Copyright
©The Author(s) 2020.
World J Radiol. Oct 28, 2020; 12(10): 213-230
Published online Oct 28, 2020. doi: 10.4329/wjr.v12.i10.213
Published online Oct 28, 2020. doi: 10.4329/wjr.v12.i10.213
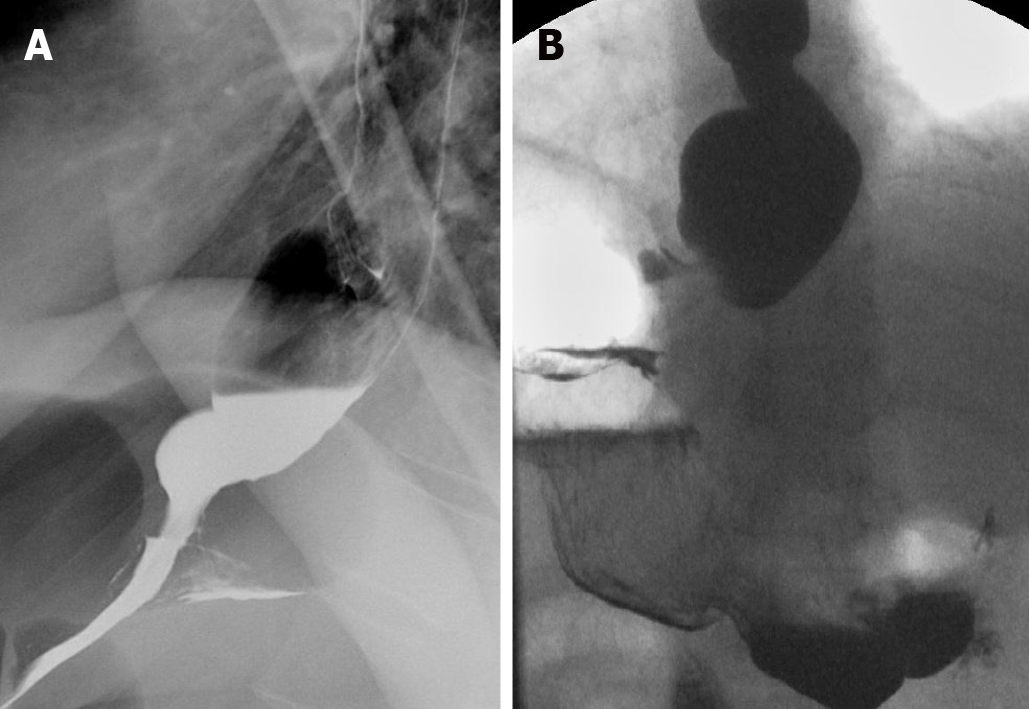
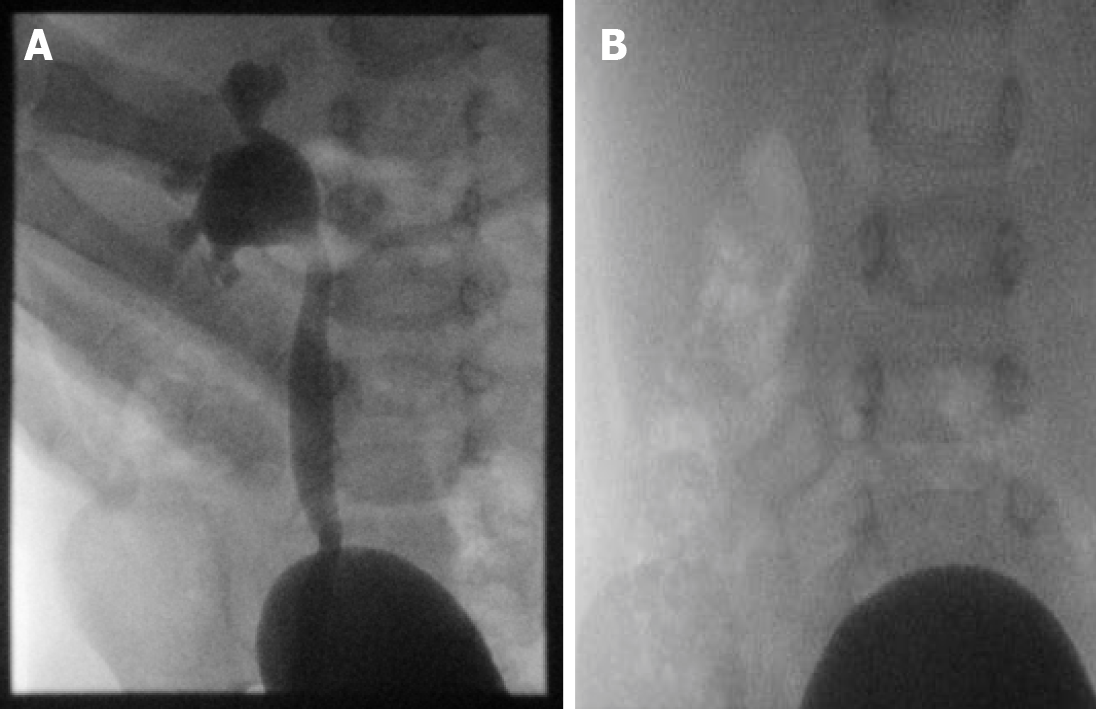
Figure 1 Achalasia.
A and B: Fluoroscopic evaluation showing esophageal dilation and distal tapering of the esophagus.
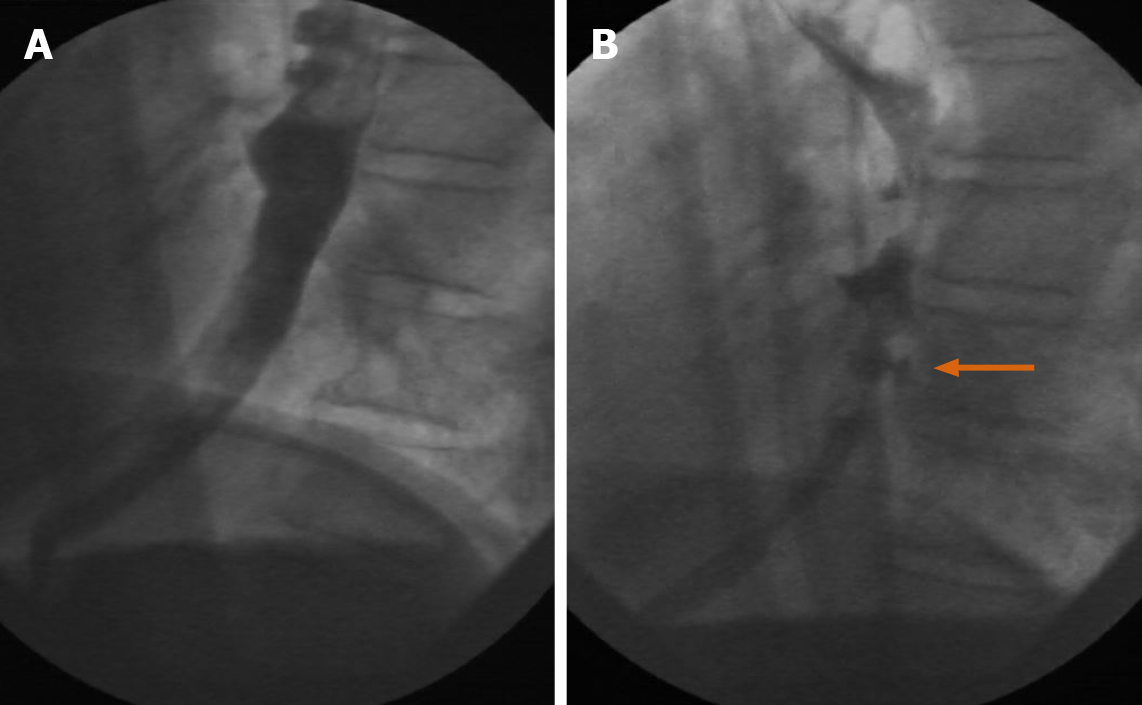
Figure 2 Esophageal pseudodiverticulosis.
A and B: Numerous outpouchings noted along the esophageal contour on oral contrast fluoroscopic examination (orange arrow).
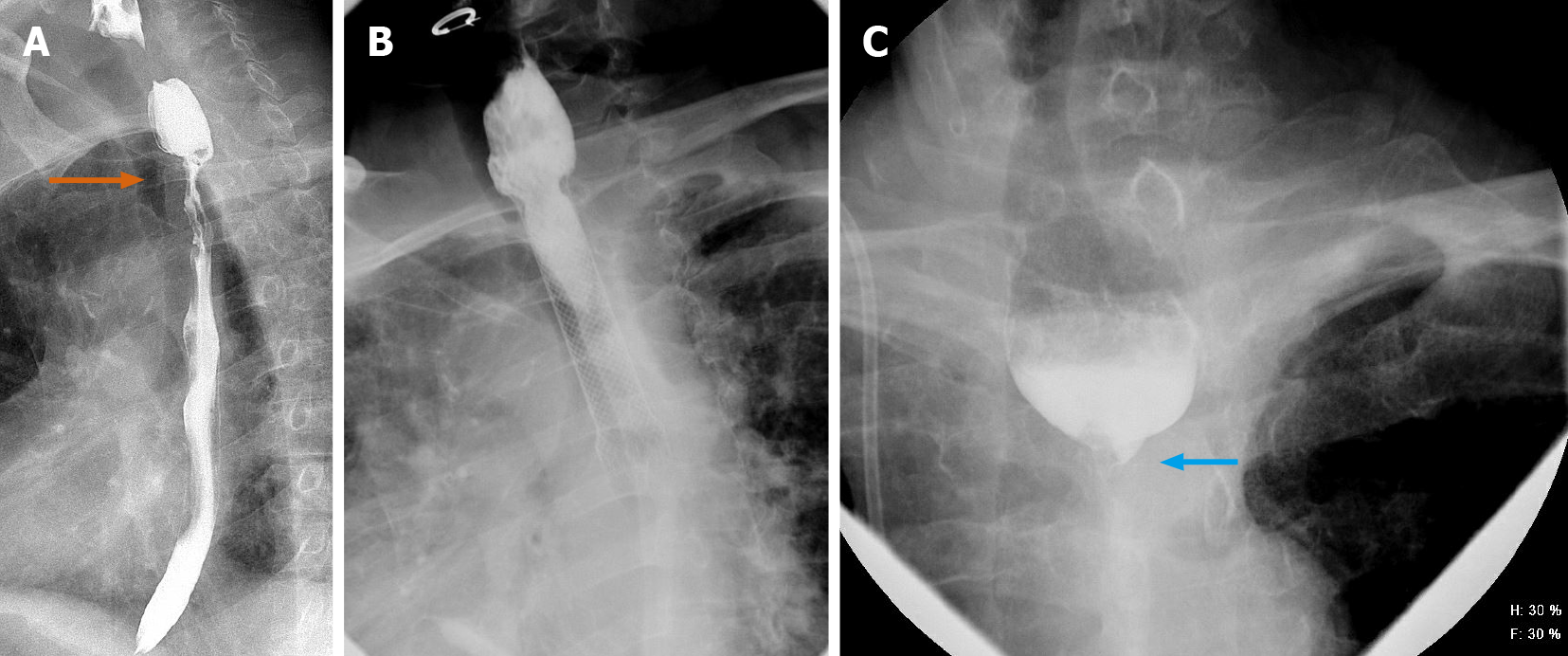
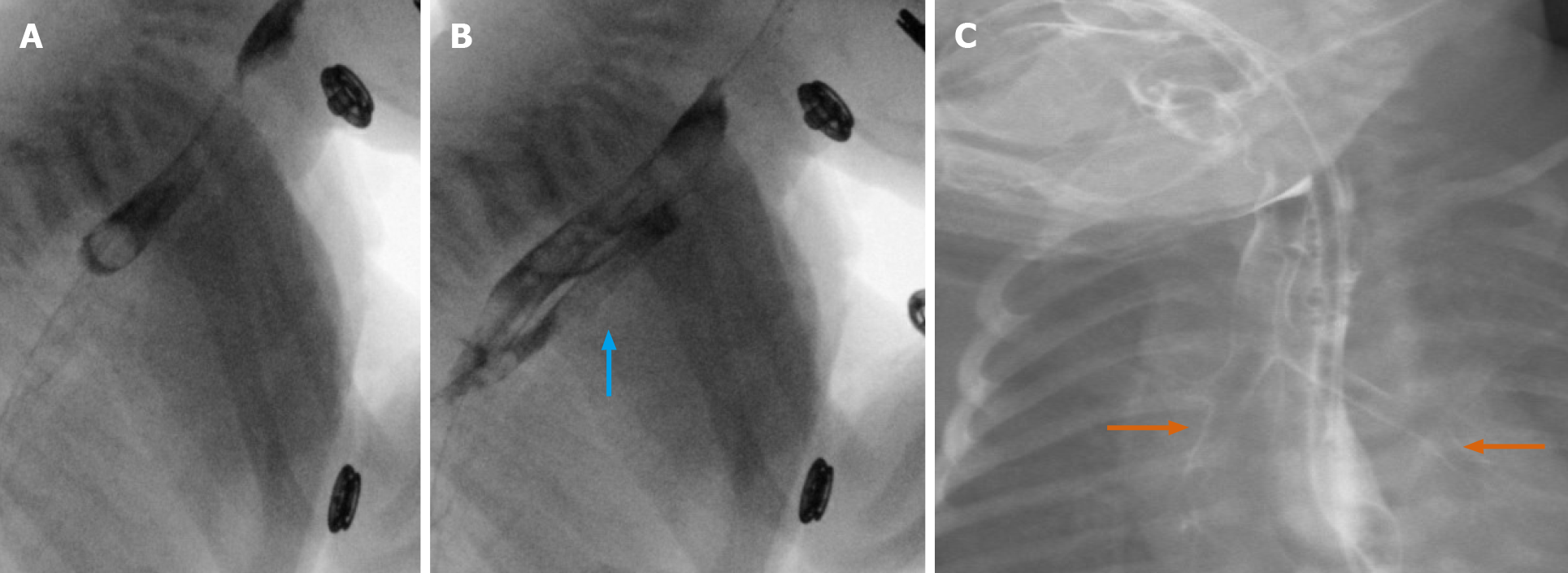
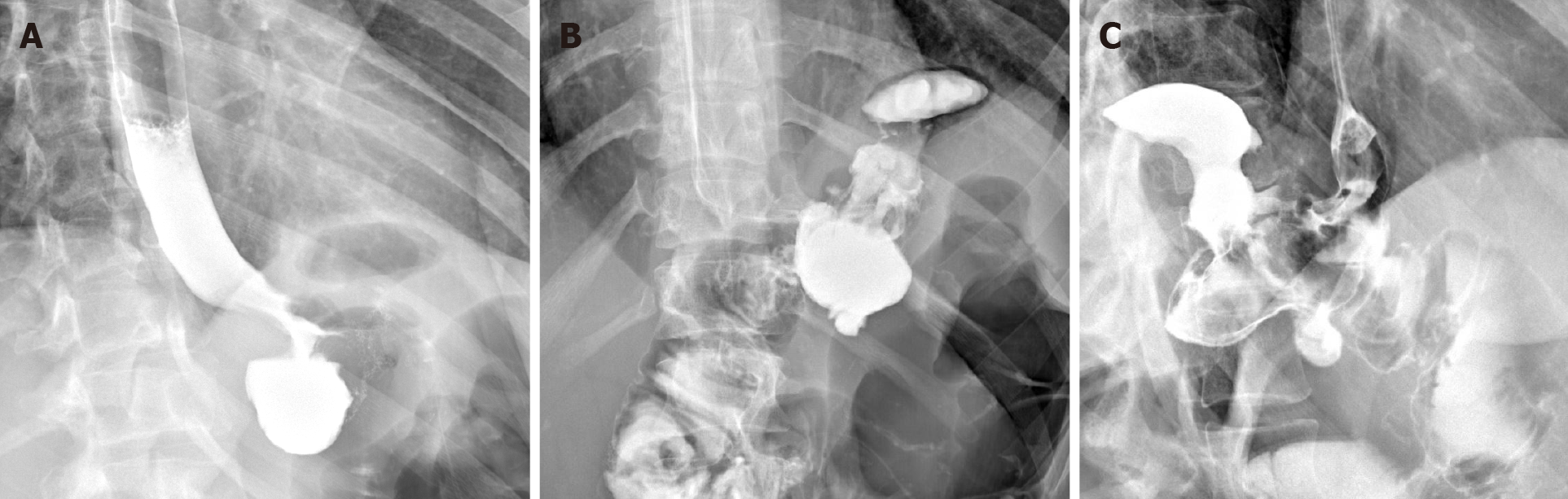
Figure 3 A 64-year-old male.
A-C: Carcinoma of the esophagus showing long segment moderate stenosis with irregular border and “apple core” appearance at the upper esophagus (orange arrow, upper left). Stent was placed, with follow-up exam showing worsening stricture, with near complete occlusion of the esophagus (blue arrow).
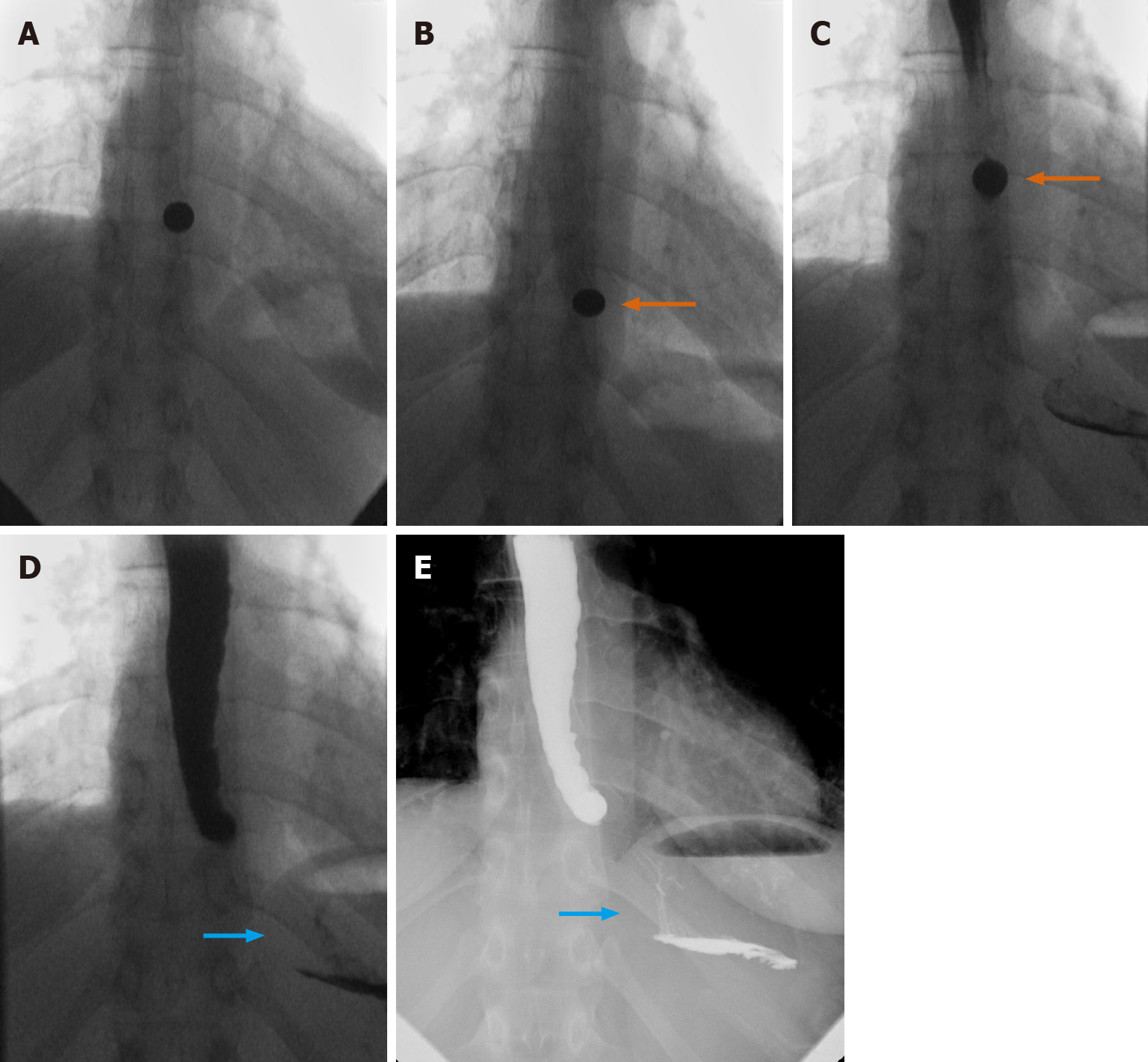
Figure 4 Nonpropulsive esophagus.
A-E: Value of “real-time” evaluation. Nonpropulsive esophagus is seen, with incomplete passage of barium tablet (orange arrows), and ultimately minimal passage of contrast (blue arrows).
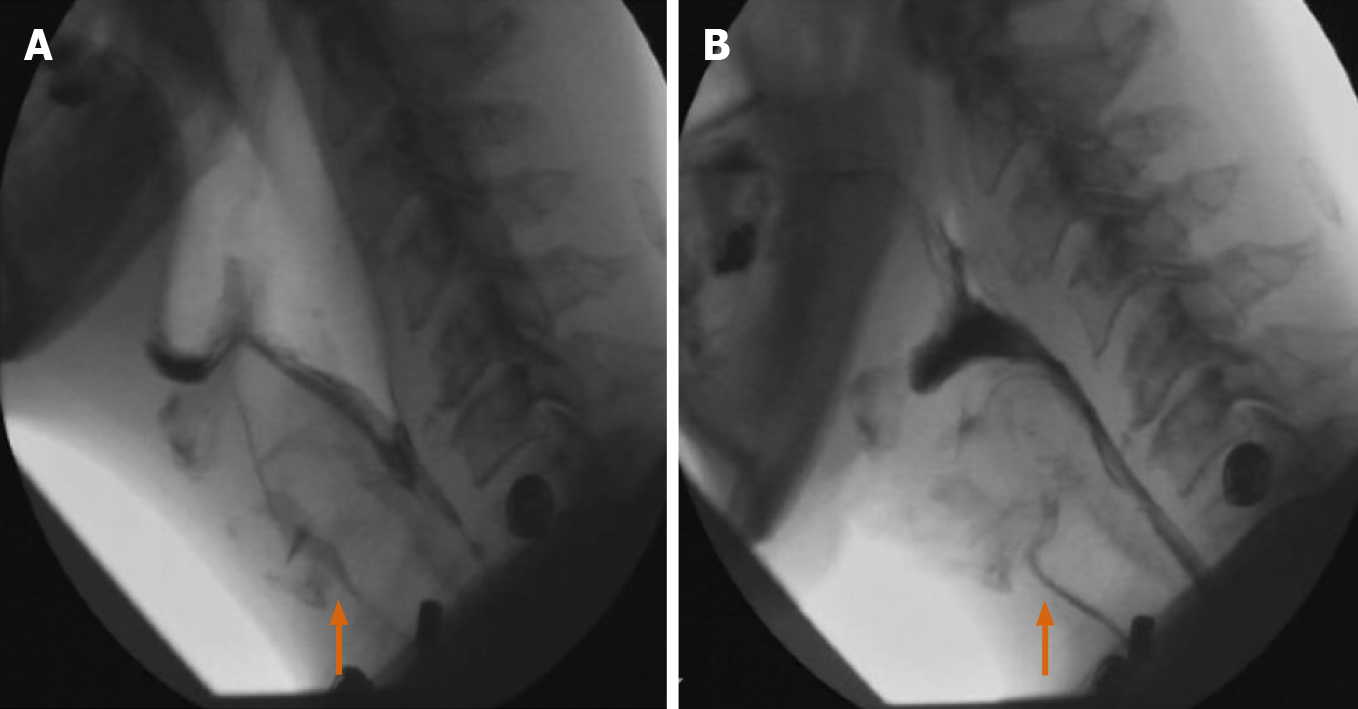
Figure 5 Fluoroscopic views of the rectal region status post anastomosis.
A tiny focal area of extraluminal contrast (blue arrow), noted in the right posterior aspect of the rectum near the suture line.
Figure 6 Modified barium swallow.
A and B: Thin liquid administration showing aspiration during Modified Barium Swallow examination. The second figure shows the same patient, showing aspiration with nectar. Real time labeling was used to identify otherwise difficult-to-differentiate consistencies (orange arrows).
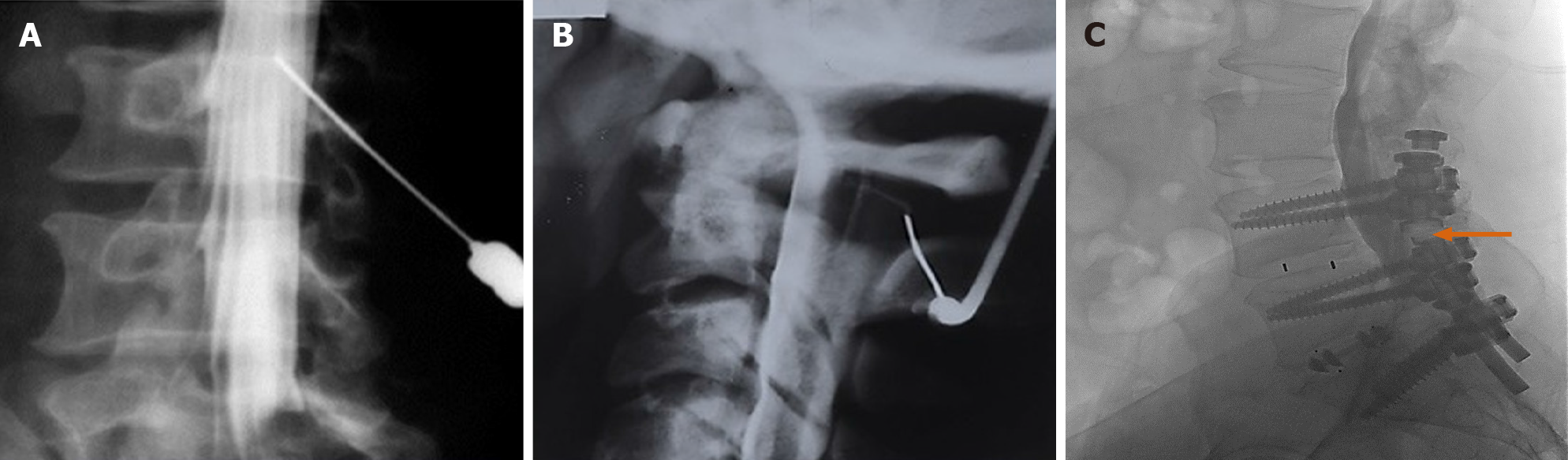
Figure 7 Myelography.
A-C: Needle positioning using real-time fluoroscopy for introduction of non-ionic contrast into the intrathecal space. Real time evaluation allows for close monitoring of contrast placement in the setting of pre-existing hardware (orange arrow), which may limit evaluation on other modalities.
Figure 8 Hysterosalpingogram shows bilateral spillage through both Fallopian tubes, as part of an infertility workup.
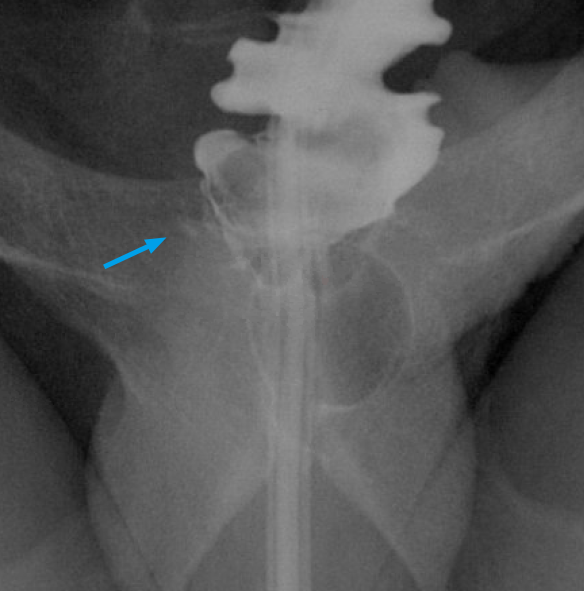
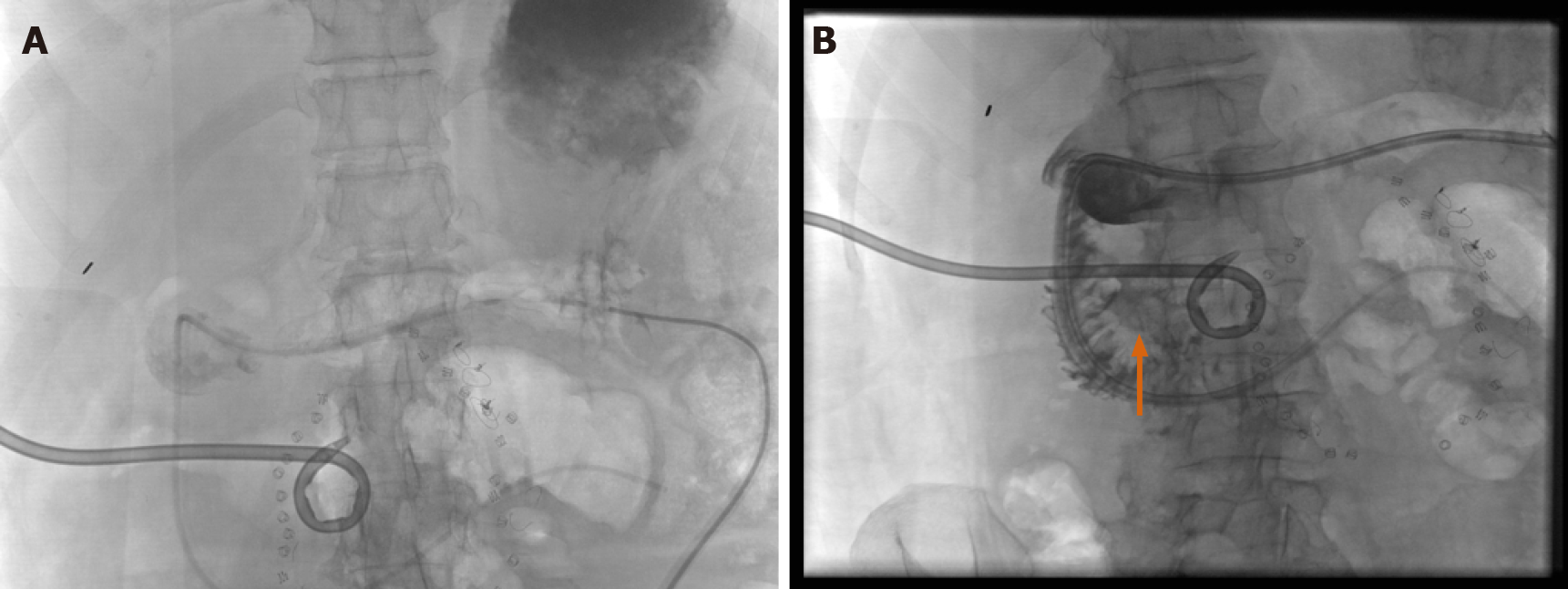
Figure 9 Retrograde urethrocystogram.
A and B: Retrograde urethrocystogram showing significant stricture of the bulbar urethra. Post-urethroplasty fluoroscopic examination showing focal extravasation of contrast (orange arrow). Foley catheter was therefore not removed.
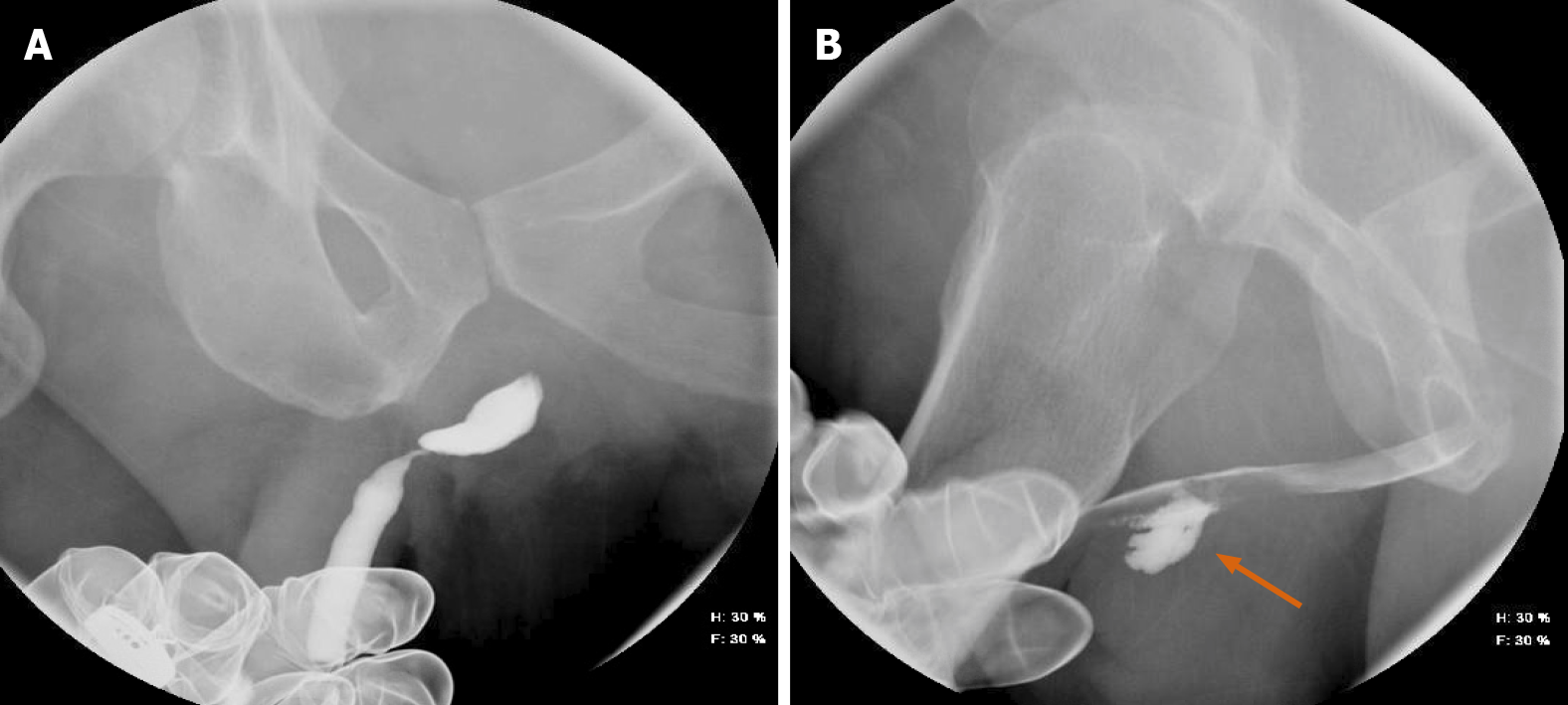
Figure 10 Fluoroscopy.
A and B: Fluoroscopy demonstrating Grade IV severity of hydronephrosis, with resolution.
Figure 11 A 10-mo-old female.
A-C: Lateral and supine fluoroscopic images demonstrating a fistulous tract between the proximal esophagus and proximal trachea on lateral views (vertical blue arrow), with striking outline of the trachea and mainstem bronchi, compatible with tracheoesophageal fistula (orange arrows).
Figure 12 A 4-wk-old male.
A-C: Intestinal malrotation, with duodenal structures appearing to the right of the midline. Follow-up study, performed several days later, with similar characteristic findings (orange arrows).
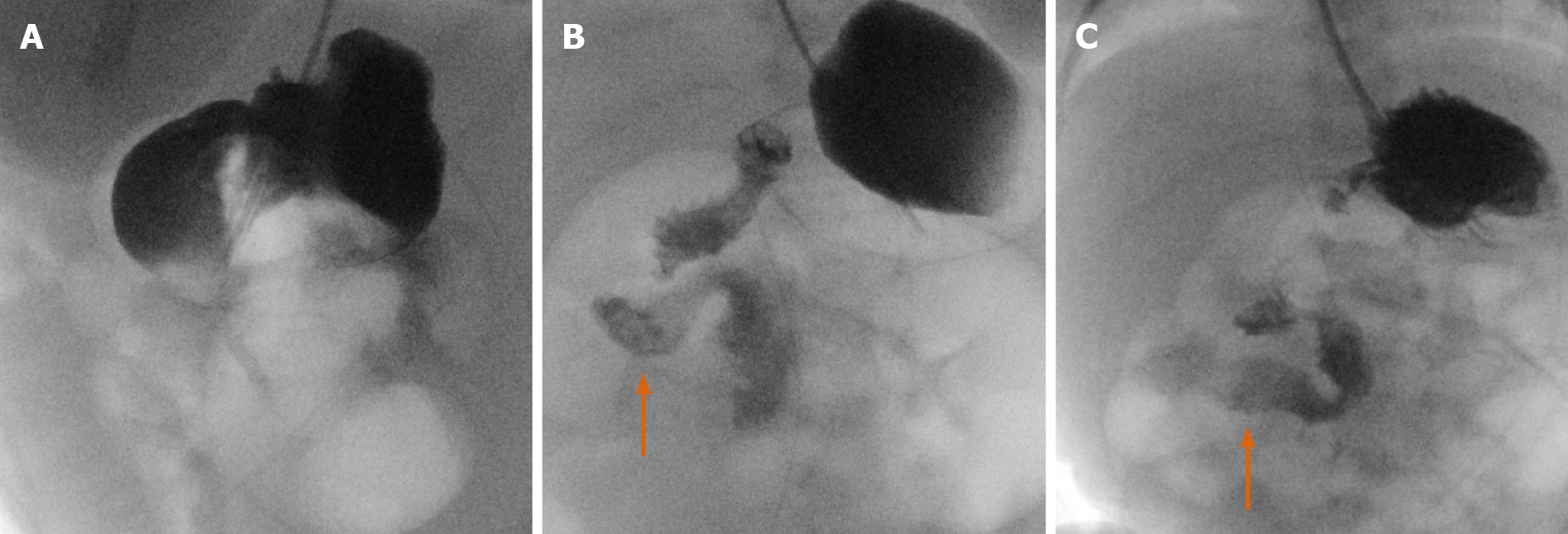
Figure 13 A 2-year-old male.
A-E: Overnight emergent pediatric intussusception reduction from start to finish with multi-modality. Initial computed tomography shows suspected ileocolic intussusception (orange arrows). Subsequent ultrasound of the right lower quadrant with confirmatory findings with telescoping bowel loops. Final two images showing fluoroscopically guided contrast enema, with visualization of telescoped bowel loops (blue arrow) and subsequent resolution.
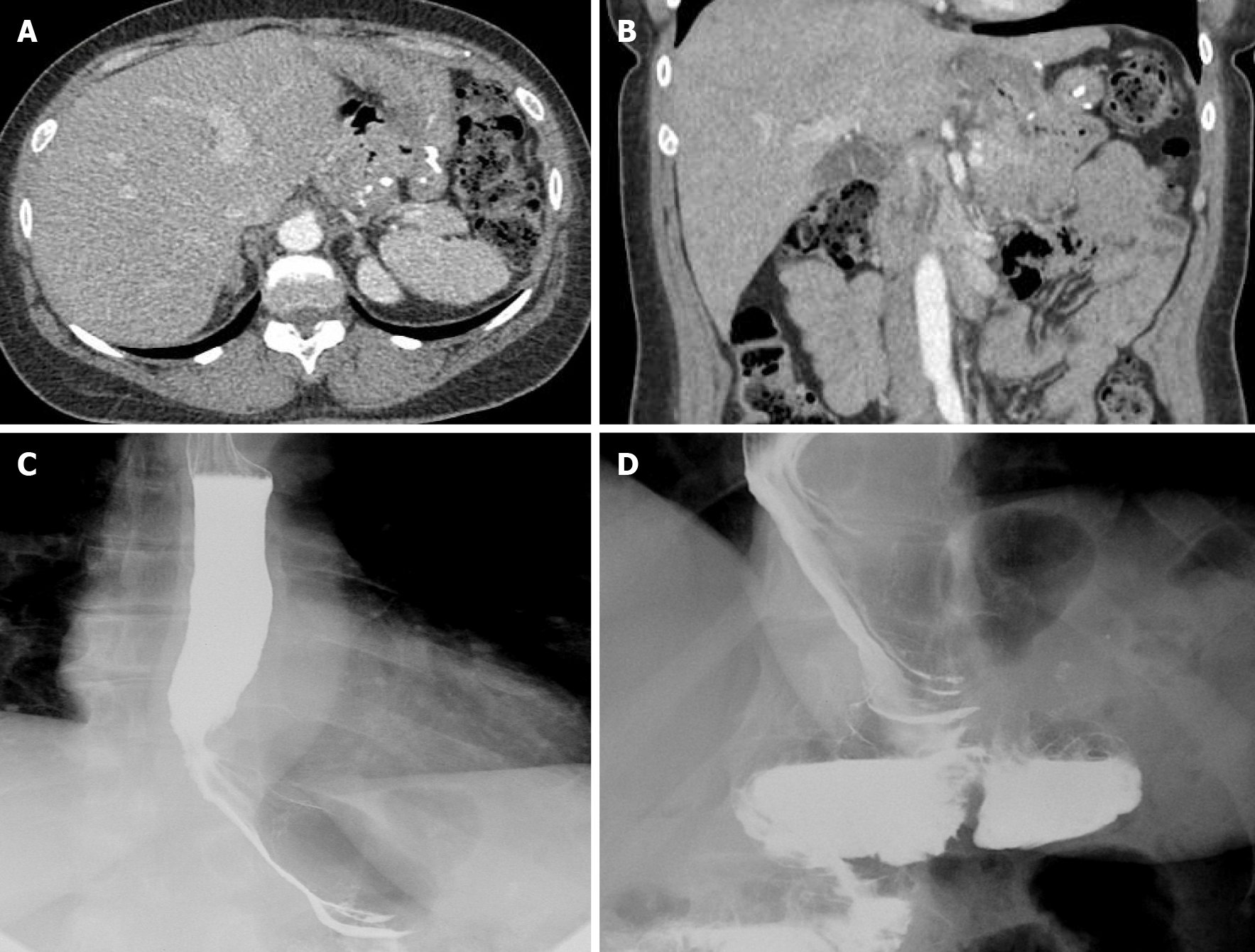
Figure 14 “Beyond computed tomography” in the determination of bowel extraluminal collections.
A: The supine position is utilized in computed tomography, where the G-port of a GJ tube was injected with contrast, then seen localizing to the dependent fundus; B: Real-time fluoroscopic projections with patient in the near-lateral position, showing a fistulous communication with anterior abscess and duodenal sweep (vertical orange arrow).
Figure 15 A 34-yr-old female.
A-C: Contained gastric leak in a patient status post both gastric sleeve and Roux-en-Y procedures, with steep oblique and delay imaging showing contrast entering a contained leak and quite easily seen on fluoroscopic examination. Finding was not identified on initial computed tomography examination.
Figure 16 Status post previous gastric sleeve bypass surgery with conversion to Roux-en-Y bypass.
A and B: Initial contrast computed tomography evaluation of patient (status post gastric bypass) presenting with abdominal pain. The computed tomography was read as negative; C and D: Subsequent discovery of gastro-gastric fistula observed with fluoroscopy. Right anterior oblique positioning was utilized. Findings were then positively correlated on upper endoscopic examination.
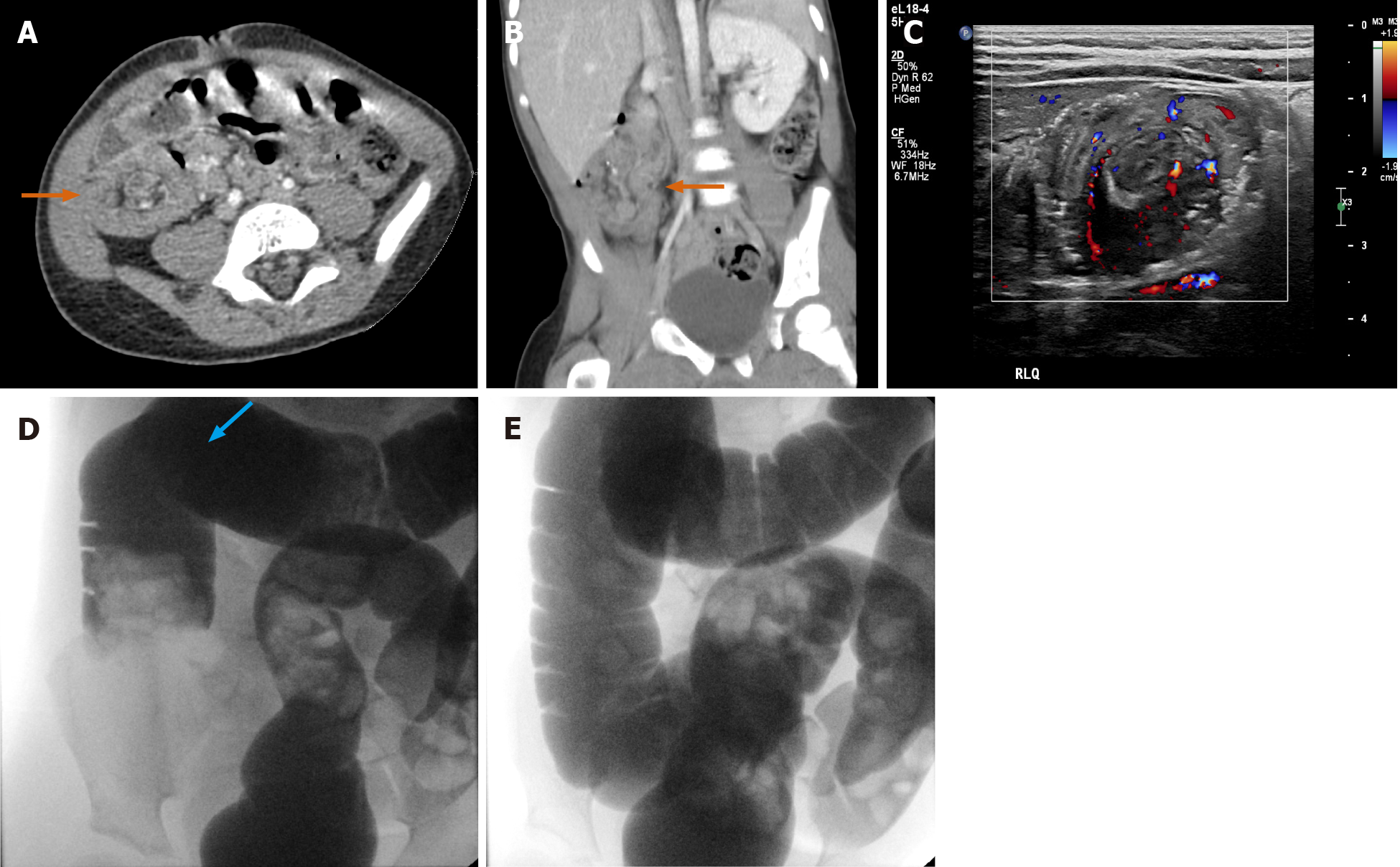
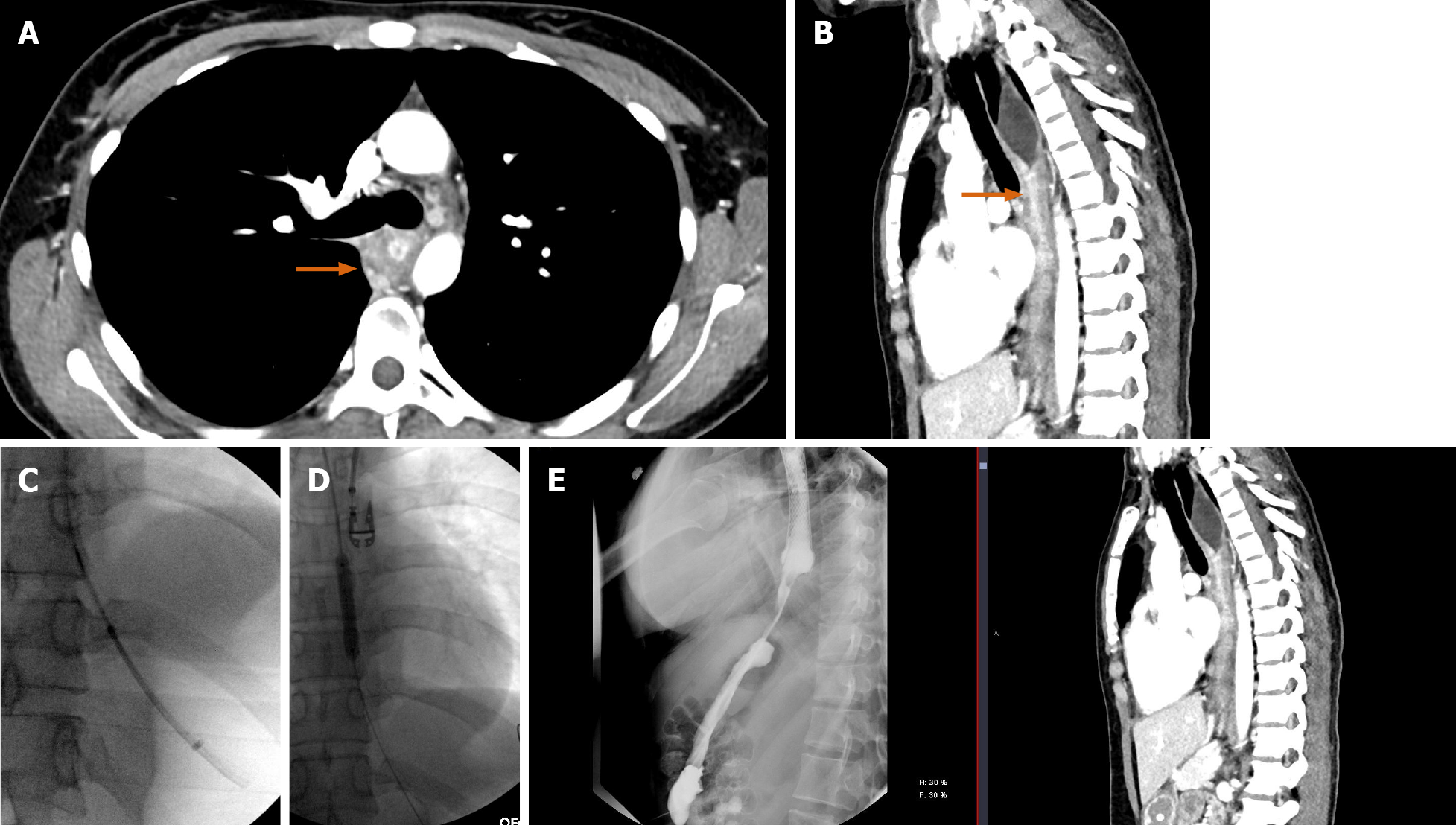
Figure 17 A 26-yr-old male.
A and B: Axial and sagittal computed tomography (CT) images showing long-segment esophageal stenosis related to caustic ingestion (orange arrows); C and D: With an initial upper endoscopy aborted, repeat upper endoscopy with the addition of fluoroscopic guidance allowed passage through a known stricture and eventual stent placement; E: Subsequent fluoroscopic upper gastrointestinal examination showing free contrast passage through the stented esophagus, with direct sagittal comparison to the initial CT in the sagittal plane.
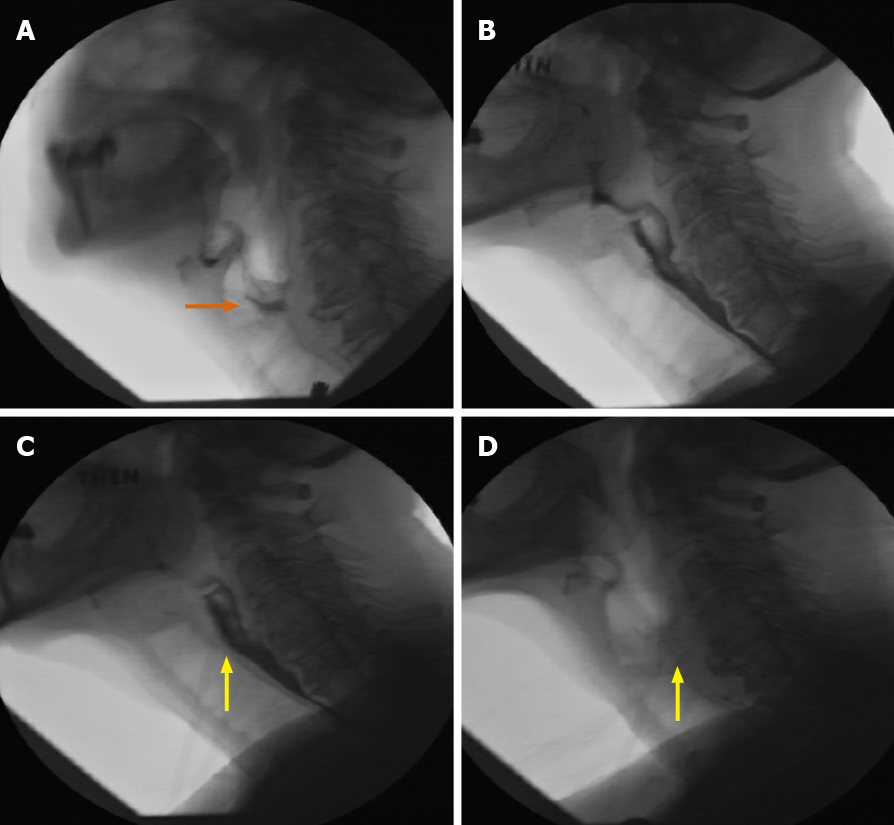
Figure 18 A 69-yr-old female.
A: Initial fluoroscopic examination of a patient with dysphagia demonstrating disorganized swallow and penetration to the level of the vocal cords (orange arrow); B: Follow-up fluoroscopic swallow examination (without neostigmine) demonstrating improvement in organized swallow with only mild flash penetration; C and D: Immediate follow-up examination with administration of neostigmine, showing no significant penetration at multiple consistencies, along with significant improvement in organized swallow (yellow arrows). Neurology consultation concurred with the diagnosis of myasthenia gravis, particularly based on the fluoroscopic series of examinations.
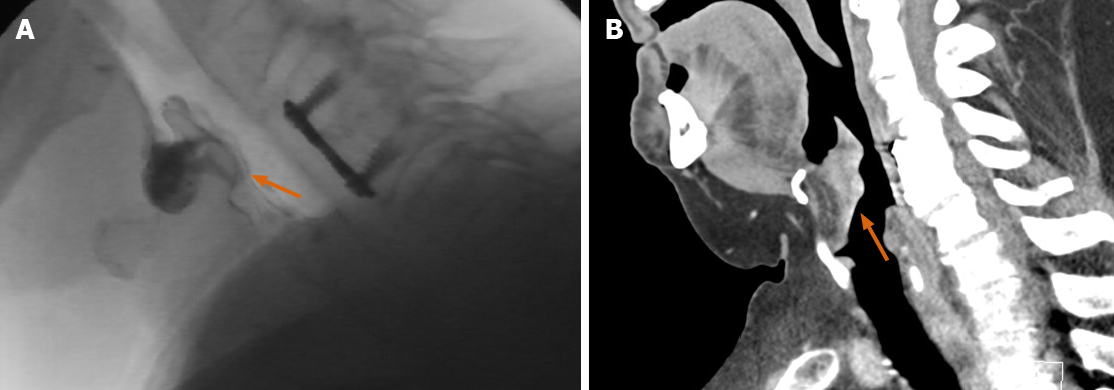
Figure 19 A 64-yr-old male.
A: Incidental discovery of a prominent soft tissue density at the inferior aspect of the epiglottis on fluoroscopic modified barium swallow examination (orange arrow); B: Computed tomography neck, performed after incidental fluoroscopic discovery. Identification of an enlarged, irregular, and enhancing epiglottis concerning for primary mucosal malignancy (orange arrow).
- Citation: Shalom NE, Gong GX, Auster M. Fluoroscopy: An essential diagnostic modality in the age of high-resolution cross-sectional imaging. World J Radiol 2020; 12(10): 213-230
- URL: https://www.wjgnet.com/1949-8470/full/v12/i10/213.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i10.213