Published online Dec 26, 2017. doi: 10.4330/wjc.v9.i12.842
Peer-review started: September 13, 2017
First decision: October 23, 2017
Revised: November 1, 2017
Accepted: November 27, 2017
Article in press: November 27, 2017
Published online: December 26, 2017
Processing time: 100 Days and 6.5 Hours
Patients with critical limb ischemia necessitate immediate intervention to restore blood flow to the affected limb. Endovascular procedures are currently preferred for these patients. We describe the case of an 80-year-old female patient who presented to our department with ischemic rest pain and ulceration of the left limb. The patient had history of left femoral popliteal bypass surgery, femoral thromboendarterectomy and patch angioplasty of the same limb 2 years ago. Doppler sonography and magnetic resonance angiography revealed an occlusion of the left superficial femoral artery (SFA) and popliteal artery and of all three infra-popliteal arteries. Due to severe comorbidities, the patient was scheduled for a digital subtraction angiography. An antegrade approach was first attempted, however the occlusion could not be passed. After revision of the angiography acquisition, a stent was identified at the level of the mid SFA, which was subsequently directly punctured, facilitating the retrograde crossing of the occlusion. Thereafter, balloon angioplasty was performed in the SFA, popliteal artery and posterior tibial artery. The result was considered suboptimal, but due to the large amount of contrast agent used, a second angiography was planned in 4 wk. In the second session, drug coated balloons were used to optimize treatment of the SFA, combined with recanalization of the left fibular artery, to optimize outflow. The post-procedural course was uneventful. Ischemic pain resolved completely after the procedure and at 8 wk of follow-up and the foot ulceration completely healed.
Core tip: Herein, we present a patient with critical ischemia of the lower limb, due to long occlusive disease of the femoro-popliteal and below-the-knee arteries who was successfully treated using an endovascular approach after failed bypass surgery and using the direct stent puncture technique. This case demonstrates that an endovascular approach may be extremely valuable even in very long, complex occlusive peripheral artery disease. This may further shift treatment from surgical to endovascular treatment in the near future.
- Citation: Korosoglou G, Eisele T, Raupp D, Eisenbach C, Giusca S. Successful recanalization of long femoro-crural occlusive disease after failed bypass surgery. World J Cardiol 2017; 9(12): 842-847
- URL: https://www.wjgnet.com/1949-8462/full/v9/i12/842.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i12.842
The prevalence and mortality of peripheral artery disease (PAD) rapidly increased during the last years due to prolonged life expectancy and is estimated to affect ≥ 30% of older patients within the next few years[1,2]. Particularly patients with critical limb ischemia (CLI) show poor outcome with high risk for major amputation and high death rates within the first year after diagnosis[3,4]. Such patients very frequently suffer from comorbidities, like renal failure and diabetes mellitus[5] and are at high risk for septic shock if perfusion is not promptly re-established.
In patients with CLI, arterial revascularization should be performed without delay. Current guidelines provided by the task force for the treatment of PAD recommend an “endovascular first” approach in patients with CLI, taking the potential risk and the anticipated success rate of interventional treatment option into account[6]. Procedural decision should also consider the localization, complexity and length of the vascular lesions, as well as local expertise, comorbidities such as diabetes mellitus and renal failure and patients’ preferences[7].
Herein, we present the case of an 80-year-old female patient with CLI due to long occlusive disease of the femoral superficial, popliteal and all 3 infra-popliteal arteries, who was successfully treated endovascularly in 2 sessions.
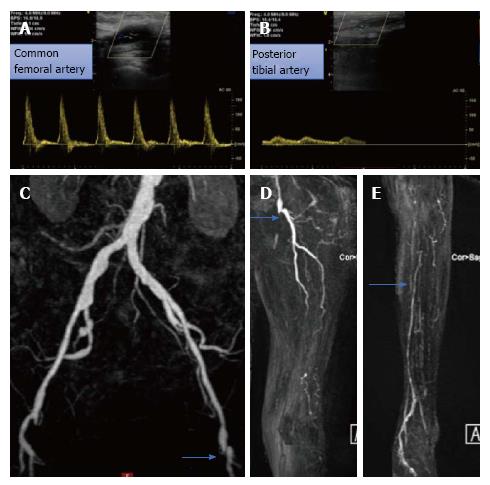
An 80-year-old female patient was referred to our department due to CLI with ulceration of the left limb (Rutherford Class 5), accompanied by ischemic rest pain. The patient had history of multi-vessel coronary artery disease with non-ST elevation myocardial infarction 3 mo ago. Left ventricular function was moderately reduced. In addition, she had history of arterial hypertension, hyperlipidemia, prior cigarette smoking and type 2 diabetes mellitus. Furthermore, atrial fibrillation was present. The laboratory markers showed reduced renal function with a creatinine of 1.4 mg/dL with an estimated glomerular filtration rate of GFR = 36 mL/min per 1.73 m². White blood count and C-reactive protein were increased (12300/μL and 18.3 mg/L, respectively) at the time of presentation. Clinical inspection revealed the presence of a forefoot ulcer without presence of gangrenous necrosis. The patient had history of left femoral popliteal bypass surgery as well as femoral thromboendarterectomy and patch angioplasty surgery 2 years ago. Duplex sonography relieved biphasic flow in the left iliac external and common femoral artery and a long occlusion of the femoral and popliteal artery with blunted monophasic flow in the posterior tibial artery (Figure 1A and B). No flow was present in the anterior tibial and in the fibular arteries. The ankle-brachial-index was severely reduced at 0.30. Magnetic resonance angiography (MRA) confirmed these findings, exhibiting no stenosis of the iliac arteries (Figure 1C), a long total occlusion of the left superficial femoral (SFA) (blue arrow in D showing flush occlusion of the SFA) and of the popliteal artery with collateral filling to the proximal part of the posterior tibial artery (blue arrow in Figure 1E) and occlusion of the anterior tibial, the tibiofibular tract and of the fibular artery (Figure 1D and E).
The patient had a history of chronic renal disease (creatinine = 1.4 mg/dL, GFR = 35 mL/min per 1.73 m2), atrial fibrillation, chronic obstructive lung disease (GOLD Class 3), type 2 diabetes mellitus and multi-vessel coronary artery disease with prior non-ST elevation infarction 3 mo ago.
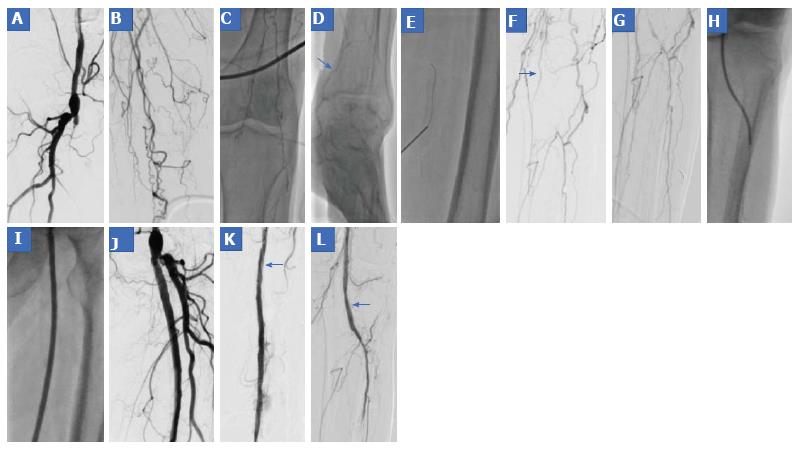
Due to history of failed bypass surgery and severe cardio-pulmonary comorbidities the patient was scheduled for invasive digital subtraction angiography (DSA). After inserting a 6F guiding cross-over introducer sheath (Terumo Destination®, Terumo interventional systems, Eschborn, Germany) by puncture of the right CFA, DSA confirmed flush occlusion of the left SFA (Figure 2A) with no native vessels depicted in the upper leg and in the proximal lower leg (Figure 2B and C) and with scarce filling of the posterior tibial artery (blue arrow in Figure 2D) (Video 1). Subsequently, 500 mg aspirin and 5000 IU of heparin were injected and antegrade recanalization was attempted using different hydrophilic tapered and non-tapered guidewires. However, antegrade crossing of the occlusion failed, possibly due to presence of scarred tissue in this area after surgery. After careful revision of the initial moving table non-DSA acquisition (Video 1), a stent was identified at the level of the mid SFA, which was subsequently directly punctured, facilitating the retrograde insertion of a 0.035’’ advantage guidewire (Terumo interventional systems, Eschborn, Germany) (Figure 2E and Video 1). Subsequently, retrograde passage of a 0.018’’ advantage guidewire was achieved over a 0.035’’ TrailBlazer support catheter, which was then snared in the 6F guiding cross-over sheath. Then, the retrograde 0.035’’ support catheter was pulled back and a second antegrade 0.035’’ support catheter was inserted over the 6F guiding cross-over sheath, which passed over the SFA through the punctured stent and was advanced to the level of the popliteal artery (blue arrow in Figure 2F). Over this 0.035’’ support catheter, a 0.014’’ advantage guidewire was advanced to the proximal anterior tibial artery and its intraluminal localization was confirmed by DSA (Figure 2G). Balloon angioplasty was then performed using a 2.5 mm × 200 mm Armada balloon (Figure 2H) in the infra-popliteal level and 5.0 mm × 200 mm and 6.0 mm × 200 mm Armada balloons (Figure 2I) (Abbott Vascular Deutschland GmbH) in the popliteal and SFA, respectively. Due to extensive dissection of the proximal SFA a 6.0 mm × 80 mm Innova self-expanding bare metal stent was placed (Boston Scientific, Ratingen, Germany). The final angiographic result, which can be depicted in Figure 2J-L was judged as suboptimal due to the absence of outflow in the lower leg. However, intervention was stopped at this point due to contrast agent administration of approximately 200 mL with chronic renal disease. The patient was put on treatment with 100 mg aspirin, 75 mg clopidogrel and 5 mg fondaparinux daily and was scheduled for re-angiography after 4 wk.
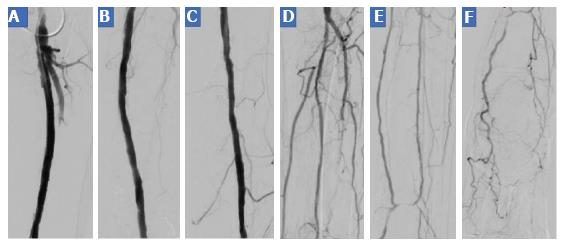
In the second session antegrade puncture of the left CFA was performed directly above the implanted stent in the proximal SFA with subsequent insertion of a short 6F guiding introducer sheath. DSA revealed moderate restenosis of the mid SFA and of the popliteal artery, which were treated using 5.0 mm × 120 mm and 6.0 mm × 120 mm Impact Pacific (Medtronic GmbH, Meerbusch, Germany) drug coated balloons, respectively. In addition, recanalization of the fibular artery was performed, resulting in functional 2 vessel out-flow of the shortly occluded posterior tibial and of the fibular artery to the left foot. Final DSA images can be appreciated in Figure 3.
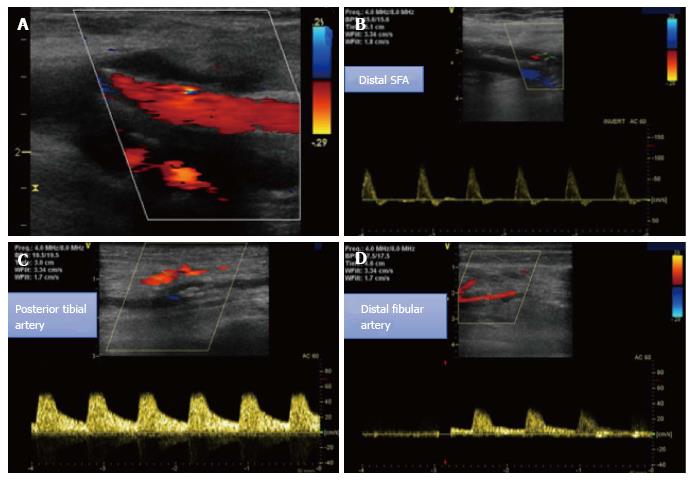
The clinical course of the patient was uneventful, and she was discharged at the following day. Ischemic pain had resolved completely, and the foot ulceration healed after 3 wk. The ankle-brachial-index increased to 0.98. The patient was set on treatment with 5 mg ramipril, 20 mg atorvastatin, 5 mg bisoprolol, 75 mg clopidogrel and 15 mg rivaroxaban per day. After 8 wk, duplex sonography exhibited a well perfused SFA with biphasic flow in the distal SFA and in the popliteal artery and monophasic flow of the distal fibular and posterior tibial artery (Figure 4).
This is a case reporting on the usefulness of interventional treatment by the direct stent puncture technique in a very complex lesion with long occlusive disease of the SFA, popliteal artery and below-the-knee arteries.
CLI is associated with high amputation and mortality rates, depending on concomitant risk factors and treatment options[8]. From a pathophysiologic point of view, ischemia of the limb is reversible, but causes irreversible tissue death, if left untreated. In patients presenting with CLI, current guidelines by the task force for the treatment of PAD recommend an “endovascular first” approach depending on the anatomy and complexity of the underlying lesions. However, with long occlusion of the SFA and popliteal artery bypass surgery should be considered due to rather poor technical success rates and high risk for re-occlusion, especially in segments with predicted poor patency rates in the distal downstream segments[7]. In our case, long femoro-popliteal occlusive disease was present along with occlusion of the proximal tibial posterior artery and total occlusion of the tibiofibular tract, of the fibular and the anterior tibial artery. Despite the complexity of the lesion, we chose an interventional approach due to failed bypass surgery and cardiac comorbidities. We used the direct stent puncture technique, which was previously described as an efficient and safe option for intraluminal stent recanalization in femoro-popliteal occlusive lesions[9,10], exhibiting high technical success rates and low rates of peri- and postprocedural complications, such as distal embolization and hematoma at the puncture site[11]. Like previously reported cases, we punctured an occluded stent in the mid SFA, facilitating retrograde recanalization. In contrast to most of the reported cases however, the lesion in our patient was more complex, as it did not end in the femoro-popliteal segment, but also involved the proximal and mid part of crural arteries. Thus, due lesion complexity and chronic renal disease, we decided to tackle the lesion in 2 sessions to minimize the risk for contrast induced nephropathy. Indeed, a high amount of contrast agent was necessary within the first recanalization session. Although the final angiographic results after the first session was not optimal due to remaining dissections in the SFA and poor outflow in the crural arteries, vasculature remained open during pharmacologic treatment with aspirin, clopidogrel and fondaparinux for 4 wk. During the second session, further treatment with drug coated balloons was possible, along with recanalization of a crural artery, leading to much better outflow to the foot. This case demonstrates that an “endovascular first” approach may be a valuable and ultimately successful even in very long, complex occlusive lesions, which may further shift treatment from surgical to endovascular treatment procedures in the future.
An 80-year-old female patient with peripheral artery disease (PAD) and long occlusion of the femoro-popliteal artery and below-the-knee arteries after failed bypass surgery, who presented with critical limb ischemia (CLI).
PAD with CLI (Rutherford Class 5).
Venous ulcer, neuropathic diabetic ulcer.
Laboratory markers showed increased inflammation due to the arterial ulcer. In addition, a reduced renal function with an estimated glomerular filtration rate of 36 mL/min per 1.73 m² was noticed.
PAD was diagnosed by duplex sonography and magnetic resonance angiography (MRA) and was confirmed by digital subtraction angiography (DSA).
PAD with CLI (Rutherford Class 5).
Endovascular strategy using percutaneous balloon angioplasty and without stent placement.
The direct stent puncture technique has been used for the recanalization of complex femoro-popliteal occlusive disease in cases were an antegrade recanalization is not successful. The lesion in the patient was more complex, as it did not end in the femoro-popliteal segment, but also involved the proximal and mid part of crural arteries.
CLI is a life-threatening condition due to advanced occlusive PAD, usually accompanied by ischemic rest pain, arterial ulcers and gangrene. If left untreated this condition will in major amputation, sepsis and death.
In patients with complex femoro-popliteal occlusive disease, the direct stent puncture technique may facilitate recanalization of very long occlusive lesions without the need of bypass surgery. An endovascular first approach needs to be considered in such patients, who usually are bad candidates for surgery due to cardiopulmonary disease and other comorbidities.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chello M, Najafi M, Teragawa H, Ueda H S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Gallino A, Aboyans V, Diehm C, Cosentino F, Stricker H, Falk E, Schouten O, Lekakis J, Amann-Vesti B, Siclari F. Non-coronary atherosclerosis. Eur Heart J. 2014;35:1112-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 120] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 2. | Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, Norman PE, Sampson UK, Williams LJ, Mensah GA. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382:1329-1340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2122] [Cited by in RCA: 2449] [Article Influence: 204.1] [Reference Citation Analysis (0)] |
| 3. | Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FG, Gillespie I, Ruckley CV, Raab GM; BASIL trial Participants. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: An intention-to-treat analysis of amputation-free and overall survival in patients randomized to a bypass surgery-first or a balloon angioplasty-first revascularization strategy. J Vasc Surg. 2010;51:5S-17S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 470] [Cited by in RCA: 402] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 4. | Zheng ZJ, Rosamond WD, Chambless LE, Nieto FJ, Barnes RW, Hutchinson RG, Tyroler HA, Heiss G; ARIC Investigators. Lower extremity arterial disease assessed by ankle-brachial index in a middle-aged population of African Americans and whites: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Prev Med. 2005;29:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Malyar N, Fürstenberg T, Wellmann J, Meyborg M, Lüders F, Gebauer K, Bunzemeier H, Roeder N, Reinecke H. Recent trends in morbidity and in-hospital outcomes of in-patients with peripheral arterial disease: a nationwide population-based analysis. Eur Heart J. 2013;34:2706-2714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 148] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 6. | European Stroke Organisation. Tendera M, Aboyans V, Bartelink ML, Baumgartner I, Clément D, Collet JP, Cremonesi A, De Carlo M, Erbel R, Fowkes FG, Heras M, Kownator S, Minar E, Ostergren J, Poldermans D, Riambau V, Roffi M, Röther J, Sievert H, van Sambeek M, Zeller T; ESC Committee for Practice Guidelines. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2851-2906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1042] [Cited by in RCA: 1067] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 7. | Lawall H, Huppert P, Espinola-Klein C, Zemmrich CS, Ruemenapf G. German guideline on the diagnosis and treatment of peripheral artery disease - a comprehensive update 2016. Vasa. 2017;46:79-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Golomb BA, Dang TT, Criqui MH. Peripheral arterial disease: morbidity and mortality implications. Circulation. 2006;114:688-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 383] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 9. | Gandini R, Del Giudice C, Assako Ondo EP, Spano S, Stefanini M, Simonetti G. Stent puncture for recanalization of occluded superficial femoral artery stents. J Endovasc Ther. 2012;19:30-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Manzi M, Palena LM, Brocco E. Clinical results using the direct stent puncture technique to treat SFA in-stent occlusion. J Endovasc Ther. 2012;19:461-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Palena LM, Manzi M. Direct stent puncture technique for intraluminal stent recanalization in the superficial femoral and popliteal arteries in-stent occlusion: outcomes from a prospective clinical analysis of diabetics with critical limb ischemia. Cardiovasc Revasc Med. 2013;14:203-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |