Published online Apr 26, 2017. doi: 10.4330/wjc.v9.i4.296
Peer-review started: January 28, 2016
First decision: March 23, 2016
Revised: February 24, 2017
Accepted: March 12, 2017
Article in press: March 13, 2017
Published online: April 26, 2017
Processing time: 456 Days and 2.1 Hours
The purpose of this paper is to summarize the need, feasibility, safety, legality, and ethical perspectives of pacemaker reutilization in low- and middle-income countries (LMICs). It will also describe, in-depth, Project My Heart Your Heart (PMHYH) as a model for pacemaker reuse in LMICs. The primary source of the discussion points in this paper is a collection of 14 publications produced by the research team at the University of Michigan and its collaborative partners. The need for pacemaker reutilization in LMICs is evident. Numerous studies show that the concept of pacemaker reutilization in LMICs is feasible. Infection and device malfunction are the main concerns in regard to pacemaker reutilization, yet many studies have shown that pacemaker reuse is not associated with increased infection risk or higher mortality compared with new device implantation. Under the right circumstances, the ethical and legal bases for pacemaker reutilization are supported. PMHYH is a proof of concept pacemaker donation initiative that has allowed funeral home and crematory directors to send explanted devices to an academic center for evaluation and re-sterilization before donation to underserved patients in LMICs. The time is now to pursue large-scale studies and trials of pacemaker reuse for the betterment of society. PMHYH is leading the way in the effort and is poised to conduct a prospective randomized, non-inferiority, multicenter study to confirm the clinical efficacy and safety of pacemaker reuse, for clinical and legal support.
Core tip: The purpose of this paper is to summarize the need, feasibility, safety, legality, and ethical perspectives of pacemaker reutilization in low- and middle-income countries (LMICs). It also illustrates Project My Heart Your Heart as a model for pacemaker reuse in LMICs. The primary source of the discussion points in this paper is a collection of 14 publications produced by experts at the University of Michigan and their collaborative partners.
- Citation: Runge MW, Baman TS, Davis S, Weatherwax K, Goldman E, Eagle KA, Crawford TC. Pacemaker recycling: A notion whose time has come. World J Cardiol 2017; 9(4): 296-303
- URL: https://www.wjgnet.com/1949-8462/full/v9/i4/296.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i4.296
The purpose of this paper is to summarize the need for, feasibility, safety, legality, and ethical perspectives of pacemaker reutilization in low- and middle-income countries (LMICs). It will also show Project My Heart Your Heart (PMHYH) as a model for pacemaker reuse in LMICs. The source of the discussion points in this paper is a collection of 14 publications[1-14] produced by experts at the University of Michigan and their collaborative partners.
Cardiovascular disease (CVD) comprises about 30% of all deaths in the world, more than any other singular disease or condition[15]. CVD causes twice as many deaths as the major contemporary infectious diseases-human immunodeficiency virus/acquired immune deficiency syndrome, malaria, and tuberculosis[16]. Major advances in the science of medicine, and a greater emphasis on primary prevention have improved the morbidity and mortality attributed to CVD in the industrialized world[17]. A similar improvement has not taken place in LMICs. Of the 17.5 million deaths worldwide in 2012, which were due to CVD, over 75% occurred in LMICs[15].
The disparity in CVD care between developed nations and LMICs is especially evident in the field of heart rhythm disorders. It is estimated that 1 million individuals die every year because they cannot access bradyarrhythmia therapy[18]. Pacemaker implantation, a common treatment for bradyarrhythmia, is strikingly uncommon where it is most needed - in LMICs. In 2005, 752 pacemakers were implanted per million individuals residing in the United States and an average of 475 per million were implanted in European countries[19]. In the same year there were only 22, 14, and 4 pacemaker implantations per million in Thailand, Peru, and Bangladesh, respectively[19]. This disparity remained unchanged in a 2009 survey showing that while 767 pacemakers were implanted per million individuals in the United States and 782 per million in France, only 30, 5, and 4 per million were placed in patients in Peru, Bangladesh, and Pakistan, respectively[20].
The World Bank defines LMICs as any nation, whose gross per capita national product is under United States $12736[21]. Thus, not surprisingly, a major hurdle for patients in LMICs in need of a pacemaker is its prohibitive cost. A pacemaker generally costs between $2500 and $3000, with leads priced as high as $800 and $1000[5]. Implantable cardioverter-defibrillator (ICD) generators, used to treat life threatening ventricular tachy-arrhythmias, may cost between $20000 and $40000, with leads priced sometimes over $10000[5]. It is often the case that the cost of a pacemaker or an ICD far exceeds the per capita annual economic output of individuals in LMICs[19].
Founded in 1984, Heartbeat International is a charity, which aims to distribute pacemakers and ICDs approaching the use-by-date to a dozen or more recipient implantation centers in LMICs. Device manufacturers such as Medtronic, St Jude Medical, Boston Scientific, and more recently BIOTRONIK have supported this work. Since its beginnings, Heartbeat International has distributed over 14000 near-expired devices to needy patients[18]. Nonetheless, this supply of near-expired devices cannot possibly satisfy the enormous unmet need for pacemakers and ICDs in LMICs.
In the developed world, pacemaker implantation commonly results from sinus node dysfunction[22]. In LMICs however, the most common reason patients undergo pacemaker implantation is complete heart block[23,24]. This difference is in part due to greater prevalence of infectious diseases in LMICs vs developed nations. Chagas disease, for example, is caused by an infection with Trypanosomiasis cruzi, and is particularly common in Latin America[25]. Seventy-two percent of pacemaker recipients in a Brazilian study by Oliveira et al[26] were seropositive for Trypanosomiasis cruzi. Also contributing to the great need in LMICs for cardiac implantable electronic devices - pacemakers and ICDs - is coronary artery disease, owing to increased tobacco use and an increased prevalence of hypertension and diabetes worldwide[14].
Pacemaker reuse is a feasible and efficacious method to reduce the health disparity between developed economies and LMICs. The concept of pacemaker reuse has been considered for decades. For example, in the early 1990s, 5% of pacemakers implanted in Sweden were reused devices[27]. However, as Sweden joined the European Union, this practice ended. Due to the high demand for devices in LMICs, lack of sufficient supply of expired devices, and financial constraints of LMIC citizens to afford new devices, pacemaker and ICD reutilization must be re-considered.
Postmortem pacemaker donation from the funeral industry is a potential source of devices harvested for the purpose of reutilization[1]. In the United States alone 225000 pacemakers are implanted each year[19]. And while in a recent pacemaker recipient registry the mean longevity of pacemakers was 11.2 ± 2.6 years, patients receiving the devices often do not live that long[28]. Brunner et al[29] found that only 66% of pacemaker recipients are still alive at 5 years after implantation.
According to funeral directors, 85% of the deceased with pacemakers and ICDs are buried with their device[8]. Of those devices removed prior to burial, some are donated to charity to be reused, though many, indeed the majority, are treated as waste or abandoned[30]. Pacemakers must be extracted before the deceased are cremated due to the risk of device explosion, and according to The Cremation Association of North America, the rate of cremation in the United States is projected to rise from 39% in 2010 to 59% in 2025[31]. The vast majority (over 90%) of patients with pacemakers, when surveyed, were positively inclined to advance directives to donate their devices postmortem to poor patients in LMICs[32].
In 2008, Detroit area funeral homes rendered 50 pacemakers to World Medical Relief[12]. Eighteen of these devices met the threshold of at least 70% of battery life remaining[12]. In a 2012 study, flyers were mailed to the Michigan Funeral Directors Association regarding device collection - and of the 3176 devices returned, 21% had acceptable battery life (≥ 75% or ≥ 4 years estimated longevity)[1]. Thus, funeral homes and crematories represent a useful source for pacemakers and ICDs with adequate battery life to be reused in LMICs.
An additional source of pacemakers for reutilization is devices explanted in hospitals due to changing clinical indications. A study at The University of Michigan found that 52% of pacemakers, 54% of ICDs, and 48% of cardiac resynchronization therapy defibrillators explanted for clinical indications, other than elective replacement indicator, had sufficient battery life (≥ 48 mo or > 75% battery life) and appeared to function well[11]. According to the National Cardiovascular Data Registry, between 2010 and 2012, over 63500 devices were explanted annually in the United States[11]. If the yield nationwide were similar to that of The University of Michigan, perhaps as many as 13000 pacemakers and ICDs with sufficient battery could be harvested from this pool each year for donation[11].
While supplying pacemakers from the funeral homes, crematories, and hospitals appears viable, obtaining leads from these sources is less so. Leads are generally not reusable for at least three reasons: (1) lead extraction would add a great deal of complexity to the donation process; (2) the integrity of most extracted leads would be inadequate for repurposing; and (3) cleaning and sterilization of the leads would be fraught with significant technical challenges[5]. Thus, a patient in a LMIC would either have to receive a donated new lead or purchase a new lead himself or herself. Both of these are plausible options, especially because the cost of the leads is much less than the pacemakers or defibrillators. This might be possible with charitable donations from companies[5]. Also, given that at government-run facilities in LMICs, patients would not be required to pay for the implantation procedure, if lead donations were to fall short of the demand, a patient and his or her family could potentially pool resources to pay for a new pacemaker or ICD lead. This is especially true given that manufacturers in India currently produce a low-cost lead priced near $200[3].
With regards to safety, there are two prime concerns that must be considered in regard to pacemaker and ICD reutilization: Infection and device malfunction. Adequate sterilization requires removal of all organic material. This task is made difficult by the composition and geometry of the epoxy header[5]. Nonetheless, several studies have shown that pacemaker reuse does not result in higher rates of infection or mortality when compared with new pacemaker surgery. Romero et al[33] described four trials enrolling a total of 603 subjects, in whom reuse did not result in greater infection risk. Similarly, Nava et al[34] reported comparable infection rates between new and refurbished pacemakers. Panja et al[35] found comparable mortality and infection rates for new and used pacemakers. In a meta-analysis of studies with hard outcomes of pacemaker reuse[4], pooled patient data (n = 2270) from 18 trials indicated that there was no significant difference in infection rate between new and reused pacemakers. This analysis did find that in 0.68% of cases, device malfunction became apparent at the time of pacemaker surgery or shortly thereafter, which admittedly is far higher than the risk of malfunction for a new pacemaker. While the studies comprised in the analysis were heterogeneous, and some important information may not have been universally reported, none of the papers indicated that the malfunction lead to patient death.
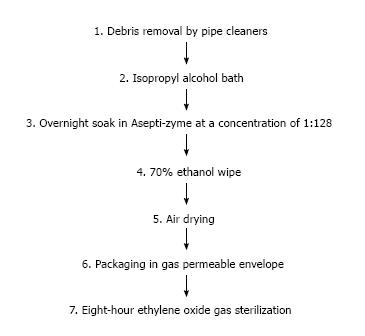
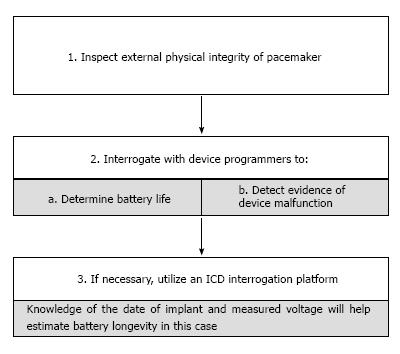
To minimize the risk of infection and device malfunction, comprehensive protocols for device cleaning, sterilization, and functionality testing must be developed. One such sterilization process, used successfully for pacemaker reutilization in previous studies[36,37], is shown in Figure 1. Key areas of any proposed cleaning protocol must be the treatment of set-screws and header connections[6]. In prior reports, set-screw abnormalities developed during extraction led to most malfunctions in refurbished devices[8,34]. The complex process of device handling at the funeral home and shipment to a collection center exposes the pacemakers to an additional risk of damage, which may not be grossly evident. Thus it is imperative to assess the major pacemaker functions, so that no patient experiences critical device failure[30]. Aspects of proper pacemaker interrogation are shown in Figure 2.
Anecdotal evidence of safety in pacemaker reutilization is strong. Twelve of the 50 devices donated to World Medical Relief from Detroit Metropolitan funeral homes, mentioned above, were offered to impoverished patients at the Philippine General Hospital (PGH) in Manila. The patients were screened by the local social services, which determined that these individuals were not in a position to pay the local market price for the pacemaker. There were no acute complications at the time of implantation, and a 2-mo follow-up showed that none of the pacemakers malfunctioned or became infected.
One powerful example of successful pacemaker reutilization is a patient at PGH. In a 2010 publication, Romero et al[2] detailed implantation of a pacemaker, which had been procured post-mortem, into a 65-year-old Filipino woman. This woman, a widow with two adult children, experienced third-degree heart block and was recommended to have a temporary pacemaker but ultimately refused a permanent pacemaker implantation due to lack of financial resources. She requested to be discharged, but returned one week later to the hospital with another syncopal episode. With her family unable to afford a new pacemaker, World Medical Relief donated a pacemaker obtained post-mortem with battery life of about 85%, and this reused pacemaker was implanted without complication. She showed no signs or symptoms of infection and her pacemaker had normal function 6-mo after the implantation.
The prime legal hurdle for pacemaker reprocessing in the United States is that the Food and Drug Administration (FDA) considers cardiac implantable electronic devices to be single-use devices (SUDs)[5]. Reuse of SUDs is highly regulated and while pacemaker reuse is technically possible, the United States FDA currently views it as “an objectionable practice”[38]. It is important to note that reuse of dialysis filters is commonplace in the United States and falls under stringent regulation[5]. For pacemaker reuse though, there exist other legal concerns to consider.
One is a concern among device manufacturers regarding a potential for legal action as a consequence of reused device failure. This sort of action is unlikely for two reasons. First, there are very few laws regarding SUDs in LMICs[5]. The United States is a highly litigious country, but the legal environment in countries where pacemakers would be reused is generally less susceptible to civil litigation[5]. Second, there is little tying device manufacturers to reuse of their products. Pacemakers are labeled as SUDs, warranties do not cover reuse, and none of the manufacturers sanctions pacemaker reuse. These two points notwithstanding, patients in LMICs receiving these devices must be made fully aware of the pacemaker origin, that the pacemaker no longer adheres to the original equipment manufacturer specifications, and that there may be rare risks of which we are not aware[5].
Ownership of explanted devices, post-mortem or after an extraction due to new clinical circumstances, presents an additional legal obstacle. There are no United States federal statutes addressing the ownership of medical devices after the patient’s death or a generator replacement procedure[5]. So theoretically patients, physicians, device manufacturers, and insurers could all lay claim to explanted devices. In Sweden in the 1990s, when pacemaker reuse was frequent, ownership of an explanted device was understood to belong to the medical center, which had placed the device[5]. In Holland and Canada, devices have traditionally been property of the patients or their heirs[39]. Alternatively, the medical professional who implants pacemakers could insist that the devices be returned to him/her for analysis[5]. An agency within the United States Department of Health and Human Services provides payment for the cost of the pacemakers and ICDs and associated implantation costs for a lion share of the elderly and the disabled, and it is conceivable that the payer might legally seek to own the product[5]. Device manufacturers may also lay claim through a contractual agreement that states the devices must be returned to the company after explantation for quality improvement[5]. Heart Rhythm Society endorses the return of devices to manufacturers for assessment and quality improvement[40].
Ultimately, under the precept of patient autonomy, which is deeply embedded in the medical ethics, device removal from a deceased patient without express patient or next of kin authorization is probably objectionable[5]. While insurers may wish to lay claim, premiums and/or taxes paid by the patient fund these entities. Any other claims for the device would do not prevail over patient’s property rights. In fact, the National Institutes of Health has embraced the notion of patient ownership[41]. An advance directive/pacemaker living will would officially outline patient wishes and authorize the funeral and crematory directors to retrieve pacemakers for donation or send them back to the manufacturer[5].
Health can be viewed through a prism of both private (individual) and societal (collective) good[13], and as such must be considered from many ethical and moral perspectives. In considering pacemaker reuse, the first question to ask is “does donating a device not approved for use in the donor country create a double standard too great to be morally acceptable[13]?” The World Health Organization (WHO) maintains that the donated device quality should be high enough so that the donor would find it acceptable[42]. Refurbished pacemakers would certainly be deemed unacceptable by the WHO given that their use in the United States is not approved[13].
Under egalitarian principles the ethics regarding pacemaker reuse is less clear. The most basic provision of health care to all is justified under most egalitarianism conceptions[13]. However, under egalitarian conceptions one would assert that there must be equal quality of healthcare resources available to all patients. This stance comports with the WHO and argues against pacemaker reutilization[13].
Utilitarian theories in the health care domain emphasize the utility of being healthy[13]. Much like how food banks acquire donated food and deliver it for those in need despite the fact that some items may not be “readily marketable”, pacemaker reutilization is consistent with the utilitarian concept given that the recipient benefit exceeds any harm to device donor[13]. Utilitarian theories often follow the rule of the greatest good for the greatest number of people[13]. In the context of pacemaker reutilization, the good that can be provided through device return for quality improvement must be considered and weighed against the good of reutilization. It can be argued however, that after a certain number of devices are returned to the manufacturer, the devices remaining will provide the most benefit through pacemaker reutilization[5].
According to the Difference Principle, proposed by Rawls[43], inequalities should be arranged “to the greatest benefit of the least advantaged”. In a 2010 WHO World Health Report[44], authors noted that 100 million people are impoverished every year due to their inability to meet the costs of the health care they need. Whether the recipients of reutilized pacemakers are the least advantaged is debatable. However, if pacemaker reuse improves patient physical condition and well-being, it may likely be considered tolerable under the Difference Principle[13]. As with many of the other theories discussed, a thorough exploration of the benefits and detriments of pacemaker reutilization is needed for a complete reconciliation with the Difference Principle[13].
The burdens, risks, and acceptable criteria of pacemaker reutilization must be considered as well. While the use of reprocessed pacemakers appears to be beneficial, measures need be in place to ensure that if a device malfunction or infection occurs, the implanting institution is capable of handling an emergency immediately and the patient is still able to receive a functioning device[13]. Nonmaleficence must be considered, as some patients may not be able to adhere to the recommended and important follow up with the implanting institution[5]. There is a potential of causing more harm than good with pacemaker reutilization if the patient is not able to access regular follow-up, and this risk requires careful examination[5]. Decisions on acceptable pacemaker condition, battery life, and resource distribution should be made collaboratively by all stakeholders - including members of the medical field and the lay public - to ensure equitable distribution of donated devices[13]. The risk of a “black market” for refurbished pacemakers is real and proper procedural strategies must be implemented to avoid foul play[5]. It is essential that there is a robust tracking system of the devices from the point of donation, through reprocessing, shipment, distribution to local implanting centers, and ultimately to the recipient patients. Careful patient screening for clinical and financial need can help ensure that the right resources get to the right recipient in the right place at the right time[5].
Voltaire is often quoted “the best is the enemy of the good”[45]. In the face of no reasonable alternative, as is the case for many in the target population for pacemaker reutilization, the benefit provided through a donated refurbished device significantly outweighs the possible risks[7]. A re-sterilized pacemaker can enhance the quality of life or even preserve life with no loss of equivalent moral value; thus it is a practice that ought to be pursued[7].
PMHYH shows that pacemaker donation involving funeral homes and crematories and an academic medical center is a viable means of providing underserved patients in LMICs with much needed device therapy[6]. PMHYH was founded in 2010 by physicians within The University of Michigan Frankel Cardiovascular Center in collaboration with World Medical Relief, the Michigan Funeral Directors Association, and a company that recycles the metallic by-products of the cremation process (Implant Recycling, LLC)[14]. The goal of PMHYH is to create a blueprint for treating those with severe bradyarrhythmia in LMICs[9].
Device acquisition is a key aspect of PMHYH. Specifically, funeral home industry is afforded access to an infrastructure of resources for obtaining consent from families of the deceased for pacemaker removal and an easy charge-free shipment of pacemaker after its removal[6]. As of 2013, PMHYH had collected over 10000 devices from funeral directors in the state of Michigan and 21% of the devices had ≥ 75% battery life or ≥ 4 years expected longevity[8].
Any pacemakers acquired will be subject to stringent interrogation to inspect for evidence of damage, to ensure sufficient battery life, and to check other important performance measures. To satisfy device manufacturers, interrogation printouts, necessary for reuse, can be provided after PMHYH interrogation[5]. For manufacturers, this is certainly more information than when devices are buried with the deceased or discarded as medical waste[5]. Devices with sufficient battery life that pass interrogation will then undergo a validated cleansing and sterilization protocol.
Once sterilized, devices can be packaged and made ready for shipment. Device storage prior to shipment, interrogation, cleaning, and sterilization would all occur at a centralized center of excellence. Project MHYH estimates the cost of the entire collection, reprocessing, and distribution to be roughly $75-$100 per device. Assuming implanting physicians and hospitals are willing to provide their services free of charge or at an acceptably low rate, individual and corporate donations would allow the pacemakers and ICDs to be provided to patients without charge[6].
In order for an institution to become a recipient of donated refurbished pacemaker or ICD, implanting hospitals will be required to provide some evidence of the existing infrastructure, where the implantation may take place, as well as physician and staff expertise in pacemaker and ICD implantation and related care[6]. This may include a visit from physicians in the United States and other nations who are affiliated with PMHYH. Upon approval of the institution and arrival of the devices, local physicians will implant the refurbished devices with new leads into patients with the greatest need based on recipients’ financial status and degree of conduction disease[9]. These same local physicians will then provide necessary follow-up services. This course of action taken by local physicians will aid in implantation success and patient health, and will reduce even further the risk for manufacturers of liability and potential legal action. The established relationships between PMHYH and UP-PGH in the Philippines and Indus Hospital in Karachi, Pakistan are good examples of the cross-institutional coordination necessary for pacemaker reuse and may prove valuable for future, large-scale implementation.
A web-based database would be created, allowing physicians to monitor patients with refurbished pacemakers[6]. This hopefully would restrain any inappropriate sale of refurbished pacemakers as well as provide a means (beyond routine follow-up) for communication between implanting physicians and patients in the case of device recall, or other emergent issues[6].
A brief summary of the PMHYH model, from collection to implantation, is shown in Table 1[8].
| 1. ID device for potential reuse |
| 2. Obtain signed consent from family |
| 3. Train funeral directors in device explantation |
| 4. Send device to center of excellence for investigation |
| a. Center does interrogation to assure adequate battery life and other performance-testing specifications |
| b. Use cutoff of ≥ 70% battery life |
| 5. Devices that pass all quality-control measures undergo process to erase all patient identifiers |
| 6. Sterilize and package |
| 7. Send device to nonprofit charitable organization that specializes in delivering medical equipment for distribution to low- and middle-income countries |
| 8. Device implanted with new unused leads |
Numerous studies show that the concept of pacemaker reutilization in LMICs is feasible. Most ethical concepts support pacemaker reuse. Rates of malfunction for reused devices have been found in prior studies to be no higher than that for new devices. The increased rate of malfunction found in the recent meta-analysis while concerning, is a risk believed to be acceptable for patients in dire need of bradyarrhythmia therapy in LMICs[10]. PMHYH is poised to conduct a prospective randomized, non-inferiority, multicenter study to confirm the clinical efficacy and safety of pacemaker reuse, for clinical and legal support.
There exists now a wonderful opportunity to positively affect countless lives in impoverished countries through pacemaker reutilization. A resource, which is currently not used, could enhance quality of life and extend life in LMICs and the time is now to pursue trials of pacemaker reuse for the betterment of society.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A, A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Amiya E, Barili F, Lee TM, Peteiro J S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Baman TS, Crawford T, Sovitch P, Meier P, Sovitch N, Gakenheimer L, Kirkpatrick J, Wasserman B, Samson G, Oral H. Feasibility of postmortem device acquisition for potential reuse in underserved nations. Heart Rhythm. 2012;9:211-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Romero J, Romero A, Kirkpatrick JN, Lange DC, Eagle KA, Baman TS. Pacemaker reuse in a 65-year-old woman in the Philippines with severe medical need. Pacing Clin Electrophysiol. 2010;33:e8-e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Baman TS, Eagle KA. Cardiac device reutilization: is it time to “go green” in underserved countries? Pacing Clin Electrophysiol. 2011;34:651-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Baman TS, Meier P, Romero J, Gakenheimer L, Kirkpatrick JN, Sovitch P, Oral H, Eagle KA. Safety of pacemaker reuse: a meta-analysis with implications for underserved nations. Circ Arrhythm Electrophysiol. 2011;4:318-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Kirkpatrick JN, Papini C, Baman TS, Kota K, Eagle KA, Verdino RJ, Caplan AL. Reuse of pacemakers and defibrillators in developing countries: logistical, legal, and ethical barriers and solutions. Heart Rhythm. 2010;7:1623-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Baman TS, Kirkpatrick JN, Romero J, Gakenheimer L, Romero A, Lange DC, Nosowsky R, Fuller K, Sison EO, Tangco RV. Pacemaker reuse: an initiative to alleviate the burden of symptomatic bradyarrhythmia in impoverished nations around the world. Circulation. 2010;122:1649-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Aragam KG, Baman TS, Kirkpatrick JN, Goldman EB, Brown AC, Crawford T, Oral H, Eagle KA. The ethics of pacemaker reuse: might the best be the enemy of the good? Heart. 2011;97:2005-2006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Badin A, Baman TS, Eagle KA, Crawford TC. Pacemaker reutilization for those in underserved nations: examining preliminary data and future prospects. Interventional Cardiology. 2013;5:695-702. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Gakenheimer L, Romero J, Sovitch P, Machado C, Eagle K, Baman T. Pacemakers: Are They Really a Renewable Resource? EP Lab Digest 2010, [accessed 2015 Dec 13]. Available from: http: //www.eplabdigest.com/articles/Pacemakers-Are-They-Really-A-Renewable-Resource. |
| 10. | Hughey AB, Baman TS, Eagle KA, Crawford TC. Pacemaker reuse: an initiative to help those in underserved nations in need of life-saving device therapy. Expert Rev Med Devices. 2013;10:577-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Gakenheimer L, Romero J, Baman TS, Montgomery D, Smith CA, Oral H, Eagle KA, Crawford T. Cardiac implantable electronic device reutilization: battery life of explanted devices at a tertiary care center. Pacing Clin Electrophysiol. 2014;37:569-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Baman TS, Romero A, Kirkpatrick JN, Romero J, Lange DC, Sison EO, Tangco RV, Abelardo NS, Samson G, Grezlik R. Safety and efficacy of pacemaker reuse in underdeveloped nations: a case series. J Am Coll Cardiol. 2009;54:1557-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | VanArtsdalen J, Goold SD, Kirkpatrick JN, Goldman E, Eagle K, Crawford T. Pacemaker reuse for patients in resource poor countries: is something always better than nothing? Prog Cardiovasc Dis. 2015;55:300-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Reddy K, Vedanthan R, Kimaiyo S, Hughey A, Eagle K, Crawford T. Delivering Care Where It’s Needed. American Scientific: Promoting Cardiovascular Health Worldwide: Perspective on the 12 Recommendations from the Institute of Medicine 2013; 36-41. [accessed 2015 Dec 13] Available from: http: //www.scientificamerican.com/products/cardiovascular-health. |
| 15. | Who. int. WHO | Cardiovascular diseases (CVDs). [accessed 2015 Dec 13]. Available from: http: //www.who.int/mediacentre/factsheets/fs317/en. |
| 16. | Lopez AD, Mathers , CD , Ezzati M, Jamison D, Murray C. Global Burden of Disease and Risk Factors. Washington, DC: World Bank Publications 2006; . |
| 17. | Joshi R, Jan S, Wu Y, MacMahon S. Global inequalities in access to cardiovascular health care: our greatest challenge. J Am Coll Cardiol. 2008;52:1817-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 18. | Heartbeatintl. org. Heartbeat International. Home. 2015. [accessed 2015 Dec 13]. Available from: http: //www.heartbeatsaveslives.org/advocacy-kit. |
| 19. | Mond HG, Irwin M, Ector H, Proclemer A. The world survey of cardiac pacing and cardioverter-defibrillators: calendar year 2005 an International Cardiac Pacing and Electrophysiology Society (ICPES) project. Pacing Clin Electrophysiol. 2008;31:1202-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 124] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 20. | Mond HG, Proclemer A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009--a World Society of Arrhythmia’s project. Pacing Clin Electrophysiol. 2011;34:1013-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Data. worldbank.org. New Country Classifications-Data. [accessed 2015 Dec 13]. Available from: http: //data.worldbank.org/news/new-country-classifications-2015. |
| 22. | Birnie D, Williams K, Guo A, Mielniczuk L, Davis D, Lemery R, Green M, Gollob M, Tang A. Reasons for escalating pacemaker implants. Am J Cardiol. 2006;98:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Millar RN. 1998 survey of cardiac pacing in South Africa--report of the working group on registries of the cardiac arrhythmia society of South Africa (CASSA). S Afr Med J. 2001;91:873-876. [PubMed] |
| 24. | Thomas MO, Oke DA, Ogunleye EO, Adeyanju FA. Bradypacing: indications and management challenges in Nigeria. Pacing Clin Electrophysiol. 2007;30:761-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Blum JA, Zellweger MJ, Burri C, Hatz C. Cardiac involvement in African and American trypanosomiasis. Lancet Infect Dis. 2008;8:631-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Oliveira BG, Velasquez-Melendez G, Rincón LG, Ciconelli RM, Sousa LA, Ribeiro AL. Health-related quality of life in Brazilian pacemaker patients. Pacing Clin Electrophysiol. 2008;31:1178-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Rydén L. Re-use of devices in cardiology. Proceedings from a Policy Conference at the European Heart House, 5-6 February, 1998. Eur Heart J. 1998;19:1628-1631. [PubMed] |
| 28. | Benkemoun H, Sacrez J, Lagrange P, Amiel A, Prakash A, Himmrich E, Aimè E, Mairesse GH, Guénon C, Sbragia P. Optimizing pacemaker longevity with pacing mode and settings programming: results from a pacemaker multicenter registry. Pacing Clin Electrophysiol. 2012;35:403-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Brunner M, Olschewski M, Geibel A, Bode C, Zehender M. Long-term survival after pacemaker implantation. Prognostic importance of gender and baseline patient characteristics. Eur Heart J. 2004;25:88-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 93] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 30. | Gakenheimer L, Lange DC, Romero J, Kirkpatrick JN, Sovitch P, Oral H, Eagle KA, Baman TS. Societal views of pacemaker reutilization for those with untreated symptomatic bradycardia in underserved nations. J Interv Card Electrophysiol. 2011;30:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Cremation Association of North America. [accessed 2015 Dec 13]. Available from: http: //www.cremationassociation.org/?page=AboutCANA. |
| 32. | Kirkpatrick JN, Ghani SN, Burke MC, Knight BP. Postmortem interrogation and retrieval of implantable pacemakers and defibrillators: a survey of morticians and patients. J Cardiovasc Electrophysiol. 2007;18:478-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 33. | Nava S, Morales JL, Márquez MF, Barrera F, Gómez J, Colín L, Brugada J, Iturralde P. Reuse of pacemakers: comparison of short and long-term performance. Circulation. 2013;127:1177-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Panja M, Sarkar CN, Kumar S, Kar AK, Mitra S, Sinha DP, Chatterjee A, Roy S, Sarkar NC, Majumder B. Reuse of pacemaker. Indian Heart J. 1996;48:677-680. [PubMed] |
| 35. | Mendes GC, Brandão TR, Silva CL. Ethylene oxide sterilization of medical devices: a review. Am J Infect Control. 2007;35:574-581. [PubMed] |
| 36. | Rutala WA, Weber DJ. Infection control: the role of disinfection and sterilization. J Hosp Infect. 1999;43 Suppl:S43-S55. [PubMed] |
| 37. | US FDA Compliance Manuals. CPG Sec 310.100 Pacemaker Reuse (CPG) 7124.12). [accessed 2015 Dec 12]. Available from: http: //www.fda.gov/ICECI/ComplianceManuals/CompliancePolicy GuidanceManual/ucm073891.htm. |
| 38. | Jackson M. Issues affecting refurbishment and re-use of pacemakers. Aust Health Rev. 1996;19:68-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 39. | Carlson MD, Wilkoff BL, Maisel WH, Carlson MD, Ellenbogen KA, Saxon LA, Prystowsky EN, Alpert JS, Cain ME, Ching EA. Recommendations from the Heart Rhythm Society Task Force on Device Performance Policies and Guidelines Endorsed by the American College of Cardiology Foundation (ACCF) and the American Heart Association (AHA) and the International Coalition of Pacing and Electrophysiology Organizations (COPE). Heart Rhythm. 2006;3:1250-1273. [PubMed] [DOI] [Full Text] |
| 40. | US Department of Health and Human Services, National Institutes of Health. Improving Medical Implant Performance Through Retrieval Information: Challenges and Opportunities. NIH Technology Assessment Conference Summary. 2000;. |
| 41. | WHO medical device regulations. [accessed 2015 Dec 13]. Available from: http: //www.who.int/medical_devices/publications/en/MD_Regulations.pdf. |
| 42. | Rawls J. A theory of justice. Cambridge (Ma): Harvard University Press 1971; . |
| 43. | WHO. World Health Report: Health Systems Financing: The Path to Universal Coverage. Geneva: Universal Coverage 2010; . |
| 44. | Ratcliffe S. Concise Oxford Dictionary Of Quotations. Oxford: Oxford University Press 2011; 389. |