Published online Mar 26, 2017. doi: 10.4330/wjc.v9.i3.289
Peer-review started: August 30, 2016
First decision: September 27, 2016
Revised: October 28, 2016
Accepted: January 11, 2017
Article in press: January 14, 2017
Published online: March 26, 2017
Processing time: 209 Days and 21.6 Hours
The spasm provocation test (SPT) is an important test in the diagnosis of vasospastic angina (VSA). In many cases, this test is performed as the gold standard test, and VSA is considered not present if the SPT is negative. However, some patients continue to experience chest symptoms despite a negative SPT. In this study, we report four cases in which SPT was repeated to evaluate chest symptoms despite the negative results of the first SPT. Two men in their 70s, one woman in her 60s, and one woman in her 70s, all with chest symptoms, underwent a second SPT at 4, 3, 2, and 3 years, respectively, after the first SPT, which was negative. Three patients had positive results in the second SPT (75%). In conclusion, even when SPT is negative, the diagnosis of VSA should be made with clinical symptoms in consideration. In some cases, a second SPT may be required to confirm the diagnosis of VSA.
Core tip: The spasm provocation test (SPT) is an important examination when diagnosing vasospastic angina (VSA). In general, if the SPT is negative, VSA is considered not present. However, we encountered four patients who underwent a second SPT although the first SPT was negative. In these patients, some show a positive second SPT result. SPT is not a perfect examination, and in the clinical setting, the diagnosis of VSA should be made with the consideration of their clinical symptoms and examinations.
- Citation: Teragawa H, Fujii Y, Uchimura Y, Ueda T. Importance of a second spasm provocation test: Four cases with an initial negative spasm provocation test. World J Cardiol 2017; 9(3): 289-295
- URL: https://www.wjgnet.com/1949-8462/full/v9/i3/289.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i3.289
Coronary spasm is characterized by transient vasoconstriction of the epicardial coronary artery, leading to myocardial ischemia. Coronary spasm is the cause of not only typical rest angina but also exertional angina, acute myocardial infarction, and sudden cardiac death[1,2]. Therefore, the diagnosis of vasospastic angina (VSA) should be made with certainty. VSA is diagnosed by the presence of chest symptoms accompanied by transient ST deviation on the electrocardiogram (ECG)[3,4]. This can, however, be difficult in the clinical setting because angina attacks do not necessarily occur during the one day of ECG monitoring or because ST changes are not always documented by ECG even in the presence of chest symptoms. In such cases, the spasm provocation test (SPT) can be used[3-5]. In the clinical setting, SPT is the gold standard examination to diagnose VSA. However, we observed some cases in which chest symptoms continued despite a negative SPT. Here, we report four such cases in which a second SPT was performed to evaluate chest symptoms despite negative results in the first SPT.
At our institution, SPT is performed in the afternoon. Vasodilators are stopped 2 d before SPT. For SPT, acetylcholine (ACh) is usually used as the provocation drug, with 30 and 50 μg for the right coronary artery (RCA) and 50 and 100 μg for the left coronary artery (LCA). If the SPT results are negative with these doses, additional doses of ACh (80 μg for the RCA and 200 µg for the LCA) and/or ergonovine maleate (EM; 20, 40, and 60 μg for the LCA) are sometimes added. A positive SPT is defined as the presence of transient vasoconstriction > 90% in response to intracoronary infusions of provocative drugs on coronary angiograms. The positive result is accompanied by the usual chest symptoms and/or ischemic ST deviations in the patient’s ECG[3].
