Published online Dec 26, 2017. doi: 10.4330/wjc.v9.i12.838
Peer-review started: September 21, 2017
First decision: October 23, 2017
Revised: November 20, 2017
Accepted: December 3, 2017
Article in press: December 3, 2017
Published online: December 26, 2017
Processing time: 92 Days and 11.2 Hours
We present a case of a patient who presented with chest pain, and on diagnostic coronary angiography appeared to have a grossly angulated yet significant coronary stenosis. This was proven to be an artefactual appearance on further assessment with intravascular ultrasound imaging. We describe the causes and associations of coronary tortuosity with other arteriopathy, and highlight challenges in the interpretation of tortuous vessels to accurately assess luminal narrowing and suitability for coronary intervention. We describe a case of artefactual coronary stenosis, and its thorough assessment with intravascular ultrasound. A literature review describes the pathogenesis of coronary tortuosity, and links with other cardiovascular disease. Readers will gain an understanding of the challenge in determining the severity of luminal stenosis based on coronary angiography alone in tortuous coronary anatomy, the use of intravascular ultrasound in this setting, and the allied vasculopathies of interest.
Core tip: Coronary arteries are inherently tortuous, and are assessed at angiography, compressing a 3D structure into a 2D picture. An overly tortuous artery may resemble true luminal stenosis, rather than mere angulation, and may be interpreted as a significant coronary stenosis. We present a remarkably angulated coronary artery, which appeared to bear a significant stenosis. On further assessment with pressure wire study and intravascular ultrasound we found there to be no significant lesion. We demonstrate an artefactual false-positive finding, and describe our clinical approach to avoid mistaking such a lesion for one that requires intervention, with a review of the literature.
- Citation: Edroos SA, Sayer JW. Artefactual angulated lesion on angiography: A case report and review of literature. World J Cardiol 2017; 9(12): 838-841
- URL: https://www.wjgnet.com/1949-8462/full/v9/i12/838.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i12.838
Coronary artery tortuosity poses many challenges in its assessment and further investigation. We present a case with ambiguous appearances at coronary angiography, clarified with intravascular imaging, and discuss the possible underpinning causes to consider when evaluating a tortuous epicardial artery.
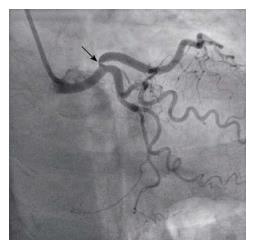
An 80-year-old Caucasian hypertensive patient presented with atypical chest discomfort that was present both at rest and on exercise. She had no cardiovascular risk factors. She was normotensive, with BP 126/72, and heart rate 70. Her ECG was normal. Transthoracic echocardiography demonstrated preserved left ventricular function. A coronary angiogram appeared to show a severe lesion in the proximal left anterior descending coronary artery, at its origin (Figure 1). She underwent a pressure wire study to this territory, to confirm its significance, with plans to carry out further intracoronary imaging to determine whether percutaneous intervention was feasible in view of the lesion’s ostial location and extreme angulation.
The pressure wire study was repeatedly negative, with instantaneous wave-free ratio of 0.97 and fractional flow reserve of 0.92 at maximal hyperaemia with systemic adenosine. Intravascular ultrasound demonstrated a normal calibre vessel throughout, with no significant atheroma seen (Video 1), contrary to the angiographic profile of the vessel.
Arteries are rarely straight, and a degree of curvature is inevitable from their path from the aorta to distal tissue beds. Angulation, or widespread coronary tortuosity, is often seen, though its relevance is dependent on the context in which it is found, with coexistant congenital diseases and the possibility of an artefactual appearance, as described here, complicating interpretation.
An inordinate degree of tortuosity has been observed in ageing, hypertension, diabetes mellitus and atherosclerosis, where it may be seen in all arterial vessels, from aorta to arteriole, and throughout the venous system. Arterial tortuosity may be quantified by a number of tortuosity indices, which in general assimilate the number of curvatures of an artery away from its overall direction of travel, measured in end-diastole. Though arterial curvature is usually benign, severe tortuosity may impede blood flow in coexistant atherosclerotic disease, embolus or systemic hypoperfusion predisposing to end organ ischaemia[1].
Degenerative arterial tortuosity is distinct from a group of inherited arteriopathies. Extreme arterial tortuosity has been seen in a number of congenital syndromes, including Loeys-Dietz syndrome, with genetic mutations of the transforming growth factor-β receptor, Marfan Syndrome, affecting fibrillin-1, and Arterial Tortuosity Syndrome, with mutation of the SLC2A10 gene. The underlying mechanism for the effects of these deletions is unclear. They manifest as gross, diffuse arterial sinuosity affecting coronary, great vessels, carotid and vertebral arteries, and are associated with cerebrovascular infarct or aneurysm, aortic dissection and adverse overall cardiovascular outcomes[2].
In a prospective study of coronary tortuosity in 1010 patients presenting for diagnostic coronary angiography, the incidence of epicardial coronary artery tortuosity appears to be higher in females, and its presence was correlated with hypertension yet negatively correlated with hyperlipidaemia, smoking and atherosclerosis. No significant difference was seen in major adverse cardiovascular events over a 4 year follow-up period between those with or without coronary tortuosity[3]. Conversely tortuous microvessels induce increased shear forces on blood transiting through its conduit, inducing platelet activation. This is thought to be thrombogenic, with higher mural thrombus and platelet activation seen in preclinical modelling of tortuous arterioles[4].
There appears to be an underlying genetic cause linking a continuum of arterial phenotypes from coronary tortuosity, via fibromuscular dysplasia and culminating in spontaneous coronary artery dissection (SCAD) with myocardial infarction. Patients with SCAD have been observed to have a high prevalence of coronary tortuosity, and this is higher still in those with recurrent SCAD. Fibromuscular dysplasia is associated with SCAD, with a recent report of SMAD3 gene deletion underpinning a presentation of SCAD[5-7].
Native tortuosity of an epicardial coronary artery may resemble a significant luminal stenosis when straightened through passage of a guidewire. The guidewire induces a linear shape upon a conduit that is normally curved, and there is invagination of the redundant tissue which impinges on the vessel lumen. This appearance disappears when the guidewire is retracted and the natural curvature of the vessel is restored, confirming an artefactual stenosis. This has been termed the “accordion effect”. The right coronary artery has scant surrounding tissue in the atrioventricular groove in comparison to the left coronary system, and is thought to be particularly prone to this appearance with instrumentation[8]. Our case demonstrates a normal vessel lumen that appears to resemble coronary stenosis on angiographic views due to its angulation.
We demonstrate the importance of intravascular imaging in excluding a significant atherosclerotic process. The use of intravascular ultrasound has previously been described as a gold standard test, above coronary angiography, in clarifying the course of a segment of ambiguous coronary anatomy and its relationship with other vessels[9]. However these measurements are reliant on the passage of a guidewire through a curved artery, and care must be taken in intracoronary measurements in tortuous vessels. Coronary tortuosity has recently been described as a potential cause of foreshortening of vessel length in Optical Coherence Tomography (OCT), and overestimation of vessel diameter by up to 12%, due an eccentric position of the OCT catheter in a nonlinear segment of vessel, and/or the straightening effect and movement of redundant tissues as seen with the accordion effect. This effect was minimised by using a floppy rather than a stiff guidewire in this OCT study[10].
We conclude that the appearances of severe coronary stenosis in this angulated and tortuous vessel is an artefactual appearance, which was proven to have neither arteriosclerosis nor significant intraluminal narrowing on further assessment. This case highlights the importance of multimodality assessment of tortuous vessels, where luminal stenosis may be overestimated by coronary angiography. The accordion effect at coronary angiography, and underestimation of vessel length with overestimation of vessel diameter at intracoronary imaging, require careful interpretation of data for correct diagnosis. The links between coronary tortuosity and other arteriopathies are currently the subject of investigation, with a possible underpinning genetic aetiology.
The patient described atypical exertional chest pain, with no prior cardiovascular risk factors.
Coronary angiography initially appeared to demonstrate a severe lesion in the proximal left anterior descending coronary artery, which was demonstrated to be a false positive finding in an angulated artery with no significant coronary stenosis, through further physiological and anatomical testing.
Further assessment of a lesion of this nature may be carried out using functional assessment, with a pressure wire study, or anatomical assessment, with intravascular ultrasound, as demonstrated here.
The authors used intravascular ultrasound to demonstrate a normal calibre of coronary artery. An alternative modality of optical coherence tomography may be used.
The above approach identified a false positive finding of possible coronary stenosis, which when ruled out prevented inappropriate treatment with a coronary artery stent.
The authors describe the aetiology of coronary angulation, which may be degenerative or heritable, and though epicardial tortuosity has not been shown to be associated with an increase in major adverse cardiovascular events an association with spontaneous coronary artery dissection, and the potential for misinterpretation of angulation as luminal stenosis, are important considerations when assessing lesions.
The authors learned the importance of multimodality assessment of apparent coronary lesions to justify, and subsequently rule out, the need for intervention in a case of marked coronary artery curvature, and present an approach to prevent mis-interpretation.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Schoenhagen P, Teragawa H S- Editor: Cui LJ L- Editor: A E- Editor: Lu YJ
| 1. | Langer HE, Birth U. Patient education in chronic polyarthritis. 3. Intermediate results of a prospective, controlled study of the effectiveness and side effects of patient seminars for polyarthritis patients. Z Rheumatol. 1988;47:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 318] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Myers RD, Veale WL, Yaksh TL. Preference for ethanol in the rhesus monkey following chronic infusion of ethanol into the cerebral ventricles. Physiol Behav. 1972;8:431-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Li Y, Shen C, Ji Y, Feng Y, Ma G, Liu N. Clinical implication of coronary tortuosity in patients with coronary artery disease. PLoS One. 2011;6:e24232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Scull SA, Dow MB, Athreya BH. Physical and occupational therapy for children with rheumatic diseases. Pediatr Clin North Am. 1986;33:1053-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Eleid MF, Guddeti RR, Tweet MS, Lerman A, Singh M, Best PJ, Vrtiska TJ, Prasad M, Rihal CS, Hayes SN. Coronary artery tortuosity in spontaneous coronary artery dissection: angiographic characteristics and clinical implications. Circ Cardiovasc Interv. 2014;7:656-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 227] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 6. | Garcia-Bermúdez M, Moustafa AH, Barrós-Membrilla A, Tizón-Marcos H. Repeated Loss of Consciousness in a Young Woman: A Suspicious SMAD3 Mutation Underlying Spontaneous Coronary Artery Dissection. Can J Cardiol. 2017;33:292.e1-292.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Henkin S, Negrotto SM, Tweet MS, Kirmani S, Deyle DR, Gulati R, Olson TM, Hayes SN. Spontaneous coronary artery dissection and its association with heritable connective tissue disorders. Heart. 2016;102:876-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 127] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 8. | Deligonul U, Tatineni S, Johnson R, Kern MJ. Accordion right coronary artery: an unusual complication of PTCA guidewire entrapment. Cathet Cardiovasc Diagn. 1991;23:111-113. [PubMed] |
| 9. | Baumgart D, Haude M, Birgelen Cv CV, Ge J, Görge G, Erbel R. Assessment of ambiguous coronary lesions by intravascular ultrasound. Int J Cardiovasc Intervent. 1999;2:3-12. [PubMed] |
| 10. | Danson EJ, Hansen P, Bhindi R. Wire bias in coronary measurement using optical coherence tomography. Cardiovasc Interv Ther. 2017; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |