Published online Apr 26, 2015. doi: 10.4330/wjc.v7.i4.215
Peer-review started: October 22, 2014
First decision: November 27, 2014
Revised: January 7, 2015
Accepted: February 4, 2015
Article in press: February 9, 2015
Published online: April 26, 2015
Processing time: 180 Days and 8 Hours
AIM: To examine the contribution of treatment resistant depression (TRD) to mortality in depressed post-myocardial infarction (MI) patients independent of biological and social predictors.
METHODS: This secondary analysis study utilizes the Enhancing Recovery in Coronary Heart Disease (ENRICHD) clinical trial data. From 1834 depressed patients in the ENRICHD study, there were 770 depressed post-MI patients who were treated for depression. In this study, TRD is defined as having a less than 50% reduction in Hamilton Depression (HAM-D) score from baseline and a HAM-D score of greater than 10 in 6 mo after depression treatment began. Cox regression analysis was used to examine the independent contributions of TRD to mortality after controlling for the biological and social predictors.
RESULTS: TRD occurred in 13.4% (n = 103) of the 770 patients treated for depression. Patients with TRD were significantly younger in age (P = 0.04) (mean = 57.0 years, SD = 11.7) than those without TRD (mean = 59.2 years, SD = 12.0). There was a significantly higher percentage of females with TRD (57.3%) compared to females without TRD (47.4%) [χ2 (1) = 4.65, P = 0.031]. There were significantly more current smokers with TRD (44.7%) than without TRD (33.0%) [χ2 (1) = 7.34, P = 0.007]. There were no significant differences in diabetes (P = 0.120), history of heart failure (P = 0.258), prior MI (P = 0.524), and prior stroke (P = 0.180) between patients with TRD and those without TRD. Mortality was 13% (n = 13) in patients with TRD and 7% (n = 49) in patients without TRD, with a mean follow-up of 29 mo (18 mo minimum and maximum of 4.5 years). TRD was a significant independent predictor of mortality (HR = 1.995; 95%CI: 1.011-3.938, P = 0.046) after controlling for age (HR = 1.036; 95%CI: 1.011-1.061, P = 0.004), diabetes (HR = 2.912; 95%CI: 1.638-5.180, P < 0.001), heart failure (HR = 2.736; 95%CI: 1.551-4.827, P = 0.001), and smoking (HR = 0.502; 95%CI: 0.228-1.105, P = 0.087).
CONCLUSION: The analysis of TRD in the ENRICHD study shows that the effective treatment of depression reduced mortality in depressed post-MI patients. It is important to monitor the effectiveness of depression treatment and change treatments if necessary to reduce depression and improve cardiac outcomes in depressed post-MI patients.
Core tip: Treatment resistant depression (TRD) was associated with increased mortality in post-myocardial infarction (MI) patients with depression. Conversely, effective treatment of depression with cognitive behavioral therapy with or without medication decreased mortality in post-MI patients who were depressed. Since TRD post-MI patients are at higher risk for mortality, closer follow-up and more aggressive treatment for depression and risk factor modification is needed to improve patient outcome. It is important to monitor the effectiveness of depression treatment and change treatments if necessary to reduce depression and improve cardiac outcomes in post-MI patients with depression.
- Citation: Banankhah SK, Friedmann E, Thomas S. Effective treatment of depression improves post-myocardial infarction survival. World J Cardiol 2015; 7(4): 215-223
- URL: https://www.wjgnet.com/1949-8462/full/v7/i4/215.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i4.215
Depression predicts morbidity and mortality in patients after myocardial infarction (MI)[1-5]. Depression in post-MI patients is associated with increased mortality. A meta-analysis of 29 studies with an average of 16 mo follow-up and a total of 16889 patients revealed that post-MI depression is associated with more than doubling in odds of all cause mortality (OR = 2.25, 95%CI: 1.73-2.93; P < 0.001)[6]. Prevalence of depression is about 20% in patients with MI, compared to 5% in the general population[7,8]. Depression predicts a poorer prognosis and lower functional status in post-MI patients[4].
Treating depression in depressed post-MI patients should improve their long-term prognosis; however, in randomized clinical trials treating depression in depressed post-MI patients, did not improve their survival[9-12].
Cognitive behavioral therapy, plus adjunctive sertraline treatment in the case of insufficient response, did not improve mortality or nonfatal re-infarction with a mean 29 mo follow-up in post-MI patients with depression and/or low perceived social support (LPSS) enrolled in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) clinical trial[9]. There was no difference in event-free survival between the intervention and usual care groups (75.5% vs 74.7%). The intervention resulted in a temporary reduction in depression, which was present at 6 mo but disappeared by 30 mo after randomization[9]. Similarly, depression treatment did not improve cardiac event-free survival (treatment group 86.2% vs usual care group 87.3%) during the 18 mo of follow-up in the Myocardial Infarction and Depression-Intervention Trial (MIND-IT)[11]. Antidepressant medication (sertraline) for depressed patients with heart disease (n = 369) resulted in a slight, but non-significant reduction in recurrent MI and death after an average of 30 mo of follow-up (RR = 0.77; 95%CI: 0.51-1.16) in the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART)[10]. The recent 8-year follow-up of the MIND-IT trial that evaluated the effects of antidepressant treatment in depressed post-MI patients revealed that the treatment group’s mortality was not reduced when compared usual care group[12]. However, patients who actually received treatment for depression, regardless of group assignment, had an improved mortality (HR = 0.52, 95%CI: 0.28-0.97).
Secondary analyses of data from subgroups within clinical trials hint that the effectiveness of the treatment of depression might be a factor in whether treatment improves health outcomes. In an on-treatment secondary analysis of the 1834 depressed patients from the ENRICHD intervention and control groups showed significantly lower risk of recurrent MI and death in patients taking selective serotonin reuptake inhibitors (SSRIs) from both the usual care and treatment group. During an average of 29 mo of follow-up, 26% of patients who did not receive antidepressants died or had a recurrent MI vs 21.5% of patients on antidepressant therapy. Use of SSRIs was associated with significant reduction in risk of death or nonfatal MI (HR = 0.72; 95%CI: 0.44-1.22) and of all-cause mortality (HR = 0.73; 95%CI: 0.34-1.38)[13].
In patients with at least 1 prior episode of major depression in the ENRICD intervention group whose depression did not improve over the first 6 mo had higher late mortality (unimproved 21.2% vs improved 10.4%) and were more likely to be taking antidepressant medication and have a higher body mass index at enrollment than patients whose depression symptoms improved. In the usual care arm of ENRICHD, improvement in depression was not related to mortality[2].
In a 7-year follow-up analysis of SADHART, patients whose major depression did not respond to medication experienced 2.39 times as much mortality (28.4%) as those whose depression was treated effectively (15.6%)[14].
The ENRICHD study did not find that randomized treatment of depression in depressed post-MI patients decreased mortality or morbidity. Even with extensive effort to treat their depression, many patients in the intervention arm did not improve their depression symptoms after 6 mo of treatment. Instead, they seem to have a treatment refractory depression that was resistance to current available therapy. This finding and other subsequent analysis of ENRICHD studies left health professionals without clear direction for the treatment of depression in post-MI patients.
Clinical studies show that not all depressed patients respond adequately to treatment. Fava et al[15] meta-analysis of 36 clinical trials demonstrated that about 50% of depressed patients have an adequate response to antidepressant therapy, 15% had partial response, and 20%-35% did not respond to depression treatment. Patients who do not respond adequately labeled as treatment resistant. Depression was considered treatment resistant when at least 2 trials of different antidepressant therapy with adequate dose/duration/compliance failed to produce a significant clinical improvement in depression symptoms[16].
Patients with treatment resistant depression (TRD) in previous studies may have masked the effect of reducing depression on improvement of survival of depressed post-MI patients. In a cohort study of 4037 depression post-MI patients, 12.1% of the patients had treatment-resistant depression and they were 1.71 times as likely to die than treated patients[17].
The current study focuses on TRD and compares survival of patients with TRD to survival of patients who responded to treatment of depression.
This secondary data analysis uses longitudinal data from the ENRICHD randomized clinical trial. The limited use de-identified data set was obtained from the National Heart, Lung, and Blood Institute (NHLBI) after University of Maryland full IRB review.
ENRICHD was the first randomized multi-center study to examine the effect of psychosocial intervention on survival in patients who were depressed and/or had LSSP after an MI. This study was sponsored by the NHLBI, and recruitment started in October 1996 and ended in October 1999. Patients were enrolled in the ENRICHD study within 28 d of an acute MI.
All patients with an acute MI admitted to 1 of the 73 participating hospitals were screened for acute MI eligibility including MI documented by cardiac enzymes and by chest pain with typical ST-T changes or new Q waves. Complete ENRICHD inclusion and exclusion criteria are published elsewhere[9]. After informed consent was obtained, patients were screened for depression and/or LPSS. If either depression or LPSS was present, patients were randomly assigned to the intervention or usual care arm. Participants had follow-up examinations at 6 and 18 mo and annually thereafter. The primary end-point of the study was the occurrence of re-infarction or all cause mortality[9].
Cognitive behavioral therapy (CBT) was utilized as the standard of the ENRICHD intervention[18]. Intervention group patients with scores higher than 24 on the Hamilton rating scale for depression (HAM-D) or who had < 50% reduction in BDI score after 5 wk were referred to study psychiatrists for pharmacotherapy consideration. If there were no contraindications, sertraline hydrochloride was used as the drug of choice. The maximum CBT duration was 6 mo[9].
Patients in the usual care arm of the study received only the care provided by their primary care providers, which was standard medical care for post-MI patients. Patients in both groups received health education regarding cardiovascular disease and its management and both groups received standard medical treatment as practiced in that institution.
Baseline assessment in ENRICHD included demographics, cardiovascular health history, risk factors, current medications, detailed medical record documentation of the course of treatment for the acute MI, an electrocardiogram, the Depression Interview and Structured Hamilton (DISH), beck depression inventory (BDI), and ENRICHD social support inventory (ESSI).
The DISH is a semi-structured interview developed for ENRICHD trial and was used for screening and diagnosing depression[19] using principles and criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)[20]. The DISH incorporated material from the 17-item version of the Hamilton Rating Scale for Depression (HAM-D)[21], the Structured Interview Guide for the Hamilton Depression Scale (SIGH-D)[22], the Diagnostic Interview Schedule (DIS)[23], and the modified versions of the DIS[24]. The DISH depression severity score was based on the 17-item HAM-D. The first 9 items on HAMD-D are 5 point Likert format ranging from 0 (absent) to 4 (severe). The last 8 items are 3 point Likert format ranging from 0 (absent) to 2 (clearly present). The possible score ranges from 0 to 50. Scores of > 10 indicates the presence of depression symptoms. Higher total scores indicate more depression symptom severity. The concurrent validity of DISH was evaluated using the Pearson correlation coefficient between 17-item HAM-D embedded in the DISH and BDI scores that resulted in a correlation of 0.76 (P < 0.001)[19]. The DISH was administered at the screening phase of the ENRICHD study and at 6 mo follow-up.
The BDI[25] was used in the ENRICHD study to evaluate baseline depression status and assess progress during treatment and follow-up. The BDI is the most widely use depression instrument in clinical and research settings. The BDI is considered 1 of the best methods to assess presence and severity of depression. It is easy to use and only takes 5 min to complete by the patient or provider. The BDI is a 21-item inventory, and each item is rated on a 0 to 3 scale with a total score ranging from 0 to 64. BDI scores > 10 indicate depression, scores of 10-15 mild depression, 16-23 moderate depression, and 24-64 severe depression. Concurrent validity of BDI was established by comparing BID to HAM-D that positively correlated (r = 0.71, n = 87). This indicates an acceptable concurrent validity of BDI. The BDI was administered to all participants at baseline, 6, 12, 18 mo and annually thereafter.
The ESSI was used in the ENRICHD study to assess perceived social support at baseline and durng treatment and follow-up. It was developed for ENRICHD study to measure functional social support. The ESSI was used as a screening tool to determine patients’ eligibility for ENRICHD based on low social support, and to assess changes in patients’ social support following treatment. The ESSI is a 7-item inventory, and item 1 to 6 is rated on a 1 to 5 scale, which indicates none to all respectively. Item 7 is not rated on numeric scale. The total score ranges from 6 to 30 with lower scores indicating LPSS. A score < 3 on 2 or more items and a total score < 18, or a score of 2 on 2 items without regard to total score indicated LPSS which was the criteria for inclusion in ENRICHD trial[26]. In this study, 3 variables derived from ESSI instrument that were: live alone, perceived social support, and social isolation. Live alone was the seventh question on the ESSI questionnaire (“do you live alone?”) that was separated and transferred into the study dataset. Perceived social support was the total score on the ESSI and social isolation was dichotomous value based on scoring the ESSI. Social isolation was defined as meeting the ENRICHD criteria for LPSS. The reliability of ESSI was estimated by using test-retest reliability that showed no significant differences in mean scores administered 1 mo apart (P = 0.98). The internal reliability was measured with the use of Cronbach’s alpha that revealed an alpha of 0.88, which indicates a high internal consistency. The intra-class correlation coefficient was 0.94, reflecting excellent reproducibility[26]. The ESSI was administered to all participants at baseline, 6, 12, 18 mo and annually thereafter.
The study sample consists of the depressed patients in either arm of ENRICHD who received treatment for depression and completed the DISH at 6 mo. Treatment was defined as any combination of CBT and/or antidepressant medication. TRD was defined as < 50% improvement of 6-mo HAM-D score from baseline in patients with 6-mo HAM-D > 10. The outcome variable in this study was all cause mortality. All deaths were documented and verified by the ENRICHD investigators.
Data analysis: Normality of distributions of continuous variables was examined; no variables had extreme values that needed transformation[27]. Missing data was < 5% thus there was not a need to examine patterns of missing data[27]. All inferential tests were conducted at the 0.05 level of significance. Statistical procedures were performed using SPSS version 20.0 software.
Cox regression analyses was used to examine the hypothesis. The proportional hazards assumption of Cox regression was confirmed. The contribution of each biological (age, female gender, minority status, and presence of diabetes, history of heart failure, hypertension, prior MI, prior stroke, and current smoker), social (lives alone, perceived social support, social isolation), and psychological (baseline depression symptoms and TRD) predictor to mortality was initially examined in individual Cox regression analyses. Age was centered on 34 years, the lowest age in the study for ease of interpretation. The reference group (0) for dichotomous predictors was the un-named category. A combined model was constructed with biological, psychological, and social factors that predicted mortality at P < 0.20 in the individual analyses. Based on prior research showing differences between men and women in reporting depression[28,29], the interaction of TRD and female gender was added to the model. Similarly, based on prior research showing differences between minorities and non-minorities in reporting depression[30], the interaction of TRD and minorities status was added to the model. Neither of the interaction were significant predictors of mortality so they were not included in the final parsimonious Cox regression combined model. Biostatistician reviewed the statistical methods of this study.
Sample description: A total of 770 ENRICHD participants were depressed at the study entry and received depression treatment (Table 1). These participants received cognitive behavior treatment (CBT) (n = 469, 60.9%), or antidepressant medication (n = 85, 11%), or both (n = 216, 28.1%). The sample included 365 (47%) women and 239 (31%) minority participants. Ages ranged from 34 to 85 with a mean of 59 (SD = 12) years. Treatment resistant depression was present in 103 (13.4%) of the patients who were treated for depression.
| Characteristics | Treated DepressedPost-MI1 | TRDn = 1031 | Non TRDn = 6671 | |
| Demographics and biological characteristics | ||||
| Age, mean (SD), yr | 59.2 (12.0) | 57.0 (11.7) | 59.5 (12.0) | t = -2.07, P = 0.04 |
| Gender, female | 365 (47.4) | 59 (57.3) | 306 (45.9) | χ2 (1) = 4.65, P = 0.031 |
| Ethnicity, minority | 239 (31.0) | 32 (31.1) | 207 (31.0) | χ2 (1) = 0.0, P = 0.995 |
| Education: | χ2 (2) = 3.76, P = 0.153 | |||
| Basic or no HS degree | 187 (24.3) | 25 (24.3) | 162 (24.3) | |
| HS without college degree | 419 (54.4) | 64 (62.1) | 355 (53.2) | |
| Advanced education | 146 (19.0) | 13 (12.6) | 133 (19.9) | |
| Body mass index, mean (SD) | 29.2 (6.1) | 29.7 (6.3) | 29.2 (6.1) | t = 0.77, P = 0.444 |
| Diabetes | 264 (34.3) | 42 (40.8) | 222 (33.3) | χ2 (1) = 2.41, P = 0.120 |
| History of heart failure | 101 (13.1) | 17 (16.5) | 84 (12.6) | χ2 (1) = 1.28, P = 0.258 |
| Hypertension | 458 (59.5) | 70 (68.0) | 388 (58.2) | χ2 (1) = 4.56, P = 0.033 |
| Prior MI | 187 (24.3) | 22 (21.4) | 165 (24.7) | χ2 (1) = 0.41, P = 0.524 |
| Prior stroke | 70 (9.1) | 13 (12.9) | 57 (8.7) | χ2 (1) = 1.80, P = 0.180 |
| Current smoker | 254 (33.0) | 46 (44.7) | 208 (31.2) | χ2 (1) = 7.34, P = 0.007 |
| Social characteristics | ||||
| Live alone | 322 (41.8) | 46 (44.7) | 276 (41.4) | χ2 (1) = 0.32, P = 0.570 |
| Social support | 356 (46.2) | 54 (52.4) | 302 (45.3) | χ2 (1) = 1.84, P = 0.176 |
| Psychological characteristics | ||||
| Depression | χ2 (2) = 16.7, P > 0.001 | |||
| Major depression | 398 (51.7) | 69 (67.0) | 329 (49.3) | |
| Minor depression | 348 (45.2) | 28 (27.2) | 320 (48.0) | |
| Dysthymia | 24 (3.1) | 6 (5.8) | 18 (2.7) | |
| Psychosocial measures | ||||
| Baseline Depression Symptom Severity (BDI), mean (SD) | 17.7 (7.8) | 22.4 (9.3) | 17.0 (7.4) | t = 6.62, P < 0.001 |
| Baseline Perceived Social Support (ESSI), mean (SD) | 24.5 (6.4) | 22.9 (7.0) | 24.7 (6.3) | t = -2.74, P = 0.006 |
| Baseline Depression Symptom (HAM-D), mean (SD) | 17.9 (6.3) | 20.9 (6.5) | 17.4 (6.1) | t = 5.07, P < 0.001 |
The statistical methods of this study were reviewed by Erika Friedmann from University of Maryland.
Baseline characteristics of patients with and without TRD were compared (Table 1). Patients with TRD were significantly younger (P = 0.04), more likely to be female (P = 0.031), be hypertensive (P = 0.033), and have lower perceived social support (P = 0.006) than those without TRD. Major depression was significantly more common (P < 0.001) and baseline depression symptom severity assessed with the BDI was significantly worse (P < 0.001) among patients who experienced TRD.
Of the 770 participants, there were 62 (8%) deaths with an average follow-up of 29 mo. All cause mortality tended to be higher in the patients with TRD (13/103: 13%) than those whose depression responded to treatment (49/667: 7%) (χ2 = 3.35, P = 0.05).
In univariate Cox regression analysis (Table 2), age (P < 0.001), female gender (P = 0.005), diabetes (P < 0.001), history of heart failure (P < 0.001), hypertension (P = 0.002), prior MI (P < 0.001), prior stroke (P < 0.001), current smoker (P = 0.002) and live alone (P = 0.032) were significant predictors of mortality. Minority status (P = 0.943), perceived social support (P = 0.279), social isolation (P = 0.446), and baseline depression symptoms (P = 0.978) did not predict mortality.
| B | SE | Wald | Sig. | HR | 95%CI | |
| Biological factors | ||||||
| Age1 | 0.048 | 0.011 | 19.205 | < 0.001 | 1.05 | 1.027-1.073 |
| Female gender | 0.741 | 0.266 | 7.791 | 0.005 | 2.098 | 1.247-3.531 |
| Minority status | 0.020 | 0.272 | 0.005 | 0.943 | 1.020 | 0.599-1.737 |
| Diabetes | 1.448 | 0.272 | 28.401 | < 0.001 | 4.255 | 2.498-7.247 |
| Heart failure | 1.495 | 0.275 | 29.507 | < 0.001 | 4.461 | 2.601-7.652 |
| Hypertension | 1.002 | 0.322 | 9.675 | 0.002 | 2.723 | 1.449-5.120 |
| Prior MI | 0.961 | 0.261 | 13.533 | < 0.001 | 2.616 | 1.567-4.365 |
| Prior stroke | 1.165 | 0.306 | 14.496 | < 0.001 | 3.207 | 1.760-5.843 |
| Current smoker | -1.128 | 0.361 | 9.781 | 0.002 | 0.324 | 0.160-0.656 |
| Social factors | ||||||
| Live alone | 0.552 | 0.258 | 4.591 | 0.032 | 1.737 | 1.048-2.880 |
| Perceived social support | -0.046 | 0.028 | 2.768 | 0.096 | 0.955 | 0.904-1.008 |
| Social isolation | -0.197 | 0.258 | 0.582 | 0.446 | 0.822 | 0.496-1.361 |
| Psychological factor | ||||||
| Baseline depression symptom severity | < 0.001 | 0.016 | 0.001 | 0.978 | 1.000 | 0.968-1.032 |
| Treatment resistant depression | 0.534 | 0.312 | 2.927 | 0.087 | 1.705 | 0.925-3.143 |
In the combined simultaneous Cox regression model, TRD (P = 0.046), age (P = 0.004), diabetes (P < 0.001), and history of heart failure (P = 0.001) were significant independent predictors of mortality; current smoker tended to predict mortality (P = 0.087) (Table 3).
| B | SE | Wald | Sig. | HR | 95%CI | |
| Biological factors | ||||||
| Age1 | 0.035 | 0.012 | 8.280 | 0.004 | 1.036 | 1.011-1.061 |
| Diabetes | 1.069 | 0.294 | 13.243 | 0.000 | 2.912 | 1.638-5.180 |
| Heart failure | 1.007 | 0.290 | 12.089 | 0.001 | 2.736 | 1.551-4.827 |
| Current smoker | -0.690 | 0.403 | 2.932 | 0.087 | 0.502 | 0.228-1.105 |
| Social factors | ||||||
| None | ||||||
| Psychological factor | ||||||
| Treatment resistant depression | 0.691 | 0.347 | 3.967 | 0.046 | 1.995 | 1.011-3.938 |
When the interaction between female gender and TRD and minority status and TRD were each added to the model, the interactions were not significant (P = 0.467, P =0.87, respectively). Neither interaction was added to the final model. In the final model TRD contributed significantly to mortality (P = 0.046) after controlling for age, diabetes, heart failure, and currently smoking. Patients with TRD had approximately double the risk of all cause mortality compared with patients without TRD (95%CI: 1.011-3.938). Other significant independent predictors of mortality were age, diabetes and heart failure.
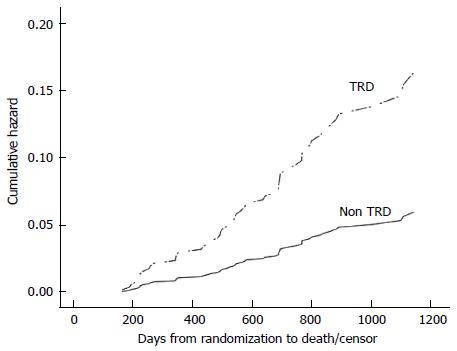
This study showed a significant improvement in survival in depressed post-MI patients whose depression was effectively treated (Figure 1). Among treated depressed post-MI patients, TRD was a significant independent predictor of mortality after controlling for biological and social factors.
Not all depressed patients respond adequately to treatment, and their depression does not improve significantly with current depression treatments. These depressed patients are treatment resistant[13]. Recent studies do not show improved mortality of acute myocardial infarction patients after treatment for depression[8-12]. One explanation of this may be that previous studies of post-MI patients included a subgroup of patients with TRD who may have impacted the results. The presence of the TRD sub-group may cause a failure in the study’s ability to show improved survival in the intervention group.
The purpose of this study was to examine the differences in mortality between patients with TRD and those without TRD. The significant predictors for mortality among depressed post-MI patients whose depression was treated were; age, diabetes, and history of heart failure. The presence of TRD significantly predicted mortality after controlling for these other factors (HR = 1.995). TRD was associated with an increased risk of mortality when compared to non-TRD patients. This finding is consistence with the 7-year follow-up analysis of the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) [10]. Initial findings of SADHEART revealed a non-significant reduction in re-current MI and death (RR = 0.77; 95%CI: 0.51-1.16) in treated depressed individuals. At that time, they did not examine the difference between survival in those individuals who responded and not respondent to depression treatment. Subsequently, the 7-year follow-up analysis of the SADHART trial found that patients with major depression who responded to treatment with sertraline had a reduction in mortality vs non-responders (15.6% vs 28.4%; HR = 2.39)[14]. The current study extends this finding from post MI patients with major depression to less psychologically distressed patients, namely post MI patients with dysthymia through major depression. Further the current study began treatment with cognitive behavioral therapy and added medication if depression was not responsive. This study is also consistent with Scherrer et al’s[17] cohort study’s finding that post-MI patients with TRD had increased mortality. The criteria for TRD in that study were that: the patient received (1) electroconvulsive therapy, (2) a monoamine oxidase inhibitor, or (3) two or more antidepressant at the same time. In contrast, the current study uses depression measurement tools to identify post-MI patients with TRD.
This re-analysis of the ENRICHD study data clearly shows that successful treatment of depression decreases mortality in post-MI patients. It also demonstrates that current depression treatments are not effective in treating all depressed post-MI patients. According to this study, over 13% of treated patients still suffered from depression at the end the treatment. This is consistent with the Scherre study, which showed 12.1% of post-MI patients experienced TRD. Perhaps a treatment that is more effective in alleviating depression would improve survival in post-MI patients. Until more effective treatments are developed, closer follow-up of depression symptoms, aggressive treatment of depression, actively treating other modifiable risk factors, and modifying risky health behaviors may lead to a better survival in post-MI patients with TRD.
This study was a secondary data analysis of an existing trial. This places limitation to this study regarding control over the variable definition, measurement, data collection and other crucial aspects of the study design. With this study, we were not able to establish causality of the contributions of TRD for mortality. The study findings were only able to provide evidence of the associations between the variables. Despite the limitations of this study, the strengths outweigh the limitations of the study. Using a large existing database, this study has the advantage of providing a representative sample. Women and minorities were well represented in the ENRICHD data. ENRICHD included detailed questionnaire development, data collection procedures, data management, and quality control measures. The use of ENRICHD dataset provided an opportunity to use high quality dataset without the high cost and effort of obtaining this type and amount of data.
The analysis of TRD in ENRICHD shows that treatment of depression in the ENRICHD sample was effective in reducing mortality in those whose depression was effectively reduced by cognitive behavioral therapy and/or anti-depressant medication. By separating out those who were depressed and whose treatment was effective it was possible to evaluate the contribution of effective treatment of depression to mortality in post-MI patients. The findings of this study provided evidence that depressed patients with TRD have more than double the risk of mortality when compared with patients whose depression is effectively treated. This sub-group of depressed patients with TRD did not improve their depression symptoms with their current depression treatment. Closer follow-ups of depression symptoms, aggressive treatment of depression, aggressively treating other modifiable risk factors, and modifying risky health behaviors may lead to a better chance of survival in TRD post-MI patients.
As shown in this current study, depression is a risk factor for mortality among TRD post-MI patients. Yet the question remains how to best treat it. Future research is needed to address the development of effective treatment for depression. Both ENRICHD and SADHART trials reported small effect size using current depression interventions, this suggest a need to increase efficacy of current interventions for depressed post-MI patients. The results of the present study accentuate the need for future research for drug development and effective interventions to alleviate depression symptoms in order to improve cardiac outcomes.
The potential mechanisms linking depression and impaired cardiovascular prognosis are still poorly understood and remain an area that is in need of more research. Future studies are needed to give insight and provide evidence that will direct us toward a future in which we, health providers, are able to help and improve survival in post-MI patients who have TRD.
This study provided evidence that TRD is associated with increased mortality in post-MI patients who are depressed. Conversely, effective treatment of depression with cognitive behavioral therapy without or with medication decreased mortality in post-MI patients who were depressed. Since, TRD post-MI patients are at higher risk for mortality, closer follow-up and more aggressive treatment for depression and risk factor modification is needed to improve patients’ outcomes. This may lead to an integrated treatment strategy that may decrease risk of mortality in post-MI patients. It is important to monitor the effectiveness of depression treatment and change treatments if necessary to reduce depression and improve cardiac outcomes in post-MI patients who are depressed.
This manuscript was prepared using the Enhancing Recovery in Coronary Heart Disease (ENRICHD) limited access dataset obtained from the NHLBI Biologic Specimen and Data Repository Information Coordinating Center and does not necessarily reflect the opinions or views of the ENRICHD Study or the NHLBI. The authors thank the investigators, coordinators, staff, and patients of the ENRICHD Study.
Depression increases mortality after myocardial infarction (MI). Clinical trials have not demonstrated a reduction in mortality with depression treatment. Depression treatment is not effective in a substantial proportion of the depressed patients. The presence of treatment resistant depression (TRD) may explain why previous clinical trials did not demonstrate decreased mortality when depression was treated.
Recent clinical studies show that not all depressed patients respond adequately to treatment, and their depression does not improve significantly with current depression treatments. These patients have TRD. Presently, there is no study that shows improved outcome of depressed patients with acute MI by treating depression. This can be explained by the presence of TRD in some post-MI patients, which would impact the results of the study. The presence of TRD may cause a failure in the study’s ability to show improved survival in the intervention group.
This study considers the presence of TRD in depressed post-MI patients and its influence on prior analysis. Treatment resistant depression is a possible explanation for why previous clinical trials did not demonstrate decreased mortality when depression was treated. The result of this study reveals that TRD significantly predicts mortality after controlling for biological and social factors. Among depression treated post MI patients, TRD was associated with an increased risk of mortality when compared to non-TRD patients. Depressed patients with TRD have double the risk of mortality when compared with patients whose depression is effectively treated.
This study provides new evidence that depressed patients with TRD did not improve their mortality with current depression treatment, and they are in desperate need for more efficacious depression treatment. Closer follow-ups of depression symptoms, aggressive treatment of other modifiable risk factors, and modifying risky health behaviors may lead to a better chance of survival in depressed post-MI patients. This knowledge may assist primary care providers regarding clinical decision making that provides a better treatment options for patients.
TRD is a term describing patients with depression symptoms that do not improve after treatment is completed. In other words, the total hamilton depression (HAM-D) score does not decrease more than 50% from baseline with a total HAM-D score above 10 after completing depression treatment.
Authors showed that effective treatment of depression improved survival of patients after AMI. This paper is well described, and includes important clinical findings.
P- Reviewer: Chang ST, Kounis NG, Kurisu S, Tampi RR S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Huffman JC, Smith FA, Blais MA, Taylor AM, Januzzi JL, Fricchione GL. Pre-existing major depression predicts in-hospital cardiac complications after acute myocardial infarction. Psychosomatics. 2008;49:309-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Carney RM, Blumenthal JA, Freedland KE, Youngblood M, Veith RC, Burg MM, Cornell C, Saab PG, Kaufmann PG, Czajkowski SM. Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study. Psychosom Med. 2004;66:466-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 227] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 3. | Lane D, Carroll D, Lip GY. Anxiety, depression, and prognosis after myocardial infarction: is there a causal association? J Am Coll Cardiol. 2003;42:1808-1810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Bush DE, Ziegelstein RC, Tayback M, Richter D, Stevens S, Zahalsky H, Fauerbach JA. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol. 2001;88:337-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 410] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 5. | Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1162] [Cited by in RCA: 984] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 6. | Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry. 2011;33:203-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 378] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 7. | Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21:30-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 566] [Cited by in RCA: 576] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 8. | Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. 2003;54:227-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 371] [Cited by in RCA: 347] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 9. | Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffe A. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106-3116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1276] [Cited by in RCA: 1190] [Article Influence: 54.1] [Reference Citation Analysis (0)] |
| 10. | Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Krishnan KR, van Zyl LT, Swenson JR, Finkel MS. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 974] [Cited by in RCA: 917] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 11. | van Melle JP, de Jonge P, Honig A, Schene AH, Kuyper AM, Crijns HJ, Schins A, Tulner D, van den Berg MP, Ormel J. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry. 2007;190:460-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 240] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 12. | Zuidersma M, Conradi HJ, van Melle JP, Ormel J, de Jonge P. Depression treatment after myocardial infarction and long-term risk of subsequent cardiovascular events and mortality: a randomized controlled trial. J Psychosom Res. 2013;74:25-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Taylor CB, Youngblood ME, Catellier D, Veith RC, Carney RM, Burg MM, Kaufmann PG, Shuster J, Mellman T, Blumenthal JA. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry. 2005;62:792-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 347] [Cited by in RCA: 386] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 14. | Glassman AH, Bigger JT, Gaffney M. Psychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression: seven-year follow-up of SADHART participants. Arch Gen Psychiatry. 2009;66:1022-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Fava M, Davidson KG. Definition and epidemiology of treatment-resistant depression. Psychiatr Clin North Am. 1996;19:179-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 513] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 16. | Berlim MT, Turecki G. Definition, assessment, and staging of treatment-resistant refractory major depression: a review of current concepts and methods. Can J Psychiatry. 2007;52:46-54. [PubMed] |
| 17. | Scherrer JF, Chrusciel T, Garfield LD, Freedland KE, Carney RM, Hauptman PJ, Bucholz KK, Owen R, Lustman PJ. Treatment-resistant and insufficiently treated depression and all-cause mortality following myocardial infarction. Br J Psychiatry. 2012;200:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation 1996; . |
| 19. | Freedland KE, Skala JA, Carney RM, Raczynski JM, Taylor CB, Mendes de Leon CF, Ironson G, Youngblood ME, Krishnan KR, Veith RC. The Depression Interview and Structured Hamilton (DISH): rationale, development, characteristics, and clinical validity. Psychosom Med. 2002;64:897-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 92] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | American Psychiatric Association. Diagnostic and statistical manual of mental disorder, 4th ed. Washington, D.C. : American Psychiatric Association 1994; . |
| 21. | Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21041] [Cited by in RCA: 22811] [Article Influence: 350.9] [Reference Citation Analysis (0)] |
| 22. | Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1988;45:742-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1356] [Cited by in RCA: 1475] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 23. | Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3421] [Cited by in RCA: 2953] [Article Influence: 67.1] [Reference Citation Analysis (0)] |
| 24. | Carney RM, Rich MW, Freedland KE, Saini J, teVelde A, Simeone C, Clark K. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med. 1988;50:627-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 405] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 25. | Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23191] [Cited by in RCA: 23295] [Article Influence: 862.8] [Reference Citation Analysis (0)] |
| 26. | Vaglio J, Conard M, Poston WS, O’Keefe J, Haddock CK, House J, Spertus JA. Testing the performance of the ENRICHD Social Support Instrument in cardiac patients. Health Qual Life Outcomes. 2004;2:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 173] [Cited by in RCA: 223] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 27. | Tabachnick BG, Fidell LS. Using Multivariate Statistic. 5th ed. New York: Pearson Education, Inc 2007; . |
| 28. | Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29:85-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1396] [Cited by in RCA: 1358] [Article Influence: 42.4] [Reference Citation Analysis (0)] |
| 29. | Nolen-Hoeksema S. Gender differences in depression. CDPS. 2001;10:173-176. [RCA] [DOI] [Full Text] [Cited by in Crossref: 739] [Cited by in RCA: 645] [Article Influence: 71.7] [Reference Citation Analysis (0)] |
| 30. | Ghafoori B, Barragan B, Tohidian N, Palinkas L. Racial and ethnic differences in symptom severity of PTSD, GAD, and depression in trauma-exposed, urban, treatment-seeking adults. J Trauma Stress. 2012;25:106-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |