Published online Sep 26, 2016. doi: 10.4330/wjc.v8.i9.520
Peer-review started: May 3, 2016
First decision: June 17, 2016
Revised: July 8, 2016
Accepted: July 20, 2016
Article in press: July 22, 2016
Published online: September 26, 2016
Processing time: 144 Days and 17 Hours
Myocardial infarction and sudden cardiac death are frequently the first manifestation of coronary artery disease. For this reason, screening of asymptomatic coronary atherosclerosis has become an attractive field of research in cardiovascular medicine. Necropsy studies have described histopathological changes associated with the development of acute coronary events. In this regard, thin-cap fibroatheroma has been identified as the main vulnerable coronary plaque feature. Hence, many imaging techniques, such as coronary computed tomography, cardiac magnetic resonance or positron emission tomography, have tried to detect noninvasively these histomorphological characteristics with different approaches. In this article, we review the role of these diagnostic tools in the detection of vulnerable coronary plaque with particular interest in their advantages and limitations as well as the clinical implications of the derived findings.
Core tip: Noninvasive diagnosis of vulnerable coronary plaque has become of major interest in preventive cardiology. Certain histological features have been related with an increased risk of plaque rupture. Coronary computed tomography has been largely used for this aim, and some lesion characteristics have been consistently associated with acute coronary syndrome in several studies. Moreover, a growing body of evidence suggests the potential role of cardiac magnetic resonance and positron emission tomography in high-risk lesion detection. These promising results should be put in perspective to select the high-risk population that may benefit the most from the use of coronary vulnerable plaque imaging screening.
- Citation: Pozo E, Agudo-Quilez P, Rojas-González A, Alvarado T, Olivera MJ, Jiménez-Borreguero LJ, Alfonso F. Noninvasive diagnosis of vulnerable coronary plaque. World J Cardiol 2016; 8(9): 520-533
- URL: https://www.wjgnet.com/1949-8462/full/v8/i9/520.htm
- DOI: https://dx.doi.org/10.4330/wjc.v8.i9.520
Atherosclerosis constitutes the leading cause of morbidity and mortality in the developed countries, mostly secondary to acute coronary syndromes (ACS)[1]. Moreover, the progressive aging of the population forecasts an exponential growth of the prevalence of cardiovascular disease[2]. In this clinical scenario, detection of patients at risk of suffering an ACS has become one of the major goals in cardiology. Traditional cardiovascular risk factors have been extensively used for this aim. Nevertheless, they fail to anticipate the occurrence of an ACS, especially in certain populations[3,4], so myocardial infarction and sudden cardiac death (SCD) are frequent first manifestations of coronary disease. This situation has boosted the interest in subclinical detection of atherosclerosis. In this regard, quantification of calcium score with coronary computed tomography (CCT)[5] as well as ultrasound evaluation of carotid atherosclerosis[6,7] have demonstrated their utility for cardiovascular risk reclassification[8,9]. In any case, in spite of a very common detection of coronary atherosclerosis in autopsy series among young adults[10] the incidence of ACS in this population is very low[1]. Thus, the onus should be shifted onto the detection of lesions that are prone to develop a coronary event.
Classical studies supported that ACS were caused mainly by lesions with severe stenosis[11]; however, PROSPECT trial[12], a prospective intravascular ultrasound (IVUS) and virtual histology (VH) follow-up of non-culprit lesions after ACS, revealed that most of the events are derived from angiographically mild stenosis (< 50%). Again autopsy studies have provided relevant information regarding the atherosclerotic plaque characteristics in culprit lesions. The most frequent presentation is plaque rupture, followed by plaque erosion[13]. Rarely (2%-7% of the cases) the ACS are related with a calcified nodule morphology[14]. These lesions are unfailingly associated with a variable amount of thrombus[15]. Given that plaque rupture is the most common substrate of acute coronary events, vulnerable plaques are defined as lesions at the greatest risk of rupture, with subsequent thrombosis or rapid stenosis progression (Table 1)[16]. Therefore, they are also named high-risk or thrombosis-prone plaques.
| Culprit lesion | Coronary lesion considered to be responsible for the clinical event, usually plaque complicated by intraluminal thrombosis |
| Thrombosed plaque | Plaque with an overlying thrombus extending into the vessel lumen either occlusive or non-occlusive |
| Eroded plaque | Thrombosed plaque (mainly fibrotic or proteoglycan-rich) due to loss or dysfunction of endothelial cells without associated rupture |
| Plaque with calcified nodule | Heavily calcified protruding plaque with loss or dysfunction of endothelial cells |
| Vulnerable, high-risk or thrombosis prone plaque | Plaque at increased risk of thrombosis and rapid stenosis progression TCFA: Inflamed plaque with a thin cap covering a lipid-rich necrotic core |
| Vulnerable patient | Patient at high-risk to experience a cardiovascular ischemic event due to a high atherosclerotic burden, high-risk plaques and/or thrombogenic blood |
When ruptured plaques leading to acute coronary events were studied in necropsies, they usually presented a large necrotic core with a thin overlying fibrous cap together with inflammatory cells and little calcification[17]. Moreover, unlike lesions related to stable disease, these plaques showed expansive or positive remodeling not causing significant narrowing of the coronary lumen[18]. Thus, plaques with these histomorphologic features but intact fibrous cap, named thin-cap fibroatheroma (TCFA), were assumed to be prone to rupture. This concept was evaluated in a detailed histologic analysis of atherosclerotic plaques from a large series of patients who suffered SCD[19]. This study established a relevance hierarchy of morphological features that may influence plaque rupture. In a general analysis a thin fibrous cap (< 84 μm) was able to exclude stable lesions. Interestingly, among TCFA with a cap thickness < 54 μm cross-section area stenosis was most likely < 74%. Finally, when fibrous cap thickness was not considered in the analysis, inflammation, characterized by macrophage plaque infiltration, as well as a large necrotic core emerged as typical features of potentially unstable lesions. In this regard, aforementioned PROSPECT trial[12] was able to confirm these findings in vivo with IVUS. In this study plaque burden ≥ 70%, minimal luminal area ≤ 4 mm2 and TCFA characteristics on VH were independently associated with subsequent major adverse cardiovascular events (MACE) derived from non-culprit lesions.
Some considerations should be kept in mind to understand the clinical relevance of vulnerable plaque detection. All the plaque ruptures do not inevitably cause an ACS[20], whereas disruption and healing is the typical mechanism of plaque stenosis growth[21,22]. Thus, a perfect storm scenario, with confluence of plaque vulnerability, inflammatory state, platelet activation and impaired fibrinolysis, is necessary for ACS occurrence[23]. However, given that substrate presence is a conditio sine qua non and the other involved factors (homeostasis disbalance and thrombogenicity) are difficult to establish and/or variable in time, noninvasive detection of vulnerable plaques may be clinically relevant[24], especially in very high risk patients[25].
Hence, in this paper we review the different noninvasive diagnostic tools to evaluate vulnerable coronary plaques, with a detailed description of the relevant information they provide as well as their particular strengths and limitations (Table 2). We focus specially on the technique with the greatest evidence in this field, CCT, mentioning other available imaging tools with promising perspective such as cardiac magnetic resonance (CMR) imaging and positron emission tomography (PET).
| CCT | CMR | PET | |
| Plaque characterization | Plaque morphology | Plaque morphology Tissue characterization of plaque | Inflammation (FDG) Macrophage infiltration (new tracers) |
| Vulnerable features | Positive remodeling Low attenuation Spotty calcification Napkin-ring sign | Positive remodeling T1 hyperintensity Late gadolinium enhancement | Increased tracer uptake |
| Clinical relevance | Strong association with ACS Prediction of slow-flow after PCI Evaluation of response to statins | Initial data of association of T1 hyperintense plaques with slow-flow, ACS and response to statins | Differentiation between ACS and stable coronary disease |
| Limitations | Radiation exposure Heavy calcification Overlap in attenuation ranges Inability to detect plaque erosion | Direct relation between spatial resolution and acquisition time Susceptibility to motion artifacts | Low spatial and temporal resolution Myocardial background uptake Expensive and limited availability |
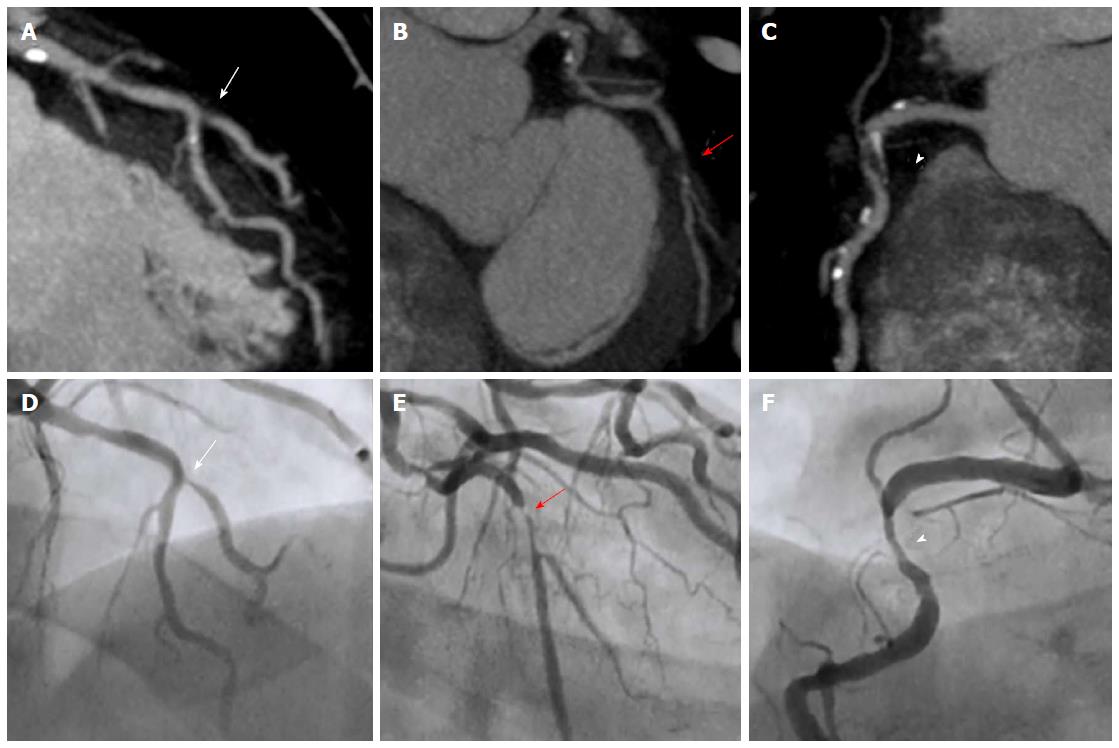
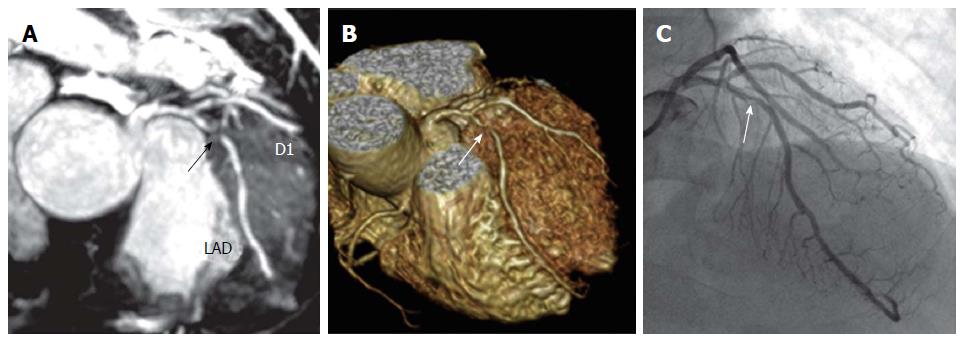
CCT not only provides information about the presence of significant stenoses with a high diagnostic accuracy[26] (Figure 1) but also allows a sensitive noninvasive direct evaluation of coronary atherosclerosis[27]. Coronary calcium score determination[28] as well as non-calcified plaque detection, even in the absence of significant stenosis[29-31], have demonstrated their value to predict MACE. Moreover, a large and systematic meta-analysis highlighted the relevance of luminal stenosis severity assessment with CCT[32], showing an increasing risk of the composite end-point of cardiac death or myocardial infarction for absence (0.04%), non-obstructive (1.29%) and obstructive (6.53%) coronary artery disease. It has shown a particular utility in chest pain evaluation at the emergency room[33]. There is also data supporting the capacity of CCT to evaluate coronary anatomy to determine the best revascularization strategy[34].
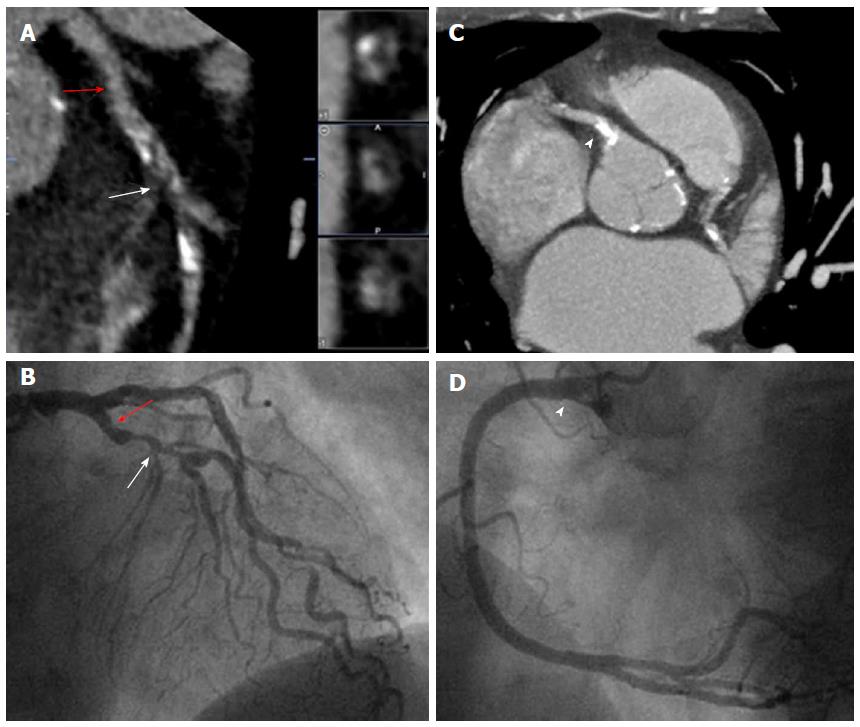
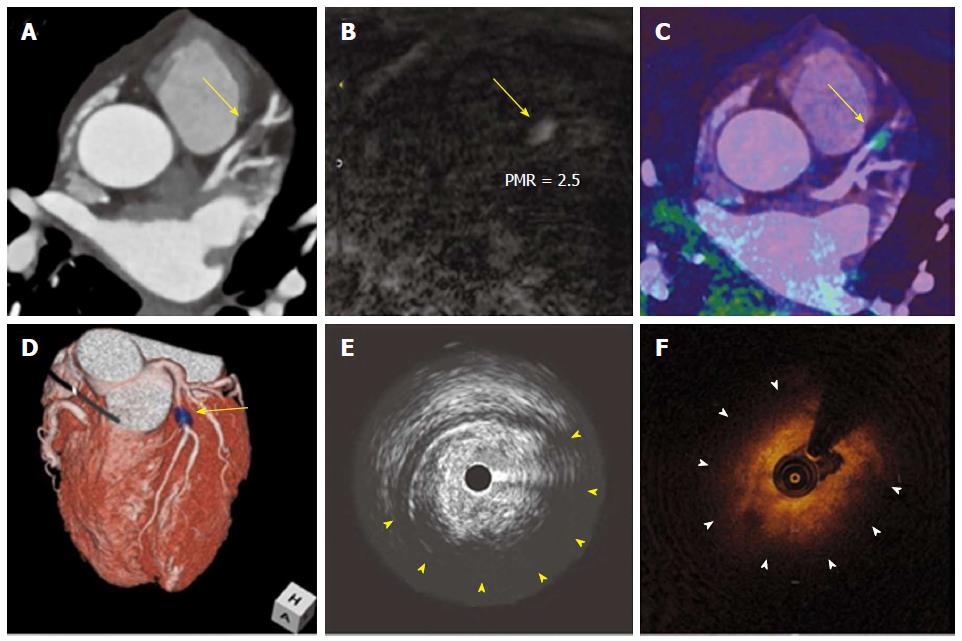
Certainly, the most relevant information is derived from the direct evaluation of coronary plaque with CCT. By consensus[35] the lesions are classified in 3 categories: Non-calcified, calcified and mixed plaques (Figure 2). In this regard, for a further assessment of CCT accuracy in coronary plaque qualitative analysis, head-to-head comparisons with VH have been performed. Pundziute et al[36] found a good correlation between both diagnostic tools in plaque characterization, with more fibrotic and fibro-fatty components in non-calcified plaque. Besides, the majority of TCFA in IVUS corresponded to mixed plaques in CCT. Hereof, Choi et al[37] established that plaques with > 10% necrotic core by VH showed significantly lower HU values in CCT. All the studies have shown a good agreement in non-calcified plaque quantification between both techniques[38-40]. However, there were contradictory results in plaque composition analysis using predefined Hounsfield unit (HU) ranges, due to overlapping in these values[38,40]. On the other hand, optical coherence tomography (OCT) has also been used as reference intravascular imaging technique. Kashiwagi et al[41] divided plaques in TCFA and non-TCFA according to OCT findings and studied the CCT plaque characteristics. Positive remodeling, lower attenuation values and ring-like enhancement (napkin-ring sign) on CCT were significantly more common in OCT-derived TCFA lesions. The later feature showed a good diagnostic accuracy for high-risk plaque detection and was independently associated with acute events. Moreover, napkin-ring sign has been independently associated with necrotic/lipid core area, non-core plaque area and total vessel area in post-mortem histopathological correlation[42]. However, although the presence of low attenuation and positive remodeling in CCT could identify rupture plaques in another study[43], they failed to differentiate plaque erosions leading to ACS from stable lesions. Lastly, CCT accuracy for plaque composition characterization was also evaluated with near-infrared spectroscopy (NIRS), showing a good correlation of plaque burden and non-calcified plaque area and density with cholesterol deposition in the coronary wall[27].
Thereby, even with first generation 16-rows scanners, culprit lesion characteristics could be evaluated in ACS[44]. When these lesions were compared with those in patients with stable angina, positive expansive remodeling, low attenuation (< 30 HU) non-calcified plaques and spotty calcification were detected more frequently (Figure 3). Furthermore, the combination of these three features increased the positive predictive value to 95%. These findings were corroborated with a prospective multimodal imaging protocol in acute coronary events[45]. Again lower radiological density with lower calcium score and larger remodeling index were more common in culprit lesions. Interestingly, these plaque characteristics were confirmed with IVUS and VH.
Beyond the classical tools for CCT analysis, there are new approaches with promising results in coronary plaque evaluation. Fujimoto et al[46] showed that the presence of delayed plaque enhancement in serial CCT acquisition was associated with high-risk plaque features. They hypothesized that this finding may be explained by plaque neovascularization and/or inflammation. In the same direction, a contrast agent formed by iodinated nanoparticles has been probed to detect macrophages in a preclinical model of atherosclerosis[47].
The hypothesis that aforementioned morphological patterns are able to identify thrombosis-prone plaques was evaluated in prospective studies. Motoyama et al[48] analyzed for the first time CCT plaque characteristics associated with the incidence of ACS in the follow-up. In this study, the presence of positive remodeling and/or low attenuation plaque was independently associated with ACS (HR = 22.8; P < 0.001) (Figure 3). Napkin-ring sign is another feature that has been associated with thrombosis-prone plaque. In a large series this sign was the strongest predictor of ACS among the vulnerable plaque characteristics[49]. On the other hand, a case-control study[50] demonstrated that when a semiautomated quantitative analysis of CCT was implemented, total and relative plaque volume and non-calcified plaque were significantly higher in patients who suffered an acute coronary event. This method of evaluation also had additive value to classical cardiovascular risk factors and conventional CCT reading for ACS prediction. Nevertheless, on top of the some methodological limitations[51], there is contradictory results in large prospective series. Among patients derived from ROMICAT II cohort[52], acute chest pain in emergency room, presence of a least one of high risk features (positive remodeling, low attenuation, spotty calcification and napkin-ring sign) was an independent predictor of ACS, even after adjustment by clinical risk factors and > 50% or > 70% stenosis[52]. Conversely, when stable patients were evaluated, plaque feature analysis, although improved predictive accuracy, did not significantly increase model discrimination index for acute coronary events[53]. Interestingly, the relevance of high-risk plaque detection on CCT was analyzed in another important cohort from a patient-based and lesion-based perspective[54]. In the former, vulnerable plaque was independently associated with prognosis. However, presence of high-risk features failed to predict ACS in a lesion-based analysis. Additionally, when serial CCT was available, plaque progression emerged as an independent predictor of events. Putting all these data in perspective, although vulnerable plaque CCT features may predict ACS the clinical relevance of these finding still needs to be clarify.
Influence of CCT plaque characteristics in percutaneous coronary interventions outcome was evaluated as well. The incidence of slow-flow phenomenon in patients with stable coronary disease was related with the presence of circumferential plaque calcification, a higher positive remodeling index and a lower plaque density in previous CCT[55]. In fact, circumferential plaque calcification showed the strongest independent association with this complication.
Finally, when CCT was used to evaluate the response to statin therapy[56] a greater decrease of total plaque volume, due to reduction in low attenuation plaque, was detected among patients under treatment, without differences in lumen volume and remodeling index changes between the groups. Thus, CCT may play a role in evaluation of the response to lipid-lowering drugs.
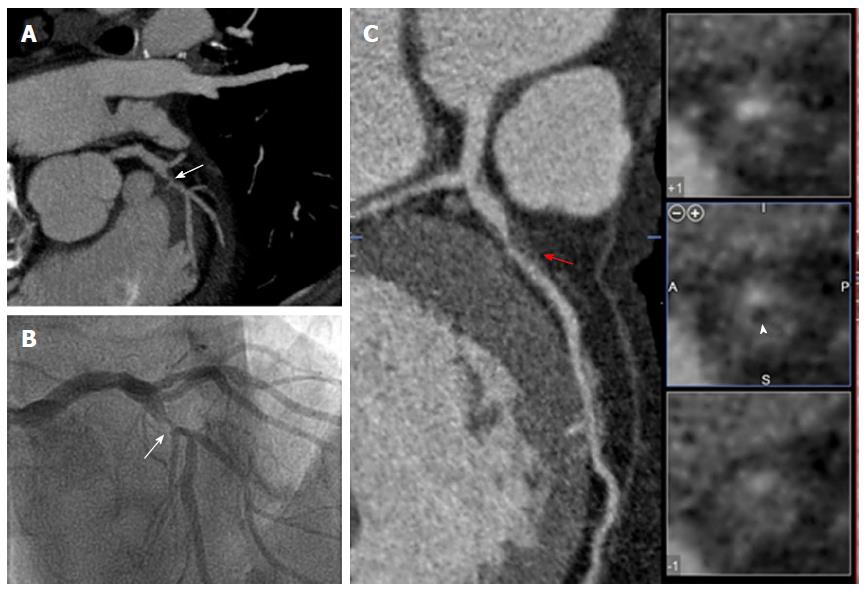
Despite the promising data, CCT is far from be free of limitations in vulnerable coronary plaque analysis. First, precise definition of plaque components is hampered by inherent limited spatial resolution of this imaging technique. Thus, results of non-calcified plaque quantification may be inconsistent[39,57]. Moreover, as previously mentioned, CCT plaque characterization is restricted by the overlap in radiological attenuation ranges for the different types of lesions[58,59] (Figure 4). In this regard, dual-source CCT, whose 2 different energies provide differing attenuation of materials, have shown to improve differentiation of necrotic core and fibrous plaque ex vivo[60]. Nevertheless, these results worsened when applied in vivo[38,60]. Thus, CCT acquisition technology needs to be refined to establish a generalizable HU-based categorization for accurate evaluation of components of the coronary plaque. Second, heavily calcified plaque may obscure detailed plaque evaluation due to partial volume effect. Finally, as previously mentioned, CCT has failed to detect plaque erosion[43], which constitutes the second more frequent presentation of culprit lesions[13].
