Published online Jul 26, 2014. doi: 10.4330/wjc.v6.i7.685
Revised: February 20, 2014
Accepted: May 16, 2014
Published online: July 26, 2014
Processing time: 228 Days and 4 Hours
We present the case of a 65-year-old male with vasospastic angina (VSA) whose condition worsened during the perioperative period. He had been diagnosed with VSA 10 years prior. He was treated with two types of vasodilators and had not experienced any chest symptoms for 5 years. At this juncture, he underwent surgery for relapsed maxillary sublingual carcinoma. He had taken two vasodilators one day prior to surgery. Intravenous infusion of nitroglycerin (NTG) was initiated immediately before the surgery and continued the following day. Instead of stopping NTG, a dermal isosorbide dinitrate tape was applied on post-operative day 1. Two days later, a complete atrioventricular block with pulseless electrical activity appeared. After cardiopulmonary resuscitation, emergent coronary angiography showed severe coronary spasm in both the left and right coronary arteries. Intracoronary infusion of nitroglycerin and epinephrine with percutaneous cardiopulmonary support relieved the coronary spasm. During the perioperative period, several factors can trigger coronary vasospasm, including the discontinuation of vasodilators. Thus, surgeons, anesthetists, and cardiologists should watch for coronary vasospasm during this period and for worsening coronary spasm when discontinuing vasodilators in patients at risk for VSA.
Core tip: Coronary spasm during the perioperative period often emerges severely as either cardiogenic shock or ventricular fibrillation. Although there are several surgery-related factors that influence the activity of coronary spasm, discontinuing vasodilators during the perioperative period is an important problem in patients with vasospastic angina (VSA). We encountered an outpatient with VSA whose condition had been stabilized using two types of vasodilators but subsequently worsened, leading to cardiogenic shock during the perioperative period. In light of this event, physicians should carefully evaluate their patients regarding the possibility of a coronary spasm during the perioperative period.
- Citation: Teragawa H, Nishioka K, Fujii Y, Idei N, Hata T, Kurushima S, Shokawa T, Kihara Y. Worsening of coronary spasm during the perioperative period: A case report. World J Cardiol 2014; 6(7): 685-688
- URL: https://www.wjgnet.com/1949-8462/full/v6/i7/685.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i7.685
The abrupt cessation of vasodilators causes rebound coronary spasm in patients with vasospastic angina (VSA)[1-6]. During the perioperative period, physicians sometimes have to discontinue oral vasodilators, even in patients with VSA. Furthermore, other factors that worsen VSA occur during the perioperative period. Thus, VSA activity may be accelerated during this interval. However, little is known about VSA management during this period[7,8]. In this study, we present a case in which coronary spasm worsened during the perioperative period.
A 65-year-old male, who was diagnosed with VSA 10 years prior and treated with two types of vasodilators (benidipine hydrochloride, 8 mg/d, and nicorandil, 5 mg/d) was admitted to the Department of Otolaryngology at our institution to undergo surgery for relapsed maxillary sublingual carcinoma. He had a coronary risk factor due to smoking (30/d × 37 years). With regard to the results of the interview and medical records, the patient experienced spontaneous and/or imminent episodes of VSA several times per year for the first 5 years, but he had experienced no chest symptoms for the past 5 years. On admission, his vitals were stable. Blood examination, electrocardiogram (ECG), and echocardiography showed no specific findings.
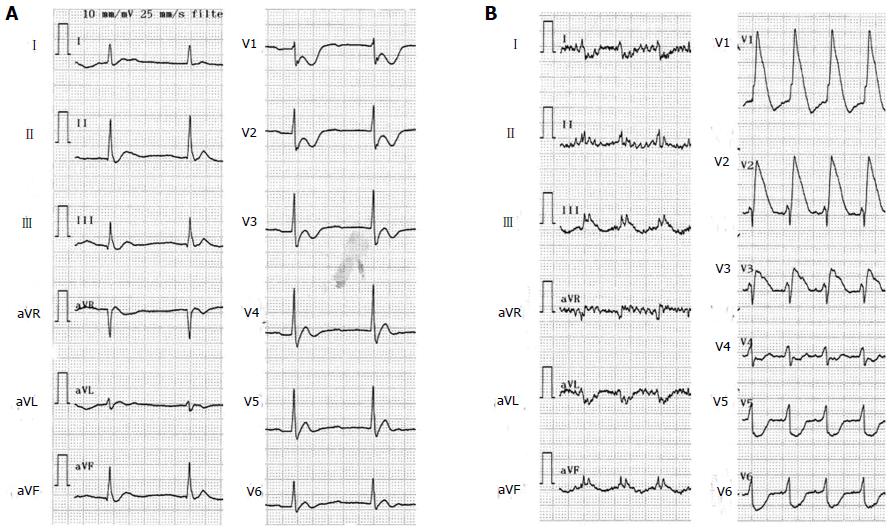
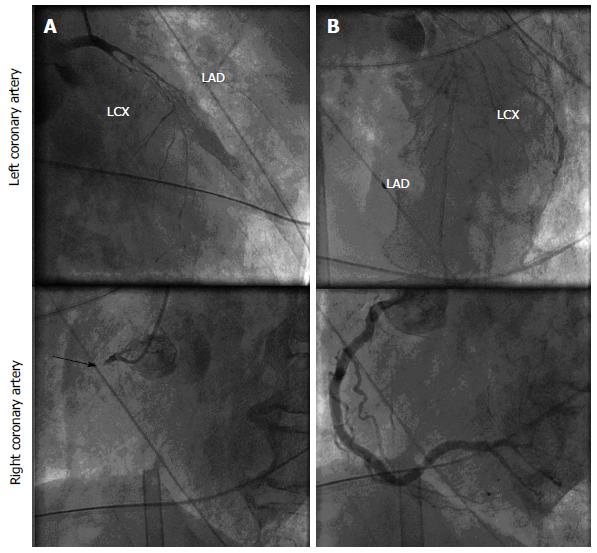
On pre-operative day 1, the patient took the same 2 vasodilators; this oral medication was stopped on the day of surgery. Instead, from the morning of the surgery, an intravenous infusion of nitroglycerin (NTG) at 2 mL/h was started. A large left maxillary resection and submaxillotomy were performed. On post-operative day 1, the patient was sedated with midazolam. Intravenous NTG was stopped on post-operative day 1, and a dermal isosorbide dinitrate tape was applied. In the evening of post-operative day 2, his blood pressure decreased, and ECG showed a complete atrioventricular atrioventricular block (Figure 1A). Pulseless electrical activity (PEA) was subsequently noticed, and cardiopulmonary resuscitation was initiated with repeated infusions of epinephrine. Ventricular fibrillation and PEA were repeated and percutaneous cardiopulmonary support (PCPS) was started 1 h later. ECG at that time showed ST elevations in leads II, III, aVF, and V1-3 (Figure 1B). Emergent coronary angiography revealed an occlusion at the proximal segment of the right coronary artery, and severe and diffuse narrowing due to coronary spasms of the left coronary artery (Figure 2A). Intracoronary infusions of nitroglycerin and epinephrine (20-100 μg) were repeated, which relieved the bilateral coronary spasms (Figure 2B). Intravenous NTG and dopamine were continued, and PCPS was removed 4 d later. From post-operative day 19, oral benidipine hydrochloride at 8 mg/d was started, in addition to intravenous NTG infusion. From post-operative day 21, NTG infusion was discontinued, and only oral benidipine hydrochloride was prescribed. Thereafter, the patient had no chest symptoms; however, he died on post-operative day 74 from hydrocephalus due to the original disease.
We describe a case with VSA, where the condition was stable for 5 years but worsened during the perioperative period. The cessation or reduction of vasodilators worsens coronary spasm in patients with VSA[1-6]. In fact, we have seen several VSA cases in which noncompliance to vasodilators increased angina attacks in the clinical setting. In the perioperative period, vasodilators sometimes have to be stopped or reduced, even in patients with VSA. Thus, VSA management during the perioperative period is of pivotal importance, based on the knowledge gained from the present case.
Although the occurrence or exacerbation of VSA during the perioperative period is not frequent[8], the problem certainly exists. At our institution, the incidence from 1999 to 2008 was 0.042% (17 cases/40466 operations, unpublished data). Koshiba et al[7] reviewed the clinical characteristics of perioperative coronary spasm and raised several important points, including possible contributing factors and the surgical site. Contributing factors for perioperative coronary spasm may include inadequate anesthesia, use of vasopressors, vagal nerve stimulation, drugs other than vasopressors, epidural block, hypotension, mechanical stimulation of the heart, allergic reaction, and/or mental stress. Regarding the surgical site, abdominal surgery was performed in 49% of cases. At our institution, abdominal surgeries comprised 76% of all perioperative VSA cases (13 of 17), and upper abdominal surgery was the most frequent type with 65% (11 of 17 cases, unpublished data). An increase in vagal nerve stimulation, a possible contributing factor, may be the result of abdominal surgery, which was the most frequently performed procedure. Nagayoshi et al[8] reported a case of perioperative coronary spasm at their institution and showed that the surgical risks are fairly low in patients who developed coronary spasm in the perioperative period. Preoperative consultations with a cardiologist were reported in only 2 of 18 cases with perioperative coronary spasm. Therefore, a cardiologist should be consulted before surgery in patients with known VSA or coronary artery disease (CAD). In the clinical setting, even though the presence of VSA or CAD has not been indicated, we sometimes encounter patients who have taken vasodilators and experienced no chest symptoms. A preoperative cardiology consultation should be recommended, even for such patients. Cardiologists should check all patient information, including interview notes, medical records, and preoperative cardiovascular examinations, and consider the possibility of a coronary spasm.
Discontinuing vasodilators, including calcium-channel blockers, during the perioperative period is another important factor[1-6]. In principle, vasodilators should be taken during the perioperative period; however, the surgery, which normally requires the discontinuation of these medications, must proceed as planned. In the present case, where a large left maxillary resection and submaxillotomy were performed, vasodilators were discontinued during the surgery. Under such circumstances, two alternatives exist: intravenous vasodilators and dermal nitrate tape/patch. We previously conducted a survey regarding the perioperative management of VSA patients by 31 cardiologists from the Hiroshima Prefecture (unpublished data). Based on the results of the questionnaires, intravenous vasodilators was not routine but frequently given, depending on the patient’s VSA status, in 93% of cases. The patient’s VSA status includes VSA episodes while taking oral medications, spasm-provocation test results (e.g., organic stenosis, multivessel spasm, severely provoked spasm), and the number of vasodilators (more than or equal to 2). Intravenous vasodilators generally include NTG, nicorandil, and diltiazem, and determining when to stop the intravenous vasodilators may be a problem. They can be instantly stopped in VSA patients who can take oral vasodilators, particularly those with low VSA activity. However, in patients who cannot take vasodilators orally, are compelled to use a dermal nitrate tape/patch, or have a high VSA activity, the use of intravenous vasodilators and oral medications (or dermal nitrate tape/patch) simultaneously may be necessary for 1 or 2 d. In the present case, because the patient used a dermal NTG tape after terminating intravenous NTG, the vasodilating effect may have decreased, leading to severe VSA. In contrast, a dermal nitrate tape/patch is usually prescribed for VSA patients with less active disease. In our survey, 69% of all effective answers indicated that the dermal nitrate tape/patch was used in patients who had taken vasodilators for an extensive period, in spite of a low probability of having VSA. Long-term use of nitrates, particularly a dermal nitrate tape/patch, increases the possibility of nitrate tolerance[9-11]; therefore, physicians should be extremely judicious in prescribing these drugs.
Learning from the present case, we recommend the following management of coronary spasm during the perioperative period: (1) not only the cardiologist but also the surgeon and anesthetist have to rule out the presence of VSA according to the patient’s medical records, interview, and results from the preoperative cardiovascular examinations; (2) if VSA is established, vasodilators must be included in the patient’s treatment plan. If there is a suspicion of VSA, i.e., the patient has been taking vasodilators for a long time, the regimen should be continued during the perioperative period; and (3) the use of intravenous vasodilators should be determined on the basis of the patient’s VSA activity. During the transition from IV to oral administration, no gap should be allowed. The simultaneous use of two drugs may be required for 1 or 2 d.
In conclusion, perioperative coronary spasm has been proven to exist, despite its low frequency. In evaluating a patient’s medical history and presenting symptoms, physicians should consider and investigate the possibility of perioperative coronary spasm. Intravenous infusion of vasodilators during the perioperative period is sometimes required, but a discontinuation may pose a risk of coronary spasm for the patient.
A 65-year-old male with vasospastic angina (VSA) whose condition worsened during the perioperative period.
Authors’ present a case in which coronary spasm worsened during the perioperative period.
The patient had been diagnosed with VSA 10 years prior.
Teragawa et al present an interesting case report about worsening of coronary spasm during the perioperative period in a patients with previous diagnosis of vasospastic angina.
P- Reviewer: Petix NR, Rassaf T S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
| 1. | Lange RL, Reid MS, Tresch DD, Keelan MH, Bernhard VM, Coolidge G. Nonatheromatous ischemic heart disease following withdrawal from chronic industrial nitroglycerin exposure. Circulation. 1972;46:666-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 139] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Engelman RM, Hadji-Rousou I, Breyer RH, Whittredge P, Harbison W, Chircop RV. Rebound vasospasm after coronary revascularization in association with calcium antagonist withdrawal. Ann Thorac Surg. 1984;37:469-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Lette J, Gagnon RM, Lemire JG, Morissette M. Rebound of vasospastic angina after cessation of long-term treatment with nifedipine. Can Med Assoc J. 1984;130:1169-1171, 1174. [PubMed] |
| 4. | Dimmitt SB, Beilin LJ, Hockings BE. Verapamil withdrawal as a possible cause of myocardial infarction in a hypertensive woman with a normal coronary angiogram. Med J Aust. 1988;149:218. [PubMed] |
| 5. | Kostis WJ, Suh WM, Palacios IF. Acute myocardial infarction caused by multivessel coronary spasm due to calcium channel blocker withdrawal. Catheter Cardiovasc Interv. 2011;78:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Kurabayashi M, Okishige K, Asano M, Suzuki H, Shimura T, Iwai S, Kato N, Ihara K, Aoyagi H, Isobe M. Cardiopulmonary arrest caused by coronary spasm after coronary vasodilator withdrawal during the peri-operative period of gastrectomy. Intern Med. 2013;52:81-84. [PubMed] |
| 7. | Koshiba K, Hoka S. Clinical characteristics of perioperative coronary spasm: reviews of 115 case reports in Japan. J Anesth. 2001;15:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Nagayoshi Y, Kawano H, Kojima S, Soejima H, Kaikita K, Nakayama M, Sumida H, Sugiyama S, Ogawa H. Significance of coronary vasospasm in the perioperative management of non-cardiac surgery. Circ J. 2012;76:1965-1971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Dalal JJ, Yao L, Parker JO. Nitrate tolerance: influence of isosorbide dinitrate on the hemodynamic and antianginal effects of nitroglycerin. J Am Coll Cardiol. 1983;2:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Parker J. Nitrate tolerance. A relevant clinical problem? Drugs. 1987;33 Suppl 4:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Hirai N, Kawano H, Yasue H, Shimomura H, Miyamoto S, Soejima H, Kajiwara I, Sakamoto T, Yoshimura M, Nakamura H. Attenuation of nitrate tolerance and oxidative stress by an angiotensin II receptor blocker in patients with coronary spastic angina. Circulation. 2003;108:1446-1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |