Published online May 26, 2015. doi: 10.4330/wjc.v7.i5.287
Peer-review started: September 17, 2014
First decision: October 14, 2014
Revised: January 4, 2015
Accepted: March 30, 2015
Article in press: April 2, 2015
Published online: May 26, 2015
Processing time: 249 Days and 14 Hours
AIM: To compare the predictive value of three methods of epicardial fat (EF) assessment for presence of significant coronary artery disease (CAD) [i.e., epicardial fat volume (EFV), EFV indexed with body surface area (EFV/BSA) and EFV indexed with body mass index (EFV/BMI)].
METHODS: The study was performed on 170 patients (85 women and 85 men) with clinical suspicion of CAD. They aged 26-89 years with a median age of 54 years. The patients were classified into three groups: Group 1: 58 patients with normal coronary arteries; group 2: 48 patients with non-significant CAD and group 3: 64 patients with significant CAD. The three methods for assessment of epicardial fat were retrospectively studied to determine the best method to predict the presence of significant CAD.
RESULTS: The three methods for epicardial fat quantification and measurements, i.e., EFV, EFV/BSA and EFV/BMI with post- hoc analysis showed a significant difference between patients with significant coronary artery disease compared to the normal group. Receiver operating characteristic curve analysis showed no significant difference between the three methods of epicardial fat measurements, the area under curve ranging between 0.6 and 0.62. The optimal cut-off was 80.3 cm3 for EFV, 2.4 cm3/m2 for EFV indexed with BMI and 41.7 cm3/(kg/m2) for EFV indexed with BSA. For this cut-off the sensitivity ranged between 0.92 and 0.94, while specificity varied from 0.31 to 0.35.
CONCLUSION: Any one of the three methods for assessment of epicardial fat can be used to predict significant CAD since all have the same equivalent predictive value.
Core tip: There is a great correlation between the volume of epicardial fat and presence of significant coronary artery disease. There are different methods for quantification of epicardial fat volume (EFV). The aim of the study is to compare the predictive value of the three methods used for quantification of epicardial fat (EFV, EFV indexed with body surface area and EFV indexed with body mass index) for presence of significant coronary artery disease. The study concluded the three methods for assessment of epicardial fat have the same equivalent predictive value for significant coronary artery disease and any one of them can be used as a sensitive predictor for significant coronary artery disease.
- Citation: Saad Z, El-Rawy M, Donkol RH, Boghattas S. Quantification of epicardial fat: Which method can predict significant coronary artery disease? World J Cardiol 2015; 7(5): 287-292
- URL: https://www.wjgnet.com/1949-8462/full/v7/i5/287.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i5.287
Epicardial fat (EF) is the visceral fat of the heart deposited under the visceral layer of the pericardium. Under normal physiological conditions, EF tissue displays biochemical, mechanical and thermogenic cardioprotective properties. Under pathological circumstances, EF can be strongly related to the development of coronary artery disease (CAD). The accumulation of EF is known to be a rich source of free fatty acids and a number of proinflammatory cytokines[1-3].
It has been hypothesized that EF may act as a paracrine (immunological) organ that influences the coronary arteries by promoting chronic inflammation and endothelial dysfunction[4-6].
Several imaging modalities can be used to quantify EF volume (EFV) such as echocardiography, computed tomography, and magnetic resonance imaging[7]. Due to distinct low attenuation values of fat on computed tomography (CT). ECG-gated cardiac CT with its high spatial resolution and true volume coverage of the heart, allows accurate measurement of epicardial and thoracic fat distances and volumes[6,7].
Besides EFV, some authors derived a second parameter, the body surface area indexed EFV (EFV/BSA)[8,9]; however, comparison between these two parameters has not been considered. Moreover, despite the predictive value of higher body mass index for cardiovascular event[10,11], the added value of body mass index (BMI)-adjusted EFV (EFV/BMI) also has not been previously assessed as well.
The aim of the current study is to compare the predictive value of the three methods for EF assessment (EFV, EFV/BSA and EFV/BMI) for presence of significant CAD.
A total of 170 consecutive patients with clinical suspicion of coronary artery disease (CAD) aged 26-89 years with a median age of 54 years (85 women and 85 men) were included in our study From November 2012 through February 2014. Patients underwent 128-MDCT according to appropriate use criteria for cardiac computed tomography[12]. All participants provided written informed consent and the study was approved by institutional ethics committee.
The patients were divided into 3 groups according to the severity of coronary artery stenosis assessed by quantitative coronary angiography. Patients in group 1 have normal coronary arteries. Patients in group 2 were have non-significant coronary artery stenosis with percent-diameter stenosis less than 50%. Patients in group 3 have significant CAD with percent-diameter stenosis more than 50% or occlusion[13].
Our patients were scanned with a 128-multidetector computed tomography (MDCT) dual source scanner (SOMATOM Flash; Siemens Medical Solutions, Erlangen, Germany). Patients with uncontrolled heart rate (> 65 beats per minute) received oral beta blocker (metoprolol 50 mg) before the CT scan. Sublingual nitroglycerin 0.5 mg was administrated before the scan to achieve coronary vasodilation. A non-contrast CT scan was performed to determine the total calcium burden of the coronary tree (sequential scan with 32 Å~ 0.6-mm collimation, tube current 60 mA at 120 kV). Contrast-enhanced CT angiography data were acquired with the use of a spiral scan with 32 Å~ 0.6-mm collimation, 330-ms gantry rotation, pitch of 0.2, and tube voltage at 120 kV.
Sequential ECG-triggering scans were performed in 142 patients with controlled heart rate and retrospective ECG-gating scans with tube current modulation were performed in 28 patients due to heart rate variability. Intravenous contrast agent (60-90 mL; 350 mg iodine/mL) was injected with flow rate of 5.0 mL/s followed by a 30-mL saline chaser[1].
Image interpretation: The total calcium score was calculated and interpretation of CCTA was analysed for all patients using commercially available software packages “Syngo Via”, Siemens Healthcare, Forchheim, Germany.
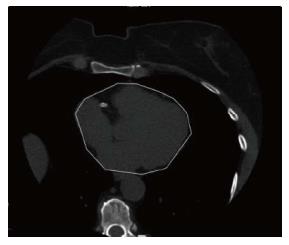
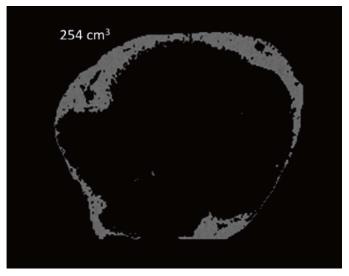
EFV was measured blindly by two observers for all patients using an offline workstation (Aquarius NetStation; TeraRecon Inc., San Mateo, CA). Using the 3.0-mm-thick axial slices used for calcium scoring, the parietal pericardium was traced manually in every 4th slice starting from the aortic root to the cardiac apex[1] (Figure 1). The computer software then automatically interpolated and traced the parietal pericardium in all slices interposed between the manually traced slices. The automatically traced slices were examined and verified for accuracy. Fat voxels were identified using threshold attenuation values of -30 to -190 HU (Figure 2).
Division the estimated EFV of every patient by patient’s BSA calculated the indexed EFV to BSA (EFV/BSA). Also, division of EFV by patient’s BMI calculated the indexed EFV to BMI (EFVB/MI).
The statistical analysis was performed by StatDirect 2.8.0 and Mecalc 9.2.1.0 (for ROC curve analysis and comparison). Because the analyzed quantitative variables (EFV, EFV/BMI, EFV/BSA, BMI, BSA and age) were not normally distributed (Shapiro and Wilk test), the values are expressed as medians with interquartile range. Dichotomous data are presented as frequency (percent).
Differences in characteristics of patients were compared using Pearson’s χ2 test for dichotomous variables (or Fisher’s exact test when appropriate) and Kruskall-Wallis test for continuous test.
To compare the predictive performance for risk of significant CAD between the three EF parameters, we plotted receiver operating characteristic (ROC) curve from which the optimal cutoff was derived and we calculated the area under curve (AUC). AUC, optimal cutoff, sensitivity and specificity for each EFP and pairwise comparison of AUC have been determined. A two-tailed P-value less than 0.05 were considered as statistically significant; significant differences are presented with asterisk in the tables. The statistical methods of this study were reviewed by a biostatistician.
Table 1 illustrated the important clinical findings and measurements of the patients among the three groups of patients.
| Group 1 n = 58 | Group 2 n = 48 | Group 3 n = 64 | P | |
| Age | 48.5 (40.3-50.0) | 56 (48.5-64.5) | 55 (50-62) | 0.004 |
| Male | 21 (36.2) | 32 (57.1) | 32 (50) | 0.008 |
| Hypertension | 24 (41.4) | 29 (60.4) | 37 (57.8) | 0.090 |
| Diabetes mellitus | 23 (39.7) | 34 (70.8) | 43 (67.2) | 0.001 |
| Smoking | 5 (8.6) | 4 (8.3) | 14 (21.8) | 0.065 |
| Familial history | 7 (12.1) | 2 (4.2) | 6 (9.4) | 0.351 |
| BMI | 28.4 (25.9-33.9) | 29.5 (25.9-33.1) | 31.6 (29.3-33.1) | 0.007 |
| BSA | 1.80 (1.74-1.88) | 1.85 (1.78-1.94) | 1.88 (1.81-1.95) | 0.093 |
Comparison of EF parameters with CT coronary angiography results is presented in Table 2. Comparison of EFP medians revealed a progressive increase from group 1 to group 3. The medians where 81, 104 and 113 for EFV (cm3), 2.7, 3.7 and 3.8 for EVV/BMI (cm3/m2) and 45.6, 53.9 and 61.8 for EFV/BSA [cm3/(kg/m2)]. Nevertheless, the post- hoc analysis showed significant difference only between groups 1 and group 3 for all EFP: P = 0.002 for EFV, P = 0.012 for EFVBMI, and P = 0.007 for EFVBSA.
| Group 1 | Group 2 | Group 3 | P | |
| EFV (cm3) | 81 (59.4-124) | 104 (83.5-126) | 113 (92-138) | 0.004 |
| EFVBMI (cm3/m2) | 2.7 (1.9-3.9) | 3.7 (2.5-4.3) | 3.8 (3.0-4.6) | 0.014 |
| EFVBSA [cm3/(kg/m2)] | 45.6 (35.3-66.9) | 53.9 (44.4-68.6) | 61.8 (48.1-75.4) | 0.011 |
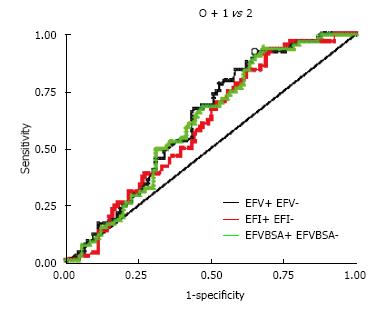
ROC curve for the three the EFP is presented in Figure 3. AUC was 0.62 for EFV, 0.6 for EFVBMI and 0.61 for EFVBSA and pairwise comparison failed to show significant difference. The optimal cut-off was 80.3 cm3 for EFV, 2.4 cm3/m2 for EFVBMI and 41.7 cm3/(kg/m2) for EFVBSA. Sensitivity and specificity were respectively 0.92 and 0.35 for EFV, 0.93 and 0.31 for EFVBMI, and 0.94 and 0.32 for EFVBSA.
Noninvasive quantitative measurement of epicardial fat volume from CT is feasible, and may play a clinical role in cardiovascular risk assessment[6]. It have shown its reproducibility and correlation to CAD presence, severity, and prognosis[14-16].
Recently, multiple studies have shown a deleterious relationship between epicardial fat burden and coronary atherosclerosis, arrhythmogenesis and major adverse cardiovascular events (MACE)[17,18]. In this study, the epicardial fat volume is correlated with the presence of coronary artery stenosis. In agreement with this findings, Alexopoulos et al[19] observed on coronary CT angiography a significant increase in epicardial fat volume with increasing coronary luminal stenosis; epicardial fat volume was also larger in patients with mixed or noncalcified plaques.
A recent study by Nakazato et al[20] assessed the relationship of epicardial fat volume to weight, BMI and waist circumference, and evaluated whether changes in these parameters over a 4-year period influenced epicardial fat volume measured by noncontrast CT in a relatively healthy asymptomatic population. They found that weight, BMI and waist circumference demonstrated moderate cross-sectional relationships to epicardial fat volume, and that changes in these parameters were related to epicardial fat volume change.
In another study, Shmilovich et al[9] assessed the body surface area indexed EVF in a healthy population and validated it as a predictor of major adverse cardiovascular events.
By reviewing the literature, the two parameters EFV and EFV/BSA, have no clear evidence of differences in their accuracies and predictive values[9,18-20]. In the current study we compared the predictive value of three EFP for the presence of significant CAD. To our knowledge, no similar studies have been performed before and EFV/BMI has not previously assessed also, the predictive value of EF/VBSA for CAD has not been compared with EFV.
The major outcome of the present study, derived from the ROC curve analysis, is that the three methods for assessing the EF have an equivalent predictive value for significant CAD and any one of them can be used as a predictor for significant CAD. Therefore, the clinical impact of the indexed EFV seems to be limited. To note that in the series using the indexed EFV to BSA, the benefit of such indexing has not been evaluated and ROC curve analysis has not been applied for assessment of possible increase in the predictive value for total occlusion of coronary arteries[16] or major adverse cardiovascular events[9].
According to the traditional academic point system, the accuracies of the three methods for measuring EF are classified as poor considering that the AUC are in the range 0.6-0.7. This limited accuracy is related mainly to the low specificity, ranging from 0.31 to 0.35, while the sensitivity is high, varying from 0.92 to 0.94, therefore the three methods can be considered as sensitive but poorly specific predictors for significant CAD. Consequently, indexing EFV by BSA or BMI doesn’t improve significantly the sensitivity and, more importantly, the specificity of EF for significant CAD.
In the current study, the optimal cut-off was 80.3 cm3 for EFV, 2.4 cm3/m2 for EFVBMI and 41.7 cm3/(kg/m2) for EFVBSA. The optimal cut-off for EFVBSA was lower than the value 50 cm3/m2 reported by Ueno et al[16] (labeled VEAT in their series), despite a higher median value in our series: 53.7 cm3/m2vs 47.1 cm3/m2. This difference is likely related to the definition of the end-point itself: significant CAD in the current study vs total occlusion of the coronary arteries in the series of Ueno et al[16]. More recently, Shmilovich et al[9] derived the threshold for the upper normal limit of indexed EF to BSA in a healthy population. The indexed EFV was also non-normally distributed, and the 75th-percentile was 47.1 cm3/m2, while in our series the 75th-percentile for the group 1 (composed of patients without CAD) 1 was 66.9 cm3/m2. Clearly, these values cannot be compared considering the major differences in the design of the two studies, the series of Shmilovich et al[9] including only asymptomatic patients with low risk and without clinical or biological risk factors for CAD.
Analysis of the correlation between the EFP and CT coronary angiography results revealed a trend of increase form group 1 to group 3. This result is similar to the conclusion of Taguchi et al[21] that pericardial fat is the strongest independent variable for the severity of CAD. Nevertheless, only groups 1 and 3 differed significantly. The overlap of values, for all EFP, between groups 2 and 3 may explain in great part the low specificity observed for the optimal cut-off. This point merits further analysis to achieve a higher predictive value of EF for significant CAD.
Relatively small number of studied patients with no available follow up data to observe the outcome or prognostic value of EFP considered a study limitation. Additionally our study may be affected by selection bias as we evaluate patients with clinical suspicion of CAD.
In conclusion, the major outcome of the present study that the three methods for assessment of EF have the same equivalent predictive value for significant CAD and any one of them can be used as a sensitive predictor for significant CAD. Additionally, we provided a threshold for each one of the three EFP. For further validation of this threshold additional larger study is recommended.
Epicardial fat (EF) under normal physiological conditions, EF tissue displays biochemical, mechanical and thermogenic cardio protective properties. Under pathological circumstances, EF can be strongly related to the development of coronary artery disease (CAD). Several imaging modalities can be used to quantify EF volume (EFV) such as echocardiography, computed tomography, and magnetic resonance imaging.
ECG-gated cardiac computed tomography with its high spatial resolution and true volume coverage of the heart, allows accurate measurement of epicardial fat volumes. Besides EFV, some authors derived a second parameter, the body surface area indexed EFV (EFV/BSA); however, comparison between these two parameters has not been considered. Moreover, despite the predictive value of higher body mass index for cardiovascular event, the added value of body mass index (BMI)-adjusted EFV (EFV/BMI) also has not been previously assessed as well. The current study compares the predictive value of the three methods for EF assessment (EFV, EFV/BSA and EFV/BMI) for presence of significant CAD.
In the current study the authors compared the predictive value of three EFP for the presence of significant CAD. To our knowledge, no similar studies have been performed before and EFV/BMI has not previously assessed also, the predictive value of EF/VBSA for CAD has not been compared with EFV. The major outcome of the present study is that the three methods for assessing the EF have an equivalent predictive value for significant CAD. Furthermore the authors provided a threshold for each one of the three EF parameters.
The study results suggested that; any one of the three methods for assessment of epicardial fat can be used to predict significant CAD since all have the same equivalent predictive value.
EF is the visceral fat of the heart deposited under the visceral layer of the pericardium and has the same origin as abdominal visceral fat.
This is a good study in which the authors compare the predictive value of three methods used for quantification of epicardial fat [i.e., EFV, EFV indexed with body surface area (EFV/BSA) and EFV indexed with body mass index (EFV/BMI)] for presence of significant CAD. The results are interesting and suggest that any one of the three methods for assessment of epicardial fat can be used to predict significant CAD since all have the same equivalent predictive value.
P- Reviewer: Haidara M, Wan Y S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Iwasaki K, Matsumoto T, Aono H, Furukawa H, Samukawa M. Relationship between epicardial fat measured by 64-multidetector computed tomography and coronary artery disease. Clin Cardiol. 2011;34:166-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Iacobellis G, Bianco AC. Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends Endocrinol Metab. 2011;22:450-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 391] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 3. | Baker AR, Silva NF, Quinn DW, Harte AL, Pagano D, Bonser RS, Kumar S, McTernan PG. Human epicardial adipose tissue expresses a pathogenic profile of adipocytokines in patients with cardiovascular disease. Cardiovasc Diabetol. 2006;5:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 460] [Cited by in RCA: 502] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 4. | Aydın H, Toprak A, Deyneli O, Yazıcı , D , Tarçın Ö, Sancak S, Akalın S. Epicardial Fat Tissue Thickness Correlates with Endothelial Dysfunction and Other Cardiovascular Risk Factors in Patients with Metabolic Syndrome. Metab Syndr Relat Disord. 2010;8:229-234. [RCA] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Sacks HS, Fain JN. Human epicardial fat: what is new and what is missing? Clin Exp Pharmacol Physiol. 2011;38:879-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Dey D, Nakazato R, Slomka P J, Berman D S. CT Quantification of Epicardial Fat: Implications for Cardiovascular Risk Assessment. Curr. Cardiovasc Imaging Rep. 2012;5:352-359. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Marwan M, Achenbach S. Quantification of epicardial fat by computed tomography: why, when and how? J Cardiovasc Comput Tomogr. 2013;7:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Dagvasumberel M, Shimabukuro M, Nishiuchi T, Ueno J, Takao S, Fukuda D, Sata M. Gender disparities in the association between epicardial adipose tissue volume and coronary atherosclerosis: A 3-dimensional cardiac computed tomography imaging study in Japanese subjects. Cardiovasc Diabetol. 2012;11:106. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Shmilovich H, Dey D, Cheng VY, Rajani R, Nakazato R, Otaki Y, Berman DS. Threshold for the Upper Normal Limit of Indexed Epicardial Fat Volume: Derivation in a Healthy Population and Validation in an Outcome-Based Study. Am J Cardiol. 2011;108:1680-1685. [RCA] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, Lang CC, Rumboldt Z, Onen CL, Lisheng L. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640-1649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1902] [Cited by in RCA: 1907] [Article Influence: 95.4] [Reference Citation Analysis (0)] |
| 11. | Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083-1096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3582] [Cited by in RCA: 3259] [Article Influence: 203.7] [Reference Citation Analysis (0)] |
| 12. | Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O’Gara P, Rubin GD. ACCF/SCCT/ACR/AHA/ASE/ASN/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. Circulation. 2010;122:e525-e555. [RCA] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 234] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 13. | Stadius ML, Alderman EL. Coronary artery revascularization. Critical need for, and consequences of, objective angiographic assessment of lesion severity. Circulation. 1990;82:2231-2234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Nichols JH, Samy B, Nasir K, Fox CS, Schulze PC, Bamberg F, Hoffmann U. Volumetric measurement of pericardial adipose tissue from contrast-enhanced coronary computed tomography angiography: A reproducibility study. J Cardiovasc Comput Tomogr. 2008;2:288-295. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Wang TD, Lee WJ, Shih FY, Huang CH, Chang YC, Chen WJ, Chen MF. Relations of Epicardial Adipose Tissue Measured by Multidetector Computed Tomography to Components of the Metabolic Syndrome Are Region-Specific and Independent of Anthropometric Indexes and Intraabdominal Visceral Fat. J Clin Endocrinol Metab. 2009;94:662-669. [RCA] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Ueno K, Anzai T, Jinzaki M, Yamada M, Jo Y, Maekawa Y, Ogawa S. Increased Epicardial Fat Volume Quantified by 64-Multidetector Computed Tomography is Associated With Coronary Atherosclerosis and Totally Occlusive Lesions. Circulation. 2009;73:1927-1933. [RCA] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 80] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Ahn SG, Lim HS, Joe DY, Kang SJ, Choi BJ, Choi SY, Yoon MH, Hwang GS, Tahk SJ, Shin JH. Relationship of epicardial adipose tissue by echocardiography to coronary artery disease. Heart. 2008;94:e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 222] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 18. | Thanassoulis G, Massaro JM, O’Donnell CJ, Hoffmann U, Levy D, Ellinor PT, Benjamin EJ. Pericardial Fat Is Associated With Prevalent Atrial Fibrillation: The Framingham Heart Study. Circ Arrhythm Electrophysiol. 2010;3:345-350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 357] [Cited by in RCA: 362] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 19. | Alexopoulos N, McLean DS, Janik M, Arepalli CD, Stillman AE, Raggi P. Epicardial adipose tissue and coronary artery plaque characteristics. Atherosclerosis. 2010;210:150-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 247] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 20. | Nakazato R, Rajani R, Cheng VY, Shmilovich H, Nakanishi R, Otaki Y, Dey D. Weight change modulates epicardial fat burden: A 4-year serial study with non-contrast computed tomography. Atherosclerosis. 2012;220:139-144. [RCA] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | Taguchi R, Takasu J, Itani Y, Yamamoto R, Yokoyama K, Watanabe S, Masuda Y. Pericardial fat accumulation in men as a risk factor for coronary artery disease. Atherosclerosis. 2001;157:203-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 211] [Article Influence: 8.8] [Reference Citation Analysis (0)] |