Published online Sep 26, 2015. doi: 10.4330/wjc.v7.i9.579
Peer-review started: April 29, 2015
First decision: May 14, 2015
Revised: June 27, 2015
Accepted: July 21, 2015
Article in press: July 23, 2015
Published online: September 26, 2015
Processing time: 145 Days and 8.2 Hours
Constrictive pericarditis (CP) is an inflammatory disease of pericardium. Pericardial calcification in X-ray provides a clue for the diagnosis of CP. An extensive “eggshell” type of calcification is rarely seen in CP. We hereby report a case of CP with eggshell calcification of pericardium, encircling whole of the heart. A need for multimodality imaging and hemodynamic assessment followed by surgical pericardiectomy is discussed.
Core tip: Idiopathic contrictive pericarditis (CP) with extensive pericardial calcification is rarely seen. We hereby report a case of CP with extensive “eggshell” calcification of heart, who presented with right heart failure. A need for multimodality imaging and hemodynamic assessment is discussed in the article.
- Citation: Vijayvergiya R, Vadivelu R, Mahajan S, Rana SS, Singhal M. Eggshell calcification of the heart in constrictive pericarditis. World J Cardiol 2015; 7(9): 579-582
- URL: https://www.wjgnet.com/1949-8462/full/v7/i9/579.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i9.579
Constrictive pericarditis (CP) is an inflammatory disease of pericardium. Its etiology includes infection, connective tissue disorders, chest trauma, irradiation, post-cardiac surgery and idiopathic-type[1]. Extensive pericardial calcification is rarely seen in CP. We hereby report a case of CP presented with extensive “eggshell” like calcification of whole of pericardium.
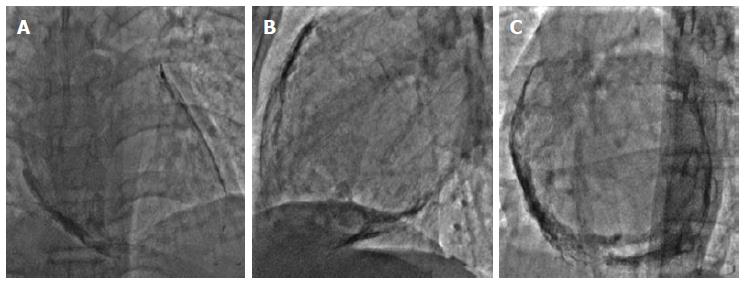
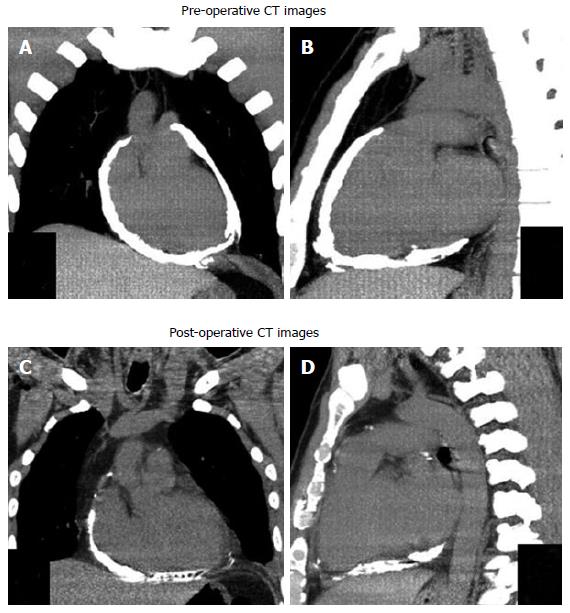
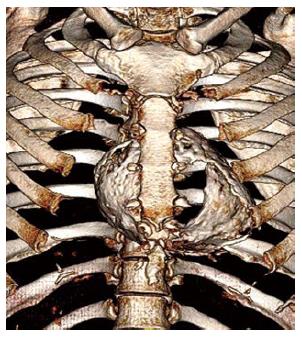
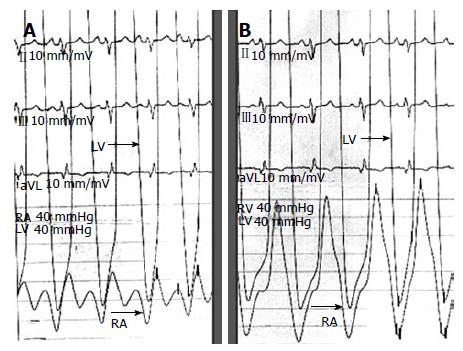
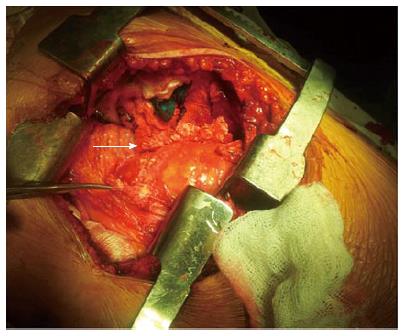
A 43-year-old male presented with shortness of breath, NYHA class-III of 6-mo duration. There was no history of fever, productive cough, joint pain, orthopnea and pedal edema. Clinical examination revealed a jugular venous pulse of 18 cm, prominent X and Y descents. Cardiac auscultation revealed a pericardial knock. Two-dimensional echocardiogram showed 10-mm thick, calcified pericardium; about 25%-variation in mitral diastolic flow velocities with respiration and a dilated inferior vena cava of 24-mm dimension. Fluoroscopy revealed dense circumferential calcification all around the heart (Figure 1). A computed tomography (CT) scan confirmed the circumferential thick pericardial calcification like an eggshell, encircling the heart (Figures 2 and 3). Angiography revealed normal epicardial coronaries without any external compression. Hemodynamic data revealed elevated mean right atrial (RA) pressure of 20 mmHg. Right ventricle (RV) and left ventricle (LV) end-diastolic pressure was 23 and 28 mmHg, respectively. Pulmonary artery systolic and mean pulmonary capillary wedge pressures were 44 and 24 mmHg, respectively. There was near equalization of elevated RA, RV and LV end-diastolic pressures. Right atrial pressure tracing showed prominent X and Y descent (Figure 4A), and ventricular pressure tracing showed typical “dip-and-plateau configuration” (Figure 4B) suggestive of CP. He had surgical pericardiectomy for densely calcified CP. Following median thoracotomy, thickened, calcified, firmly adherent pericardium was resected and excised from anterior and left lateral aspect of the heart (Figure 5). The densely adherent pericardium from surface of right atrium and posterior wall was not resected. Histopathology of pericardium revealed dystrophic calcification without any evidence of granulomatous or giant cell inflammation. Mycobacterial and fungal cultures of the excised pericardium were negative. He had uneventful recovery and was discharged on 7th post-operative day. A post–operative CT scan showed absence of calcified pericardium along antero-lateral surface of the heart (Figures 2C and D). He remained asymptomatic during 1-year follow-up.
Constrictive pericarditis is a sequale of chronic inflammation of pericardium. Among the various etiologies, idiopathic type is a common cause for CP[1,2], which was present in index case. The clinical presentation is mostly of right heart failure. Any patient presented with dyspnea, raised jugular venous pulse, hepatic and systemic venous congestion should be evaluated for CP. Pericardial calcification in chest X-ray can suggest CP, however it is present in only 5%-27% of cases[3]. Extensive “eggshell” like calcification is rarely seen in CP[4], as was present in index case. Echocardiography is an initial imaging test for diagnosis of CP[5]. In patients with equivocal echocardiography findings, CT or Cardiac Magnetic Resonance can confirm the diagnosis[5]. The extent of severe calcification and involvement of adjacent structures is clearly defined by CT, as demonstrated in index case. Cardiac catheterization is required for hemodynamic assessment and to rule out coronary compression by calcified thickened pericardium[6]. A multi-modality imaging and hemodynamic assessment is essential for proper evaluation of CP[5]. Surgical pericardiectomy is the definite treatment for CP. Those with calcified and firmly adherent pericardium, median thoracotomy is preferred over antero-lateral thoracotomy[7]. Calcified CP also has higher surgical risk, incomplete pericardial resection and poor hemodynamic outcomes following surgery[7]. However, index case had a successful outcome following partial antero-lateral pericardiectomy via median sternotomy approach. In conclusion, we present a case of idiopathic CP with extensive eggshell calcification of the heart, who had successful surgical pericardiectomy, and had a favourable long term outcome.
A 43-years-old male presented with shortness of breath, New York Heart Association class-III of 6-mo duration.
Clinical examination revealed a raised jugular venous pulse with prominent X and Y descents.
Cardiac auscultation revealed a pericardial knock. Two-dimensional echocardiogram showed 10-mm thick, calcified pericardium with significant trans-mitral diastolic flow velocities variation.
Fluoroscopy revealed dense circumferential calcification all around the heart. A computed tomography scan confirmed the circumferential thick pericardial calcification like an eggshell, encircling the heart. Cardiac catheterization revealed near equalization of elevated right atrial, right ventricle, and left ventricle end-diastolic pressures and ventricular pressure tracing showed typical “dip-and-plateau” pattern suggestive of constrictive pericarditis.
He had surgical pericardiectomy for densely calcified CP. Histopathology of pericardium revealed dystrophic calcification without any evidence of granulomatous or giant cell inflammation. An importance of multi-modality imaging with hemodynamic assessment is discussed in management of constrictive pericarditis.
This is an interesting article on calcified constrictive pericarditis. The paper is nicely documented.
P- Reviewer: Durandy Y, Lymperopoulos A, Mehta JL S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | LeWinter MM, Hopkins WE. Pericardial diseases. Braunwald’s heart disease. 10th Edition. WB: Saunders publications 2015; 1636-1657. |
| 2. | Cameron J, Oesterle SN, Baldwin JC, Hancock EW. The etiologic spectrum of constrictive pericarditis. Am Heart J. 1987;113:354-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 146] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Ling LH, Oh JK, Breen JF, Schaff HV, Danielson GK, Mahoney DW, Seward JB, Tajik AJ. Calcific constrictive pericarditis: is it still with us? Ann Intern Med. 2000;132:444-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Yetkin U, Ilhan G, Calli AO, Yesil M, Gurbuz A. Severe calcific chronic constrictive tuberculous pericarditis. Tex Heart Inst J. 2008;35:224-225. [PubMed] |
| 5. | Klein AL, Abbara S, Agler DA, Appleton CP, Asher CR, Hoit B, Hung J, Garcia MJ, Kronzon I, Oh JK. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013;26:965-1012.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 451] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 6. | Robb JF, Laham RJ, Moscucci M. Profile in pericardial disease. Grossman & Baim’s cardiac catheterization, angiography and intervention. 8th Edition. Lippincott Williams & WilkinsL: Wolters Kluwer publications 2014; 1045-1059. |
| 7. | Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 847] [Cited by in RCA: 764] [Article Influence: 36.4] [Reference Citation Analysis (0)] |