Published online Nov 26, 2016. doi: 10.4330/wjc.v8.i11.684
Peer-review started: June 24, 2016
First decision: July 11, 2016
Revised: August 11, 2016
Accepted: September 21, 2016
Article in press: September 22, 2016
Published online: November 26, 2016
Processing time: 156 Days and 7.5 Hours
Pulmonary vein thrombosis (PVT) is a rarely encountered disease entity with varied clinical presentations. It is usually associated with lung carcinoma, lung surgeries and as a complication of the radiofrequency catheter ablation procedure for atrial fibrillation. Its clinical manifestations can vary from mild hemoptysis to lung infarction with hemodynamic compromise. A 76-year-old male presented with a 2-d history of pleuritic left sided chest pain. His past medical history included polycythemia vera, atrial fibrillation, coronary artery disease, pulmonary embolism and pulmonary hypertension. Chest radiograph was normal, troponins were normal and the 12-lead electrocardiogram did not show any ischemic changes. A computerized tomography pulmonary angiogram revealed a filling defect in the left lower lobe pulmonary vein. He was treated with subcutaneous enoxaparin and his symptoms improved. This case highlights a rare etiology of chest pain and the first reported case of the association of polycythemia vera and pulmonary vein thrombosis. A high index of suspicion is required for appropriate diagnostic work up. PVT can mimic pulmonary embolism. The diagnostic work up and treatment strategies depend on acuity of presentation.
Core tip: Pulmonary vein thrombosis (PVT) is a rare but potentially life-threatening disease entity. Its signs and symptoms are often non-specific and it can be difficult to diagnose unless there is a high index of clinical suspicion. Misdiagnosis can lead to grave consequences. We describe a case of PVT in the setting of polycythemia vera. The patient had presented with symptoms of pleuritic chest pain and the workup revealed a thrombus in the left inferior pulmonary vein. This association of polycythemia vera with PVT has not been reported in the literature previously. The PVT is a less known disease process and with this manuscript, we would like to briefly review its causes, presentation and treatment options.
- Citation: Bhardwaj B, Jacob D, Sharma A, Ghanimeh MA, Baweja P. Pulmonary vein thrombosis in a patient with polycythemia vera. World J Cardiol 2016; 8(11): 684-688
- URL: https://www.wjgnet.com/1949-8462/full/v8/i11/684.htm
- DOI: https://dx.doi.org/10.4330/wjc.v8.i11.684
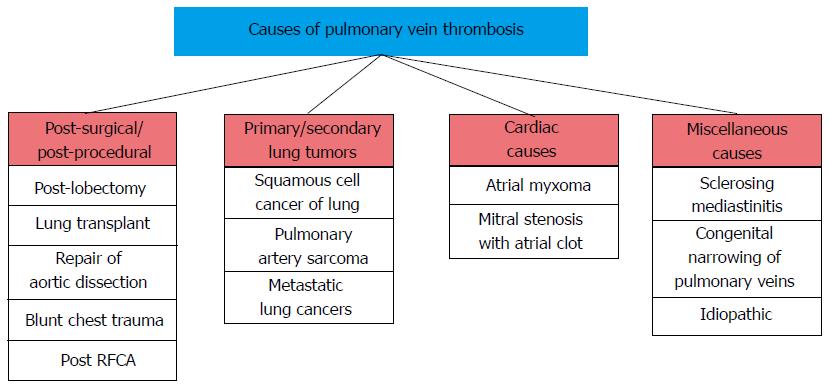
Pulmonary vein thrombosis (PVT) is a rare but potentially life threatening condition. Lung circulation has rich venous collaterals; however certain medical conditions can cause obstruction to the pulmonary veins[1]. The various etiologies for the pulmonary vein thrombosis can be broadly categorized as post lung surgery, from primary or secondary tumors of lung, cardiac causes and miscellaneous causes[2-8]. The clinical diagnosis of the PVT is difficult as its signs and symptoms can be vague and nonspecific. It can either present acutely in the form of dyspnea, pleuritic chest pain and hemoptysis or as progressive lung fibrosis and chronic pulmonary edema[9]. Several different imaging modalities have been used in diagnosing PVT including computerized tomography angiography (CTA), transesophageal echocardiography (TEE) and magnetic resonance imaging (MRI)[8-13]. PVT is managed with anticoagulation but treatments can differ depending on the various etiologies and clinical status on presentation. We are presenting a case of pulmonary vein thrombosis in a patient with polycythemia vera which is the first reported case in literature of this unique association.
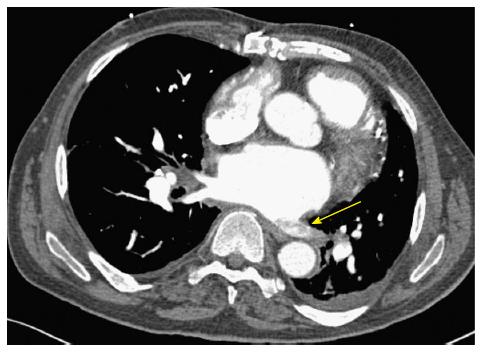
A 76-year-old male presented with a two day history of the severe left sided chest pain. The chest pain was sudden onset, unrelated to exertion but worsened with inspiration. His past medical history included polycythemia vera, coronary artery disease, pulmonary hypertension, pulmonary embolism, diastolic heart failure and permanent atrial fibrillation. He had JAK2 proven polycythemia vera and had required intermittent phlebotomy in the past. He was on chronic thromboprophylaxis with aspirin. He was on chronic anticoagulation with warfarin due to his history of pulmonary embolism. He was admitted with the suspicion for acute coronary syndrome. His troponins remained within normal limits and there were no significant electrocardiogram (ECG) changes. His ECG revealed an ejection fraction of 55% with grade 2 diastolic dysfunction and elevated pulmonary artery pressures. His labs were within normal limits other than hemoglobin of 12.9 g/dL and elevated white blood cell count of 17400. INR on arrival was 2.1. He underwent a CT angiography with suspicion for pulmonary embolism. CTA revealed a left inferior pulmonary vein thrombosis with extension into the left atrium (Figure 1) along with left lower lobe consolidation. He was immediately started on therapeutic dosage of low molecular weight heparin and antibiotics for the presumed bacterial pneumonia. His symptoms improved on the treatment and he was discharged with subcutaneous low molecular weight heparin. A follow up CT angiogram a few weeks later showed the resolution of his pulmonary vein thrombosis (Figure 2).
Pulmonary vein thrombosis is the most distal source of the upstream arterial thrombi. It is most common etiologies include lung surgeries either in the form of lung transplantation and lobectomies[2,3]. Other etiologies associated with PVT are lung cancers and sclerosing mediastinitis[5,6]. PVT has been associated with atrial myxomas and after radio frequency catheter ablation[7,8] (Figure 3).
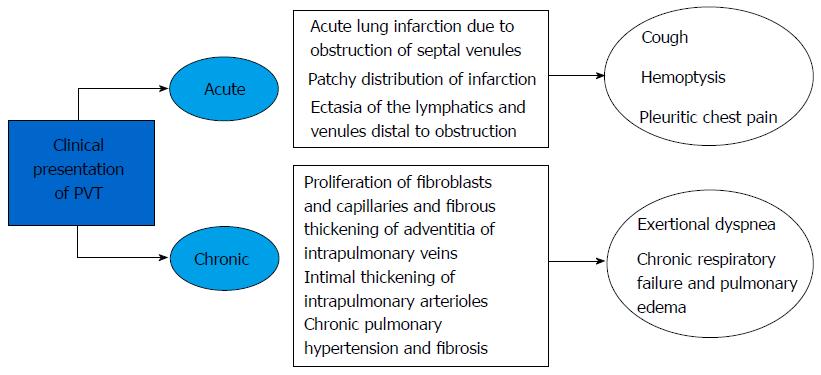
The clinical presentation of the PVT can vary depending on the number of veins involved, extent of occlusion, adequacy of the venous collaterals and degree of lymphatic obstruction (Figure 3). Historically the pulmonary vein thrombosis presentation is associated with a triad of cough, dyspnea and hemoptysis[1]. The clinical presentations can be broadly divided into acute lung infarction pattern with cough, chest pain and pleuritic chest pain or in an insidious symptom pattern with progressive pulmonary fibrosis and pulmonary edema[1,9]. Patients with chronic PVT are prone to recurrent bouts of respiratory infection. In advanced disease with involvement of more than one pulmonary vein, patients can have frequent episodes of pulmonary edema progressing to intractable heart failure[1].
Before understanding the pathophysiology of the pulmonary vein thrombosis it is important to know that both pulmonary and bronchial circulation drain into the left atrium through the pulmonary veins. Any obstruction to this flow can lead to dilation of the bronchial and pulmonary veins. The pathophysiology of the symptoms can be very similar to mitral valve stenosis, i.e., increase in pulmonary venous pressure and compensatory pulmonary arterial vasoconstriction leading to increase in right ventricular end diastolic pressures. In an animal study Wyatt et al[11] had demonstrated sequential changes in the canine lungs after the ligation of pulmonary veins which comprised of congestion, serum extravasation and alveolar hemorrhage leading to lobar consolidation.
It is a challenge to establish the diagnosis of the PVT syndrome unless there is a strong clinical suspicion. Several diagnostic modalities can help in making the diagnosis including chest X-ray, CTA[6,7,9], TEE[5,12] or MRI[10] (Figure 4 and Table 1). Chest X-ray may reveal no finding or nonspecific air space disease or opacities[2]. Modified CT angiography that is utilized to identify pulmonary artery embolus can also detect the pulmonary vein thrombosis. ECG gated MRI is the least invasive modality to demonstrate the pulmonary vein embolus extending to left atrium. MRI imaging can also differentiate the bland thrombus from a tumor thrombus[10]. Pulmonary angiography is not commonly used to diagnose PVT due the increased risks from the procedure as well as contrast exposure. A normal arterial phase and delayed or absent venous filling during the pulmonary angiogram can demonstrate a pulmonary vein thrombosis[1].
| Type of modality | Findings | Drawbacks |
| Chest X-ray | Increased vascular marking, increased hilar size Consolidation, atelectasis Mitral configuration of pulmonary conus (extensive PVT) | Nonspecific in the setting of coexistent infections Variable findings |
| CT angiography/multidetector CT | Longer delays of contrast clearance on the venous phase Filling defect in pulmonary veins | Requires IV contrast Artifact from heart motion, dense contrast, poorly opacified blood can leads the PVT undetected |
| TEE | Can detect the thrombus when it extends to the left atrium Echo dense thrombus occluding the pulmonary veins | Invasive, requires sedation Can’t detect the distal PVT |
| MRI | Least invasive methods Can differentiate blood clot from tumorous clot | Expensive Needs cooperative patients with stable cardiac rhythm |
| Pulmonary angiography | Failure to enhance the vein lumen A partial filling defect surrounded by normal contrast | Invasive and requires the contrast exposure Possibility of injury to the pulmonary artery, cardiac perforation, cardiac arrest |
The PVT can become a source of arterial thromboembolic disease. Because of the high flow in pulmonary venous circulation small fragments of the platelets and fibrinous material can constantly break off from the thrombus. Garcia et al[12] described a case of bilateral femoral arterial occlusion in a patient of PVT. It can lead to pulmonary infraction and pulmonary gangrene[1] during the acute occlusive phase and in chronic phases it can cause progressive pulmonary fibrosis[9]. There are case reports about PVT complicating old myocardial ischemia[13].
There is no clear consensus regarding the treatment of the PVT. The choice of therapy depends on the clinical status of the patient and the etiology of PVT. In case of pulmonary infraction requiring urgent intervention, surgical treatments in the form of embolectomy or lung resection might be indicated[2,14]. Appropriate use of the anticoagulation in the absence of hemorrhage can prevent clot progression and embolization. In patients where any carcinoma is involved, the use low molecular weight heparin is advisable. In the past, antibiotics were used for treating PVT[11,14]. But the role of antibiotics in the absence of infection is questionable. The use and duration of the Warfarin for PVT has not been evaluated in studies. In patients with PV, the risk of thrombosis directly correlates with hematocrit, and frequent phlebotomies to maintain this at < 45% in males and < 42% females remains the cornerstone of therapy for all patients groups. The venous thrombotic events are managed in standard fashion with parenteral heparin followed by oral anticoagulation with warfarin. The patients should be followed closely with strict monitoring of the INRs and platelet counts as the patients are at increased risk for bleeding too. Systemic anticoagulation might not be sufficient and these patients should get concomitant myelosuppressive therapy preferable with hydroxyurea as well as phlebotomies. In a study done by De Stefano et al[15] cytoreductive therapy reduced the incidence of rethrombosis by 50% especially in patients who presented with acute coronary syndrome. The use of systemic anticoagulation (after venous thromboembolism) as well as antiplatelet therapy (after cerebrovascular accidents as well as venous thromboembolism) improved the protective effect. It is recommended to use the cytoreductive chemotherapies in addition to phlebotomies in high risk patients (age > 60 years and previous thrombotic events)[16].
In our patient pulmonary venous thrombosis occurred while he was on both aspirin and warfarin with a therapeutic INR of 2.1. It was considered to be warfarin failure and his anticoagulation was changed to subcutaneous enoxaparin while continuing low dose aspirin.
In summary, we want to describe a case of pulmonary venous thrombosis in a patient with polycythemia vera. The clinical signs and symptoms of PVT can mimic pulmonary arterial embolism, acute coronary syndrome or pulmonary infections. Early recognition is imperative as PVT can lead to numerous complications including arterial thromboembolic disease. Anticoagulation can be chosen as first line therapy if there are no contraindications. Choice of anticoagulant agent can be tailored based on the clinical picture and patient comorbidities. In our case the patient developed thrombosis despite being on warfarin and was discharged on low molecular weight heparin. Cytoreductive therapies reduce the recurrence of the thrombotic events and should be considered in all high risk patients. Further studies and experience is needed to make the correct decision about the type and duration of anticoagulation in patients with PVT.
This is a unique case describing a rare presentation of polycythemia vera as a thrombotic event in pulmonary veins.
The patient presented with a left sided chest pain and the computerized pulmonary angiogram revealed a thrombus in the left lower pulmonary vein.
Coronary artery disease, pulmonary embolism and pneumonia.
The INR on arrival was 2.1, white cell count of 17400 and computerized tomographic angiogram revealed a thrombus on the left lower pulmonary vein.
A filling defect on the venous phase of the computerized pulmonary angiogram which diagnosed a thrombosis of the left lower pulmonary vein.
Patient was started on low molecular weight heparin. He was on warfarin and had a therapeutic INR when he presented with the pulmonary vein thrombosis. A computerized tomography angiography done few weeks later showed resolution of the thrombus.
Pulmonary vein thrombosis is an uncommonly encountered disease entity with various clinical presentations. It can lead to serious complications including lung infarction and hemodynamic instability. Although polycythemia vera presents with thrombosis at unusual sites but the association of pulmonary vein thrombosis with polycythemia vera has not been described in the literature so far.
Computerized tomographic pulmonary angiography is a common modalities utilized to rule out acute pulmonary embolism. It utilizes infusion of an iodinated contrast to look at the pulmonary vasculature.
The timely diagnosis of pulmonary vein thrombosis could be difficult and requires high index of suspicion. It should be considered an etiology for the clinical presentations with chest pain and dyspnea in people at high risk for thrombotic events.
A well described case of pulmonary vein thrombosis presenting as left sided chest pain. In the discussion authors have delineated the spectrum of clinical presentation and treatment options in detail. The type and duration of anticoagulants use for the pulmonary vein thrombosis has not been studied in clinical trials so far.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kettering K, Lin GM, Najafi M, Satoh H S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Williamson WA, Tronic BS, Levitan N, Webb-Johnson DC, Shahian DM, Ellis FH. Pulmonary venous infarction. Chest. 1992;102:937-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 2. | Hovaguimian H, Morris JF, Gately HL, Floten HS. Pulmonary vein thrombosis following bilobectomy. Chest. 1991;99:1515-1516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Sarsam MA, Yonan NA, Beton D, McMaster D, Deiraniya AK. Early pulmonary vein thrombosis after single lung transplantation. J Heart Lung Transplant. 1993;12:17-19. [PubMed] |
| 4. | Thelin S, Karacagil S, Grewal P, Oxelbark S, Bergqvist D. Surgical repair of type B aortic dissection complicated by early postoperative lung vein and artery thrombosis. Scand Cardiovasc J. 1999;33:248-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Kim NH, Roldan CA, Shively BK. Pulmonary vein thrombosis. Chest. 1993;104:624-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Dye TE, Saab SB, Almond CH, Watson L. Sclerosing mediastinitis with occlusion of pulmonary veins. Manifestations and management. J Thorac Cardiovasc Surg. 1977;74:137-141. [PubMed] |
| 7. | Yataco J, Stoller JK. Pulmonary venous thrombosis and infarction complicating pulmonary venous stenosis following radiofrequency ablation. Respir Care. 2004;49:1525-1527. [PubMed] |
| 8. | Stevens LH, Hormuth DA, Schmidt PE, Atkins S, Fehrenbacher JW. Left atrial myxoma: pulmonary infarction caused by pulmonary venous occlusion. Ann Thorac Surg. 1987;43:215-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Cavaco RA, Kaul S, Chapman T, Casaretti R, Philips B, Rhodes A, Grounds MR. Idiopathic pulmonary fibrosis associated with pulmonary vein thrombosis: a case report. Cases J. 2009;2:9156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 10. | Selvidge SD, Gavant ML. Idiopathic pulmonary vein thrombosis: detection by CT and MR imaging. AJR Am J Roentgenol. 1999;172:1639-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (2)] |
| 11. | Wyatt JP, Burke DR, Hanlon CR. Morphologic study of canine lungs after ligation of the pulmonary veins. Am J Pathol. 1953;29:291-303. [PubMed] |
| 12. | Garcia MJ, Rodriguez L, Vandervoort P. Pulmonary vein thrombosis and peripheral embolization. Chest. 1996;109:846-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 13. | Komatsu S, Kamata T, Imai A, Miyaji K, Ohara T, Takewa M, Shimizu Y, Yoshida J, Hirayam A, Nanto S. Idiopathic pulmonary vein thrombosis complicated with old myocardial infarction detected by multidetector row computed tomography. Cardy Case. 2011;3:e94-e97. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Burri E, Duwe J, Kull C, Glaser C, Maurer CA. Pulmonary vein thrombosis after lower lobectomy of the left lung. J Cardiovasc Surg (Torino). 2006;47:609-612. [PubMed] |
| 15. | De Stefano V, Za T, Rossi E, Vannucchi AM, Ruggeri M, Elli E, Micò C, Tieghi A, Cacciola RR, Santoro C. Recurrent thrombosis in patients with polycythemia vera and essential thrombocythemia: incidence, risk factors, and effect of treatments. Haematologica. 2008;93:372-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 248] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 16. | Cortelazzo S, Finazzi G, Ruggeri M, Vestri O, Galli M, Rodeghiero F, Barbui T. Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N Engl J Med. 1995;332:1132-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 567] [Article Influence: 18.9] [Reference Citation Analysis (0)] |