Published online Oct 26, 2016. doi: 10.4330/wjc.v8.i10.590
Peer-review started: March 9, 2016
First decision: May 17, 2016
Revised: July 15, 2016
Accepted: August 6, 2016
Article in press: August 8, 2016
Published online: October 26, 2016
Processing time: 231 Days and 20.4 Hours
To describe echocardiographically left ventricular false tendon characteristics and the correlation with ventricular repolarization abnormalities in young athletes.
Three hundred and sixteen healthy young athletes from different sport disciplines were evaluated from 2009 to 2011 during routine screening for agonistic sports eligibility. All subjects, as part of standard pre-participation screening medical evaluation, underwent a basal and post step test 12-lead electrocardiogram (ECG). The athletes with abnormal T-wave flattening and/or inversion were considered for an echocardiogram evaluation and an incremental maximal exercise test on a cycle ergometer. Arterial blood pressure and heart rate, during and after exercise, were also measured.
Twenty-one of the 316 subjects (6.9%) showed false tendons in the left ventricle. The majority of false tendons (52.38%) were localized between the middle segments of the inferior septum and the lateral wall, 19.06% between the distal segments of the septum and the lateral wall, in 5 subjects between the middle segments of the anterior and inferior walls, and in one subject between the middle segments of the anterior septum and the posterior wall. ECG abnormalities, represented by alterations of ventricular repolarization, were found in 11 subjects (52.38%), 90% of these anomalies were T wave abnormalities from V1 to V3. These anomalies disappeared with an increasing heart rate following the three minute step test as well as during the execution of the maximal exercise.
Left ventricular false tendons are frequently localized between the middle segments of the inferior septum and the lateral wall and are statistically associated with ventricular repolarization abnormalities.
Core tip: Ventricular repolarization abnormalities of subjects with false tendons were most frequently inverted T waves from V1 to V3. In this study, statistically significant associations between the presence of false tendons in the left ventricle and ventricular repolarization abnormalities in young healthy athletes were found. Furthermore, this study provides useful information for sports physicians when basic electrocardiogram abnormalities of ventricular repolarization are considered.
- Citation: Lazarevic Z, Ciminelli E, Quaranta F, Sperandii F, Guerra E, Pigozzi F, Borrione P. Left ventricular false tendons and electrocardiogram repolarization abnormalities in healthy young subjects. World J Cardiol 2016; 8(10): 590-595
- URL: https://www.wjgnet.com/1949-8462/full/v8/i10/590.htm
- DOI: https://dx.doi.org/10.4330/wjc.v8.i10.590
“False tendons” are fibrous, fibrous-muscle or muscle structures, variable in length and thickness, found in the left ventricular cavity, generally located between the free wall of the left ventricle or a papillary muscle and the interventricular septum, without connection to the mitral valves[1-3]. Turner first described the false tendons in the left ventricle (LVFT) in 1893 but the functional significance of these structures is still unclear[4].
The left ventricular false tendons are easily identifiable with bi-dimensional echocardiography. They are usually found in about 50% of autoptical examinations[5-8], most frequently in males[4,9]. The prevalence of false tendons in the left ventricle appears to be higher in young athletes than in the general population (6.9% vs 0.5% to 4.6%)[7]. This difference can be attributed to an increased use of echocardiography in young athletes. However, a young athlete often has excellent acoustic windows, physiological bradycardia and enlargement of the ventricular cavity, which permit better identification of all structures inside the ventricular cavity and in particular, the trabeculae or fibrous-muscle structures, stretched between the walls of the ventricle[10].
The primary characteristic of the false tendons to be emphasized is their tension or laxity inside the left ventricular cavity during the cardiac cycle. More frequently, false tendons are stretched in diastole and are flaccid in systole (from 71.4% to 86% of cases); in some cases they are in tension for the entire cardiac cycle (10.6%-15.4%), while in rare cases they remain flaccid for the entire cycle (1.2%-2.8%).
This type of information is very useful since the stretching of these ventricular structures can play an important role in the genesis of electrocardiographic abnormalities or real arrhythmias. This mechanical phenomenon is also the basis of the genesis of a murmur that can be appreciated on auscultation in some subjects with false tendons[1,11]. Generally, LVFTs have been considered a normal variation but in some cases, they may be related to cardiac pre-excitation, ventricular arrhythmias, dilation of the left ventricle, congenital and/or acquired heart diseases and some repolarization abnormalities on resting electrocardiograms (ECGs), including negative or biphasic T waves in precordial leads as well as early repolarization[12].
A literature review highlighted that most of the studies regarding LVFT were performed on a general population and documented a correlation with arrhythmias and structural cardiac disease, while only a few and dated investigations described the correlation with ventricular repolarization abnormalities[13] and no studies were conducted on healthy young athletes.
The purpose of this study was to describe the echocardiographic characteristics of LVFTs and their correlation with the abnormal ventricular ECG repolarization findings in a group of healthy young athletes.
The study population was composed of 316 subjects (162 males and 154 females) with a mean age of 22.3 ± 4 years, consecutively evaluated from March 2009 to November 2011. All subjects were healthy and engaged in different agonistic sports disciplines (athletics, swimming, gymnastics, basketball, football and volleyball) for a total of approximately 15-20 h a week for about 8 mo a year.
All tested athletes had a negative medical family history and a normal baseline medical examination. In most cases (71%), auscultation sounds with the characteristics of a Still’s murmur could be heard.
Each subject underwent: (1) a 12 lead ECG at rest and after a step test performed by the electrocardiographic device ESAOTE 421 ArchiMed-Esaote Biomedica. T wave flattening and the presence of T-wave inversion > 2 mm in one or more leads were considered for further investigations; (2) echocardiogram with bi-dimensional and color-Doppler evaluation using the instrument Terason T-3000 MORTARA. The echocardiographic diagnosis of false tendons in the left ventricle was based on the finding of a linear echogenic tendon, which crosses the left ventricular cavity, connecting different sites of the ventricular endocardium, and not correlated to the mitral valve apparatus. The false tendon size, thickness, pattern inside the left ventricular cavity, points of connection and tension or laxity during the cardiac cycle were evaluated; and (3) maximal exercise test on a cycle ergometer using the device Ergoline Ergometrics 800S and ECG monitoring device via CardiO2 MedGraphics, according to a protocol that included a 2 min warm-up at 20 W and subsequent increases of load for 40 W every 2 min, with active and passive recovery duration of 5 min. Values of systemic blood pressure and heart rate, during and after exercise were measured. Any cardiorespiratory symptoms and/or electrocardiographic changes during the execution of the test were noted.
Variables were reported by counts and percentages. When appropriate, comparisons were performed using a χ2 test or Fisher’s exact test. To evaluate the association between the variable of interest and the determinant, the odds ratio and 95% confidence interval (Cornfield’s method) were calculated. All the tests were considered statistically significant for P values < 0.05. The analyses were conducted with STATA v.11.
Twenty one of the 316 subjects (6.9%), 12 males and 9 females with a mean age of 22 ± 2 years, showed false tendons in the left ventricle.
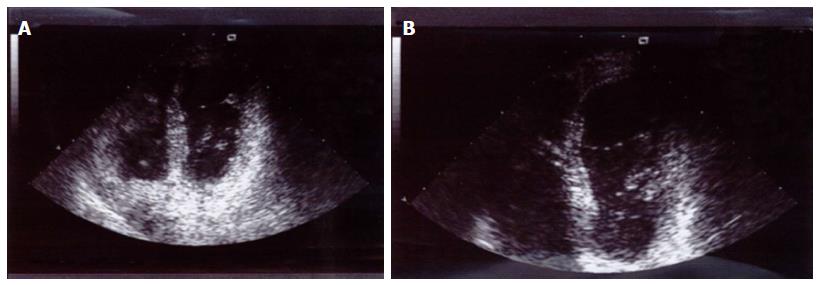
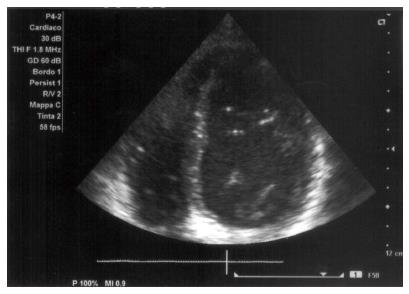
The majority of false tendons were localized between the middle segments of the inferior septum and the lateral wall (52.38%) (Figures 1 and 2), between the distal segments of the septum and the lateral wall (19.06%), between the middle segments of the anterior and inferior walls (23.8%), and between the middle segments of the anterior septum and the posterior wall (4.76%) (Table 1).
| Anatomic site of false tendon | N° (%) | Altered ventricular repolarization N° (%) |
| Middle segment inferior septum - lateral wall | 11 (52.38) | 7 (63.6%) |
| Distal segment inferior septum - lateral wall | 4 (19.06) | 2 (50%) |
| Middle segment posterior wall - anterior septum | 1 (4.76) | 0 (0%) |
| Middle segment inferior wall - anterior wall | 5 (23.8) | 2 (40%) |
| Description of altered ventricular repolarization | Frequency | % |
| Flat T wave in DII, aVF, inverted T wave in DIII | 10 | 47.6 |
| Biphasic T wave in DII, DIII and aVF after incremental max exercise test | 1 | 4.8 |
| Biphasic T wave in V2 and V3, normalize after incremental max exercise test | 1 | 4.8 |
| Inverted T wave from V1 to V3 normalizes after incremental max exercise test | 6 | 28.6 |
| Inverted asymmetric T wave from V1 to V3 normalizes after incremental max exercise test | 1 | 4.8 |
| Inverted symmetric T wave from V1 to V3, that reduces but does not normalize after incremental max exercise test | 1 | 4.8 |
| Flat T wave in DIII and inverted from V1 to V3 normalizes after incremental max exercise test | 1 | 4.8 |
ECG abnormalities represented by alterations of ventricular repolarization were found in 11 subjects (52.38%).
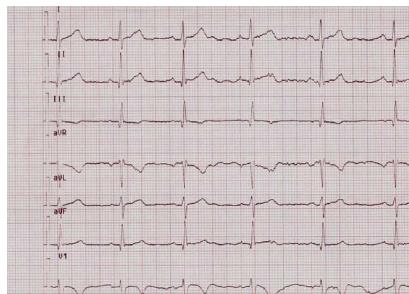
The anomalies of the phase of ventricular repolarization observed in these cases were almost always characterized by the presence of inverted T waves from V1 to V3 (9 of 11 cases with abnormalities of the ventricular repolarization phase, 81%) (Figure 3).
Only one case had diphasic T waves from V1 to V3 and an inverted T wave in DIII and aVF. In this study, 90% of the anomalies of ventricular repolarization were abnormalities of the T wave from V1 to V3.
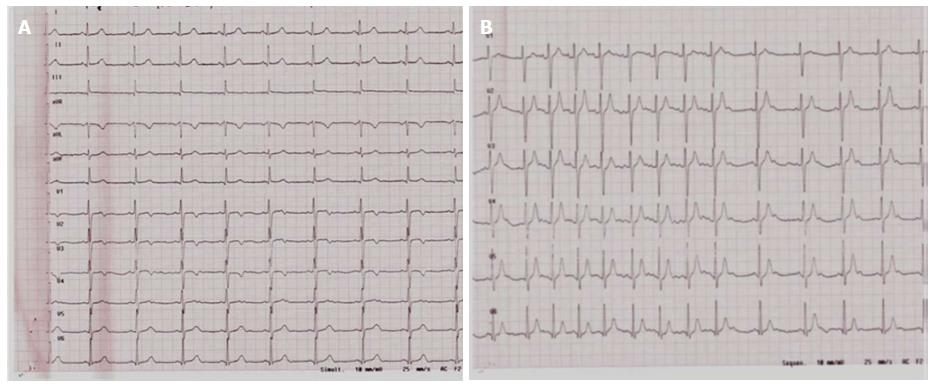
These anomalies disappeared with an increasing heart rate following three minutes of the step test as well as during the execution of the maximal exercise (Figure 4).
The association between false tendons in the left ventricle and the abnormal ventricular repolarization phase showed an odds ratio of 11 (95%CI: 3.4-35.6, P < 0.0001).
The insertion sites of false tendons most often associated with abnormalities of the ventricular repolarization were in the middle segments of the inferior septum and the lateral wall (63.6%) and the distal segments of the septum and the lateral wall (30%). However, in this case, the Fisher’s exact test did not demonstrate statistical significance (P = 0.712).
This study showed the presence of a statistically significant association between false tendons in the left ventricle and ventricular repolarization abnormalities. However, the odds ratio value is too high (a value of 11 with confidence interval width ranging from 3.4 to 3.5) due to the low number of subjects.
The false tendons were located more frequently (in over 63% of cases) between the middle segments of the interventricular septum and the lateral wall and presented a greater thickness when compared to normal tendons (> 2 mm). In 30% of cases, the false tendons stretched between the distal segments of the interventricular septum and the lateral wall.
The repolarization abnormalities were almost of the same type. Indeed, 90% of the subjects with a false tendon and an abnormal ventricular repolarization phase presented with alterations in T waves (more often reversed and symmetrical, sometimes diphasic) from V1 to V3.
The association between abnormalities of ventricular repolarization and false tendons in the left ventricle was described by Sutton et al[14] who presented three case reports regarding three patients in apparently good health with a false tendon in the left ventricle and inverted T waves in the precordial leads.
Sutton et al[14] also noted an “electro-anatomical” correlation between false tendons and ECG abnormalities as well as the absence of modifications after a long follow-up of 13 years in his study. Other authors also identified the presence of Purkinje fibres within the false tendons; this information could explain the onset of arrhythmias associated with the presence of left ventricular false tendons. Some authors investigating the possible link between false tendons and ECG abnormalities identified 71 subjects with a false tendon and studied the possible presence of arrhythmias, such as ventricular extrasystole. The authors concluded that the false tendon can contribute to the etiology of arrhythmias such as ventricular extrasystole, but they did not describe abnormalities of the ventricular repolarization phase[15,16].
The statistically significant association between the presence of false tendons in the left ventricle and abnormal ventricular repolarization phase could have several explanations. The presence of a false tendon in the left ventricle would increase, although minimally, myocardial active mass, typical of the athlete’s heart[10]. This increase in myocardial mass could activate a prolongation of the depolarization and eventually lead to T wave inversion. An alternative hypothesis considers purely mechanical aspects: the false tendon and its site of anatomical implantation (mainly medium-distal segments of the inferior septum and lateral wall) may exert mechanical traction sufficient to alter repolarization.
Finally, the fibro-muscular false tendon contains elements of the cardiac conduction system, often providing the explanation for electrocardiographic abnormalities that might be associated with these structures[4].
In clinical practice, abnormal T-wave flattening and/or inversion can be detected in different physiological and pathological conditions[17]. When considering young and healthy subjects, T-wave flattening and/or inversion were found with variable frequency, from 0.5% to 19%, and in high-level athletes they have been described as clinically negative in 60%-80%[18]. The behavior of ventricular repolarization abnormalities during the incremental maximal exercise test on a cycle ergometer has fundamental importance. This test has significant diagnostic and prognostic importance. Usually, the normalization of T waves during a maximal exercise test on an ergometer suggests their benign nature, although in some cases organic diseases of the heart cannot be excluded[19] .
The results of this study showed a statistically significant association between the presence of false tendons in the left ventricle and ventricular repolarization abnormalities in a population of young healthy subjects engaged in competitive sports. The type of false tendon most frequently associated with ventricular repolarization abnormalities was identified in the middle-distal segments of the inferior interventricular septum and the lateral wall. Ventricular repolarization abnormalities of subjects with false tendons were all of the same type, indeed, the electrocardiogram showed inverted T waves from V1 to V3. These anomalies also regressed with the increase in heart rate during the physical exercise or incremental maximal exercise test on a cycle ergometer. A common electrocardiographic pattern can be described in athletes with a false left ventricular tendon. In fact, the ventricular repolarization abnormalities in the electrocardiogram in these individuals were similar and showed the same behavior under stress. The limitations of our study are related to the low number of participants and the lack of long term follow-up to evaluate eventual modifications.
In conclusion, the present study showed a statistically significant association between the presence of false tendons in the left ventricle and ventricular repolarization abnormalities in a population of young healthy subjects engaged in competitive sports.
The type of false tendon most frequently associated with ventricular repolarization abnormalities was identified among the middle-distal segments of the inferior interventricular septum and the lateral wall. Nonetheless, the results of this study may provide useful information for sports physicians when basic ECG abnormalities of ventricular repolarization are found.
False tendons are fibrous, fibrous-muscle or muscle structures, variable in length and thickness, found in the left ventricular cavity, generally located between the free wall of the left ventricle or a papillary muscle and the interventricular septum, without connection to the mitral valves. In 1893, Turner first described the false tendons in the left ventricle (LVFT) but the functional significance of these structures is still unclear. The left ventricular false tendons are easily identifiable with bi-dimensional echocardiography. They are usually found in 50% of autoptical examinations, mostly in males. Generally, LVFTs have been considered a normal variation but in some cases could be related to cardiac pre-excitation, ventricular arrhythmias, dilation of the left ventricle, congenital and/or acquired heart disease and some repolarization abnormalities on a resting electrocardiogram (ECG), including negative or diphasic T waves in precordial leads as well as early repolarization. Only a few studies have investigated the correlation between LVFTs and ventricular repolarization abnormalities and to our knowledge, no studies have been carried out on healthy young athletes. In this study they evaluated and described the echocardiographic characteristics of LVFTs and their correlation with the abnormal ventricular ECG repolarization findings in a group of healthy young athletes.
The results of this study clarified the functional significance of left false tendons, adding useful information for the interpretation of abnormal ventricular ECG repolarization findings during the pre-participation screening of healthy athletes.
The present study describes a statistically significant association between the presence of false tendons in the left ventricle and ventricular repolarization abnormalities for the first time. This finding certainly provides useful information for sports medicine physicians for the interpretation of ECG abnormalities found in otherwise healthy athletes during the pre-participation screening evaluation.
This study provides useful information for sports physicians about sport eligibility evaluation for athletes when basic ECG abnormalities of ventricular repolarization are found.
LVFTs: Fibrous, fibrous-muscle or muscle structures generally located between the free wall of the left ventricle or a papillary muscle and the interventricular septum, without connection to the mitral valves; ECG: Electrocardiogram; VRA: Ventricular repolarization abnormalities.
This is an interesting study that is well written and uses appropriate methods. It was suggested that another image demonstrating the LV false tendon should be provided as this is a key aspect of the study and should be better illustrated.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Azevedo C, Jankowski P, Simkhovich B S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Kenchaiah S, Benjamin EJ, Evans JC, Aragam J, Vasan RS. Epidemiology of left ventricular false tendons: clinical correlates in the Framingham Heart Study. J Am Soc Echocardiogr. 2009;22:739-745. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Witter BA, DeCristofaro D. Echocardiography of left ventricular trabeculations, bands and false tendons. Am J Cardiol. 1993;71:499-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Turner W. Another Heart with Moderator Band in Left Ventricle. J Anat Physiol. 1896;30:568-569. [PubMed] |
| 4. | Silbiger JJ. Left ventricular false tendons: anatomic, echocardiographic, and pathophysiologic insights. J Am Soc Echocardiogr. 2013;26:582-588. [PubMed] |
| 5. | Philip S, Cherian KM, Wu MH, Lue HC. Left ventricular false tendons: echocardiographic, morphologic, and histopathologic studies and review of the literature. Pediatr Neonatol. 2011;52:279-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Loukas M, Louis RG, Black B, Pham D, Fudalej M, Sharkees M. False tendons: an endoscopic cadaveric approach. Clin Anat. 2007;20:163-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Gerlis LM, Wright HM, Wilson N, Erzengin F, Dickinson DF. Left ventricular bands. A normal anatomical feature. Br Heart J. 1984;52:641-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Luetmer PH, Edwards WD, Seward JB, Tajik AJ. Incidence and distribution of left ventricular false tendons: an autopsy study of 483 normal human hearts. J Am Coll Cardiol. 1986;8:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Gualano SK, Bolling SF, Gordon D, Wilson A, Bach DS. High prevalence of false chordae tendinae in patients without left ventricular tachycardia. Pacing Clin Electrophysiol. 2007;30 Suppl 1:S156-S159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Paolo Z. Cardiologia dello Sport. Edit. CESI. 2007;208-209. |
| 11. | Casta A, Wolf WJ. Left ventricular bands (false tendons): echocardiographic and angiocardiographic delineation in children. Am Heart J. 1986;111:321-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Liu Y, Mi N, Zhou Y, An P, Bai Y, Guo Y, Hong C, Ji Z, Ye P, Wu C. Transverse false tendons in the left ventricular cavity are associated with early repolarization. PLoS One. 2015;10:e0125173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Salazar J. Left ventricular anomalous muscle band and electrocardiographic repolarization changes. Pediatr Cardiol. 1997;18:434-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Sutton MG, Dubrey S, Oldershaw PJ. Muscular false tendons, aberrant left ventricular papillary musculature, and severe electrocardiographic repolarisation abnormalities: a new syndrome. Br Heart J. 1994;71:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Suwa M, Hirota Y, Kaku K, Yoneda Y, Nakayama A, Kawamura K, Doi K. Prevalence of the coexistence of left ventricular false tendons and premature ventricular complexes in apparently healthy subjects: a prospective study in the general population. J Am Coll Cardiol. 1988;12:910-914. [PubMed] |
| 16. | Suwa M, Hirota Y, Nagao H, Kino M, Kawamura K. Incidence of the coexistence of left ventricular false tendons and premature ventricular contractions in apparently healthy subjects. Circulation. 1984;70:793-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Serra-Grima R, Estorch M, Carrió I, Subirana M, Bernà L, Prat T. Marked ventricular repolarization abnormalities in highly trained athletes’ electrocardiograms: clinical and prognostic implications. J Am Coll Cardiol. 2000;36:1310-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ, Gorgels A, Hancock EW, Josephson M, Kligfield P. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2009;119:e241-e250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 300] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 19. | Zorzi A, ElMaghawry M, Rigato I, Cardoso Bianchini F, Crespi Ponta G, Michieli P, Migliore F, Perazzolo Marra M, Bauce B, Basso C. Exercise-induced normalization of right precordial negative T waves in arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol. 2013;112:411-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |