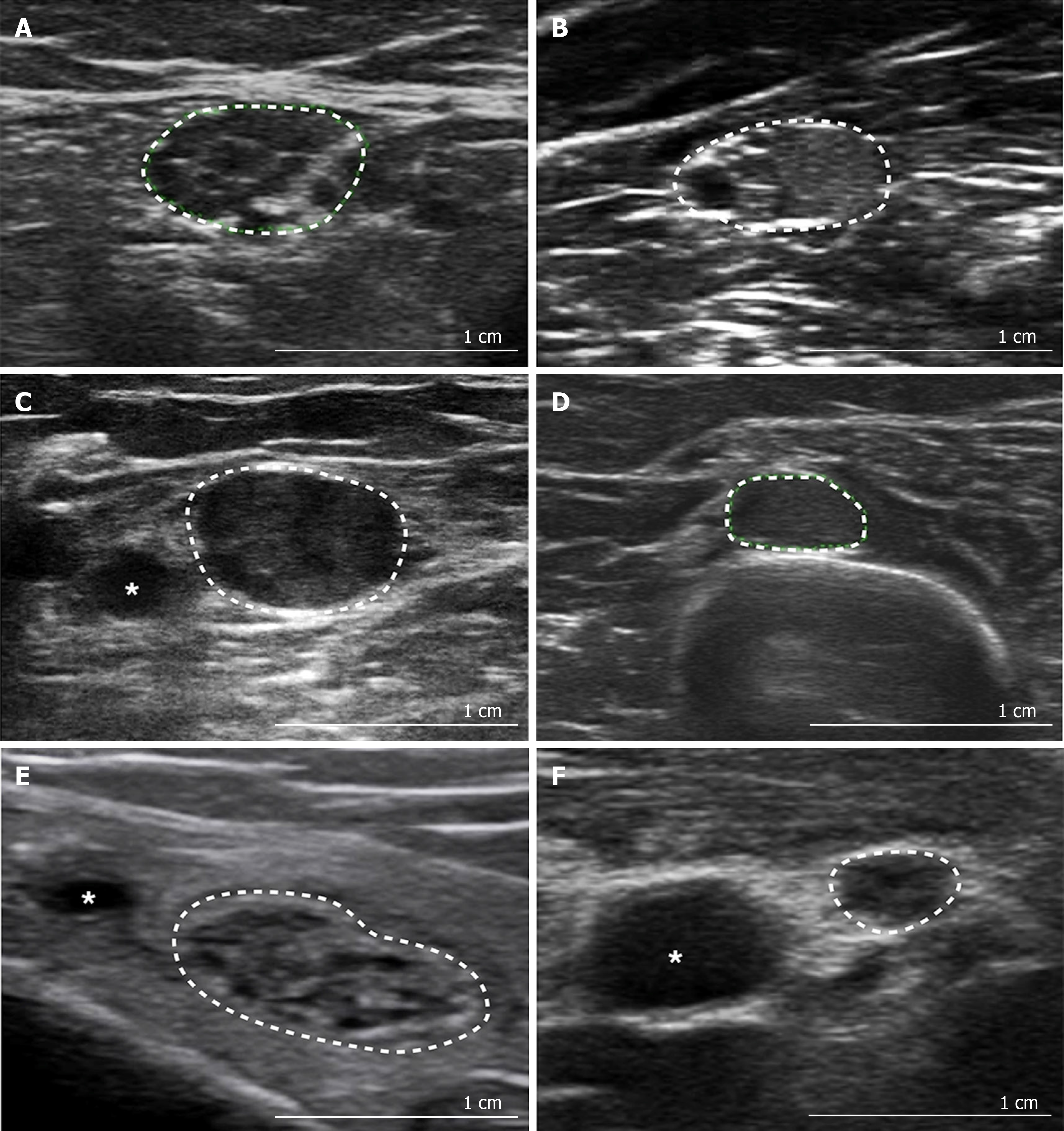
Figure 2 Patterns of neuromuscular ultrasound in peripheral neuropathy.
A: Non-homogenously enlarged, hypoechoic fascicles in Charcot Marie Tooth disease type 1A [tibial nerve at the ankle, cross-sectional area (CSA) 49 mm2]; B: Hyperechoic and hypoechoic fascicles in chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) (median nerve in the forearm, CSA 65 mm2); C: Interruption of the fascicular structure in multifocal acquired demyelinating sensory and motor neuropathy (median nerve at the elbow, CSA 91 mm2); D: Enlarged CSA, in a region normally associated with mono- or oligo-fascicular appearances, in a patient with CIDP (radial nerve at the spiral groove, CSA 27 mm2); E: Enlarged CSA, with reasonably normal fascicular architecture, due to increased perineurial connective tissue in hypertrophic neuropathy (tibial nerve at the ankle, CSA 95 mm2); F: Normal CSA with distorted fascicular architecture in amyloid neuropathy (median nerve at midpoint of the arm, CSA 8 mm2). Citation: Gallardo E, Noto Y, Simon NG. Ultrasound in the diagnosis of peripheral neuropathy: structure meets function in the neuromuscular clinic. J Neurol Neurosurg Psychiatry 2015; 86: 1066-1074. Copyright© The Authors 2020 with permission from BMJ Publishing Group Ltd.
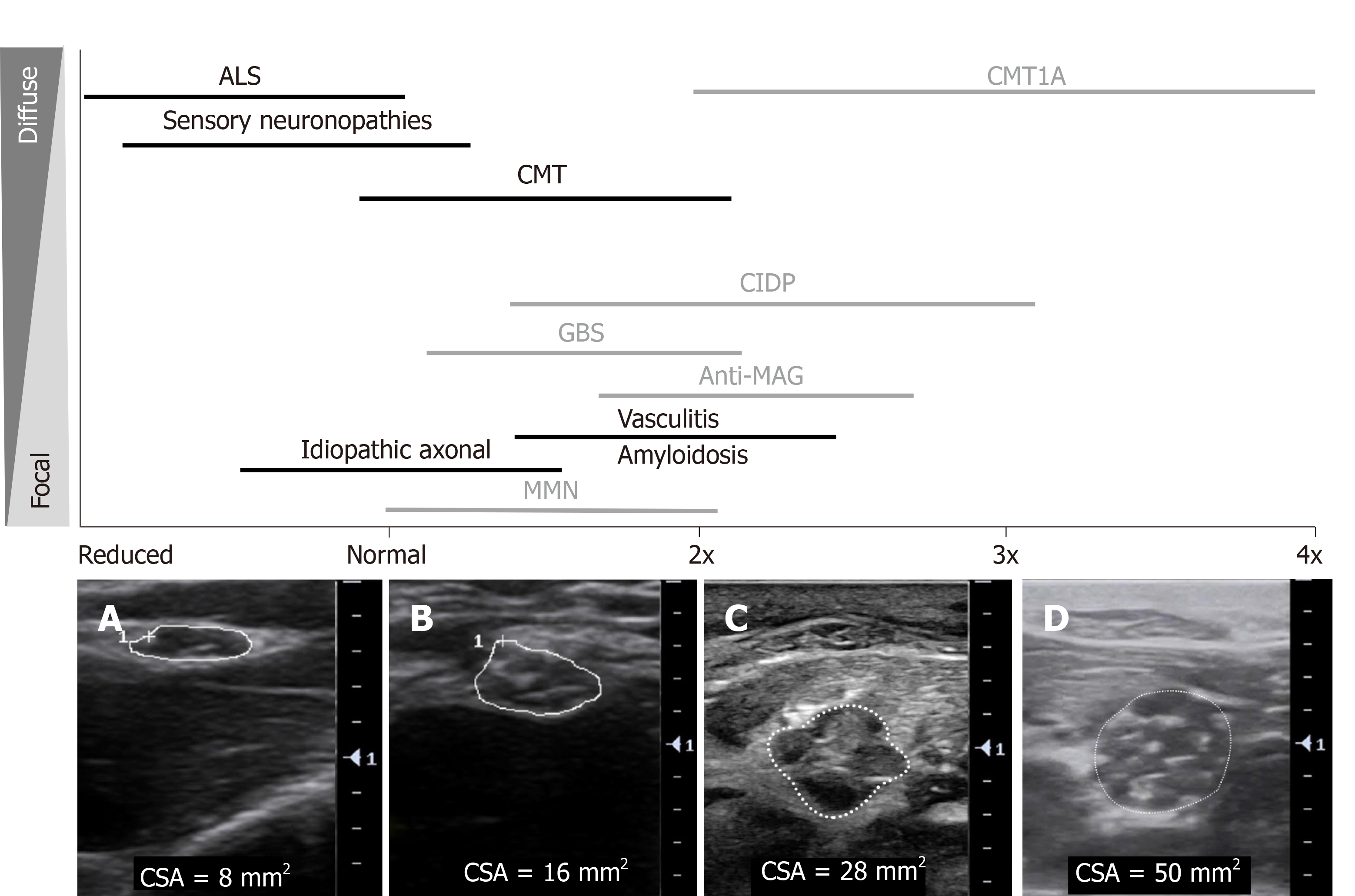
Figure 3 An overview of sonographic findings in inherited and acquired polyneuropathies: degree and distribution of nerve enlargement.
Black: Axonal neuropathies, Grey: Demyelinating neuropathies. Cross-sectional area (CSA) shown in: A: Median nerve at the elbow in a patient with amyotrophic lateral sclerosis, CSA 8 mm2; B: Median nerve at the elbow in a healthy control, CSA 16 mm2; C: Median nerve in the forearm in a patient with chronic inflammatory demyelinating polyradiculoneuropathy, CSA 28 mm2, with heterogeneously enlarged, hypoechoic fascicles; D: Median nerve in the forearm in a patient with Charcot Marie Tooth disease type 1A, CSA 50 mm2, with more homogenously enlarged, hypoechoic fascicles. ALS: Amyotrophic lateral sclerosis; CMT1A: Charcot Marie Tooth disease type 1A; CMT: Charcot-Marie-Tooth disease; CIDP: Chronic inflammatory demyelinating polyradiculoneuropathy; GBS: Guillain-Barre syndrome; MAG: Myelin-associated glycoprotein; MMN: Multifocal motor neuropathy; CSA: Cross-sectional area.
- Citation: Carroll AS, Simon NG. Current and future applications of ultrasound imaging in peripheral nerve disorders. World J Radiol 2020; 12(6): 101-129
- URL: https://www.wjgnet.com/1949-8470/full/v12/i6/101.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i6.101