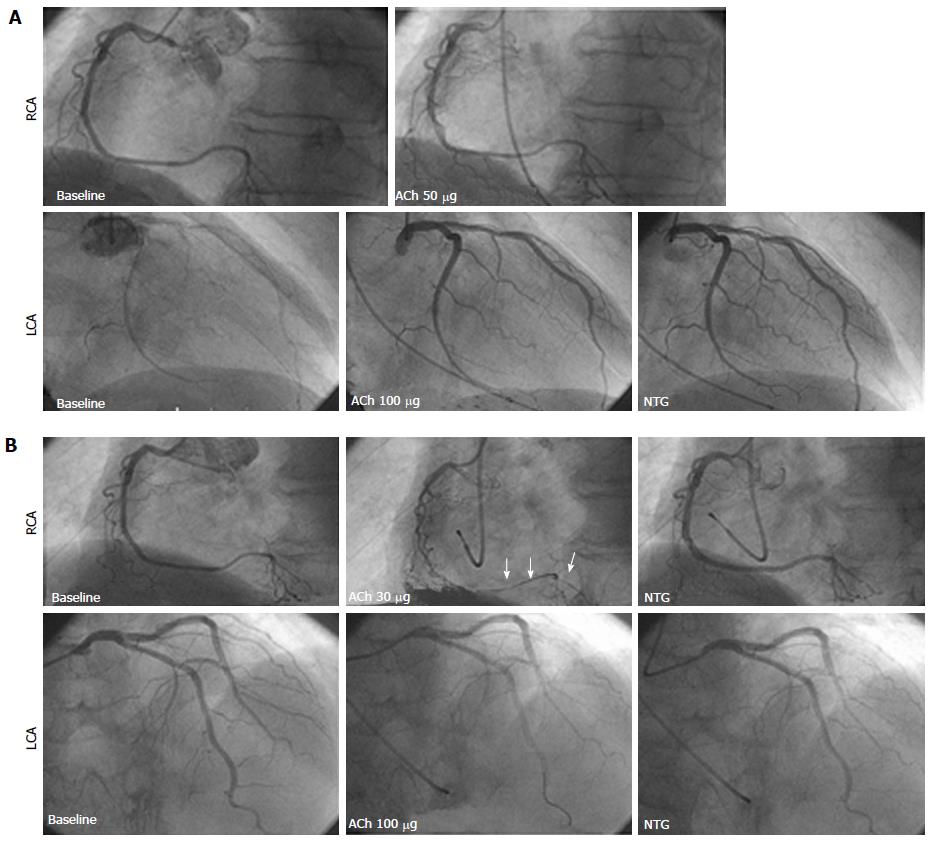
A man in his 70s underwent an SPT because of chest pain at rest. His coronary risk factors were smoking (30 cigarettes per day for 30 years) and hypertension. The SPT showed negative results after intracoronary infusions of ACh with 50 μg for the RCA and 100 μg for the LCA (Figure 1A). Thereafter, he continued to experienced chest pain at rest but did not seek further help for his chest symptoms. Four years later, he felt severe chest pain at rest in the early morning, which was relieved by sublingual nitroglycerin (NTG). Therefore, he underwent a second SPT, which was positive for the RCA with an intracoronary infusion of 30 μg ACh. The result was accompanied by the usual chest symptoms and ECG changes, despite negative LCA results after an intracoronary infusion of NTG (Figure 1B). At that time, we used a pressure wire inserted into the distal RCA. The distal intracoronary pressure /aortic pressure (Pd/Pa) decreased from 0.99 at baseline to 0.73 after the ACh infusion. He was diagnosed with VSA and discharged with a prescription for a calcium channel blocker (CCB).
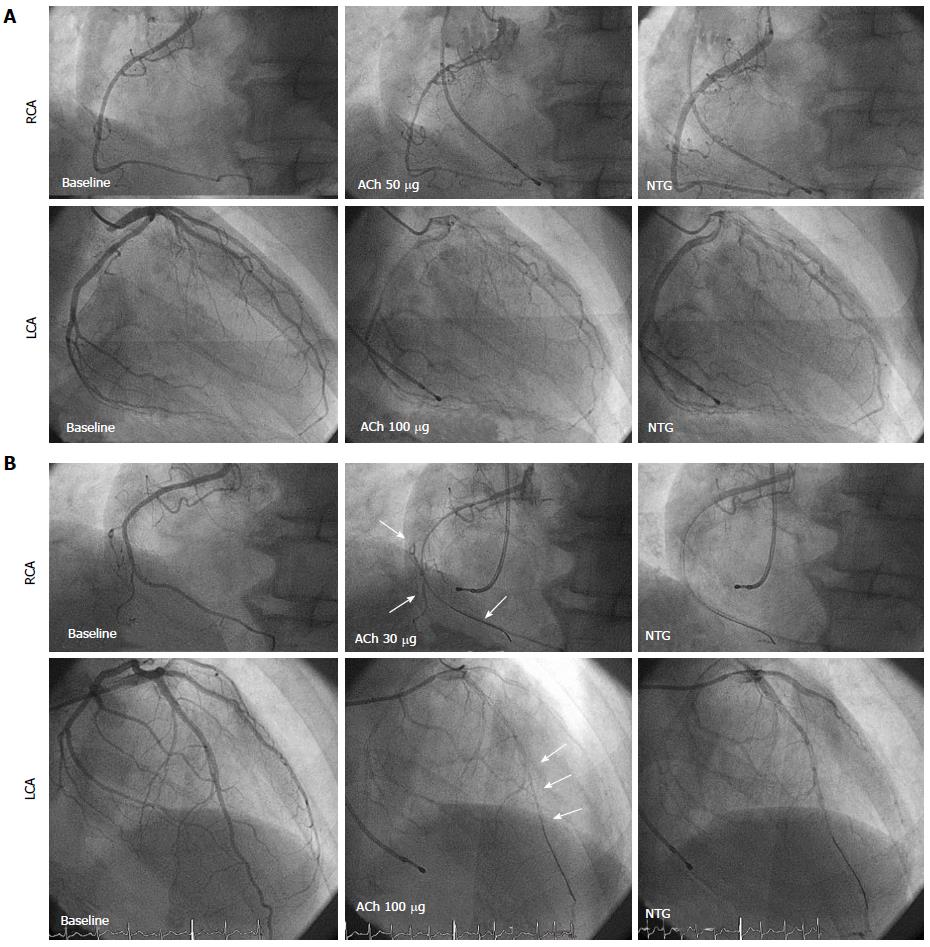
A male in his 70s underwent an SPT because of chest pain at rest, which occurred for 1-2 min and frequently 3-4 times/wk. He had no coronary risk factors. The SPT showed moderate vasoconstriction of the RCA after 50 μg ACh and moderate vasoconstriction of the LCA after 100 µg ACh (Figure 2A). However, he did not experience chest symptoms or ST deviation on ECG during the SPT. Hence, the SPT result was judged as negative. His chest symptoms continued thereafter, and he had severe chest pain at midnight 3 years later; therefore, he underwent a second SPT 3 years after the first SPT. The second SPT showed positive results for both the RCA after intracoronary infusions of 50 µg ACh and the LCA after infusions of 100 µg ACh (Figure 2B). The test was accompanied by the usual chest symptoms. The Pd/Pa decreased from 0.96 at baseline to 0.75 during the RCA spasm and from 0.93 at baseline to 0.74 during the left anterior descending coronary artery (LAD) spasm. He was diagnosed with VSA and was discharged with CCB medication.
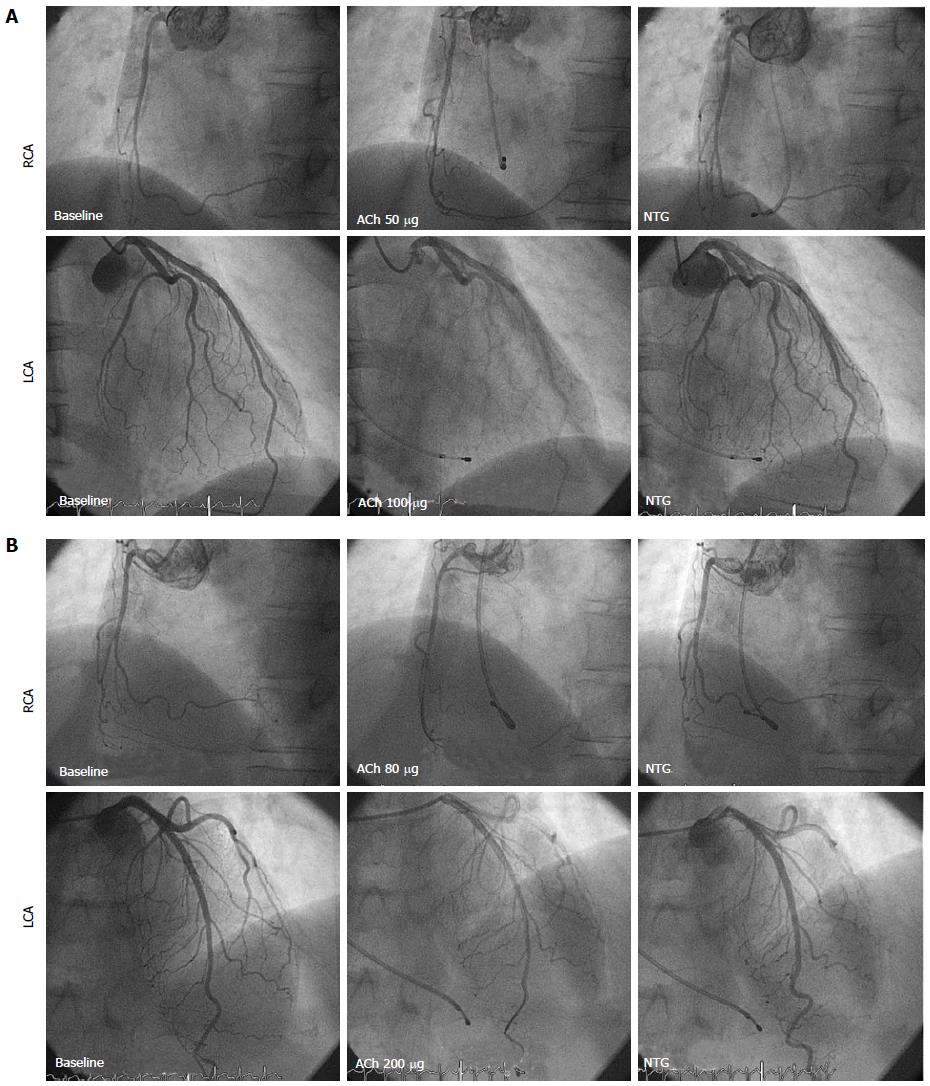
A female in her 60s underwent an SPT due to 1-2-min chest pain at rest during the night. She had no coronary risk factors. The SPT showed negative RCA results after 50 μg ACh and for the LCA after an intracoronary infusion of 100 μg ACh (Figure 3A). Nevertheless, her symptoms continued. CCB did not help, and she underwent the second SPT 3 years after the first SPT. The second SPT showed negative RCA results after 80 μg ACh and for the LCA after 200 μg ACh (Figure 3B). The Pd/Pa did not change significantly, from 1.00 at baseline to 0.92 with 80 μg ACh in the RCA and from 0.95 at baseline to 0.93 with 200 μg ACh in the LAD. She was discharged with analgesic and anti-depressive medication.
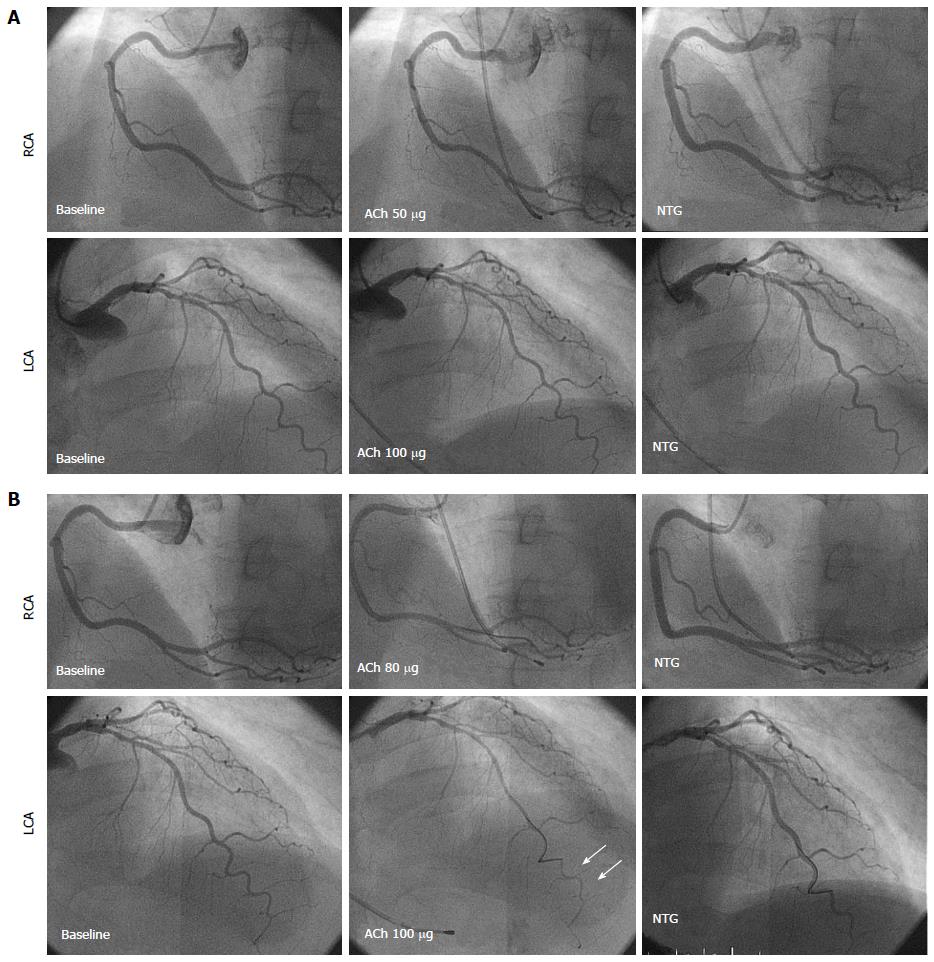
A female in her 70s underwent an SPT to evaluate chest pain in the evening lasting for 1 min. Her coronary risk factors were hypertension and lipid disorder. The SPT showed negative RCA results after 50 µg ACh and for the LCA after 100 μg ACh (Figure 4A). Thereafter, her chest symptoms were infrequent, but she felt severe chest pain at rest 3 years later, when she presented at our institution for the second SPT. The second SPT showed negative RCA results after an intracoronary infusion of 50 μg ACh, and severe vasoconstriction at the distal LAD without chest symptoms and ECG changes after an intracoronary infusion of 100 μg ACh (Figure 4B). At the time, the Pa/Pa decreased from 0.90 at baseline to 0.73 after the ACh infusion. Based on the angiograms and pressure wire findings, she was diagnosed with VSA. She was discharged with CCB medication and has not experienced chest symptoms since.
In summary, there were three positive results from a second SPT (75%) of four cases that experienced chest symptoms and had negative results for the first SPT.
In the present report, we present four patients who underwent a second SPT for the evaluation of chest symptoms, despite negative results from the first SPT. Of the four cases, there were three positive cases (75%). From these cases, we learned that SPT is not an absolute and final examination for diagnosing VSA.
SPT has been widely adopted as the final examination for the diagnosis of VSA. However, several factors may affect a positive SPT finding, such as VSA activity, time of day when the SPT is performed, and the duration of the withdrawal of vasodilators. VSA activity is variable, not only daily but also seasonally or yearly[3], and this may contribute to the difference in SPT results. According to the time spent performing the SPT, it may be ideal to perform the SPT when VSA angina attacks occur easily, particularly in the morning. However, at our institution, SPTs are performed only in the afternoon. In these four cases presented here, both the first and second SPTs were performed at the same time in the afternoon. For the withdrawal of vasodilators before SPT, vasodilators were withheld at least 48 h before SPT[3,6]; however, 2 d may be insufficient for the withdrawal of long-acting CCBs. This factor may contribute to the discrepancy of SPT results.
The SPT procedure is another important problem. The maximal doses of 50 μg ACh for the RCA and 100 µg for the LCA, in general, are recommended[3]. However, SPT using higher ACh doses of 80 µg for the RCA and 200 μg for the LCA[7,8] and/or using a combination of ACh and EM[6,8], have recently been recommended. The use of higher ACh doses and/or a combination of ACh and EM may decrease the number of incomplete SPTs. In case 3, we judged the results as negative after higher ACh intracoronary infusion doses for the second SPT. To deny the possibility of VSA, it may be ideal to perform the SPT using higher concentrations of ACh. In addition, we used a pressure wire in all four cases. Using a pressure wire in SPT may be useful for diagnosing VSA[9] because the presence of myocardial ischemia can be detected promptly when the Pd/Pa is continuously monitored. Although an SPT using a pressure wire is not always recommended in all patients, this technique may provide additional information for VSA diagnosis and may, therefore, be useful for the second SPT.
In our cases shown here, there were the gaps of 3 to 4 years between the first and second SPT. During these periods, vascular dysfunction and/or atherosclerotic changes were newly developed. Thus, we cannot deny the possibility that coronary spasticity emerges during such periods, leading to a positive result for second SPT despite a negative result of the first SPT.
Even when the SPT is negative, the diagnosis of VSA should be with clinical symptoms in consideration. In some cases, a second SPT may be needed to confirm the diagnosis of VSA. Cardiologists should keep these concepts in mind.
There are four patients who underwent a spasm provocation test (SPT) for a second time to evaluate chest symptoms despite negative results for the first SPT.
Vasospastic angina, which was diagnosed with the second SPT.
Microvascular angina, chest pain syndrome and gastroesophageal reflux disease.
All labs were within normal limits.
In 3 of 4 patients, the second SPT showed positive results with the angiographical coronary vasoconstriction, accompanied by usual chest symptoms and reduced intracoronary pressure measured with a pressure wire and/or ischemic changes of the electrocardiogram (ECG).
Vasodilators, including calcium-channel blockers, were administered in 3 patients who had positive results in the second spasm SPT, and analgesics and anti-depressive medication were administered in 1 patient with a negative result for the second SPT.
There are many case reports and studies of the spasm provocation test; however, this is the first report showing positive results for the second SPT despite negative results for the first SPT.
Vasospastic angina (VSA) is characterized by the transient vasoconstriction of the epicardial coronary artery, leading to myocardial ischemia. It is the cause of not only rest angina but also exertional angina, acute coronary syndrome and ischemic cardiac arrest. VSA is diagnosed with chest symptoms and transient ischemic changes of the ECG, mainly at rest, but there are many cases in which the diagnosis is difficult when only based on chest symptoms and ECG monitoring. In such cases, an SPT using acetylcholine and/or ergonovine are performed and the results of the SPT are considered the final decision.
Even when SPT is negative, the diagnosis of VSA should be made with the consideration of clinical symptoms. In some cases, a second SPT may be needed to confirm the diagnosis of VSA.
This paper is interesting.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kettering K, Peteiro J, Sabate M S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Yasue H, Kugiyama K. Coronary spasm: clinical features and pathogenesis. Intern Med. 1997;36:760-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 165] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51:2-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 378] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 3. | Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina) (JCS 2013). Circ J. 2014;78:2779-2801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 356] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 4. | Beltrame JF, Crea F, Kaski JC, Ogawa H, Ong P, Sechtem U, Shimokawa H, Bairey Merz CN. International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2015;pii:ehv351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 179] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 5. | Sueda S, Kohno H, Fukuda H, Ochi N, Kawada H, Hayashi Y, Uraoka T. Frequency of provoked coronary spasms in patients undergoing coronary arteriography using a spasm provocation test via intracoronary administration of ergonovine. Angiology. 2004;55:403-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Sueda S, Kohno H, Ochi T, Uraoka T. Overview of the Acetylcholine Spasm Provocation Test. Clin Cardiol. 2015;38:430-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 7. | Sueda S, Kohno H, Miyoshi T, Sakaue T, Sasaki Y, Habara H. Maximal acetylcholine dose of 200 μg into the left coronary artery as a spasm provocation test: comparison with 100 μg of acetylcholine. Heart Vessels. 2015;30:771-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Sueda S, Miyoshi T, Sasaki Y, Sakaue T, Habara H, Kohno H. Sequential spasm provocation tests might overcome a limitation of the standard spasm provocation tests. Coron Artery Dis. 2015;26:490-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Teragawa H, Fujii Y, Ueda T, Murata D, Nomura S. Case of angina pectoris at rest and during effort due to coronary spasm and myocardial bridging. World J Cardiol. 2015;7:367-372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |