Published online Jul 26, 2015. doi: 10.4330/wjc.v7.i7.373
Peer-review started: January 27, 2015
First decision: February 7, 2015
Revised: April 13, 2015
Accepted: May 7, 2015
Article in press: May 8, 2015
Published online: July 26, 2015
Processing time: 192 Days and 10.3 Hours
The advent of ambulatory blood pressure monitoring permitted examination of blood pressures during sleep and recognition of the associated circadian fall in pressure during this period. The fall in pressure, called the “dip”, is defined as the difference between daytime mean systolic pressure and nighttime mean systolic pressure expressed as a percentage of the day value. Ten percent to 20% is considered normal. Dips less than 10%, referred to as blunted or absent, have been considered as predicting an adverse cardiovascular event. This view and the broader concept that white coat hypertension itself is a forerunner of essential hypertension is disputable. This editorial questions whether mean arterial pressures over many hours accurately represent the systolic load, whether nighttime dipping varies from measure to measure or is a fixed phenomenon, whether the abrupt morning pressure rise is a risk factor or whether none of these issues are as important as the actual night time systolic blood pressure itself. The paper discusses the difference between medicated and nonmedicated white coat hypertensives in regard to the cardiovascular risk and suggests that further work is necessary to consider whether the quality and duration of sleep are important factors.
Core tip: While the blunted or absent nighttime pressure dip in nonmedicated white coat hypertensives is generally believed to be a predictor of adverse cardiovascular events, it does not appear to present the same risk in medicated white coat patients. Of the many measurable pressure issues, including pulse pressure and morning surge, during sleep and with awakening, only the mean systolic pressure appears to be the predictor of risk.
- Citation: Bloomfield D, Park A. Night time blood pressure dip. World J Cardiol 2015; 7(7): 373-376
- URL: https://www.wjgnet.com/1949-8462/full/v7/i7/373.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i7.373
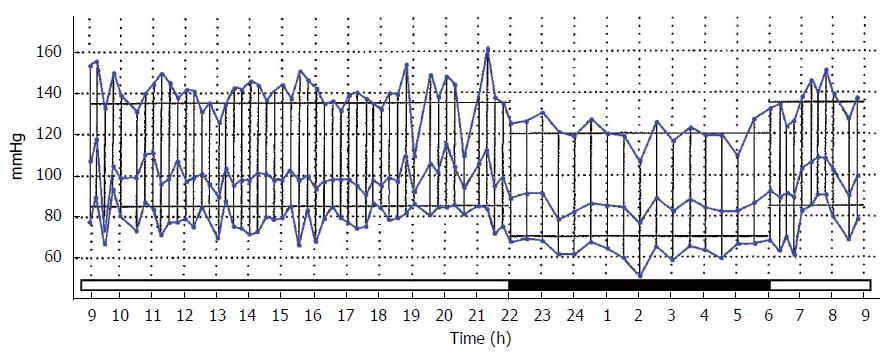
The circadian fall in blood pressure during sleep[1] has been fully examined only since the development of ambulatory blood pressure monitoring (ABPM) and its occurrence in white coat hypertension (WCH) has not been generally elucidated. First described in 1988, the night time dip has become an accepted measure of cardiovascular risk[1-4]. The dip is defined as the difference between the mean systolic pressure in the day and mean systolic pressure during the night, expressed as a percentage of the day time mean, with the accepted normal between 10% and 20%[5]. A representative ABPM tracing with a normal night time dip is shown in Figure 1.
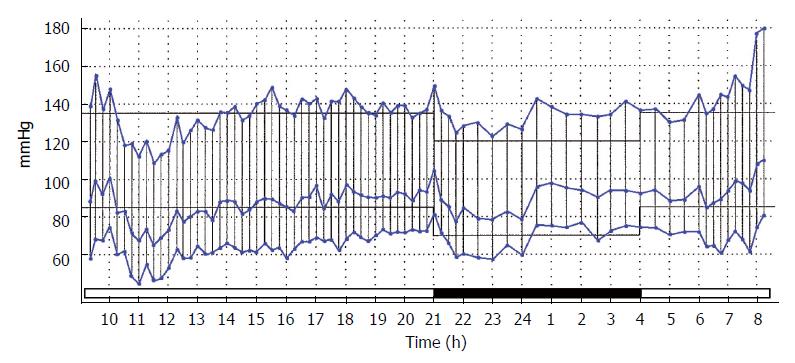
Dips less than 10% are described as absent or blunted and those in excess of 20% are known as exaggerated or extreme[6]. An example of a blunted dip, such as would be recognized as predicting an adverse cardiovascular event, is shown in Figure 2.
Identification of medical risk factors, particularly cardiovascular ones, carries a couple of requirements. The definition of the conditions must be accepted and unchallengeable and the observations on which this designation is based must be unassailable. These conditions are not met with the night time dip.
The utility of the definition of night time dip is far from practical. It is assumed that the mean systolic pressures are utilized but there is such variation in the actual systolic values during the 24 h that the mean hides much information and bears little relationship to actual daily events. The utilization of average or maximum systolic pressures would be equally inaccurate. In white coat hypertension, mean and average systolic pressures are artificially elevated by the white coat episode.
The ambulatory monitoring data is also soft. It is known that repeated studies do not necessarily provide the same result. Dippers may become non dippers on subsequent testing[7].
Furthermore, the patient-designated “time of sleep” is actually the time of going to bed. The true time of falling asleep clearly cannot be indicated with this methodology. Consequently, the pressures used in the sleep vs awake calculations are slightly but inherently inaccurate.
Reported studies in night time dip have almost always been performed in untreated hypertensive patients[8]. In the real world, ABPM is rarely performed in such patients. In our experience, patients are referred for this study to ascertain the effectiveness of the treatment or when progressive medication has failed to control the hypertension. It would be expected that cardiovascular risks would be more evident in the uncontrolled hypertensive patients, however, our studies with medicated patients[8] have shown no greater incidence of blunted night time dip in uncontrolled hypertensives, controlled hypertensives or white coat hypertensives. Sufficient reduction in the night time pressure may in fact be blunted or negated by protective reflexes if these pressures are already reduced by medication.
Over bridging these considerations is the understanding that the cardiovascular risk associated with the rupture of atheromatous plaques in the coronary and cerebral arteries are essentially systolic issues. They may be related to actual systolic levels or pulse pressure rather than mean pressures or degree of nocturnal dipping.
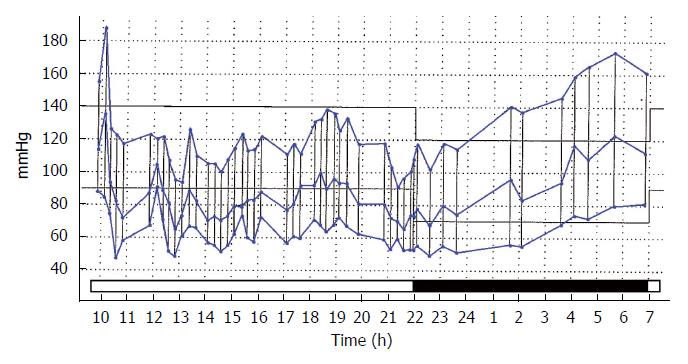
Masked hypertension, the condition in which the home or the ABPM pressures are significantly higher than the office values must be given considerations here. It is seldom diagnosed in clinical practice as there is little incentive to prescribe ABPM or home pressure devices if the pressure is normal, but occasionally, accidental or incidental incidences of blood pressure measurement may reveal this condition and some explanation is required when masked hypertension is revealed during sleep. This may eliminate the night time dip. Night time narrow peaks of systolic hypertension can occur with dreaming, wider systolic elevations with obstructive sleep apnea and steadily rising pressures are seen with essential hypertension (Figure 3).
A widened pulse pressure has also been recognized as an indicator of cardiovascular risk. White coat hypertensives have a widened pulse pressure during the white-coat episodes but not at night. Analysis of our studies in dippers and non-dippers, hypertensives, white coaters and normal subjects, has found that there is no statistical difference in pulse pressure values between day and night. With the exception of isolated systolic hypertension, a widened pulse pressure occurs in patients who do not have elevated blood pressure as their principle diagnosis and includes those with aortic regurgitation, arteriovenous shunts, thyrotoxicosis and other cardiovascular disorders that, in themselves, increase the risk of death.
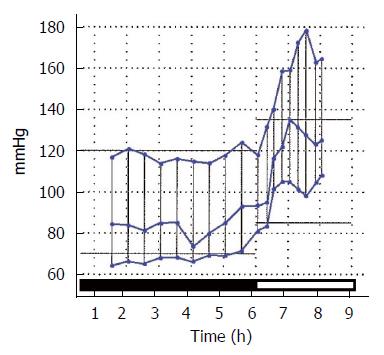
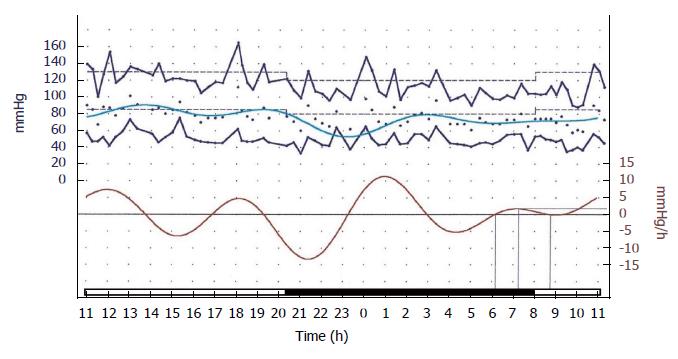
Associated with the night time dip, the morning blood pressure surge has been blamed for the increase in cardiovascular events in the morning hours. It is measured as mmHg increase per hour in the mean pressure and it is generally accepted that a rise greater that 10 is significant as a cardiovascular risk factor. Figure 4 shows a typical exaggerated increase in the pressure during the process of awakening.
However, when the rate of rise is continuously calculated during the 24 h ABPM recording, many instances of “significance” are seen to occur at times other than in the morning. Figure 5 adequately depicts this point.
A large study has found that the night time systolic pressure itself, rather than the surge, the dip or the pulse pressure has been shown to correlate more closely with the clinical events[9].
It is clear that the blood pressure at night, in some negative way, impacts the cardiovascular system. What particular element of the pressure, whether it is its depth or its systolic/diastolic width or whether the heart rate or length or quality of sleep is the causative factor remains to be determined.
Unfortunately, the tool to answer these questions, the ambulatory blood pressure monitor, is underutilized in the United States, largely because the study remains non-reimbursable. As it may hold some basic but unknown secrets of cardiovascular health and disease, the “night time dip” warrants a much more extensive investigation.
P- Reviewer: Artunc F, Dizon JM, Patanè S S- Editor: Ji FF L- Editor: A E- Editor: Wang CH
| 1. | Koroboki E, Manios E, Psaltopoulou T, Vemmos K, Michas F, Alexaki E, Zakopoulos N. Circadian variation of blood pressure and heart rate in normotensives, white-coat, masked, treated and untreated hypertensives. Hellenic J Cardiol. 2012;53:432-438. [PubMed] |
| 3. | Mousa T, el-Sayed MA, Motawea AK, Salama MA, Elhendy A. Association of blunted nighttime blood pressure dipping with coronary artery stenosis in men. Am J Hypertens. 2004;17:977-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Bellelli G, Frisoni GB, Lucchi E, Guerini F, Geroldi C, Magnifico F, Bianchetti A, Trabucchi M. Blunted reduction in night-time blood pressure is associated with cognitive deterioration in subjects with long-standing hypertension. Blood Press Monit. 2004;9:71-76. [PubMed] |
| 5. | Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8787] [Cited by in RCA: 8985] [Article Influence: 408.4] [Reference Citation Analysis (0)] |
| 6. | Kario K, Schwartz JE, Pickering TG. Changes of nocturnal blood pressure dipping status in hypertensives by nighttime dosing of alpha-adrenergic blocker, doxazosin: results from the HALT study. Hypertension. 2000;35:787-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 114] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Delaney A, Pellizzari M, Speiser PW, Frank GR. Pitfalls in the measurement of the nocturnal blood pressure dip in adolescents with type 1 diabetes. Diabetes Care. 2009;32:165-168. [PubMed] |
| 8. | Yogendran L, Abdelqader A, Mohamed M, Schuler T, Bloomfield D. Nighttime Pressure Dip in White Coat Hypertension. J Heart Disease. 2014;11:72. |
| 9. | Hermida RC, Moya A, Crespo JJ, Otero A, Dominguez M, Rios MT, Castineira C, Mojon A, Fernandez JR, Ayala DE. Asleep blood pressure is an independent predictor of cardiovascular events: the Hygia project. J Heart Disease. 2014;11:36. |