CMR not only allows a precise ventricular volume quantification[61] and myocardial tissue characterization[62,63], but also is able to detect the presence of significant (> 50%) coronary atherosclerosis with similar accuracy than CCT[64,65] (Figure 5). In any case, in CMR spatial resolution is directly proportional to scan time. Thus, the necessary high resolution for coronary imaging carries an inherent increased susceptibility to motion artifacts[66]. The most effective measure to optimize image resolution without affecting artifact susceptibility is to reduce the field of view[67], which is difficult if a whole coronary tree analysis is pursued. Apart from that, several strategies have been implemented to avoid aforementioned limitation: Techniques to accelerate image acquisition[68,69], cardiac[70] and respiratory[71] motion compensation and new sampling methods[72,73]. However, even with the last technical advances a whole-heart coronary CMR angiography still takes at least 5 min[74,75], which limits its translation to clinical practice.
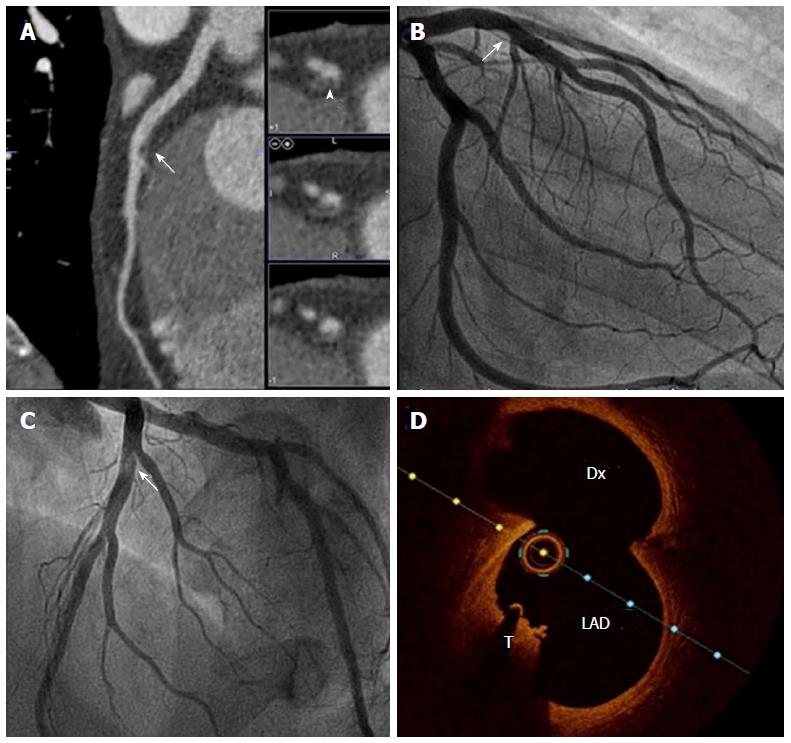
Although the aforementioned limitations make the acquisition challenging, non-contrast black-blood sequences have shown a good correlation with IVUS in luminal area and coronary plaque burden determination[76,77]. Interestingly, methemoglobin produced during clot maturation has the potential of shortening T1 relaxation time, which allows coronary thrombus detection with T1-weighted sequences[78,79]. The diagnostic accuracy of this noninvasive technique was proven to be high when it was evaluated against invasive coronary angiography[80] and OCT[81] (Figure 6). On the other hand, in a head-to-head comparison with CCT the presence of high intensity lesions on T1 sequences was associated with features of vulnerable plaque, such as positive remodeling, low attenuation and spotty calcification[82]. Moreover, this CMR finding was also associated with prognosis: Higher incidence of slow-flow phenomenon after percutaneous coronary intervention[82], coronary events during the follow-up[83], and regression of plaque in response to statin therapy[84]. Finally, T2-weighted sequences have demonstrated their ability to detect coronary vessel wall edema, in probable relation with plaque neovascularization, in initial studies[85,86].
Targeted as well as non-targeted contrast agents have been used to evaluate coronary arteries with CMR. When nonspecific gadolinium contrast is used, the presence of hyperenhancement has been linked to the severity of coronary atherosclerosis[79]. Additionally, a progressive reduction of coronary hyperenhancement has been noted in serial CMR after acute myocardial infarction[87]. Contrarily, many targeted contrast agents, directed to specific components of the plaque, are currently under investigation. Among them some have already reached positive data for coronary evaluation in large animals and/or humans: Fibrin-specific[88-90] and elastin-specific[91] contrast agents, gadofluorine[92,93], albumin-binding[94-96] contrast agent, and iron oxide-based[97] contrast. However, due to the growing field of molecular imaging a detailed discussion of these agents exceed the scope of this review.
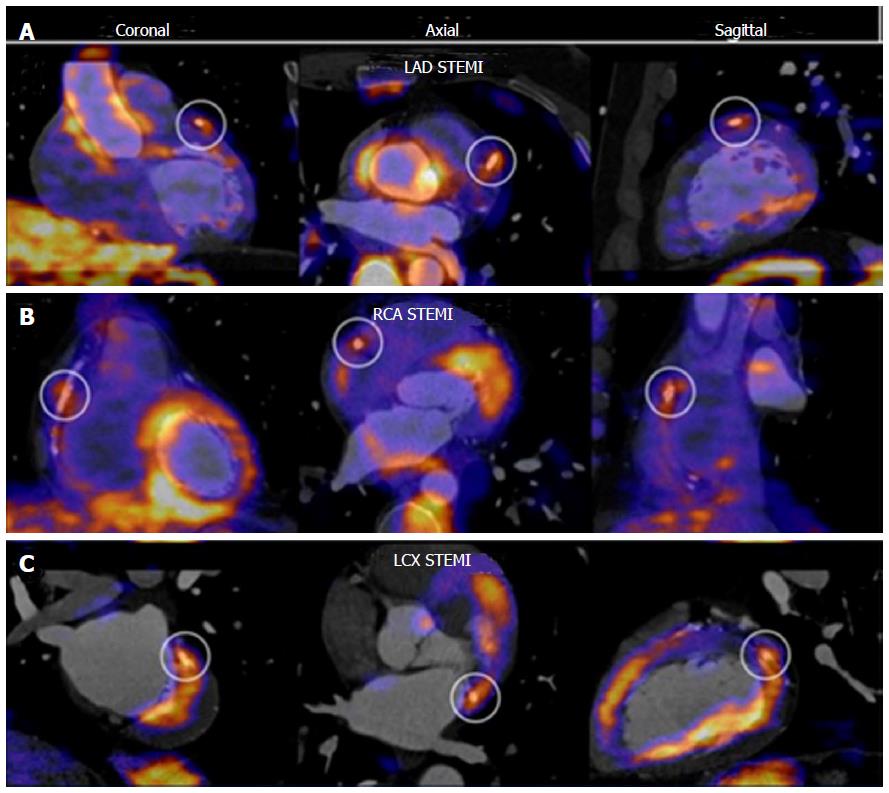
Besides the detailed morphological characterization provided by CCT and CMR, quantification of inflammation is a key feature in vulnerable coronary plaque evaluation. In this regard, nuclear imaging techniques have been extensively used for this purpose in atherosclerosis[98,99]. PET is the preferred tool, due to its superior spatial resolution over single photon emission tomography (SPECT), and is usually combined with computed tomography for a better anatomical definition. Fluorodeoxyglucose (FDG) is the most widely used tracer in this field. However, coronary evaluation is hampered by the significant myocardial uptake of FDG. To override this limitation, free fatty myocardial metabolism was favored with a low-carbohydrate high fat preparation[100]. This strategy was initially proven to detect coronary plaque inflammation[101]. Moreover, when coronary PET was evaluated in ACS as well as in stable angina after stent implantation, a higher FDG uptake was noted not only in the culprit lesions but also in the left main and ascending thoracic aorta of the patients with acute coronary events (Figure 7)[102]. This suggests the presence of spread arterial wall inflammation in the former group. Conversely, Dweck et al[103] demonstrated the ability of the new tracer 18F-sodium fluoride to detect coronary atherosclerosis without the limitation of myocardial metabolism artifact. Increased uptake was also associated with coronary calcium score, Framingham risk score, prior cardiovascular events and angina. Lastly, new tracers targeted against other markers of inflammation such as macrophage infiltration (11C-PK11195[104] and 68Ga-DOTATATE[105]) have been successfully tested.
Noninvasive imaging tools have shown their capacity to detect features related with vulnerable coronary plaque. CCT has been largely tested with this aim. Certain plaque characteristics, such as positive remodeling, low attenuation, spotty calcification and napkin-ring sign, have been systematically associated with ACS occurrence. Regarding CMR, results of plaque morphology characterization are similar than CCT but the inherent acquisition limitations hampered its extension to clinical practice. Moreover this technique allows tissue characterization of the coronary plaques through T1- and T2-weighted sequences and contrast-enhanced imaging. Finally, PET has emerged as a promising molecular imaging technique being able to detect coronary inflammation and even macrophage infiltration in vivo. In any case, given that the presence of vulnerable plaque features is not irredeemably linked to the occurrence of an ACS, larger studies are needed to clarify the patient subgroup that may benefit from non-invasive detection of high-risk plaques. This aspect is of special interest due to the large population that may be the target of a noninvasive imaging strategy for acute coronary events prevention. In this regard, cost-effectiveness should also be evaluated carefully in the future.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Dominguez-Rodriguez A, Kusmic C, Puddu PE, Siegel C S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ. Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report From the American Heart Association. Circulation. 2016;133:447-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1864] [Cited by in RCA: 1800] [Article Influence: 200.0] [Reference Citation Analysis (0)] |
| 2. | Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2162] [Cited by in RCA: 2282] [Article Influence: 163.0] [Reference Citation Analysis (0)] |
| 3. | Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak JF, Shea S, Sidney S, O'Leary DH, Chan C. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the coronary artery risk development in young adults study and multi-ethnic study of atherosclerosis. Circulation. 2009;119:382-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 257] [Cited by in RCA: 243] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 4. | Sibley C, Blumenthal RS, Merz CN, Mosca L. Limitations of current cardiovascular disease risk assessment strategies in women. J Womens Health (Larchmt). 2006;15:54-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Martin SS, Blaha MJ, Blankstein R, Agatston A, Rivera JJ, Virani SS, Ouyang P, Jones SR, Blumenthal RS, Budoff MJ. Dyslipidemia, coronary artery calcium, and incident atherosclerotic cardiovascular disease: implications for statin therapy from the multi-ethnic study of atherosclerosis. Circulation. 2014;129:77-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 190] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 6. | Baber U, Mehran R, Sartori S, Schoos MM, Sillesen H, Muntendam P, Garcia MJ, Gregson J, Pocock S, Falk E. Prevalence, impact, and predictive value of detecting subclinical coronary and carotid atherosclerosis in asymptomatic adults: the BioImage study. J Am Coll Cardiol. 2015;65:1065-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 355] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 7. | Sillesen H, Muntendam P, Adourian A, Entrekin R, Garcia M, Falk E, Fuster V. Carotid plaque burden as a measure of subclinical atherosclerosis: comparison with other tests for subclinical arterial disease in the High Risk Plaque BioImage study. JACC Cardiovasc Imaging. 2012;5:681-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 218] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 8. | Fernández-Friera L, Peñalvo JL, Fernández-Ortiz A, Ibañez B, López-Melgar B, Laclaustra M, Oliva B, Mocoroa A, Mendiguren J, Martínez de Vega V. Prevalence, Vascular Distribution, and Multiterritorial Extent of Subclinical Atherosclerosis in a Middle-Aged Cohort: The PESA (Progression of Early Subclinical Atherosclerosis) Study. Circulation. 2015;131:2104-2113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 383] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 9. | Naghavi M, Falk E, Hecht HS, Jamieson MJ, Kaul S, Berman D, Fayad Z, Budoff MJ, Rumberger J, Naqvi TZ. From vulnerable plaque to vulnerable patient--Part III: Executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006;98:2H-15H. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 378] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 10. | Nemetz PN, Roger VL, Ransom JE, Bailey KR, Edwards WD, Leibson CL. Recent trends in the prevalence of coronary disease: a population-based autopsy study of nonnatural deaths. Arch Intern Med. 2008;168:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Ellis S, Alderman E, Cain K, Fisher L, Sanders W, Bourassa M. Prediction of risk of anterior myocardial infarction by lesion severity and measurement method of stenoses in the left anterior descending coronary distribution: a CASS Registry Study. J Am Coll Cardiol. 1988;11:908-916. [PubMed] |
| 12. | Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J, Farhat N, Marso SP. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2252] [Cited by in RCA: 2426] [Article Influence: 173.3] [Reference Citation Analysis (0)] |
| 13. | Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000;20:1262-1275. [PubMed] |
| 14. | Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47:C13-C18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1646] [Cited by in RCA: 1719] [Article Influence: 90.5] [Reference Citation Analysis (0)] |
| 15. | Kramer MC, Rittersma SZ, de Winter RJ, Ladich ER, Fowler DR, Liang YH, Kutys R, Carter-Monroe N, Kolodgie FD, van der Wal AC. Relationship of thrombus healing to underlying plaque morphology in sudden coronary death. J Am Coll Cardiol. 2010;55:122-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 190] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 16. | Schaar JA, Muller JE, Falk E, Virmani R, Fuster V, Serruys PW, Colombo A, Stefanadis C, Ward Casscells S, Moreno PR. Terminology for high-risk and vulnerable coronary artery plaques. Report of a meeting on the vulnerable plaque, June 17 and 18, 2003, Santorini, Greece. Eur Heart J. 2004;25:1077-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 387] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 17. | Burke AP, Farb A, Malcom GT, Liang YH, Smialek J, Virmani R. Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. N Engl J Med. 1997;336:1276-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1244] [Cited by in RCA: 1175] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 18. | Schoenhagen P, Ziada KM, Kapadia SR, Crowe TD, Nissen SE, Tuzcu EM. Extent and direction of arterial remodeling in stable versus unstable coronary syndromes: an intravascular ultrasound study. Circulation. 2000;101:598-603. [PubMed] |
| 19. | Narula J, Nakano M, Virmani R, Kolodgie FD, Petersen R, Newcomb R, Malik S, Fuster V, Finn AV. Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J Am Coll Cardiol. 2013;61:1041-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 394] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 20. | Takano M, Inami S, Ishibashi F, Okamatsu K, Seimiya K, Ohba T, Sakai S, Mizuno K. Angioscopic follow-up study of coronary ruptured plaques in nonculprit lesions. J Am Coll Cardiol. 2005;45:652-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Burke AP, Kolodgie FD, Farb A, Weber DK, Malcom GT, Smialek J, Virmani R. Healed plaque ruptures and sudden coronary death: evidence that subclinical rupture has a role in plaque progression. Circulation. 2001;103:934-940. [PubMed] |
| 22. | Mann J, Davies MJ. Mechanisms of progression in native coronary artery disease: role of healed plaque disruption. Heart. 1999;82:265-268. [PubMed] |
| 23. | Arbab-Zadeh A, Nakano M, Virmani R, Fuster V. Acute coronary events. Circulation. 2012;125:1147-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 210] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 24. | Braunwald E. Noninvasive detection of vulnerable coronary plaques: Locking the barn door before the horse is stolen. J Am Coll Cardiol. 2009;54:58-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Braunwald E. Epilogue: what do clinicians expect from imagers? J Am Coll Cardiol. 2006;47:C101-C103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Mowatt G, Cook JA, Hillis GS, Walker S, Fraser C, Jia X, Waugh N. 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. Heart. 2008;94:1386-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 340] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 27. | Voros S, Rinehart S, Qian Z, Joshi P, Vazquez G, Fischer C, Belur P, Hulten E, Villines TC. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging. 2011;4:537-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 275] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 28. | Villines TC, Taylor AJ. Multi-ethnic study of atherosclerosis arterial age versus framingham 10-year or lifetime cardiovascular risk. Am J Cardiol. 2012;110:1627-1630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Lee MS, Chun EJ, Kim KJ, Kim JA, Yoo JY, Choi SI. Asymptomatic subjects with zero coronary calcium score: coronary CT angiographic features of plaques in event-prone patients. Int J Cardiovasc Imaging. 2013;29 Suppl 1:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Lin FY, Shaw LJ, Dunning AM, Labounty TM, Choi JH, Weinsaft JW, Koduru S, Gomez MJ, Delago AJ, Callister TQ. Mortality risk in symptomatic patients with nonobstructive coronary artery disease: a prospective 2-center study of 2,583 patients undergoing 64-detector row coronary computed tomographic angiography. J Am Coll Cardiol. 2011;58:510-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 177] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 31. | Yorgun H, Canpolat U, Aytemir K, Hazırolan T, Sunman H, Ateş AH, Sahiner L, Karahan S, Kaya EB, Tokgözoğlu L. Prognosis of patients with mild-moderate coronary artery stenosis detected by coronary computed tomography angiography. Int J Cardiol. 2013;168:1195-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Habib PJ, Green J, Butterfield RC, Kuntz GM, Murthy R, Kraemer DF, Percy RF, Miller AB, Strom JA. Association of cardiac events with coronary artery disease detected by 64-slice or greater coronary CT angiography: a systematic review and meta-analysis. Int J Cardiol. 2013;169:112-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Alfonso F, Salamanca J, Pozo E. Diagnóstico de síndrome coronario agudo en pacientes con dolor torácico en urgencias: ¿cambios a la vista? Emergencias. 2016;28:6-8. |
| 34. | Pozo E, Álvarez-Acosta L, Alonso D, Pazos-Lopez P, de Siqueira ME, Jacobi A, Narula J, Fuster V, Sanz J. Diagnostic accuracy of coronary ct for the quantification of the syntax score in patients with left main and/or 3-vessel coronary disease. Comparison with invasive angiography. Int J Cardiol. 2015;182:549-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Wu FZ, Wu MT. 2014 SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2015;9:e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 36. | Pundziute G, Schuijf JD, Jukema JW, Decramer I, Sarno G, Vanhoenacker PK, Reiber JH, Schalij MJ, Wijns W, Bax JJ. Head-to-head comparison of coronary plaque evaluation between multislice computed tomography and intravascular ultrasound radiofrequency data analysis. JACC Cardiovasc Interv. 2008;1:176-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 121] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 37. | Choi BJ, Kang DK, Tahk SJ, Choi SY, Yoon MH, Lim HS, Kang SJ, Yang HM, Park JS, Zheng M. Comparison of 64-slice multidetector computed tomography with spectral analysis of intravascular ultrasound backscatter signals for characterizations of noncalcified coronary arterial plaques. Am J Cardiol. 2008;102:988-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | Brodoefel H, Burgstahler C, Heuschmid M, Reimann A, Khosa F, Kopp A, Schroeder S, Claussen CD, Clouse ME. Accuracy of dual-source CT in the characterisation of non-calcified plaque: use of a colour-coded analysis compared with virtual histology intravascular ultrasound. Br J Radiol. 2009;82:805-812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 39. | Otsuka M, Bruining N, Van Pelt NC, Mollet NR, Ligthart JM, Vourvouri E, Hamers R, De Jaegere P, Wijns W, Van Domburg RT. Quantification of coronary plaque by 64-slice computed tomography: a comparison with quantitative intracoronary ultrasound. Invest Radiol. 2008;43:314-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 40. | Voros S, Rinehart S, Qian Z, Vazquez G, Anderson H, Murrieta L, Wilmer C, Carlson H, Taylor K, Ballard W. Prospective validation of standardized, 3-dimensional, quantitative coronary computed tomographic plaque measurements using radiofrequency backscatter intravascular ultrasound as reference standard in intermediate coronary arterial lesions: results from the ATLANTA (assessment of tissue characteristics, lesion morphology, and hemodynamics by angiography with fractional flow reserve, intravascular ultrasound and virtual histology, and noninvasive computed tomography in atherosclerotic plaques) I study. JACC Cardiovasc Interv. 2011;4:198-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 156] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 41. | Kashiwagi M, Tanaka A, Kitabata H, Tsujioka H, Kataiwa H, Komukai K, Tanimoto T, Takemoto K, Takarada S, Kubo T. Feasibility of noninvasive assessment of thin-cap fibroatheroma by multidetector computed tomography. JACC Cardiovasc Imaging. 2009;2:1412-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 186] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 42. | Seifarth H, Schlett CL, Nakano M, Otsuka F, Károlyi M, Liew G, Maurovich-Horvat P, Alkadhi H, Virmani R, Hoffmann U. Histopathological correlates of the napkin-ring sign plaque in coronary CT angiography. Atherosclerosis. 2012;224:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 43. | Ozaki Y, Okumura M, Ismail TF, Motoyama S, Naruse H, Hattori K, Kawai H, Sarai M, Takagi Y, Ishii J. Coronary CT angiographic characteristics of culprit lesions in acute coronary syndromes not related to plaque rupture as defined by optical coherence tomography and angioscopy. Eur Heart J. 2011;32:2814-2823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 44. | Motoyama S, Kondo T, Sarai M, Sugiura A, Harigaya H, Sato T, Inoue K, Okumura M, Ishii J, Anno H. Multislice computed tomographic characteristics of coronary lesions in acute coronary syndromes. J Am Coll Cardiol. 2007;50:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 772] [Cited by in RCA: 784] [Article Influence: 43.6] [Reference Citation Analysis (0)] |
| 45. | Hernando L, Corros C, Gonzalo N, Hernández-Antolin R, Bañuelos C, Jiménez-Quevedo P, Bernardo E, Fernández-Ortiz A, Escaned J, Macaya C. Morphological characteristics of culprit coronary lesions according to clinical presentation: insights from a multimodality imaging approach. Int J Cardiovasc Imaging. 2013;29:13-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | Fujimoto S, Kondo T, Kodama T, Takase S, Narula J. Delayed plaque enhancement by CT angiography. JACC Cardiovasc Imaging. 2012;5:1181-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | Hyafil F, Cornily JC, Feig JE, Gordon R, Vucic E, Amirbekian V, Fisher EA, Fuster V, Feldman LJ, Fayad ZA. Noninvasive detection of macrophages using a nanoparticulate contrast agent for computed tomography. Nat Med. 2007;13:636-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 341] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 48. | Motoyama S, Sarai M, Harigaya H, Anno H, Inoue K, Hara T, Naruse H, Ishii J, Hishida H, Wong ND. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54:49-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1024] [Cited by in RCA: 1079] [Article Influence: 67.4] [Reference Citation Analysis (0)] |
| 49. | Otsuka K, Fukuda S, Tanaka A, Nakanishi K, Taguchi H, Yoshikawa J, Shimada K, Yoshiyama M. Napkin-ring sign on coronary CT angiography for the prediction of acute coronary syndrome. JACC Cardiovasc Imaging. 2013;6:448-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 264] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 50. | Versteylen MO, Kietselaer BL, Dagnelie PC, Joosen IA, Dedic A, Raaijmakers RH, Wildberger JE, Nieman K, Crijns HJ, Niessen WJ. Additive value of semiautomated quantification of coronary artery disease using cardiac computed tomographic angiography to predict future acute coronary syndrome. J Am Coll Cardiol. 2013;61:2296-2305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 158] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 51. | Alfonso F. Noninvasive detection of vulnerable plaques: are we there yet? J Am Coll Cardiol. 2010;55:1163; author reply 1163-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 52. | Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, Pope JH, Hauser TH, White CS, Weiner SG. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 645] [Cited by in RCA: 654] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 53. | Fujimoto S, Kondo T, Takamura K, Baber U, Shinozaki T, Nishizaki Y, Kawaguchi Y, Matsumori R, Hiki M, Miyauchi K. Incremental prognostic value of coronary computed tomographic angiography high-risk plaque characteristics in newly symptomatic patients. J Cardiol. 2016;67:538-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 54. | Motoyama S, Ito H, Sarai M, Kondo T, Kawai H, Nagahara Y, Harigaya H, Kan S, Anno H, Takahashi H. Plaque Characterization by Coronary Computed Tomography Angiography and the Likelihood of Acute Coronary Events in Mid-Term Follow-Up. J Am Coll Cardiol. 2015;66:337-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 490] [Cited by in RCA: 645] [Article Influence: 64.5] [Reference Citation Analysis (0)] |
| 55. | Kodama T, Kondo T, Oida A, Fujimoto S, Narula J. Computed tomographic angiography-verified plaque characteristics and slow-flow phenomenon during percutaneous coronary intervention. JACC Cardiovasc Interv. 2012;5:636-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 56. | Inoue K, Motoyama S, Sarai M, Sato T, Harigaya H, Hara T, Sanda Y, Anno H, Kondo T, Wong ND. Serial coronary CT angiography-verified changes in plaque characteristics as an end point: evaluation of effect of statin intervention. JACC Cardiovasc Imaging. 2010;3:691-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 156] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 57. | Brodoefel H, Reimann A, Heuschmid M, Tsiflikas I, Kopp AF, Schroeder S, Claussen CD, Clouse ME, Burgstahler C. Characterization of coronary atherosclerosis by dual-source computed tomography and HU-based color mapping: a pilot study. Eur Radiol. 2008;18:2466-2474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 58. | Hur J, Kim YJ, Lee HJ, Nam JE, Choe KO, Seo JS, Choi DH, Kim JS, Choi BW. Quantification and characterization of obstructive coronary plaques using 64-slice computed tomography: a comparison with intravascular ultrasound. J Comput Assist Tomogr. 2009;33:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 59. | Sun J, Zhang Z, Lu B, Yu W, Yang Y, Zhou Y, Wang Y, Fan Z. Identification and quantification of coronary atherosclerotic plaques: a comparison of 64-MDCT and intravascular ultrasound. AJR Am J Roentgenol. 2008;190:748-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 141] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 60. | Obaid DR, Calvert PA, Gopalan D, Parker RA, West NE, Goddard M, Rudd JH, Bennett MR. Dual-energy computed tomography imaging to determine atherosclerotic plaque composition: a prospective study with tissue validation. J Cardiovasc Comput Tomogr. 2014;8:230-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 61. | Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC, Gerstad NA, Gillam LD, Hodgson JM, Kim RJ. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol. 2006;48:1475-1497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1092] [Cited by in RCA: 948] [Article Influence: 49.9] [Reference Citation Analysis (0)] |
| 62. | Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005;26:1461-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 616] [Cited by in RCA: 620] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 63. | Sharma V, Binukrishnan S, Schoepf UJ, Ruzsics B. Myocardial tissue characterization with magnetic resonance imaging. J Thorac Imaging. 2014;29:318-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 64. | Hamdan A, Asbach P, Wellnhofer E, Klein C, Gebker R, Kelle S, Kilian H, Huppertz A, Fleck E. A prospective study for comparison of MR and CT imaging for detection of coronary artery stenosis. JACC Cardiovasc Imaging. 2011;4:50-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 65. | Yang Q, Li K, Liu X, Bi X, Liu Z, An J, Zhang A, Jerecic R, Li D. Contrast-enhanced whole-heart coronary magnetic resonance angiography at 3.0-T: a comparative study with X-ray angiography in a single center. J Am Coll Cardiol. 2009;54:69-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 130] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 66. | Scott AD, Keegan J, Firmin DN. Motion in cardiovascular MR imaging. Radiology. 2009;250:331-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 121] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 67. | Stuber M, Botnar RM, Danias PG, Sodickson DK, Kissinger KV, Van Cauteren M, De Becker J, Manning WJ. Double-oblique free-breathing high resolution three-dimensional coronary magnetic resonance angiography. J Am Coll Cardiol. 1999;34:524-531. [PubMed] |
| 68. | Lustig M, Donoho D, Pauly JM. Sparse MRI: The application of compressed sensing for rapid MR imaging. Magn Reson Med. 2007;58:1182-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4286] [Cited by in RCA: 3173] [Article Influence: 186.6] [Reference Citation Analysis (0)] |
| 69. | Pruessmann KP, Weiger M, Scheidegger MB, Boesiger P. SENSE: sensitivity encoding for fast MRI. Magn Reson Med. 1999;42:952-962. [PubMed] |
| 70. | Fischer SE, Wickline SA, Lorenz CH. Novel real-time R-wave detection algorithm based on the vectorcardiogram for accurate gated magnetic resonance acquisitions. Magn Reson Med. 1999;42:361-370. [PubMed] |
| 71. | Henningsson M, Koken P, Stehning C, Razavi R, Prieto C, Botnar RM. Whole-heart coronary MR angiography with 2D self-navigated image reconstruction. Magn Reson Med. 2012;67:437-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 134] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 72. | Meyer CH, Hu BS, Nishimura DG, Macovski A. Fast spiral coronary artery imaging. Magn Reson Med. 1992;28:202-213. [PubMed] |
| 73. | Stehning C, Börnert P, Nehrke K, Eggers H, Stuber M. Free-breathing whole-heart coronary MRA with 3D radial SSFP and self-navigated image reconstruction. Magn Reson Med. 2005;54:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 184] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 74. | Hu P, Chan J, Ngo LH, Smink J, Goddu B, Kissinger KV, Goepfert L, Hauser TH, Rofsky NM, Manning WJ. Contrast-enhanced whole-heart coronary MRI with bolus infusion of gadobenate dimeglumine at 1.5 T. Magn Reson Med. 2011;65:392-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 75. | Nagata M, Kato S, Kitagawa K, Ishida N, Nakajima H, Nakamori S, Ishida M, Miyahara M, Ito M, Sakuma H. Diagnostic accuracy of 1.5-T unenhanced whole-heart coronary MR angiography performed with 32-channel cardiac coils: initial single-center experience. Radiology. 2011;259:384-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 76. | Gerretsen S, Kessels AG, Nelemans PJ, Dijkstra J, Reiber JH, van der Geest RJ, Katoh M, Waltenberger J, van Engelshoven JM, Botnar RM. Detection of coronary plaques using MR coronary vessel wall imaging: validation of findings with intravascular ultrasound. Eur Radiol. 2013;23:115-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 77. | He Y, Zhang Z, Dai Q, Zhou Y, Yang Y, Yu W, An J, Jin L, Jerecic R, Yuan C. Accuracy of MRI to identify the coronary artery plaque: a comparative study with intravascular ultrasound. J Magn Reson Imaging. 2012;35:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 78. | Botnar RM. Coronary plaque characterization by T(1)-weighted cardiac magnetic resonance. JACC Cardiovasc Imaging. 2009;2:729-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 79. | Yeon SB, Sabir A, Clouse M, Martinezclark PO, Peters DC, Hauser TH, Gibson CM, Nezafat R, Maintz D, Manning WJ. Delayed-enhancement cardiovascular magnetic resonance coronary artery wall imaging: comparison with multislice computed tomography and quantitative coronary angiography. J Am Coll Cardiol. 2007;50:441-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 81] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 80. | Jansen CH, Perera D, Makowski MR, Wiethoff AJ, Phinikaridou A, Razavi RM, Marber MS, Greil GF, Nagel E, Maintz D. Detection of intracoronary thrombus by magnetic resonance imaging in patients with acute myocardial infarction. Circulation. 2011;124:416-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 81. | Ehara S, Hasegawa T, Nakata S, Matsumoto K, Nishimura S, Iguchi T, Kataoka T, Yoshikawa J, Yoshiyama M. Hyperintense plaque identified by magnetic resonance imaging relates to intracoronary thrombus as detected by optical coherence tomography in patients with angina pectoris. Eur Heart J Cardiovasc Imaging. 2012;13:394-399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 82. | Kawasaki T, Koga S, Koga N, Noguchi T, Tanaka H, Koga H, Serikawa T, Orita Y, Ikeda S, Mito T. Characterization of hyperintense plaque with noncontrast T(1)-weighted cardiac magnetic resonance coronary plaque imaging: comparison with multislice computed tomography and intravascular ultrasound. JACC Cardiovasc Imaging. 2009;2:720-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 83. | Noguchi T, Kawasaki T, Tanaka A, Yasuda S, Goto Y, Ishihara M, Nishimura K, Miyamoto Y, Node K, Koga N. High-intensity signals in coronary plaques on noncontrast T1-weighted magnetic resonance imaging as a novel determinant of coronary events. J Am Coll Cardiol. 2014;63:989-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 138] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 84. | Noguchi T, Tanaka A, Kawasaki T, Goto Y, Morita Y, Asaumi Y, Nakao K, Fujiwara R, Nishimura K, Miyamoto Y. Effect of Intensive Statin Therapy on Coronary High-Intensity Plaques Detected by Noncontrast T1-Weighted Imaging: The AQUAMARINE Pilot Study. J Am Coll Cardiol. 2015;66:245-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 85. | Kim WY, Christiansen EH, Thrysøe SA, Al-Mashhadi RH, Bøtker HE, Bøttcher M, Holm NR, Falk E. First in vivo demonstration of coronary edema in culprit lesion of patient with acute coronary syndrome by cardiovascular magnetic resonance. Circ Cardiovasc Imaging. 2011;4:344-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 86. | Pedersen SF, Thrysøe SA, Paaske WP, Thim T, Falk E, Ringgaard S, Kim WY. Determination of edema in porcine coronary arteries by T2 weighted cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2011;13:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 87. | Ibrahim T, Makowski MR, Jankauskas A, Maintz D, Karch M, Schachoff S, Manning WJ, Schömig A, Schwaiger M, Botnar RM. Serial contrast-enhanced cardiac magnetic resonance imaging demonstrates regression of hyperenhancement within the coronary artery wall in patients after acute myocardial infarction. JACC Cardiovasc Imaging. 2009;2:580-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 88. | Botnar RM, Perez AS, Witte S, Wiethoff AJ, Laredo J, Hamilton J, Quist W, Parsons EC, Vaidya A, Kolodziej A. In vivo molecular imaging of acute and subacute thrombosis using a fibrin-binding magnetic resonance imaging contrast agent. Circulation. 2004;109:2023-2029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 199] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 89. | Flacke S, Fischer S, Scott MJ, Fuhrhop RJ, Allen JS, McLean M, Winter P, Sicard GA, Gaffney PJ, Wickline SA. Novel MRI contrast agent for molecular imaging of fibrin: implications for detecting vulnerable plaques. Circulation. 2001;104:1280-1285. [PubMed] |
| 90. | Spuentrup E, Botnar RM, Wiethoff AJ, Ibrahim T, Kelle S, Katoh M, Ozgun M, Nagel E, Vymazal J, Graham PB. MR imaging of thrombi using EP-2104R, a fibrin-specific contrast agent: initial results in patients. Eur Radiol. 2008;18:1995-2005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 122] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 91. | Makowski MR, Wiethoff AJ, Blume U, Cuello F, Warley A, Jansen CH, Nagel E, Razavi R, Onthank DC, Cesati RR. Assessment of atherosclerotic plaque burden with an elastin-specific magnetic resonance contrast agent. Nat Med. 2011;17:383-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 92. | Sirol M, Itskovich VV, Mani V, Aguinaldo JG, Fallon JT, Misselwitz B, Weinmann HJ, Fuster V, Toussaint JF, Fayad ZA. Lipid-rich atherosclerotic plaques detected by gadofluorine-enhanced in vivo magnetic resonance imaging. Circulation. 2004;109:2890-2896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 147] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 93. | Ronald JA, Chen Y, Belisle AJ, Hamilton AM, Rogers KA, Hegele RA, Misselwitz B, Rutt BK. Comparison of gadofluorine-M and Gd-DTPA for noninvasive staging of atherosclerotic plaque stability using MRI. Circ Cardiovasc Imaging. 2009;2:226-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 94. | Lobbes MB, Heeneman S, Passos VL, Welten R, Kwee RM, van der Geest RJ, Wiethoff AJ, Caravan P, Misselwitz B, Daemen MJ. Gadofosveset-enhanced magnetic resonance imaging of human carotid atherosclerotic plaques: a proof-of-concept study. Invest Radiol. 2010;45:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 95. | Pedersen SF, Thrysøe SA, Paaske WP, Thim T, Falk E, Ringgaard S, Kim WY. CMR assessment of endothelial damage and angiogenesis in porcine coronary arteries using gadofosveset. J Cardiovasc Magn Reson. 2011;13:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 96. | Phinikaridou A, Andia ME, Protti A, Indermuehle A, Shah A, Smith A, Warley A, Botnar RM. Noninvasive magnetic resonance imaging evaluation of endothelial permeability in murine atherosclerosis using an albumin-binding contrast agent. Circulation. 2012;126:707-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 97. | Alam SR, Shah AS, Richards J, Lang NN, Barnes G, Joshi N, MacGillivray T, McKillop G, Mirsadraee S, Payne J. Ultrasmall superparamagnetic particles of iron oxide in patients with acute myocardial infarction: early clinical experience. Circ Cardiovasc Imaging. 2012;5:559-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 123] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 98. | Rudd JH, Hyafil F, Fayad ZA. Inflammation imaging in atherosclerosis. Arterioscler Thromb Vasc Biol. 2009;29:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 99. | Sanz J, Fayad ZA. Imaging of atherosclerotic cardiovascular disease. Nature. 2008;451:953-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 402] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 100. | Wykrzykowska J, Lehman S, Williams G, Parker JA, Palmer MR, Varkey S, Kolodny G, Laham R. Imaging of inflamed and vulnerable plaque in coronary arteries with 18F-FDG PET/CT in patients with suppression of myocardial uptake using a low-carbohydrate, high-fat preparation. J Nucl Med. 2009;50:563-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 203] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 101. | Alexanderson E, Slomka P, Cheng V, Meave A, Saldaña Y, García-Rojas L, Berman D. Fusion of positron emission tomography and coronary computed tomographic angiography identifies fluorine 18 fluorodeoxyglucose uptake in the left main coronary artery soft plaque. J Nucl Cardiol. 2008;15:841-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 102. | Rogers IS, Nasir K, Figueroa AL, Cury RC, Hoffmann U, Vermylen DA, Brady TJ, Tawakol A. Feasibility of FDG imaging of the coronary arteries: comparison between acute coronary syndrome and stable angina. JACC Cardiovasc Imaging. 2010;3:388-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 243] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 103. | Dweck MR, Chow MW, Joshi NV, Williams MC, Jones C, Fletcher AM, Richardson H, White A, McKillop G, van Beek EJ. Coronary arterial 18F-sodium fluoride uptake: a novel marker of plaque biology. J Am Coll Cardiol. 2012;59:1539-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 390] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 104. | Gaemperli O, Shalhoub J, Owen DR, Lamare F, Johansson S, Fouladi N, Davies AH, Rimoldi OE, Camici PG. Imaging intraplaque inflammation in carotid atherosclerosis with 11C-PK11195 positron emission tomography/computed tomography. Eur Heart J. 2012;33:1902-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 193] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 105. | Rominger A, Saam T, Vogl E, Ubleis C, la Fougère C, Förster S, Haug A, Cumming P, Reiser MF, Nikolaou K. In vivo imaging of macrophage activity in the coronary arteries using 68Ga-DOTATATE PET/CT: correlation with coronary calcium burden and risk factors. J Nucl Med. 2010;51:193-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 106. | Asaumi Y, Noguchi T, Morita Y, Matsuyama TA, Otsuka F, Fujiwara R, Kanaya T, Nagai T, Higashi M, Kusano K. Non-contrast T1-weighted magnetic resonance imaging at 3.0 Tesla in a patient undergoing elective percutaneous coronary intervention – clinical and pathological significance of high-intensity plaque. Circ J. 2015;79:218-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 107. | Cheng VY, Slomka PJ, Le Meunier L, Tamarappoo BK, Nakazato R, Dey D, Berman DS. Coronary arterial 18F-FDG uptake by fusion of PET and coronary CT angiography at sites of percutaneous stenting for acute myocardial infarction and stable coronary artery disease. J Nucl Med. 2012;53:575-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |