Published online May 26, 2015. doi: 10.4330/wjc.v7.i5.293
Peer-review started: December 4, 2014
First decision: December 26, 2014
Revised: January 16, 2015
Accepted: March 4, 2015
Article in press: March 5, 2015
Published online: May 26, 2015
Processing time: 168 Days and 18.9 Hours
Myocarditis is a bacterial or viral inflammatory disease, often unnoticed or misdiagnosed. Athletes with myocarditis must stop practicing their activity since International medical Literature described some cases of sudden death. In the present report, we describe a case of an asymptomatic, apparently healthy, competitive athletes, who was diagnosed a myocarditis and as incidental finding a myocardial bridging. We focused the attention on the importance of anamnesis, electrocardiogram and athletes’ entourage for the diagnosis of such insidious pathologies and we evaluated the follow up, focusing the attention on electrocardiogram changes as well as on restitution ad integrum and prognosis, especially for the athletes.
Core tip: Pre participation screening allows sports physicians to diagnose potential causes of sudden death in athletes. We describe a case of an athlete with a previous myocarditis, and an incidental myocardial bridging, suspended from competition and followed in the later time. We also pointed out the question of the possible scarring of myocarditis in relation to the restart of physical activity and training.
- Citation: Quaranta F, Guerra E, Sperandii F, Santis FD, Pigozzi F, Calò L, Borrione P. Myocarditis in athlete and myocardial bridge: An innocent bystander? World J Cardiol 2015; 7(5): 293-298
- URL: https://www.wjgnet.com/1949-8462/full/v7/i5/293.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i5.293
Myocarditis is an inflammatory disease of the myocardium, possibly determined by both bacterial and viral infections. Coxsackievirus B, enteroviruses adenovirus and parvovirus B19 are often involved in acute processes[1]. Myocardial involvement caused by granulomatous or (auto) immune processes with unknown pathogenetic mechanisms, but this is less common than virus-induced myocarditis or post-infectious inflammatory cardiomyopathy.
Myocarditis is frequently anticipated by flu-like signs and symptoms like chills, fever, headache, muscle aches, general malaise. Moreover, gastrointestinal symptoms such as decreased appetite, nausea, vomiting, and diarrhoea are commonly reported. Cardiac signs and symptoms may appear a few hours to a few days since the beginning of myocardial inflammation and consist in chest pain, palpitations, dyspnea, hypotension, gallop rhythm, rales, jugular venous dilatation, and cardiac tamponade.
In rare cases, the inflammatory condition causes acute hemodynamic compromise, possibly leading to heart failure, complex arrhythmias and fatal events[2]. In reported cases, Myocarditis scenario can overlap Ischemic disease[3], and acute coronary syndrome, even an ST-segment elevation myocardial infarction.
Nevertheless, myocarditis can be undiagnosed and completely asymptomatic with not perceived short lasting fever (5-7 d).
In the absence of structural heart diseases myocarditis accounts for approximately 10% of recent-onset cardiomyopathy in adults. Early fulminant disease is still associated with a high mortality rate. Patients who survive the critical phase have a fairly good prognosis and survival from myocarditis is approximately 60%-70%. In the remaining patients progressive chronic heart failure and unpredictable sudden cardiac death remain a serious concern, often occurring years after the initial clinical event and sometimes despite complete recovery of the myocardial function.
Diagnosis is commonly carried out by integrating different methods[4].
Electrocardiogram (ECG): a sensitive cheap tool of diagnosis. Abnormal ST-T waves and conduction block are frequently observed in myocarditis as well as isolated or complex/polymorphic ventricular arrhythmias present at rest or during stress test[5]. A gradual increase in the width of the QRS complex can be a sign of exacerbation of myocarditis. Continuous ECG monitoring is crucial to detect arrhythmic burden and presence of threatening rhythm disorder.
Echocardiography: in case of echo alterations, myocarditis can be confirmed by transient wall thickening, reduced wall motion and reduced cardiac chamber size in addition to pericardial effusion on echocardiography and increase of echo reflection[6].
Cardiac magnetic resonance imaging (MRI): in addition to the cinematic mode on MRI, T1-weighted early signal enhancement and gadolinium-delayed imaging of the heart are useful to make a diagnosis of myocarditis[7]. T2-weighted images reveal the regions of the heart affected by inflammation. Cardiac magnetic resonance (CMR) has emerged as a leading modality in the noninvasive diagnosis of myocarditis due to its ability to detect myocardial edema, hyperaemia, necrosis and fibrosis in a safe and reproducible fashion. The presence of late enhancement gadolinium (LGE) has been reported in 24%-95% of patients with myocarditis, typically being multifocal and located in the epicardium of the lateral wall and mid wall of the septum. Moreover, the long term prognosis can be determined by the magnitude of damage at MRI, since the left ventricle end diastolic volume, the presence of LGE in the septum and the total amount of LGE are the strongest independent predictors of impaired ventricular function and ventricular dilatation at follow up[8].
Blood Biochemistry: during the acute phase of myocarditis, it is possible to observe a plasma increased elevation of C-reactive protein, aspartate aminotransferase, lactate dehydrogenase, MB form of creatine kinase, and cardiac troponin T[9].
Other techniques may include computed tomography (CT) of the heart to assess possible artery disease[2,10], chest X-ray (qualitative quick assessment of cardiac enlargement and pulmonary congestion); cardiac catheterization, including endomyocardial biopsy (the gold standard for diagnosis but an invasive method not risk free and usually performed only after the acute phase and in clinical stability of the patient)[11].
Myocarditis is reported as a cause of Sudden death in athletes[2].
Italian guidelines for the pre-participation screening sustain that “subjects with certain diagnosis of myocarditis cannot be involved in any kind of sport activity, until the illness process is completely resolved, and however not before of at least 6 mo since the diagnosis was made. The competitive sport activity can be restarted only if clinical evaluation and instrumental evaluations demonstrate the lack of alterations in myocardial contractile function as well as the absence of relevant arrhythmias”[12].
A 41-year-old male, regularly involved in competitive sport (American football and weightlifting) came, on march 2013, to our Sport’s Medicine laboratory, for the annual mandatory pre-participation screening. Football screening protocol include Cardiological examination, basal ECG, Stress Test. Family and personal history was negative. Clinical examination was unremarkable.
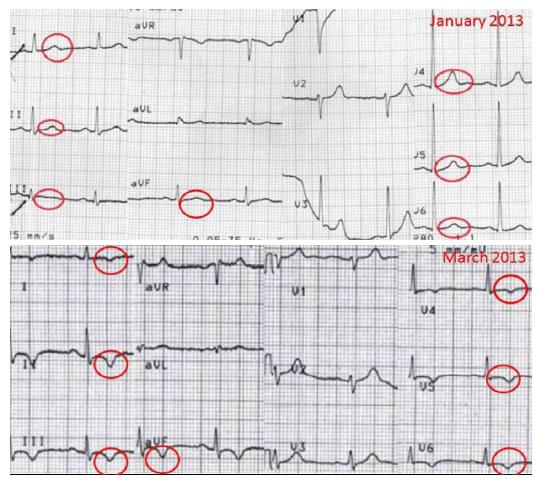
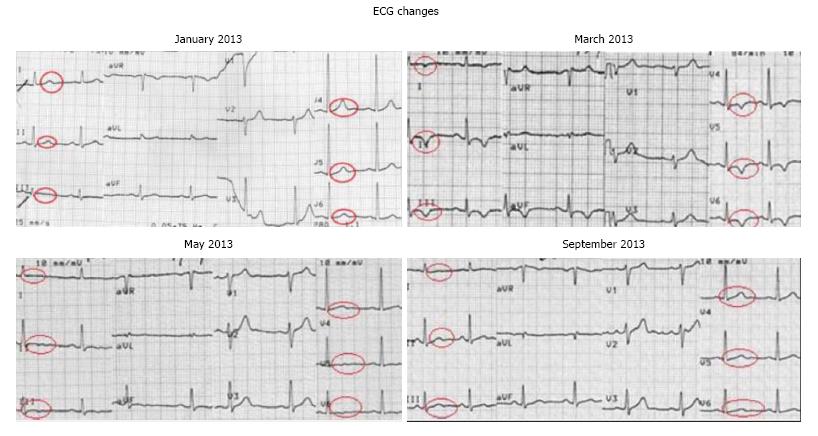
Rest-ECG showed deep T-wave inversion in ≥ 2 contiguous anterior, inferior or lateral leads, particularly in leads I, II, III, aVF and in V4-V5-V6. This pattern was absent in all the previous ECGs the patient made for previous screening, and in particular it was absent recently, when he underwent job medical exam (ECG January 2013) (Figure 1).
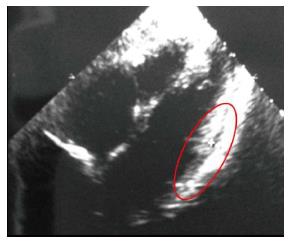
The patient underwent echocardiography which showed a mild echo-free space with pericardial effusion in the lateral wall and a slight increase in the hyper echogenicity level of the lateral portion of the left ventricle (Figure 2).
As the patient was completely asymptomatic and actually training and competing a cardiac exercise stress test was performed. T-waves inversion was stable all along the duration of the test. Patient reached 168 beats per minute at peak exercise heart rate and 200 watt of peak mechanical Power. Blood pressure kinetics was normal. No presence of Arrhythmias. No symptoms were reported. Holter ECG monitoring showed absence of ventricular arrhythmias.
The patients underwent through blood examination and biochemistry, which didn’t show any alterations.
Through anamnesis the patient remembered having experienced a “persistent flu” on January 2013, characterized by elevated fever (40 °C) and atypical chest pain which he considered aspecific and not to be referred to his General practitioner, for several days. He was administered a broad-spectrum antibiotic therapy (Cephalexin) and symptoms completely disappeared within 4 d.
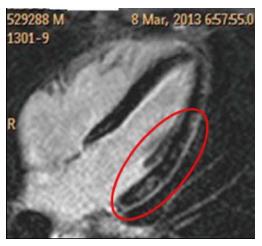
As a third level examination we performed a cardiac MRI which showed the presence of some areas of intramural and subepicardial delayed enhancement in the lateral wall, suggestive of fibrosis, in a contest of normal dimensions and function (Figure 3). The characteristic pattern of LGE in myocarditis is patchy or multifocal in a subepicardial or intramyocardial distribution, often involving the lateral wall. This feature is not pathognomonic but is clearly distinct from ischemic heart disease, which typically presents with subendocardial or transmural LGE within a coronary artery territory.
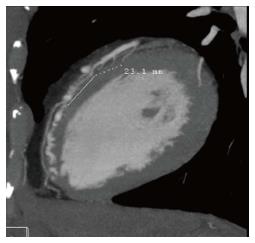
Despite it, considering the age of the athlete and possible overlapping with ischemic disease even if in absence of wall abnormalities at echo scan of the heart, we excluded coronary involvement through a CT scan of coronary arteries. As a collateral finding a coronary abnormal 23 mm superficial intramiocardial course in the medium tract of Left descending artery was found.
The intramuscular course of coronary arteries can be detected and characterized by Computed Coronary Tomographic Angiography (CCTA). CCTA is an easy and reliable tool for comprehensive in vivo diagnosis of the intramuscular course of coronary arteries. It is generally estimated that the myocardial bridging can be detected in about one-third of the adults in autopsy series, whereas the reported incidence in angiographic series is much lower < 5%. The incidence of myocardial bridging in CCTA studies (30.5%) is in concordance with the reported incidence in autopsy series[13].
We concluded for Myocarditis in association with incidental finding of Myocardial bridge (Figure 4).
According to cardiologic Italian guidelines for competitive sports, we recommended to avoid physical overload and sport practice. A therapy with low dose Bisoprolol was started and a follow up was based on monthly ECG and a repetition of echocardiography and stress-test at three months’ time.
T wave inversion pattern showed a gradual reduction in amplitude up to complete reversal after 4 mo (Figure 5).
Echocardiogram performed in October 2013 was normal and no sign of effusion was present. Stress test was within normal limits and no repolarization abnormalities could be found.
Clinical evaluation, normalization of basal ECG and echocardiogram demonstrated the complete electrical recovery of the athlete from myocarditis. He continued to be excluded from competitive sports, according to cardiologic Italian guidelines for competitive sports for the presence of intramiocardial Coronary bridge.
After one year of follow up the patient did not experience any cardiological symptoms, clinical examination was unremarkable and electrocardiographic and echocardiographic findings as well as stress test were within normal limits.
Myocarditis is a rare recognised cause of sudden death in athletes, its signs and symptoms may overlap ischemic disease as well as cardiomyopathy and it can be minimally symptomatic or able to determine rare fatal events[14]. Even in asymptomatic subjects, recognition of this disease can modify prognosis since inflammatory cardiomyopathy can determine adverse event also many years after apparently total restitution ad integrum, this is the reason why indication for clinical follow up and for adequate exercise prescription can change the patient “scenario”.
Intramiocardial bridge is a recognised cause of sudden death in athletes too[15]. The prevalence of this abnormality shows a wide range of frequency, up to 44% with 64-slice coronary CT scan[16]. In the last years Computed Scan has allowed diagnosis even in asymptomatic subjects. This finding requires, accordingly to cardiological Italian guidelines for competitive sports, to avoid competition and high intensity training.
With this report, we firstly intend to remark the relevance of anamnesis and combined techniques such as basal ECG[17], echocardiography, MRI and Computed Scan of the heart, in the diagnosis or exclusion of myocarditis when clearing athletes for competition. ECG is reported to be normal in over 32% of subjects with acute myocarditis. This can also be due to the time at which the ECG is performed, for the transitory nature of abnormalities[18]. MRI has a sensitivity of 81%, specificity of 71% and accuracy of 81% for diagnosing acute myocarditis[5].
Moreover, T wave inversion were in the same location of increased echo reflex and in proximity of mild echo free area interpreted as mild pericardial effusion, in lateral portion of left ventricle. Such data was also confirmed at MRI and at Computed Scan of the heart, with no sign of oedema, but with presence of fibrosis, indicating a past inflammatory based necrosis. This information is crucial to possibly diagnose Myocarditis as well as for the prognosis.
Secondly, we would like to underline the importance of a proper dialogue between sport physicians and the athletes, the medical team and even, in some cases, the family doctor. A focal point is that even if mandatory pre-participation screening in our country is annually based, it seems essential that sports physicians recommend to re-evaluate athletes experiencing persistent flues or not common signs and symptoms such as atypical thoracic pain, asthenia and palpitations. This information is to be extended to athletes and general practitioner.
According to actual Italian guidelines, a period of 6 mo following restitution ad integrum is sufficient to be again eligible for sport competition. With MRI, myocardial damage, previously not detected can be well appreciated as fibrosis or sub epicardial or intramural damage.
It seems important to note that the presence of delayed enhancement and fibrosis is not considered as a risk predictor in previous Italian Cardiological Guidelines for pre participation screening, in fact a complete reversal of T waves abnormalities, with preserved function and absence of symptoms and arrhythmias is considered sufficient for a restitution and integrum. Are now this concept still valid? Which is the role of Myocardial scar in determining a good prognosis? Is an ECG reversal to normality also a sign of better prognosis?
The athlete during the pre-participation screening was asymptomatic, he reported elevated fever (40 °C), atypical chest pain with asthenia and persistent flu, 2 mo before.
The athlete, with a previously normal electrocardiogram (ECG), showed T wave inversion in most leads, after a “persistent flu” with elevated fever 2 mo later.
Differential diagnosis with myocardial infarction was performed through computed tomography (CT) scan which didn’t show coronary artery disease as well as through echocardiography which showed normal systolic function.
The patient underwent blood examination (C-reactive protein, aspartate aminotransferase, lactate dehydrogenase, MB form of creatine kinase, and cardiac troponin T) which didn’t show any alterations.
The authors performed the following instrumental examinations: (1) ECG: T wave inversion in leads I, II, III, aVF and in V4-V5-V6; (2) Echocardiogram: mild echo-free space with pericardial effusion in the lateral wall and a slight increase in the hyper echogenicity level of the lateral portion of the left ventricle; (3) magnetic resonance imaging (MRI): areas of intramural and subepicardial delayed enhancement in the lateral wall, suggestive of fibrosis; and (4) CT scan: coronary abnormal 23 mm superficial intramiocardial course in the medium tract of left descending artery.
The authors didn’t perform any histological examination.
After the detection of the intramyocardial bridge the authors started a therapy with low dose bisoprolol and the authors suspended the athlete from competition and training. A monthly follow up was started.
Pre participation screening is the annual medical evaluation mandatory for competitive athlete in Italy.
It would be desirable that sports physicians recommend to re-evaluate athletes experiencing persistent flues or not common signs and symptoms such as atypical thoracic pain, asthenia and palpitations, during the sports season; this information is to be extended to athletes and general practitioner.
This case report highlights the importance of anamnesis and 12 leads ECG examination for the athletes in diagnosis of subtle transitory myocardial alterations due to infections. Moreover, despite a normalization of ECG during follow up, after a myocarditis, the authors emphasized the eventuality to focus on the possibility of myocardial scars, which can be easily detected with MRI.
P- Reviewer: Cosmi E, Dominguez-Rodriguez A, Petix NR S- Editor: Tian YL L- Editor: A E- Editor: Lu YJ
| 1. | Bowles NE, Ni J, Kearney DL, Pauschinger M, Schultheiss HP, McCarthy R, Hare J, Bricker JT, Bowles KR, Towbin JA. Detection of viruses in myocardial tissues by polymerase chain reaction. evidence of adenovirus as a common cause of myocarditis in children and adults. J Am Coll Cardiol. 2003;42:466-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 421] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 2. | Maron BJ, Haas TS, Murphy CJ, Ahluwalia A, Rutten-Ramos S. Incidence and causes of sudden death in U.S. college athletes. J Am Coll Cardiol. 2014;63:1636-1643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 227] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 3. | Costantini M, Oreto G, Albanese A, Ranieri A, De Fabrizio G, Sticchi I, Lauretti A, Capone S, Tritto C, Fachechi C. Presumptive myocarditis with ST-Elevation myocardial infarction presentation in young males as a new syndrome. Clinical significance and long term follow up. Cardiovasc Ultrasound. 2011;9:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636-2648, 2648a-2648d. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 2270] [Article Influence: 189.2] [Reference Citation Analysis (0)] |
| 5. | Zhang J, He S, Qi X, Li Y. Combined electrocardiography, coronary angiography and magnetic resonance imaging for the diagnosis of viral myocarditis: A case report. Exp Ther Med. 2014;7:1643-1646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Hiramitsu S, Morimoto S, Kato S, Uemura A, Kubo N, Kimura K, Sugiura A, Itoh T, Hishida H. Transient ventricular wall thickening in acute myocarditis: a serial echocardiographic and histopathologic study. Jpn Circ J. 2001;65:863-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Abdel-Aty H, Boyé P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D, Bock P, Dietz R, Friedrich MG, Schulz-Menger J. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. 2005;45:1815-1822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 574] [Cited by in RCA: 546] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 8. | Panovsky R, Pleva M, Feitova V, Kruzliak P, Meluzin J, Kincl V. The prognostic impact of myocardial late gadolinium enhancement. Cardiol Rev. 2014;22:128-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Lauer B, Niederau C, Kühl U, Schannwell M, Pauschinger M, Strauer BE, Schultheiss HP. Cardiac troponin T in patients with clinically suspected myocarditis. J Am Coll Cardiol. 1997;30:1354-1359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 293] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 10. | di Cesare E, Carbone I, Carriero A, Centonze M, De Cobelli F, De Rosa R, Di Renzi P, Esposito A, Faletti R, Fattori R. Clinical indications for cardiac computed tomography. From the Working Group of the Cardiac Radiology Section of the Italian Society of Medical Radiology (SIRM). Radiol Med. 2012;117:901-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, Levine GN, Narula J, Starling RC, Towbin J. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. J Am Coll Cardiol. 2007;50:1914-1931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 467] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 12. | Federazione Medico Sportiva Italiana; Protocolli cardiologici per il giudizio di idoneità allo sport agonistico 2009. Available from: http://www.ancecardio.it/it/doc/1295659063996_COCIS2009.pdf. |
| 13. | Konen E, Goitein O, Sternik L, Eshet Y, Shemesh J, Di Segni E. The prevalence and anatomical patterns of intramuscular coronary arteries: a coronary computed tomography angiographic study. J Am Coll Cardiol. 2007;49:587-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 14. | Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA. 1996;276:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1038] [Cited by in RCA: 905] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 15. | Basso C, Thiene G, Mackey-Bojack S, Frigo AC, Corrado D, Maron BJ. Myocardial bridging, a frequent component of the hypertrophic cardiomyopathy phenotype, lacks systematic association with sudden cardiac death. Eur Heart J. 2009;30:1627-1634. [PubMed] |
| 16. | Nakanishi R, Rajani R, Ishikawa Y, Ishii T, Berman DS. Myocardial bridging on coronary CTA: an innocent bystander or a culprit in myocardial infarction? J Cardiovasc Comput Tomogr. 2012;6:3-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 104] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Borrione P, Quaranta F, Ciminelli E. Pre-participation screening for the prevention of sudden cardiac death in athletes. World J Methodol. 2013;3:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (2)] |
| 18. | Di Bella G, Florian A, Oreto L, Napolitano C, Todaro MC, Donato R, Calamelli S, Camastra GS, Zito C, Carerj S. Electrocardiographic findings and myocardial damage in acute myocarditis detected by cardiac magnetic resonance. Clin Res Cardiol. 2012;101:617-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |