Published online Apr 26, 2017. doi: 10.4330/wjc.v9.i4.378
Peer-review started: July 14, 2016
First decision: September 30, 2016
Revised: October 12, 2016
Accepted: January 16, 2017
Article in press: January 18, 2017
Published online: April 26, 2017
Processing time: 290 Days and 19.3 Hours
To compare the amount of contrast used during percutaneous coronary intervention (PCI) via trans-radial access (TRA) vs trans-femoral access (TFA).
Scientific databases and websites were searched for:randomizedcontrolledtrials (RCTs). Data were extracted by two independent reviewers and was summarized as the weighted mean difference (WMD) of contrast used with a 95%CI using a random-effects model.
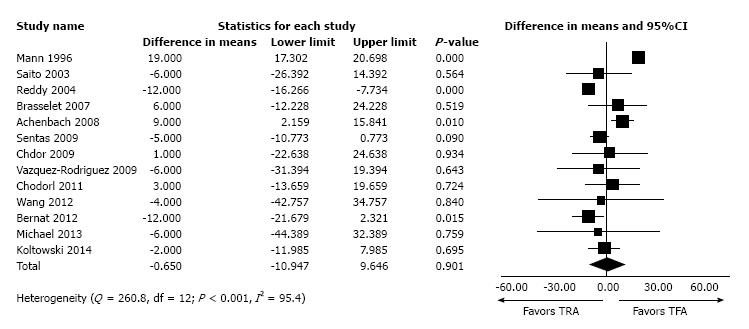
The meta-analysis included 13 RCTs with a total of 3165 patients. There was no difference between the two strategies in the amount of contrast used (WMD = - 0.65 mL, 95%CI: -10.94-9.46 mL; P = 0.901).
This meta-analysis shows that in patients undergoing PCI, the amount of contrast volume used was not different between TRA and TFA.
Core tip: Adaptation of radial access for percutaneous coronary interventions in patients with chronic kidney disease is slower because of concern about contrast-induced nephropathy from the greater contrast load. Data from individual studies vary; therefore we performed a comprehensive meta-analysis of randomized controlled trials comparing the amount of contrast used between radial access and femoral access.
- Citation: Shah R, Mattox A, Khan MR, Berzingi C, Rashid A. Contrast use in relation to the arterial access site for percutaneous coronary intervention: A comprehensive meta-analysis of randomized trials. World J Cardiol 2017; 9(4): 378-383
- URL: https://www.wjgnet.com/1949-8462/full/v9/i4/378.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i4.378
Trans-radial access (TRA) for percutaneous coronary interventions (PCIs) results in a lower risk for bleeding and vascular complications than trans-femoral access (TFA)[1-5]. However, CathPCI registry data suggest that adaption of TRA-PCI in patients with lower glomerular filtration rates (GFRs) is lower compared to patients with higher GFRs; one wonders if this could be the result of concern over the larger amount of contrast used in TRA compared to TFA[6]. Data from individual studies have been variable: Some show larger contrast volume is used with TRA[2,7], others show equal amounts used in both strategies[5,8], and yet others showless contrast used with TRA[3,9]. Therefore, we performed an updated comprehensive meta-analysis of randomized controlled trials (RCTs) comparing the amounts of contrast used in TRA and TFA during PCI.
This meta-analysis was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for systematic reviews and meta-analyses[10]. We performed a systematic search of PubMed, Embase, and the Cochrane Library and cross-referenced relevant articles using various combinations of keywords such as “radial”, “femoral”, “cardiac catheterization”, and “coronary intervention” for eligible published studies. Data were collected by two independent investigators, and disagreements were resolved by consensus. Trials were included if they enrolled patients undergoing PCI and randomly assigned them to TRA or TFA. We recorded mean contrast volume used. We also contacted corresponding authors for those articles not reporting contrast volume or reporting the median contrast used. We were able to obtain the mean contrast used for only one additional trial[11].
We summarized the data as the weighted mean difference (WMD) of contrast used with a 95%CI using Comprehensive Meta-Analysis (CMA) system version 3 (Comprehensive Meta-Analysis; Biostat Inc., Englewood, NJ, United States). A random-effects model was used to analyze data. The presence of heterogeneity across trials was evaluated using the Cochran Q test and the Higgins I2 test[12]. The measure of I2 can be interpreted as the percentage of variability resulting from heterogeneity between studies rather than sampling error[12]. Finally, an additional sensitivity analysis was performed where one study at a time was excluded, and the impact on the summary results of removing each was evaluated.
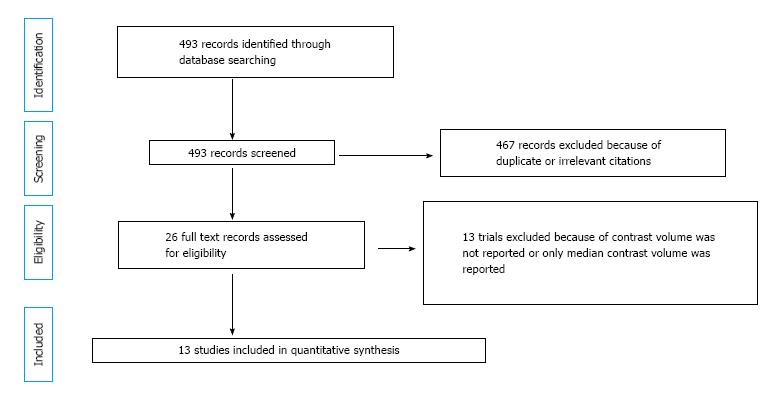
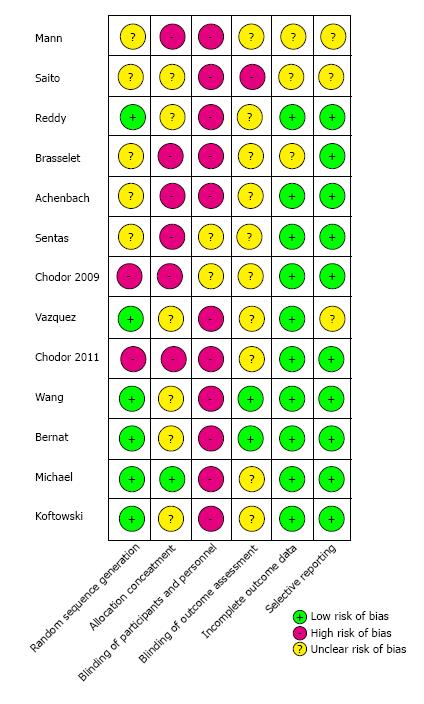
Among 26 identified RCTs, only 15 trials reported the amount of contrast used. However, data for the mean contrast used was available for only 13 RCTs, which used 3165 patients, and these were used for final analysis[4,5,7,11,13-20]. Figure 1 shows the search flow diagram. The bias assessment for each RCT is shown in Figure 2.
The characteristics of the individual trials included in the meta-analysis are shown in Table 1. Most studies were single-center studies with broad spectra of patient populations, including patients with stable angina, acute coronary syndrome, or ST-elevation myocardial infarction. The majority of the procedures were performed by radial experts.
| Ref. | Year | TRA (n) | TFA (n) | Mean contrast volume (mL) | TRA operator experience | Patient population | |
| TRA | TFA | ||||||
| Mann et al[13] | 1996 | 73 | 75 | 138 | 119 | NR | ACS |
| Saito et al[14] | 2003 | 77 | 72 | 180 | 186 | Experienced | AMI |
| Reddy et al[15] | 2004 | 25 | 50 | 123 | 135 | Low | Elective PCI |
| Brasselet et al[4] | 2007 | 57 | 57 | 97 | 91 | Intermediate-experienced | ACS |
| Achenbach et al[5] | 2008 | 152 | 155 | 88 | 79 | Experienced | ACS, Elective PCI |
| Sentas et al[16] | 2009 | 335 | 335 | 84 | 89 | Experienced | ACS, Elective PCI |
| Chodór et al[17] | 2009 | 50 | 50 | 198 | 197 | Experienced | STEMI |
| Vazquez-rodriguez et al[18] | 2009 | 217 | 222 | 275 | 281 | Experienced | AMI |
| Chodór et al[19] | 2011 | 49 | 59 | 165 | 162 | Experienced | STEMI |
| Wang et al[20] | 2012 | 60 | 59 | 160 | 164 | Experienced | STEMI |
| Bernat et al[3] | 2012 | 348 | 359 | 170 | 182 | Experienced | STEMI |
| Michael et al[7] | 2013 | 63 | 63 | 171 | 142 | Experienced | NSTEMI or elective PCI with previous CABG |
| Kołtowski et al[11] | 2014 | 52 | 51 | 63 | 65 | Experienced | STEMI |
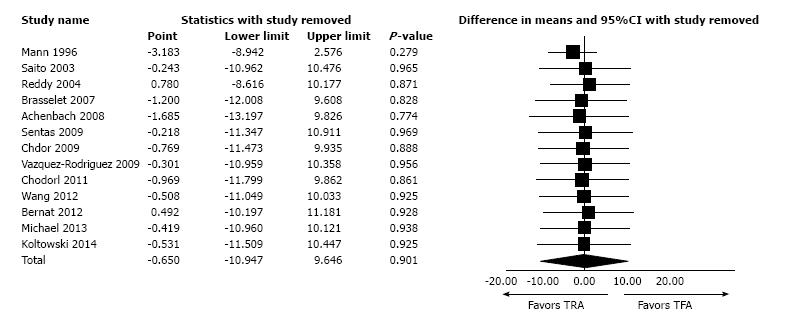
There was no difference in the amount of contrast used during either TRA or TFA (WMD = - 0.65 mL, 95%CI: -10.94 to 9.46 mL; P = 0.901; Figure 3). We found significant between-trial heterogeneity (Q = 260.8, df = 12; P < 0.001; I2 = 95.4). However, during sensitivity analysis, removal of any single study did not affect summary results (Figure 4).
In this study, we compared a broad spectrum of 3165 patients enrolled in 13 RCTs in terms of the contrast volume used during TRA or TFA during PCI. Overall, there was no difference in contrast volume use between the two access strategies. However, most trials were single-centered, and the majority of procedures were performed by radial experts.
Acute kidney injury (AKI) is a well-recognized complication of PCI that is associated with greater risk of in-hospital mortality and poor long-term outcomes[21]. The two major causes of post-PCI AKI are contrast-induced nephropathy (CIN) and renal atheroembolus[22,23]. The reported incidence of CIN post-PCI varies widely depending on numerous clinical, demographic, and procedural factors[22]. Among these, contrast volume is a well-established, dose-dependent, and potentially modifiable risk factor for CIN[22]. Although there have been reports of greater contrast use with TRA and concerns about possible subsequent CIN from this more extensive dye load[2,7,24], our meta-analysis shows that the volume of contrast used is not higher among patients undergoing PCI with TRA compared to TFA.
In contrast, a report from the British Columbia Cardiac and Renal Registries that included 69214 patients after coronary catheterization and PCI showed that chronic kidney disease (CKD) onset within 6 mo was significantly lower with TRA compared to TFA (0.5% vs 2.2%, P < 0.001) even after adjusting for baseline variables[9]. Similarly, another propensity-matched study showed that TRA, compared to TFA, was associated with a lower risk of AKI[25]. Finally, a recent meta-analysis of observational studies (adjusted by propensity score matching) showed that TRA, compared to TFA, was associated with lower risk of AKI[26]. The primary mechanism by which TRA was associated with a lower risk of kidney injury is thought to be through a reduced likelihood of renal atheroembolization because it offers the additional advantage of avoiding passage through potential atheromatous aortae and renal vessels[9,23]. The other mechanism by which TRA leads to less kidney injury is through a reduced risk of bleeding and the subsequent need for a blood transfusion. Post procedure bleeding and blood transfusion are independently associated with the development of AKI[27,28].
The potential benefits of TRA in CRD patients is in paradox to the CathPCI registry data, which show a slow adaption of TRA-PCI in patients with lower GFRs compared to patients with higher GFRs[6]. It is not clear if this is a result of misconceptions about potential increases in contrast use with radial access[24] or due to pressure from nephrologists who routinely recommend against using TRA in patient with CKD[29]. Even the Fistula First Initiative Coalition, sponsored by the Centers for Medicare and Medicaid Services, discourages use of the radial artery for access of the arterial vasculature in patients at risk for, or with known Stage 4 or 5 CKD[30]. This needs further investigation to assure we are not withholding beneficial intervention in these patient populations because of the theoretical possibility that dialysis access will be lost in the future.
This meta-analysis has several limitations. First, as with all meta-analyses, it is subject to various biases because data were combined from many studies with varying protocols. Second, most of the studies were single-centered, and the majority of procedures were performed by radial experts. Furthermore, in a majority of the trials, patients with coronary artery bypass grafts (CABG) were excluded. Therefore, the generalizability of this study may be limited, particularly to operators less-skilled in radial access and to patients with CABG. Finally, apart from the AKI-MATRIX sub-study, none of the randomized studies comparing TRA and TFA has ever systematically explored the issue of renal complications[31]. Therefore, we were not able perform the meta-analysis using AKI as one of the outcomes.
In conclusion, this meta-analysis of RCTs showed that in patients undergoing PCI, the amount of contrast volume used was not different between the TRA and TFA arms.
Trans-radial access (TRA) for percutaneous coronary interventions (PCIs) results in lower bleeding and vascular complications than trans-femoral access (TFA). A recent :randomizedcontrolledtrial (RCT) and several updated meta-analyses of RCTs have also shown that TRA also improves mortality compared to TFA in patients with acute coronary syndrome.
Despite the proven benefits of TRA for PCI, its adaptation for patients with chronic kidney disease has been slow because of concern about contrast-induced nephropathy from greater contrast use. Data from individual studies have been variable: Some show larger contrast volumes with TRA, but others show equal amounts of contrast use in both strategies.
In this study, the authors investigated the amounts of contrast used in TRA compared to TFA during PCI. This is the most comprehensive meta-analysis of RCTs in this field.
This study shows that the amount of contrast used does not differ between TRA-PCI and TFA-PCI. Therefore, TRA-PCI should not be avoided in patients with chronic kidney disease solely because of concern for increased contrast use.
The authors investigated the dose of contrast volume in patients who underwent trans-radial percutaneous coronary intervention (PCI) or trans-femoral PCI, using the meta-analysis method. They showed no difference in contrast medium between the two arms. This meta-analysis seems to be interesting.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Rauch B, Soliman E, Teragawa H S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Khan SA, Harper Y, Slomka T, John LA, Bondy BR, Shah R. An updated comprehensive meta-analysis of randomized controlled trials comparing radial versus femoral access for percutaneous interventions in patient with acute coronary syndrome. J Am Coll Cardiol. 2016;67:89-89. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Jaffe R, Hong T, Sharieff W, Chisholm RJ, Kutryk MJ, Charron T, Cheema AN. Comparison of radial versus femoral approach for percutaneous coronary interventions in octogenarians. Catheter Cardiovasc Interv. 2007;69:815-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Bernat I, Horak D, Stasek J, Mates M, Pesek J, Ostadal P, Hrabos V, Dusek J, Koza J, Sembera Z. ST-segment elevation myocardial infarction treated by radial or femoral approach in a multicenter randomized clinical trial: the STEMI-RADIAL trial. J Am Coll Cardiol. 2014;63:964-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 279] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 4. | Brasselet C, Tassan S, Nazeyrollas P, Hamon M, Metz D. Randomised comparison of femoral versus radial approach for percutaneous coronary intervention using abciximab in acute myocardial infarction: results of the FARMI trial. Heart. 2007;93:1556-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 99] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Achenbach S, Ropers D, Kallert L, Turan N, Krähner R, Wolf T, Garlichs C, Flachskampf F, Daniel WG, Ludwig J. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv. 2008;72:629-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 96] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Feldman DN, Swaminathan RV, Kaltenbach LA, Baklanov DV, Kim LK, Wong SC, Minutello RM, Messenger JC, Moussa I, Garratt KN. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: an updated report from the national cardiovascular data registry (2007-2012). Circulation. 2013;127:2295-2306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 390] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 7. | Michael TT, Alomar M, Papayannis A, Mogabgab O, Patel VG, Rangan BV, Luna M, Hastings JL, Grodin J, Abdullah S. A randomized comparison of the transradial and transfemoral approaches for coronary artery bypass graft angiography and intervention: the RADIAL-CABG Trial (RADIAL Versus Femoral Access for Coronary Artery Bypass Graft Angiography and Intervention). JACC Cardiovasc Interv. 2013;6:1138-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 93] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Cantor WJ, Puley G, Natarajan MK, Dzavik V, Madan M, Fry A, Kim HH, Velianou JL, Pirani N, Strauss BH. Radial versus femoral access for emergent percutaneous coronary intervention with adjunct glycoprotein IIb/IIIa inhibition in acute myocardial infarction--the RADIAL-AMI pilot randomized trial. Am Heart J. 2005;150:543-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 124] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Vuurmans T, Byrne J, Fretz E, Janssen C, Hilton JD, Klinke WP, Djurdjev O, Levin A. Chronic kidney injury in patients after cardiac catheterisation or percutaneous coronary intervention: a comparison of radial and femoral approaches (from the British Columbia Cardiac and Renal Registries). Heart. 2010;96:1538-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15040] [Cited by in RCA: 15872] [Article Influence: 1587.2] [Reference Citation Analysis (1)] |
| 11. | Kołtowski L, Filipiak KJ, Kochman J, Pietrasik A, Rdzanek A, Huczek Z, Scibisz A, Mazurek T, Opolski G. Access for percutaneous coronary intervention in ST segment elevation myocardial infarction: radial vs. femoral--a prospective, randomised clinical trial (OCEAN RACE). Kardiol Pol. 2014;72:604-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46497] [Article Influence: 2113.5] [Reference Citation Analysis (3)] |
| 13. | Mann JT, Cubeddu MG, Schneider JE, Arrowood M. Right Radial Access for PTCA: A Prospective Study Demonstrates Reduced Complications and Hospital Charges. J Invasive Cardiol. 1996;8 Suppl D:40D-44D. [PubMed] |
| 14. | Saito S, Tanaka S, Hiroe Y, Miyashita Y, Takahashi S, Tanaka K, Satake S. Comparative study on transradial approach vs. transfemoral approach in primary stent implantation for patients with acute myocardial infarction: results of the test for myocardial infarction by prospective unicenter randomization for access sites (TEMPURA) trial. Catheter Cardiovasc Interv. 2003;59:26-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 109] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Reddy BK, Brewster PS, Walsh T, Burket MW, Thomas WJ, Cooper CJ. Randomized comparison of rapid ambulation using radial, 4 French femoral access, or femoral access with AngioSeal closure. Catheter Cardiovasc Interv. 2004;62:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Santas E, Bodí V, Sanchis J, Núñez J, Mainar L, Miñana G, Chorro FJ, Llácer A. The left radial approach in daily practice. A randomized study comparing femoral and right and left radial approaches. Rev Esp Cardiol. 2009;62:482-490. [PubMed] |
| 17. | Chodór P, Krupa H, Kurek T, Sokal A, Swierad M, Was T, Streb W, Duszańska A, Swiatkowski A, Honisz G. RADIal versus femoral approach for percutaneous coronary interventions in patients with Acute Myocardial Infarction (RADIAMI): A prospective, randomized, single-center clinical trial. Cardiol J. 2009;16:332-340. [PubMed] |
| 18. | Vazquez-Rodriguez JM. Comparación del acceso radial frente al acceso femoral en la revascularización percutánea durante la fase aguda del infarto agudo de miocardio con elevación del segmento st. A coruña, spain: Universidade da coruña [doctoral thesis] 2009; Available from: https://www.researchgate.net/profile/Jose_Vazquez_Rodriguez/publication/275336415_TESIS-JMVR/links/55381ca90cf226723ab6161b.pdf. |
| 19. | Chodór P, Kurek T, Kowalczuk A, Świerad M, Wąs T, Honisz G, Świątkowski A, Streb W, Kalarus Z. Radial vs femoral approach with StarClose clip placement for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction. RADIAMI II: a prospective, randomised, single centre trial. Kardiol Pol. 2011;69:763-771. [PubMed] |
| 20. | Wang YB, Fu XH, Wang XC, Gu XS, Zhao YJ, Hao GZ, Jiang YF, Li SQ, Wu WL, Fan WZ. Randomized comparison of radial versus femoral approach for patients with STEMI undergoing early PCI following intravenous thrombolysis. J Invasive Cardiol. 2012;24:412-416. [PubMed] |
| 21. | Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, Singh M, Bell MR, Barsness GW, Mathew V. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259-2264. [PubMed] |
| 22. | Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 690] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 23. | Karalis DG, Quinn V, Victor MF, Ross JJ, Polansky M, Spratt KA, Chandrasekaran K. Risk of catheter-related emboli in patients with atherosclerotic debris in the thoracic aorta. Am Heart J. 1996;131:1149-1155. [PubMed] |
| 24. | Rao SV, Turi ZG, Wong SC, Brener SJ, Stone GW. Radial versus femoral access. J Am Coll Cardiol. 2013;62:S11-S20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Kooiman J, Seth M, Dixon S, Wohns D, LaLonde T, Rao SV, Gurm HS. Risk of acute kidney injury after percutaneous coronary interventions using radial versus femoral vascular access: insights from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium. Circ Cardiovasc Interv. 2014;7:190-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 26. | Andò G, Costa F, Boretti I, Trio O, Valgimigli M. Benefit of radial approach in reducing the incidence of acute kidney injury after percutaneous coronary intervention: a meta-analysis of 22,108 patients. Int J Cardiol. 2015;179:309-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 27. | Ohno Y, Maekawa Y, Miyata H, Inoue S, Ishikawa S, Sueyoshi K, Noma S, Kawamura A, Kohsaka S, Fukuda K. Impact of periprocedural bleeding on incidence of contrast-induced acute kidney injury in patients treated with percutaneous coronary intervention. J Am Coll Cardiol. 2013;62:1260-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 28. | Roy P, Raya V, Okabe T, Pinto Slottow TL, Steinberg DH, Smith K, Xue Z, Satler LF, Kent KM, Suddath WO. Incidence, predictors, and outcomes of post-percutaneous coronary intervention nephropathy in patients with diabetes mellitus and normal baseline serum creatinine levels. Am J Cardiol. 2008;101:1544-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Kern M. Should you do a radial artery cath in patients needing cabg or dialysis. Cath lab digest. 2012;20 Available from: http://www.Cathlabdigest.Com/articles/should-you-do-radial-artery-cath-patients-needing-cabg-or-dialysis. |
| 30. | Fistula first breakthrough initiative coalition. Breakthrough initiative - national coalition recommendations for the avoidance of radial artery access for procedures. Available from: http://esrdncc.Org/wp-content/uploads/2014/06/recommendation-to-avoid-radial-artery-use-in-ckd-45-esrd_10-31-11.pdf. |
| 31. | Valgimigli M, Calabrò P, Cortese B, Frigoli E, Garducci S, Rubartelli P, Andò G, Santarelli A, Galli M, Garbo R. Scientific foundation and possible implications for practice of the Minimizing Adverse Haemorrhagic Events by Transradial Access Site andSystemic Implementation of AngioX (MATRIX) trial. J Cardiovasc Transl Res. 2014;7:101-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |