Published online Apr 26, 2017. doi: 10.4330/wjc.v9.i4.391
Peer-review started: July 11, 2016
First decision: September 2, 2016
Revised: October 18, 2016
Accepted: December 16, 2016
Article in press: December 19, 2016
Published online: April 26, 2017
Processing time: 291 Days and 7.6 Hours
Aortic root rupture and cardiac tamponade during transcatheter aortic valve implantation is a frightening complication with high mortality rate. A conservative management of this complication could represent an initial strategy, especially in high-risk patients, to avoid emergent cardiac surgery. This conservative management includes: Immediate detection of pericardial effusion by echocardiography, a fast instauration of pericardial drainage, auto-transfusion and anticoagulation reversal. We describe two cases of patients who suffered this complication and were treated successfully with this initial approach.
Core tip: Aortic root rupture during transcatheter aortic valve implantation is a rare but severe complication with high mortality rate. We described two cases of aortic root rupture where we realized a conservative management with rapid anticoagulation reversal and pericardial drainage with blood auto-transfusion. These cases highlight the utility of rapid identification of aortic root hematoma and pericardial effusion by transesophageal echocardiography. Immediate detection of this complication allows to stabilize the patient avoiding further urgent interventions.
- Citation: Vannini L, Andrea R, Sabaté M. Conservative management of aortic root rupture complicated with cardiac tamponade following transcatheter aortic valve implantation. World J Cardiol 2017; 9(4): 391-395
- URL: https://www.wjgnet.com/1949-8462/full/v9/i4/391.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i4.391
Transcatheter aortic valve implantation (TAVI) is gaining ground for the treatment of severe aortic stenosis (AS) in patients with high risk of surgery or contraindications. However, it is a technical and complex procedure with intra and periprocedural risks of complications that could eventually need emergent cardiac surgery (ECS). Among the potential complications, aortic root rupture with subsequent cardiac tamponade is one of the most feared. No data are available about the best management of cardiac tamponade secondary to aortic root rupture during TAVI. Nevertheless, it is well known that ECS, especially in patients with cardiac tamponade, entails a high mortality rate[1]. Pericardiocentesis followed by conservative management of cardiac tamponade secondary to aortic root rupture during TAVI could be an initially effective approach to this complication if the prosthetic valve function is preserved.
We herein present two cases of conservative management of cardiac tamponade following aortic root rupture during TAVI.
An 89-year-old lady with symptomatic severe AS was scheduled for a TAVI. Transthoracic echocardiography (TTE) showed a severe AS (mean gradient: 48 mmHg; aortic valve area of 0.5 cm2, with preserved ejection fraction, 55%). Computed tomography scanner (CT-scan) showed severe calcification of the valve and the following measurements: Minimum/maximum annulus transverse diameter of 23 mm/26 mm, aortic root perimeter of 83 mm and aortic root area of 5 cm2. She was rejected for surgical aortic valve replacement because of high surgical risk related to advanced age (Charlson score: 6; Barthel Score: 100; Logistic Euroscore: 13.57%).
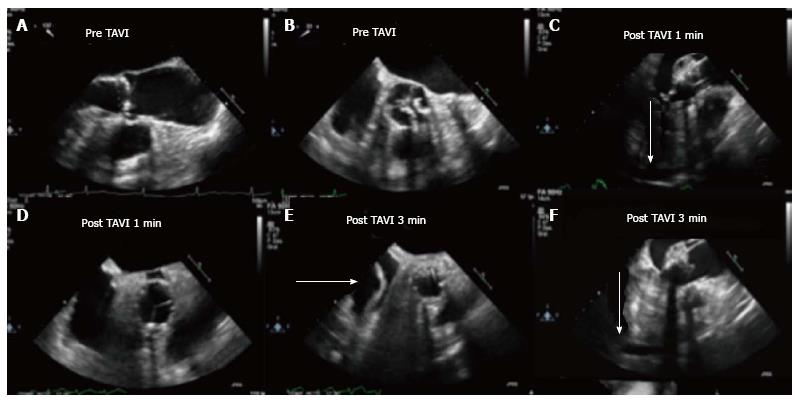
General anaesthesia and mechanical ventilation support were used to allow trans-esophageal echocardiography (TEE) guidance. TEE showed an aortic annulus diameter of 22-mm (Figure 1A and B). Anti-coagulation with unfractionated heparin adjusted for body weight was administered before the implantation. Aortic valve pre-dilatation under fast ventricular pacing was performed without complications and a 26-mm Edwards Sapien XT valve (Edwards Lifesciences, Irvine, California) was implanted.
Immediately after implantation, the patient presented sudden hypotension and TEE showed an expanding aortic root hematoma (Figure 1C and D); with progressively formation of pericardial effusion with signs of cardiac tamponade (Figure 1C, E and F). Percutaneous pericardiocentesis was performed, draining 200 mL of blood that were re-infused. Volume replacement and coagulation reversal with protamine were also performed with initial patient stabilization.
ECS was dismissed because of the high surgical risk and a conservative management was decided. During the first 72 h the patient persisted with hemodynamic instability controlled with volume load (fluid and blood) and repeated pericardial drainages to maintain a mean arterial pressure > 60 mmHg. Finally, the weaning from mechanical ventilation was successfully performed and the patient could be transferred to the conventional ward and discharged one month after the procedure.
At one-year follow-up the patient was almost fully independent for basic activities of daily living (Barthel Score: 95).
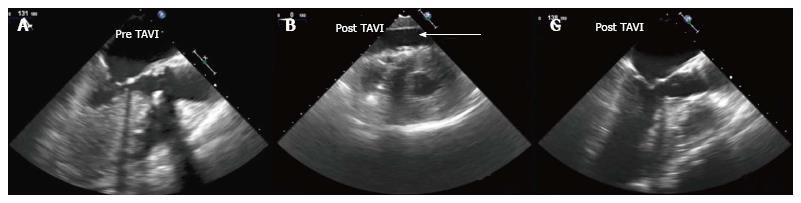
An 81-year-old woman with hypertension, renal impairment with glomerular filtration rate < 30 mL/min and severe AS (TTE mean gradient: 55 mmHg; aortic valve area of 0.78 cm2) with preserved ejection fraction (65%) was referred to TAVI. The patient had refused surgical treatment, after a complete evaluation by the Heart Team a TAVI procedure was proposed and finally accepted. TEE showed a severe calcified AS (mean-maximum transvalvular gradient were 58/100 mmHg, respectively) with an aortic annulus diameter of 22 mm. CT-scan measures (minimum/maximum annulus transverse diameters 22 mm and 27 mm, respectively; aortic root perimeter of 80 mm with an area of 4.7 cm2) and TEE lead to the selection of a 26 mm Edwards Sapien XT valve (Edwards Lifesciences, Irvine, California). Anticoagulation was reached with unfractionated heparin adjusted for body weight. Aortic valve predilatation under fast ventricular pacing was performed without complications; and the 26 mm valve was implanted. TEE immediately after TAVI showed a minimal paravalvular leak with normofunctional prosthetic valve.
However, one minute later, the patient presented sudden hypotension, and pericardial effusion and signs of cardiac tamponade appeared evident on TEE without signs of aortic root hematoma or dissection (Figure 2). Percutaneous pericardiocentesis was performed draining 300 mL of blood that were reinfused into the patient and coagulation was reversed with protamine. The patient was hemodynamically stabilized and was transferred to the acute cardiac care unit.
Pericardial drainage was performed every eight hours during two days to maintain mean arterial pressure > 60 mmHg. After successful weaning from the ventilator, the patient was dismissed from the coronary intensive care unit and was finally discharged home at day 19 after TAVI procedure.
At one month follow-up, the patient presented new onset symptoms of heart failure. A TEE showed a severe aortic regurgitation with three different jets: One main central jet (apparently secondary to valve geometry alteration with an eccentric closure of valves) and two perivalvular leaks, with minimal pericardial effusion. The patient did not respond to optimal medical treatment and persisted in functional class NYHA IV. Finally, the heart team decided a surgical approach for TAVI replacement. A biologic valve prosthesis Mitroflow 19 mm (Sorin Group Inc.) was successfully implanted and aortic root rupture was confirmed. However, the patient suffered from several postoperatively complications including septic shock that resulted in death 1 mo after second procedure.
An initially conservative management of aortic root rupture and cardiac tamponade during TAVI procedures may represent an appropriate approach in this high-risk population. Although uncontained aortic root rupture affects only to 0.5%-1% of the patients treated with a TAVI intervention, a contained rupture could occur in up to 5% of procedures[1]. Otherwise, as mentioned above, it is well known the increased risk of mortality of ECS in patients with cardiac tamponade[2]. Data on the need of ECS after TAVI is scarce, but it has been reported an incidence of about 1%[2]. In this regard, 30-d mortality rate in TAVI patients who need ECS may exceed 50%[2]. This is especially true in patients complicated with cardiac tamponade or annulus rupture in whom mortality rate may range between 60% and 100%[2-4].
There are several issues to be taken into account during the conservative management of this complication. First, it is mandatory to immediately identify the root rupture during the procedure. In this regard, intraoperative TEE is useful as aortic root hematoma could represent the first sign of aortic root rupture and may precede the development of hemodynamic instability and pericardial effusion. Aortic root hematoma was identified only in the first case. In the second case, the evidence of pericardial effusion on TEE allowed the diagnosis that was confirmed during valve-replacement surgery. Secondly, the rapid reversal of coagulation with protamine sulfate may help avoid progression of the hematoma. Finally a rapid percutaneous pericardial drainage and blood auto-transfusion connecting a drainage catheter directly into a central line is mandatory to stabilize hemodynamics of the patient.
Although it is well known that patients who need ECS present poor prognosis[2-5], except for tamponade secondary to right ventricular tears[6], it is not clear whether the patient with cardiac tamponade secondary to aortic root rupture could benefit from an invasive management.
Several mechanisms could be involved in the development of this complication. The extensive calcification of left ventricular outflow tract (LVOT), the mismatches between the aortic root and the prosthesis (TAVI oversizing) and the ellipsoid geometry of aortic root have been proposed as potential predictors of this ominous complication[1,7,8].
In the above-mentioned cases, the aortic annulus measured with CT-scan revealed an ellipsoid geometry (26 mm × 23 mm and 26 mm × 22 mm), with an eccentricity indexes of 0.12 and 0.15, respectively that did not exceed the normal value described in previous series[7]. The combination of ellipsoid geometry and the presence of severe and extensive calcification could be the cause of aortic root injury. Oversizing was calculated in 6% and 13% in our first and second case, respectively. A significant area-oversizing threshold > 20% was associated with aortic rupture[7]. However, it is plausible that an oversizing that exceeds 10% may still entail a higher risk of aortic root rupture.
An extensive study of the aortic root area with measurement of the perimeter, diameter, geometry and annulus-LVOT calcification with CT-scan, may help avoid excessive prosthesis oversizing and identify geometry incompatibility between prosthesis and landing zone because of its irregular geometry.
This initial conservative management could stabilize both patients and as a matter of fact, they were successfully discharged home. In the second case, however, further alteration of valve geometry caused severe prosthetic dysfunction and a surgical procedure was required. Eventually, the patient suffered from postoperatively complications and finally died. Nevertheless, the initial conservative management could allow further surgery in a more stable condition with higher chances of survival.
In conclusion, the risk of aortic root rupture during TAVI is difficult to predict despite an extensive study by TEE and CT-scan. Immediate detection of this complication during the TAVI procedure may allow rapid instauration of measures (anticoagulation reversal and pericardial drainage with auto-transfusion) that lead to stabilize the patient and avoid further ECS. Further investigation is needed to predict, avoid and manage the aortic root rupture in TAVI patients.
We are grateful to Dr. Susanna Prat for her contribution, analysis and interpretation of CT-scan images, and to the Acute Cardiac Care Unit staff and to the Transcatheter Aortic Valve Implantation Heart Team of our center for their collaboration.
The authors describe two cases of post-transcatheter aortic valve implantation (TAVI) cardiac tamponade with successful initial conservative management.
Sudden hypotension and hypoperfusion.
Acute bleeding (retroperitoneal, TAVI-access site bleeding), heart-block, prosthetic-valve dysfunction.
Transesophageal echocardiography and invasive hemodynamics are the main diagnostic tools.
Transesophageal echocardiography confirmed cardiac tamponade in both cases. In the case 1 showed an aortic root hematoma and pericardial effusion, in the case 2 did not identify signs of aortic root injury but identified progressive pericardial effusion.
Immediate anticoagulation reversal and pericardial drainage with autotransfusion that lead to stabilize the patient may avoid further emergency cardiac surgery.
Uncontained aortic root rupture is a rare post-TAVI complication (0.5%-1%) but with high mortality rate. TAVI patients who need emergency cardiac surgery with cardiac tamponade or aortic root rupture present a mortality rate between 60% and 100%. The data among conservative management are scarce.
The aortic root is a complex structure that connects the heart to the systemic circulation, it is composed of distinct parts extremely sensitive to injury during TAVI: Valve leaflets (with the commissure and leaflet attachment), inter leaflet triangle, the sino tubular junction and the ventriculo-aortic junction.
Immediate detection of cardiac tamponade during TAVI procedure may allow rapid instauration of measures (anticoagulation reversal and pericardial drainage with auto-transfusion) that lead to stabilize the patient and that can avoid further interventions. Transesophageal echocardiography is the main diagnostic tool.
The case report was well written, and may give rise to an interesting discussion on the described problem.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lin GM, Rauch B, Teragawa H S- Editor: Gong XM L- Editor: A E- Editor: Lu YJ
| 1. | Blanke P, Reinöhl J, Schlensak C, Siepe M, Pache G, Euringer W, Geibel-Zehender A, Bode C, Langer M, Beyersdorf F. Prosthesis oversizing in balloon-expandable transcatheter aortic valve implantation is associated with contained rupture of the aortic root. Circ Cardiovasc Interv. 2012;5:540-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 129] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 2. | Eggebrecht H, Mehta RH, Kahlert P, Schymik G, Lefèvre T, Lange R, Macaya C, Mandinov L, Wendler O, Thomas M. Emergent cardiac surgery during transcatheter aortic valve implantation (TAVI): insights from the Edwards SAPIEN Aortic Bioprosthesis European Outcome (SOURCE) registry. EuroIntervention. 2014;10:975-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Hein R, Abdel-Wahab M, Sievert H, Kuck KH, Voehringer M, Hambrecht R, Sack S, Hauptmann KE, Senges J, Zahn R. Outcome of patients after emergency conversion from transcatheter aortic valve implantation to surgery. EuroIntervention. 2013;9:446-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Pasic M, Unbehaun A, Dreysse S, Buz S, Drews T, Kukucka M, D’Ancona G, Seifert B, Hetzer R. Rupture of the device landing zone during transcatheter aortic valve implantation: a life-threatening but treatable complication. Circ Cardiovasc Interv. 2012;5:424-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Sabaté M, Cánovas S, García E, Hernández Antolín R, Maroto L, Hernández JM, Alonso Briales JH, Muñoz García AJ, Gutiérrez-Ibañes E, Rodríguez-Roda J. In-hospital and mid-term predictors of mortality after transcatheter aortic valve implantation: data from the TAVI National Registry 2010-2011. Rev Esp Cardiol (Engl Ed). 2013;66:949-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Rezq A, Basavarajaiah S, Latib A, Takagi K, Hasegawa T, Figini F, Cioni M, Franco A, Montorfano M, Chieffo A. Incidence, management, and outcomes of cardiac tamponade during transcatheter aortic valve implantation: a single-center study. JACC Cardiovasc Interv. 2012;5:1264-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 7. | Barbanti M, Yang TH, Rodès Cabau J, Tamburino C, Wood DA, Jilaihawi H, Blanke P, Makkar RR, Latib A, Colombo A. Anatomical and procedural features associated with aortic root rupture during balloon-expandable transcatheter aortic valve replacement. Circulation. 2013;128:244-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 441] [Article Influence: 36.8] [Reference Citation Analysis (0)] |
| 8. | Bax JJ, Delgado V, Bapat V, Baumgartner H, Collet JP, Erbel R, Hamm C, Kappetein AP, Leipsic J, Leon MB. Open issues in transcatheter aortic valve implantation. Part 1: patient selection and treatment strategy for transcatheter aortic valve implantation. Eur Heart J. 2014;35:2627-2638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |