Published online Apr 26, 2017. doi: 10.4330/wjc.v9.i4.371
Peer-review started: January 10, 2017
First decision: February 17, 2017
Revised: February 28, 2017
Accepted: March 12, 2017
Article in press: March 13, 2017
Published online: April 26, 2017
Processing time: 111 Days and 12.4 Hours
To assess the association of inter-ethnic vs intra-ethnic marriage with severity of coronary artery disease (CAD) in men undergoing angiography.
We conducted a prospective multicenter, multi-ethnic, cross sectional observational study at five hospitals in Saudi Arabia and the United Arab Emirates, in which we used logistic regression analysis with and without adjustment for baseline differences.
Data were collected for 1068 enrolled patients undergoing coronary angiography for clinical indications during the period of April 1st, 2013 to March 30th, 2014. Ethnicities of spouses were available only for male patients. Of those enrolled, 687 were married men and constituted the cohort for the present analysis. Intra-ethnic marriages were reported in 70% and inter-ethnic marriages in 30%. After adjusting for baseline differences, inter-ethnic marriage was associated with lower odds of having significant CAD [adjusted odds ratio 0.52 (95%CI: 0.33, 0.81)] or multi-vessel disease (MVD) [adjusted odds ratio 0.57 (95%CI: 0.37, 0.86)]. The adjusted association with left main disease showed a similar trend, but was not statistically significant [adjusted odds ratio 0.74 (95%CI: 0.41, 1.32)]. The association between inter-ethnic marriage and the presence of significant CAD and MVD was not modified by number of concurrent wives (P interaction > 0.05 for both).
Among married men undergoing coronary angiography, inter-ethnic, as compared to intra-ethnic, marriage is associated with lower odds of significant CAD and MVD.
Core tip: One thousand and sixty-eight enrolled patients underwent coronary angiography for clinical indications. Ethnicities of spouses were available for only male patients. Of the 771 males, 687 were married. Seventy percent of them were in intra-ethnic marriages and 30% in inter-ethnic marriages. After adjusting for baseline differences, inter-ethnic marriage was associated with lower odds of having significant coronary artery disease (CAD) or multi-vessel disease (MVD). The adjusted association with left main disease showed a similar trend, but was not statistically significant. The association between inter-ethnic marriage and the presence of significant CAD and MVD was not modified by number of concurrent wives.
- Citation: Daoulah A, Al-kaabi S, Lotfi A, Al-Murayeh M, Nasseri SA, Ahmed W, Al-Otaibi SN, Alama MN, Elkhateeb OE, Plotkin AJ, Malak MM, Alshali K, Hamzi M, Al Khunein S, Abufayyah M, Alsheikh-Ali AA. Inter-ethnic marriages and severity of coronary artery disease: A multicenter study of Arabian Gulf States. World J Cardiol 2017; 9(4): 371-377
- URL: https://www.wjgnet.com/1949-8462/full/v9/i4/371.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i4.371
Coronary artery disease (CAD) is a major cause of death throughout the world. The high prevalence and mortality have led to great importance in understanding the risk factors associated with CAD[1-3]. Traditional risk factors comprise the majority of the increase for cardiovascular events[4]. Additional factors such as physiological, psychological, emotional, social, and stress, both acute and chronic, have been studied[5-23]. The interactions between risk factors also have great consequences[24]. Studies investigating the association between marital status and CAD have predominantly been performed in developed countries, and none examined the role of spousal ethnicities and CAD[25-32]. Selecting a spouse is often influenced by social norms, and cultural practices typically prefer marriages between persons of the same ethnic background. However, inter-ethnic marriages are increasingly common as societal attitudes and demographic patterns change. Studies from Western societies demonstrated that such marriages are associated with increased stress and lower relationship quality[33‒35]. Due to these findings, we examined the relationship between inter-ethnic marriages and severity of CAD in two Gulf States.
The details regarding the design, methods, and endpoints of this multicenter, observational study came from the Polygamy and Risk of Coronary Artery Disease in Men Undergoing Angiography[36]. In the current study the data were collected prospectively from five hospitals in two Gulf Regions (the Kingdom of Saudi Arabia and the United Arab Emirates), during the period of April 1st, 2013 to March 30th, 2014. The study was approved by King Faisal Specialist Hospital and Research Center Institutional Review Board, and an invitation letter was given to all participants who affirmed verbal consent prior to their enrollment. For each patient undergoing coronary angiography for clinical indication, two separate data forms, one general and one angiographic, were filled out by the research assistant and assigned cardiologist, respectively. Both forms were completed before the patients were discharged from hospital. All data forms were reviewed by the assigned cardiologist then sent online to the principle investigator, who also checked the forms prior to submission for analysis. All patients undergoing coronary angiography were recruited for the study. There was no exclusion criteria.
Demographic data: Age, ethnic background; Physiologic status: Hypertension, diabetes, dyslipidemia, BMI; Life style: Smoking history; Past medical history: CAD, percutaneous coronary intervention, coronary artery bypass surgery, cerebral vascular disease, peripheral arterial disease, congestive heart failure, atrial fibrillation, chronic kidney disease. Socioeconomic data: Occupation (unemployed, private sector, government sector, self-employed), living in rural or urban area, highest level of education completed (illiterate, secondary school, university, masters, PhD), monthly income (< 1300, 1300 to 2600, 2600 to 5300, 5300 to 7900, 7900 to 10600, > 10600 USD); Number of wives: Single or multiple concurrent wives; Ethnicity of spouse (Arabic Gulf region, Arabs non-Gulf region, non-Arabic).
Reason for coronary angiography: Elective or urgent/emergent; Number of vessels involved (severity); Treatment: Medical or revascularization.
Significant CAD was defined as ≥ 70% luminal stenosis in a major epicardial vessel or ≥ 50% stenosis in the left main coronary artery. Multi-vessel disease (MVD) was defined as having more than one significant CAD; Inter-ethnic marriage was defined as Arab men from the Gulf region marrying Arab women from a non-Gulf region or non-Arab women; Intra-ethnic marriage was defined as Arab men from the Gulf region marrying Arab women from the same region.
Standard summary statistics were used to describe the cohort. Continuous variables are presented as mean ± SD and were compared across multiple groups using the analysis of variance test. Categorical variables are presented as percentages and compared using the χ2 test. The associations between inter-ethnic or intra-ethnic marriage and CAD, MVD and left main disease (LMD) were assessed using logistic regression models and quantified with odds ratios. Adjusted regression models included the following explanatory variables: Age, community setting (urban vs rural), employment, income level, education level, number of concurrent wives, and additional variables that differed by ethnicity of spouse in univariate comparisons (P < 0.1). All statistical tests were two-tailed and significance was defined as P < 0.05. No adjustments for multiple comparisons were made.
A detailed description can be found in Polygamy and Risk of Coronary Artery Disease in Men Undergoing Angiography[36].
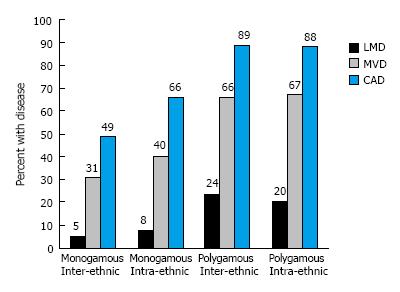
We enrolled 1068 patients in the current study. Ethnicities of spouses were available for only male patients, so the analysis excludes female patients. Of the 771 males, 685 were married; however, spouse ethnicity was not available for two of these men. Married men were categorized according to number of wives: The majority had one wife (68%), while some had a history of two wives (19%), three wives (10%) or four wives (3%). Most were in intra-ethnic marriages 481 (70%), as opposed to inter-ethnic marriages 204 (30%), Table 1. The majority of inter-ethnic marriages were between Gulf nationals and non-Gulf Arab women (65%). Men in inter-ethnic marriages were more likely to have a history of hypertension and CABG, to live in rural communities, and to be in polygamous marriages. In univariate analyses, there was a significant association between inter-ethnic marriage and presence of LMD therefore the rate of CABG was higher in these subjects when compared with those in intra-ethnic marriages, who had undergone more PCI (Table 1). In multivariate logistic regressions adjusting for baseline differences, inter-ethnic marriage was associated with lower odds of having significant CAD [adjusted odds ratio 0.52 (95%CI: 0.33, 0.81)] or MVD [adjusted odds ratio 0.57 (95%CI: 0.37, 0.86)]. The adjusted association with LMD showed a similar trend, but was not statistically significant [adjusted odds ratio 0.74 (95%CI: 0.41, 1.32)] (Figure 1). The association between inter-ethnic marriage and the presence of significant CAD or MVD was not modified by number of concurrent wives (P interaction > 0.05 for both) (Figure 2).
| All (n = 685) | Intra-ethnic (n = 481) | Inter-ethnic (n = 204) | P value | |
| Age (yr) | 59 ± 12 | 58 ± 13 | 60 ± 12 | 0.0879 |
| BMI (kg/m²) | 28 ± 6 | 28 ± 6 | 27 ± 5 | 0.4009 |
| Rural, n (%) | 27 | 25 | 34 | 0.0148 |
| DM, n (%) | 56 | 57 | 54 | 0.5226 |
| Hypertension, n (%) | 57 | 54 | 64 | 0.0209 |
| Smoking, n (%) | 54 | 53 | 57 | 0.1428 |
| Dyslipidemia, n (%) | 66 | 65 | 68 | 0.4734 |
| Past history, n (%) | ||||
| CAD | 45 | 45 | 45 | 0.9468 |
| PCI | 24 | 23 | 26 | 0.3263 |
| CABG | 6 | 5 | 9 | 0.0329 |
| Atrial fibrillation | 5 | 4 | 5 | 0.3990 |
| CHF | 13 | 13 | 11 | 0.5102 |
| CVA | 4 | 4 | 5 | 0.4388 |
| CKD | 14 | 14 | 13 | 0.7020 |
| Depression | 8 | 8 | 8 | 0.8363 |
| PAD | 2 | 2 | 3 | 0.1453 |
| Ethnicity, n (%) | 0.3597 | |||
| Arabic gulf region | 87 | 87 | 88 | |
| Arabic non-gulf | 6 | 7 | 4 | |
| Non Arabic | 7 | 6 | 8 | |
| No. of wives, n (%) | < 0.0001 | |||
| 1 | 68 | 81 | 38 | |
| 2 | 19 | 13 | 32 | |
| 3 | 10 | 5 | 22 | |
| 4 | 3 | 1 | 8 | |
| Monthly income, n (%) | 0.1760 | |||
| $ < 1300 | 50 | 50 | 52 | |
| $ 1300-2600 | 29 | 30 | 27 | |
| $ 2600-5300 | 13 | 14 | 10 | |
| $ 5300 to 7900 | 4 | 4 | 5 | |
| $ 7900 to 10600 | 2 | 1 | 3 | |
| $ > 10600 | 2 | 1 | 3 | |
| Job category, n (%) | 0.6824 | |||
| Jobless | 21 | 21 | 23 | |
| Private sector | 18 | 18 | 16 | |
| Government sector | 43 | 42 | 45 | |
| Self employs | 18 | 19 | 16 | |
| Education level, n (%) | 0.0403 | |||
| Illiterate | 42 | 42 | 40 | |
| Secondary school | 38 | 37 | 40 | |
| Post graduate | 16 | 18 | 12 | |
| Master | 3 | 2 | 7 | |
| PhD | 1 | 1 | 1 | |
| Indication for CAG, n (%) | 0.1483 | |||
| Elective | 48 | 48 | 47 | |
| NSTEACS | 46 | 44 | 50 | |
| STEMI | 6 | 8 | 3 | |
| Findings on CAG, n (%) | < 0.001 | |||
| No CAD | 28 | 29 | 27 | |
| Single vessel | 24 | 25 | 21 | |
| Double vessel | 26 | 29 | 19 | |
| Triple vessel | 22 | 17 | 34 | |
| Multi-vessel | 48 | 46 | 53 | 0.1020 |
| Left main | 12 | 10 | 17 | 0.0175 |
| Intervention, n (%) | < 0.0001 | |||
| Medical therapy | 36 | 33 | 43 | |
| PCI | 47 | 54 | 31 | |
| CABG | 17 | 13 | 26 |
Previous literature from non-Gulf regions demonstrated that inter-ethnic marriages were found to have lower income and education level and poor level of family acceptance and support when compared to intra-ethnic marriages. In addition, inter-ethnic couples reported lower relationship satisfaction, and increased conflict within the relationship over such issues as money and spending time together. These factors are associated with increased stress and lower relationship quality[33-35]. Furthermore, it is known that acute and chronic stress is associated with the development of CAD[17,18]. However, the impact of inter-ethnic marriage on the severity of CAD is unknown. Our study is the first to analyze the association between inter-ethnic vs intra-ethnic marriage and severity of CAD among men using coronary angiography, the gold standard for identifying CAD. After adjusting for baseline characteristics, we observed that inter-ethnic marriage was associated with lower odds of having significant CAD or MVD. The adjusted association with LMD showed a similar trend, but was not statistically significant. Studies from western societies reported an increase in stress within inter-ethnic marriages; however, our study found lower odds of CAD in inter-ethnic vs intra-ethnic marriage, which may suggest lower levels of stress in these marriages. A number of factors may contribute to our results. First, in the current study, 80% of the patients reported income levels of 32000 USD or less annually. Although there is family and societal pressure to marry within the same region, the overall cost of getting married and maintaining the relationship within the Gulf region is high, which may impact men from this region leading them to select a spouse from elsewhere. The high cost of marriage in the Gulf is associated with complex family interactions, which possibly creates unrealistic expectations when anticipating a marital lifestyle. This may be a source of significant stress in and of itself. Second, almost 80% of the patients in our study had low level of education. In the Gulf region, there are increased opportunities for educated men to marry, which may necessitate less educated men to select a spouse from outside the region. Additionally, the conservative social and cultural practices in the Gulf region may play a role in stress levels when compared to non-Gulf regions. Men from Gulf region who marry women from outside the region may be more health conscious than men who marry women from inside the Gulf. Classically, women from the Gulf region tend to prepare dishes rich in fat, which are atherogenic, whereas wives from elsewhere may favor dishes that are more healthy, notably those from the Arab Mediterranean region[37-39]. Non-Gulf wives may encourage their husbands to be healthy and maintain fitness, as their literacy and health awareness may be superior to that of Gulf-native women.
This study is the first to look at the association between inter-ethnic vs intra-ethnic marriages and severity of CAD using coronary angiography in men from Arabian Gulf States.
The study provides additional knowledge on the risks associated with inter-ethnic vs intra-ethnic marriages. This information will be useful for personalizing care and preventing CAD. Not only will it provide patients information concerning social risk factors, it will also help providers identify and treat adults who are at increased risk of CAD. Further studies are required to confirm our findings and to investigate the mechanism underlying these findings in order to identify possible interventions to reduce these risks. In future studies, assessment of the local culture, social and medical practices, and attitudes toward inter-ethnic marriage should be performed.
Limitations of the study include a small sample size and the lack of documentation of the length of marriages prior to cardiac catheterization; this interval may influence the findings. Our study population was selected to undergo coronary angiography if clinically indicated, and as such, cannot be generalized to all married men in the Gulf region. Additionally, 42% of the patients were illiterate and 80% reported income levels of 32000 USD or less annually; indicating that the results may not be applicable to those with higher incomes or higher levels of education. We did not look at unmeasured confounding variables such as dietary habits, physical activity, inflammatory or stress markers, or additional variables that may have played a role.
We would like to sincerely thank all patients who agreed to participate in this study.
Selecting a spouse is often influenced by social norms, and societies typically prefer marriages of the same ethnic background. However, inter-ethnic marriages are increasingly common as societal attitudes and demographic patterns change. Studies from Western societies have demonstrated that inter-ethnic marriages are associated with increased stress and lower relationship quality. The majority of these studies examine the association between marital status and coronary artery disease (CAD), but none have examined the role of spousal ethnicity and CAD.
It is unknown whether such marriages have an impact on the severity of CAD.
This study is the first to look at the association between inter-ethnic vs intra-ethnic marriages and severity of CAD using coronary angiography in men from Arabian Gulf States.
The data in this study suggest that among married men undergoing coronary angiography, inter-ethnic marriage is associated with lower odds of significant CAD and multi-vessel disease (MVD). Further studies are required to confirm these findings and to investigate the mechanism underlying these findings in order to identify possible interventions to reduce these risks. In future studies, assessment of the local culture, social and medical practices, and attitudes toward inter-ethnic marriage should be performed.
Significant coronary artery disease (CAD) was defined as ≥ 70% luminal stenosis in a major epicardial vessel or ≥ 50% stenosis in the left main coronary artery. MVD was defined as having more than one significant CAD. Inter-ethnic marriage was defined as Arab men from the Gulf region marrying Arab women from a non-Gulf region or non-Arab women. Intra-ethnic marriage was defined as Arab men from the Gulf region marrying Arab women from the same region.
The data is interesting.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Kingdom of Saudi Arabia
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Beeres M, Schoenhagen P S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Heron M. Deaths: Leading Causes for 2012. Natl Vital Stat Rep. 2015;64:1-93. [PubMed] |
| 2. | Jacobs-Wingo JL, Espey DK, Groom AV, Phillips LE, Haverkamp DS, Stanley SL. Causes and Disparities in Death Rates Among Urban American Indian and Alaska Native Populations, 1999-2009. Am J Public Health. 2016;106:906-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3462] [Cited by in RCA: 4532] [Article Influence: 412.0] [Reference Citation Analysis (1)] |
| 4. | Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7301] [Cited by in RCA: 7422] [Article Influence: 353.4] [Reference Citation Analysis (1)] |
| 5. | Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318:1460-1467. [PubMed] [DOI] [Full Text] |
| 6. | Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192-2217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1663] [Cited by in RCA: 1564] [Article Influence: 60.2] [Reference Citation Analysis (0)] |
| 7. | Krantz DS, Sheps DS, Carney RM, Natelson BH. Effects of mental stress in patients with coronary artery disease: evidence and clinical implications. JAMA. 2000;283:1800-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 83] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Krantz DS, McCeney MK. Effects of psychological and social factors on organic disease: a critical assessment of research on coronary heart disease. Annu Rev Psychol. 2002;53:341-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 245] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 9. | Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am J Prev Med. 2003;24:113-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 365] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 10. | Strike PC, Steptoe A. Psychosocial factors in the development of coronary artery disease. Prog Cardiovasc Dis. 2004;46:337-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 209] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Kuper H, Marmot M, Hemingway H. Systematic review of prospective cohort studies of psychosocial factors in the etiology and prognosis of coronary heart disease. Semin Vasc Med. 2002;2:267-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 230] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Kubzansky LD, Davidson KW, Rozanski A. The clinical impact of negative psychological states: expanding the spectrum of risk for coronary artery disease. Psychosom Med. 2005;67 Suppl 1:S10-S14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 819] [Cited by in RCA: 802] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 14. | Holmes SD, Krantz DS, Rogers H, Gottdiener J, Contrada RJ. Mental stress and coronary artery disease: a multidisciplinary guide. Prog Cardiovasc Dis. 2006;49:106-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Bhattacharyya MR, Steptoe A. Emotional triggers of acute coronary syndromes: strength of evidence, biological processes, and clinical implications. Prog Cardiovasc Dis. 2007;49:353-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 83] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Davidson KW. Emotional predictors and behavioral triggers of acute coronary syndrome. Cleve Clin J Med. 2008;75 Suppl 2:S15-S19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9:360-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 661] [Cited by in RCA: 794] [Article Influence: 61.1] [Reference Citation Analysis (0)] |
| 18. | Orth-Gomér K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman MA. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA. 2000;284:3008-3014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 380] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 19. | Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51:1237-1246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 797] [Cited by in RCA: 660] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 20. | Phillips JE, Klein WM. Socioeconomic Status and Coronary Heart Disease Risk: The Role of Social Cognitive Factors. Soc Personal Psychol Compass. 2010;4:704-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Bajekal M, Scholes S, Love H, Hawkins N, O’Flaherty M, Raine R, Capewell S. Analysing recent socioeconomic trends in coronary heart disease mortality in England, 2000-2007: a population modelling study. PLoS Med. 2012;9:e1001237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 22. | Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380:1491-1497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 649] [Cited by in RCA: 609] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 23. | Franks P, Winters PC, Tancredi DJ, Fiscella KA. Do changes in traditional coronary heart disease risk factors over time explain the association between socio-economic status and coronary heart disease? BMC Cardiovasc Disord. 2011;11:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 24. | Kivimäki M, Nyberg ST, Fransson EI, Heikkilä K, Alfredsson L, Casini A, Clays E, De Bacquer D, Dragano N, Ferrie JE. Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ. 2013;185:763-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 25. | Farr W. The influence of marriage on the mortality of the French people. In: Hastings GW, ed. Transactions of the National Association for the Promotion of Social Science 1858. London: John W. Parker & Sons, 1858: 504-513. |
| 26. | March L. Some researches concerning the factors of mortality. J Roy Stat Soc. 1912;75:505-538. [RCA] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Ben-Shlomo Y, Smith GD, Shipley M, Marmot MG. Magnitude and causes of mortality differences between married and unmarried men. J Epidemiol Community Health. 1993;47:200-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 156] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 28. | Bureau of the Census. Mortality by marital status, by age race and sex, urban and rural, United States, 1940. Vital Rep. 1945;23:43. |
| 29. | Venters M, Jacobs DR, Pirie P, Luepker RV, Folsom AR, Gillum RF. Marital status and cardiovascular risk: the Minnesota Heart Survey and the Minnesota Heart Health Program. Prev Med. 1986;15:591-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Molloy GJ, Stamatakis E, Randall G, Hamer M. Marital status, gender and cardiovascular mortality: behavioural, psychological distress and metabolic explanations. Soc Sci Med. 2009;69:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 146] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 31. | Blom M, Georgiades A, László KD, Alinaghizadeh H, Janszky I, Ahnve S. Work and marital status in relation to depressive symptoms and social support among women with coronary artery disease. J Womens Health (Larchmt). 2007;16:1305-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Lindegård B, Langman MJ. Marital state, alcohol consumption, and liability to myocardial infarction, stroke, diabetes mellitus, or hypertension in men from Gothenburg. Br Med J (Clin Res Ed). 1985;291:1529-1533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Bratter JL, Eschbach K. What about the couple? Interracial marriage and psychological distress. Social Science Research. 2006;35:1025-1047. [DOI] [Full Text] |
| 34. | Donovan S. Stress and coping techniques in successful intercultural marriages. USA: Virginia Polytechnic Institute and State University 2004; . |
| 35. | Hohmann-Marriott BE, Amato P. Relationship Quality in Interethnic Marriages and Cohabitations. Social Forces. 2008;87:825-855. [DOI] [Full Text] |
| 36. | Daoulah A, Lotfi A, Al-Murayeh M, Al-kaabi S, Al-Faifi SM, Elkhateeb OE, Alama MN, Hersi AS, Dixon CM, Ahmed W. Polygamy and Risk of Coronary Artery Disease in Men Undergoing Angiography: An Observational Study. International Journal of Vascular Medicine. 2017;2017:1925176. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Mayor S. Mediterranean diet reduces cardiovascular events in people with heart disease, study shows. BMJ. 2016;353:i2348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Stewart RA, Wallentin L, Benatar J, Danchin N, Hagström E, Held C, Husted S, Lonn E, Stebbins A, Chiswell K. Dietary patterns and the risk of major adverse cardiovascular events in a global study of high-risk patients with stable coronary heart disease. Eur Heart J. 2016;37:1993-2001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 39. | Grosso G, Marventano S, Yang J, Micek A, Pajak A, Scalfi L, Galvano F, Kales SN. A Comprehensive Meta-analysis on Evidence of Mediterranean Diet and Cardiovascular Disease: Are Individual Components Equal? Crit Rev Food Sci Nutr. 2015; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 312] [Article Influence: 44.6] [Reference Citation Analysis (0)] |