Published online Jul 26, 2014. doi: 10.4330/wjc.v6.i7.663
Revised: April 16, 2014
Accepted: May 29, 2014
Published online: July 26, 2014
Processing time: 180 Days and 21.3 Hours
Chronic inflammatory mechanisms in the arterial wall lead to atherosclerosis, and include endothelial cell damage, inflammation, apoptosis, lipoprotein deposition, calcification and fibrosis. Cardiac computed tomography angiography (CCTA) has been shown to be a promising tool for non-invasive assessment of theses specific compositional and structural changes in coronary arteries. This review focuses on the technical background of CCTA-based quantitative plaque characterization. Furthermore, we discuss the available evidence for CCTA-based plaque characterization and the potential role of CCTA for risk stratification of patients with coronary artery disease.
Core tip: This review gives an overview of the current status of noninvasive assessment of coronary artery disease (CAD) and the ability of cardiac computed tomography angiography (CCTA) and cardiac biomarkers for the diagnostic classification and risk stratification of patients with suspected and known CAD. Since all techniques described herein are available in the clinical routine and are associated with an acceptable time spent the translation to the clinical realm appears promising. Focusing on CCTA-based quantitative plaque characterization we herein present the (1) available evidence; (2) comparison with other techniques of plaque characterization; and (3) the value of “bio-imaging” for the risk stratification of patients with CAD.
- Citation: Gitsioudis G, Katus HA, Korosoglou G. Assessment of coronary artery disease using coronary computed tomography angiography and biochemical markers. World J Cardiol 2014; 6(7): 663-670
- URL: https://www.wjgnet.com/1949-8462/full/v6/i7/663.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i7.663
Sudden vessel occlusion as a consequence of atherosclerotic plaque rupture with subsequent coronary artery thrombosis is the most common cause of acute myocardial infarction (AMI) and sudden cardiac death in the industrialized world[1]. Conventional X-ray coronary angiography still remains the gold standard for detection of coronary artery disease (CAD). However, this technique is invasive and provides limited information on the composition of atherosclerotic plaque[2]. Coronary computed tomography angiography (CCTA) on the other hand, is a very fast evolving and in the meanwhile well-established non-invasive technique for the visualization of both coronary artery lumen narrowing and coronary calcification[3]. In addition, CCTA with the help of commercially available software tools provides objective and quantitative assessment of atherosclerotic plaque composition[4-6].
Based on recent developments with CCTA hardware and software technologies, including iterative reconstruction algorithms, a substantial reduction in radiation exposure and improvement of image quality could be achieved[7-11]. In addition, dedicated post-processing tools constituted major steps towards the reliable and quantitative assessment of atherosclerotic plaque composition[12-17].
The growing body of evidence for the prognostic value of CCTA-based plaque characterization underscores its potential for implementation in the clinical realm. In this regard, features indicating plaque vulnerability include a large necrotic core, thin fibrous cap and positive vessel remodeling[6,18-22]. The early and non-invasive detection of such vulnerable rupture-prone atherosclerotic lesions remains a major challenge in patient care.
First generation CCTA scanners offered limited ability for the reliable detection of coronary lesions due to technical limitations, including limited spatial and temporal resolution, and partial volume effects caused by coronary calcifications. With the development of 256- or even 320-slice multi-slice CT-scanners however, faster gantry rotation speed, Z-direction focal-spot sampling and spherical detector design could overcome these limitations, offering high isotropic spatial resolution of approximately 400-600 μm and a temporal resolution of approximately 83-175 ms[7,9,23-26].
Current SCCT guidelines introduced a scheme for the qualitative characterization of different plaque types for clinical reporting[27]. In general, the percentage of calcium content is < 20% in non-calcified plaque, between 20% and 80% in mixed plaque and > 80% in calcified plaque. The reproducibility of this qualitative assessment (calcified, non-calcified, mixed plaques) has been shown to be good for both intra- and inter-observer agreements with more than 88%[28,29]. The accuracy of this qualitative plaque characterization approach has been validated by virtual histology-intravascular ultrasound (VH-IVUS) for different plaque types[30].
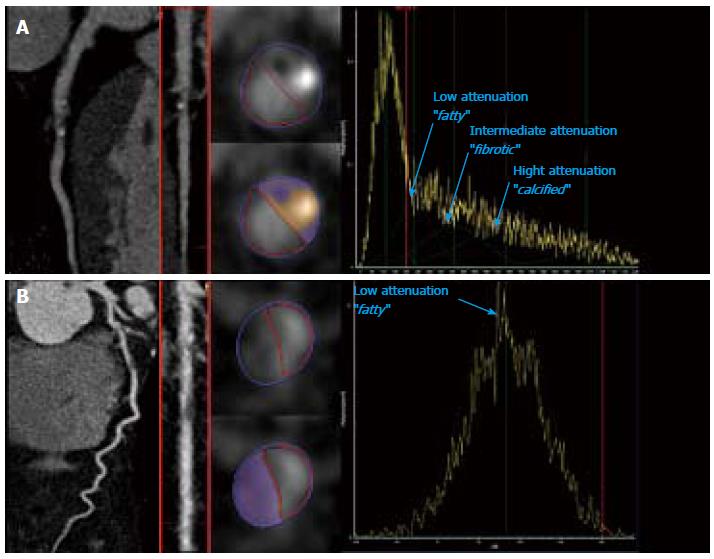
Others and we showed the feasibility and practicability of semi-automated and automated post-processing software tools for the quantitative assessment of atherosclerotic coronary plaque size and composition in patients undergoing CCTA for clinical reasons[17,31-33]. This volumetric approach allows for assessment of (1) total plaque volume, (2) plaque composition (distribution of (non-) calcified content) and (3) maximum, mean and minimum plaque intensities in hounsfield units (HU). Hoffman et al[33] showed that limits of agreement are approximately 60% for small volumes (10 mm3) and 28% for larger volumes (100 mm3). According to the tissue specific attenuation properties, three different plaque components can potentially be distinguished, including: (1) lipid-rich (14-70 HU); (2) fibrotic (71-150 HU); and (3) calcified components (> 150-200 HU)[14]. Lipid and fibrotic plaque components are often summarized as “non-calcified”. However, there is still a lack of a uniform attenuation cut-off values defining these tissue qualities due to overlapping attenuation intervals. Figure 1 shows representative examples of a (A) non-calcified and (B) of a partially calcified atherosclerotic coronary plaques with the corresponding Gaussian curves, respectively for different plaque components.
Previous ex vivo studies compared CCTA-based plaque characteristics with histopathology[34-36]. In this regard, 16- and 64-slice CCTA provided precise detection of calcified lesion, while its accuracy for the differentiation between lipid-rich and fibrotic components was lower[37-39]. Further experimental studies are now warranted to reevaluate the potential of 256- and 320-slice scanners in this context.
VH-IVUS with radiofrequency backscatter analysis is the clinical gold standard technique for the visualization of coronary vessel wall morphology[40,41]. In ex vivo studies of coronary arteries, IVUS has been shown to successful identify plaque features as regional calcification, lipid-rich necrotic cores and fibro-fatty plaques with high accuracy[42-44]. From a clinical point of view, the PROSPECTIVE trial could show the prognostic impact of IVUS-based plaque characterization in patients with acute coronary syndromes[21]. In contrast to CCTA, VH-IVUS enables for detailed measurement of fibrous cap thickness and for the detection of thin-cap fibroatheromas (TCFA)[38,45]. Pundziute et al30] showed that 32% of partially calcified plaques in CCTA were characterized as TCFA by VH-IVUS.
However, there are still some limitations both during IVUS data acquisition and in the post-processing raw data handling[46]. In addition, the assessment of the entire coronary tree requires a 3-vessel catheter-based interrogation, which may involve additional risks for the patients[21]. In this regard, CCTA would be a valuable non-invasive alternative to IVUS, especially in light of the good correlation of the 2 techniques in terms of plaque composition assessment[14,32,38,47-49].
Other intravascular imaging techniques like optical coherence tomography (OCT) and near infrared spectroscopy (NIS) have also been applied for the assessment of coronary plaque composition. OCT which is the light analogue of IVUS enables for a resolution of 10-20 μm, which is about 10 times higher than that provided by IVUS. OCT detects erosions and can also differentiate between red and white thrombus[50]. However, OCT cannot visualize vessel wall structures under the condition of blood flow, has limited penetration depths of 1-2 mm, and is therefore not appropriate for deeper imaging of blood vessels[51]. Despite continuing improvements in the performance of both IVUS and OCT, their use has been mostly limited to structural imaging so far. On the other hand, near infrared spectroscopy (NIS) belongs to a different class of imaging methods which measures absorption spectra from blood vessels in order to assess lipid content[51,52]. However, additional experimental and clinical data are required to assess the methodological reliability and to define precise clinical applications with this technique. Finally, the detection of lipid subtypes, such as oxidized low-density lipoprotein (ox LDL) is still limited using NIS.
The primary adverse outcome of CAD is acute myocardial infarction (AMI) and sudden cardiac death. Therefore, there is a great need for robust diagnostic algorithms, which may include cardiac biomarkers and non-invasive imaging techniques, for the risk stratification of patients with subclinical or presumably stable CAD. In this regard, the detection of rupture-prone coronary plaques or of elevated cardiac troponins may help the classification of patients with presumably low risk vs those with high-risk, aiding in the guidance of pharmacologic and interventional treatment strategies. Non-invasive assessment of functional wall motion analysis by dobutamine stress cardiac magnetic resonance imaging (MRI) or stress echocardiography has also been shown to identify patients at high risk for future cardiac events[53,54]. However, in contrast to CCTA these imaging modalities provide no information on coronary artery pathologies and plaque composition.
Several cardiovascular biomarkers are well established in clinical routine to complement clinical assessment and 12-lead ECG in the diagnosis, risk stratification, triage, and management of patients with suspected acute coronary syndrome (ACS). Especially cardiac troponins were shown to aid the diagnostic classification and risk stratification of patients with ACS[55-57]. Recently others and we could show an association between CTA atherosclerotic plaque characteristics and small blood level troponin increases in patients with stable CAD[58,59], which could be explained by chronic clinically silent rupture of non-calcified plaque with subsequent microembolisation. In an experimental setting, high mobility group box 1 (HMBG1) protein was found to be a critical mediator of acute ischemic injury, predicting adverse outcomes after myocardial infarction[60,61]. In addition, we could show that HMBG1 serum levels are associated with coronary calcification and with non-calcified plaque composition in patients with suspected or known stable CAD[62].
Incorporation of ox-LDL transforms macrophages into foam cells, which built the core of atherosclerotic plaques. In this regard, the presence and extent of non-calcified plaques are associated with high non-HDL, which suggest a relationship between lipid profile and plaque composition[63,64].
CRP was initially supposed to be a causal player for atherosclerotic plaque development and inflammation[65]. However, further basic science research has questioned a direct atherogenic mechanism[66,67]. Others and we could show that serum levels of hsCRP are only weakly correlated with plaque composition and coronary artery calcification and largely determined by the presence of risk factors[58,68,69]. More specific markers of inflammation could provide a stronger association with plaque formation and atherosclerotic inflammation. In this regard, the dal-PLAQUE study recently showed that myeloperoxidase levels are associated with carotid plaque inflammation, which was assessed using 18F-fluorodeoxyglucose positron emission tomography/computed tomography[70]. An overview of the most interesting studies in the area of comprehensive “bio-imaging” using cardiac computed tomography and biomarkers are presented in Table 1.
| Ref. | Biochemical markers | CT scanner | Number of patients | Results |
| Laufer et al[59] | hsTnT | 64-sl. MDCT | 615 | Even mild CAD is associated with hsTnT levels in symptomatic patients |
| Korosoglou et al[58] | hsTnT | ≥ 64-sl. MDCT | 124 | hsTnT is associated with the extend of positive remodeled NCP. Only weak association was detected for hsCRP |
| Blaha et al[68] | hsCRP | 4-sl. MDCT | 6762 | hsCRP was not associated with coronary artery calcification |
| Duivenvoorden et al[70] | hsCRP, MPO, and others | 18FDG-PET/CT | 130 | MPO levels are associated with carotid plaque inflammation |
| Andrassy et al[62] | HMBG-1 | 256-sl. MDCT | 152 | HMBG1 is associated with the composition and extend of atherosclerotic plaques |
| Nakazato et al[64] | LDL, HDL, TC | ≥ 64-sl. MDCT | 4575 | Presence and extend of NCP are associated with high non-HDL level |
| Voros et al[63] | ApoB, HDL, LDL | 64-sl. MDCT IVUS/VH | 60 | ApoB and small HDL particles are associated with larger plaque burden and more NCP plaque. Larger HDL and pre-b2-HDL particles are associated with plaque burden and less NCP |
Several CCTA outcome studies on the other hand, have assessed the prognostic value of plaque burden and plaque morphology in both symptomatic and asymptomatic cohorts[18,71-74]. The value of risk assessment in patients with CAD using a CCTA-based semi-automated plaque assessment has been recently shown[6]. Ongoing studies now investigate the potential complementary value of high-sensitive Troponin T (hsTnT) and quantitatively assessed coronary plaque burden for the risk stratification of patients with intermediate likelihood for CAD.
Imaging of coronary artery disease using CCTA is a feasible and robust approach for non-invasive plaque characterization. Growing body of evidence exists for the ability of CCTA based quantitative plaque characterization for the prediction of clinical outcome in patients with suspected or known coronary artery disease.
P- Reviewer: Biondi-Zoccai G S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, Badimon JJ, Stefanadis C, Moreno P, Pasterkamp G. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part II. Circulation. 2003;108:1772-1778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1874] [Cited by in RCA: 1802] [Article Influence: 81.9] [Reference Citation Analysis (0)] |
| 2. | Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6017] [Cited by in RCA: 6025] [Article Influence: 262.0] [Reference Citation Analysis (0)] |
| 3. | Voros S, Rinehart S, Qian Z, Joshi P, Vazquez G, Fischer C, Belur P, Hulten E, Villines TC. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging. 2011;4:537-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 275] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 4. | Achenbach S, Moselewski F, Ropers D, Ferencik M, Hoffmann U, MacNeill B, Pohle K, Baum U, Anders K, Jang IK. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation. 2004;109:14-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 644] [Cited by in RCA: 600] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 5. | Schroeder S, Kopp AF, Baumbach A, Meisner C, Kuettner A, Georg C, Ohnesorge B, Herdeg C, Claussen CD, Karsch KR. Noninvasive detection and evaluation of atherosclerotic coronary plaques with multislice computed tomography. J Am Coll Cardiol. 2001;37:1430-1435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 554] [Cited by in RCA: 507] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 6. | Versteylen MO, Kietselaer BL, Dagnelie PC, Joosen IA, Dedic A, Raaijmakers RH, Wildberger JE, Nieman K, Crijns HJ, Niessen WJ. Additive value of semiautomated quantification of coronary artery disease using cardiac computed tomographic angiography to predict future acute coronary syndrome. J Am Coll Cardiol. 2013;61:2296-2305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 158] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 7. | de Graaf FR, Schuijf JD, van Velzen JE, Kroft LJ, de Roos A, Reiber JH, Boersma E, Schalij MJ, Spanó F, Jukema JW. Diagnostic accuracy of 320-row multidetector computed tomography coronary angiography in the non-invasive evaluation of significant coronary artery disease. Eur Heart J. 2010;31:1908-1915. [PubMed] |
| 8. | Hosch W, Heye T, Schulz F, Lehrke S, Schlieter M, Giannitsis E, Kauczor HU, Katus HA, Korosoglou G. Image quality and radiation dose in 256-slice cardiac computed tomography: comparison of prospective versus retrospective image acquisition protocols. Eur J Radiol. 2011;80:127-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Chao SP, Law WY, Kuo CJ, Hung HF, Cheng JJ, Lo HM, Shyu KG. The diagnostic accuracy of 256-row computed tomographic angiography compared with invasive coronary angiography in patients with suspected coronary artery disease. Eur Heart J. 2010;31:1916-1923. [PubMed] |
| 10. | Hausleiter J, Martinoff S, Hadamitzky M, Martuscelli E, Pschierer I, Feuchtner GM, Catalán-Sanz P, Czermak B, Meyer TS, Hein F. Image quality and radiation exposure with a low tube voltage protocol for coronary CT angiography results of the PROTECTION II Trial. JACC Cardiovasc Imaging. 2010;3:1113-1123. [PubMed] |
| 11. | Hosch W, Stiller W, Mueller D, Gitsioudis G, Welzel J, Dadrich M, Buss SJ, Giannitsis E, Kauczor HU, Katus HA. Reduction of radiation exposure and improvement of image quality with BMI-adapted prospective cardiac computed tomography and iterative reconstruction. Eur J Radiol. 2012;81:3568-3576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Hamon M, Biondi-Zoccai GG, Malagutti P, Agostoni P, Morello R, Valgimigli M, Hamon M. Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: a meta-analysis. J Am Coll Cardiol. 2006;48:1896-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 317] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 13. | Mollet NR, Cademartiri F, Krestin GP, McFadden EP, Arampatzis CA, Serruys PW, de Feyter PJ. Improved diagnostic accuracy with 16-row multi-slice computed tomography coronary angiography. J Am Coll Cardiol. 2005;45:128-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 190] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 14. | Pohle K, Achenbach S, Macneill B, Ropers D, Ferencik M, Moselewski F, Hoffmann U, Brady TJ, Jang IK, Daniel WG. Characterization of non-calcified coronary atherosclerotic plaque by multi-detector row CT: comparison to IVUS. Atherosclerosis. 2007;190:174-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 202] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 15. | Ropers D, Rixe J, Anders K, Küttner A, Baum U, Bautz W, Daniel WG, Achenbach S. Usefulness of multidetector row spiral computed tomography with 64- x 0.6-mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenoses. Am J Cardiol. 2006;97:343-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 290] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 16. | Schmid M, Pflederer T, Jang IK, Ropers D, Sei K, Daniel WG, Achenbach S. Relationship between degree of remodeling and CT attenuation of plaque in coronary atherosclerotic lesions: an in-vivo analysis by multi-detector computed tomography. Atherosclerosis. 2008;197:457-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Korosoglou G, Mueller D, Lehrke S, Steen H, Hosch W, Heye T, Kauczor HU, Giannitsis E, Katus HA. Quantitative assessment of stenosis severity and atherosclerotic plaque composition using 256-slice computed tomography. Eur Radiol. 2010;20:1841-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Otsuka K, Fukuda S, Tanaka A, Nakanishi K, Taguchi H, Yoshikawa J, Shimada K, Yoshiyama M. Napkin-ring sign on coronary CT angiography for the prediction of acute coronary syndrome. JACC Cardiovasc Imaging. 2013;6:448-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 264] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 19. | Tanaka A, Kawarabayashi T, Nishibori Y, Sano T, Nishida Y, Fukuda D, Shimada K, Yoshikawa J. No-reflow phenomenon and lesion morphology in patients with acute myocardial infarction. Circulation. 2002;105:2148-2152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 198] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 20. | Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47:C13-C18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1646] [Cited by in RCA: 1719] [Article Influence: 90.5] [Reference Citation Analysis (0)] |
| 21. | Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J, Farhat N, Marso SP. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2252] [Cited by in RCA: 2426] [Article Influence: 173.3] [Reference Citation Analysis (0)] |
| 22. | Narula J, Nakano M, Virmani R, Kolodgie FD, Petersen R, Newcomb R, Malik S, Fuster V, Finn AV. Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J Am Coll Cardiol. 2013;61:1041-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 394] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 23. | Ong TK, Chin SP, Liew CK, Chan WL, Seyfarth MT, Liew HB, Rapaee A, Fong YY, Ang CK, Sim KH. Accuracy of 64-row multidetector computed tomography in detecting coronary artery disease in 134 symptomatic patients: influence of calcification. Am Heart J. 2006;151:1323.e1-1323.e6. [PubMed] |
| 24. | Stolzmann P, Scheffel H, Leschka S, Plass A, Baumüller S, Marincek B, Alkadhi H. Influence of calcifications on diagnostic accuracy of coronary CT angiography using prospective ECG triggering. AJR Am J Roentgenol. 2008;191:1684-1689. [PubMed] |
| 25. | Hsiao EM, Rybicki FJ, Steigner M. CT coronary angiography: 256-slice and 320-detector row scanners. Curr Cardiol Rep. 2010;12:68-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 123] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 26. | Voros S. What are the potential advantages and disadvantages of volumetric CT scanning? J Cardiovasc Comput Tomogr. 2009;3:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ, Cheng V, DeFrance T, Hellinger JC, Karlsberg RP. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr. 2009;3:122-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 586] [Cited by in RCA: 627] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 28. | Lehman SJ, Schlett CL, Bamberg F, Lee H, Donnelly P, Shturman L, Kriegel MF, Brady TJ, Hoffmann U. Assessment of coronary plaque progression in coronary computed tomography angiography using a semiquantitative score. JACC Cardiovasc Imaging. 2009;2:1262-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 29. | Rinehart S, Vazquez G, Qian Z, Murrieta L, Christian K, Voros S. Quantitative measurements of coronary arterial stenosis, plaque geometry, and composition are highly reproducible with a standardized coronary arterial computed tomographic approach in high-quality CT datasets. J Cardiovasc Comput Tomogr. 2011;5:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 30. | Pundziute G, Schuijf JD, Jukema JW, Decramer I, Sarno G, Vanhoenacker PK, Reiber JH, Schalij MJ, Wijns W, Bax JJ. Head-to-head comparison of coronary plaque evaluation between multislice computed tomography and intravascular ultrasound radiofrequency data analysis. JACC Cardiovasc Interv. 2008;1:176-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 121] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 31. | Otsuka M, Bruining N, Van Pelt NC, Mollet NR, Ligthart JM, Vourvouri E, Hamers R, De Jaegere P, Wijns W, Van Domburg RT. Quantification of coronary plaque by 64-slice computed tomography: a comparison with quantitative intracoronary ultrasound. Invest Radiol. 2008;43:314-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 32. | Boogers MJ, Broersen A, van Velzen JE, de Graaf FR, El-Naggar HM, Kitslaar PH, Dijkstra J, Delgado V, Boersma E, de Roos A. Automated quantification of coronary plaque with computed tomography: comparison with intravascular ultrasound using a dedicated registration algorithm for fusion-based quantification. Eur Heart J. 2012;33:1007-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 190] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 33. | Hoffmann U, Moselewski F, Nieman K, Jang IK, Ferencik M, Rahman AM, Cury RC, Abbara S, Joneidi-Jafari H, Achenbach S. Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography. J Am Coll Cardiol. 2006;47:1655-1662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 437] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 34. | Becker CR, Nikolaou K, Muders M, Babaryka G, Crispin A, Schoepf UJ, Loehrs U, Reiser MF. Ex vivo coronary atherosclerotic plaque characterization with multi-detector-row CT. Eur Radiol. 2003;13:2094-2098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 180] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 35. | Schroeder S, Kuettner A, Leitritz M, Janzen J, Kopp AF, Herdeg C, Heuschmid M, Burgstahler C, Baumbach A, Wehrmann M. Reliability of differentiating human coronary plaque morphology using contrast-enhanced multislice spiral computed tomography: a comparison with histology. J Comput Assist Tomogr. 2004;28:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 122] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 36. | Nikolaou K, Becker CR, Muders M, Babaryka G, Scheidler J, Flohr T, Loehrs U, Reiser MF, Fayad ZA. Multidetector-row computed tomography and magnetic resonance imaging of atherosclerotic lesions in human ex vivo coronary arteries. Atherosclerosis. 2004;174:243-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 72] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 37. | Schroeder S, Kuettner A, Wojak T, Janzen J, Heuschmid M, Athanasiou T, Beck T, Burgstahler C, Herdeg C, Claussen CD. Non-invasive evaluation of atherosclerosis with contrast enhanced 16 slice spiral computed tomography: results of ex vivo investigations. Heart. 2004;90:1471-1475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Obaid DR, Calvert PA, Gopalan D, Parker RA, Hoole SP, West NE, Goddard M, Rudd JH, Bennett MR. Atherosclerotic plaque composition and classification identified by coronary computed tomography: assessment of computed tomography-generated plaque maps compared with virtual histology intravascular ultrasound and histology. Circ Cardiovasc Imaging. 2013;6:655-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 39. | Sarwar A, Rieber J, Mooyaart EA, Seneviratne SK, Houser SL, Bamberg F, Raffel OC, Gupta R, Kalra MK, Pien H. Calcified plaque: measurement of area at thin-section flat-panel CT and 64-section multidetector CT and comparison with histopathologic findings. Radiology. 2008;249:301-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 40. | García-García HM, Mintz GS, Lerman A, Vince DG, Margolis MP, van Es GA, Morel MA, Nair A, Virmani R, Burke AP. Tissue characterisation using intravascular radiofrequency data analysis: recommendations for acquisition, analysis, interpretation and reporting. EuroIntervention. 2009;5:177-189. [PubMed] |
| 41. | Mehta SK, McCrary JR, Frutkin AD, Dolla WJ, Marso SP. Intravascular ultrasound radiofrequency analysis of coronary atherosclerosis: an emerging technology for the assessment of vulnerable plaque. Eur Heart J. 2007;28:1283-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 42. | Murashige A, Hiro T, Fujii T, Imoto K, Murata T, Fukumoto Y, Matsuzaki M. Detection of lipid-laden atherosclerotic plaque by wavelet analysis of radiofrequency intravascular ultrasound signals: in vitro validation and preliminary in vivo application. J Am Coll Cardiol. 2005;45:1954-1960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 43. | Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002;106:2200-2206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 785] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 44. | Nair A, Margolis MP, Kuban BD, Vince DG. Automated coronary plaque characterisation with intravascular ultrasound backscatter: ex vivo validation. EuroIntervention. 2007;3:113-120. [PubMed] |
| 45. | Kubo T, Imanishi T, Takarada S, Kuroi A, Ueno S, Yamano T, Tanimoto T, Matsuo Y, Masho T, Kitabata H. Assessment of culprit lesion morphology in acute myocardial infarction: ability of optical coherence tomography compared with intravascular ultrasound and coronary angioscopy. J Am Coll Cardiol. 2007;50:933-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 625] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 46. | Garcìa-Garcìa HM, Gogas BD, Serruys PW, Bruining N. IVUS-based imaging modalities for tissue characterization: similarities and differences. Int J Cardiovasc Imaging. 2011;27:215-224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 127] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 47. | Choi BJ, Kang DK, Tahk SJ, Choi SY, Yoon MH, Lim HS, Kang SJ, Yang HM, Park JS, Zheng M. Comparison of 64-slice multidetector computed tomography with spectral analysis of intravascular ultrasound backscatter signals for characterizations of noncalcified coronary arterial plaques. Am J Cardiol. 2008;102:988-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 48. | Voros S, Rinehart S, Vazquez-Figueroa JG, Kalynych A, Karmpaliotis D, Qian Z, Joshi PH, Anderson H, Murrieta L, Wilmer C. Prospective, head-to-head comparison of quantitative coronary angiography, quantitative computed tomography angiography, and intravascular ultrasound for the prediction of hemodynamic significance in intermediate and severe lesions, using fractional flow reserve as reference standard (from the ATLANTA I and II Study). Am J Cardiol. 2014;113:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 49. | Voros S, Rinehart S, Qian Z, Vazquez G, Anderson H, Murrieta L, Wilmer C, Carlson H, Taylor K, Ballard W. Prospective validation of standardized, 3-dimensional, quantitative coronary computed tomographic plaque measurements using radiofrequency backscatter intravascular ultrasound as reference standard in intermediate coronary arterial lesions: results from the ATLANTA (assessment of tissue characteristics, lesion morphology, and hemodynamics by angiography with fractional flow reserve, intravascular ultrasound and virtual histology, and noninvasive computed tomography in atherosclerotic plaques) I study. JACC Cardiovasc Interv. 2011;4:198-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 156] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 50. | Kume T, Akasaka T, Kawamoto T, Ogasawara Y, Watanabe N, Toyota E, Neishi Y, Sukmawan R, Sadahira Y, Yoshida K. Assessment of coronary arterial thrombus by optical coherence tomography. Am J Cardiol. 2006;97:1713-1717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 338] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 51. | Rosenthal A, Jaffer FA, Ntziachristos V. Intravascular multispectral optoacoustic tomography of atherosclerosis: prospects and challenges. Imaging Med. 2012;4:299-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 52. | Waxman S, Dixon SR, L’Allier P, Moses JW, Petersen JL, Cutlip D, Tardif JC, Nesto RW, Muller JE, Hendricks MJ. In vivo validation of a catheter-based near-infrared spectroscopy system for detection of lipid core coronary plaques: initial results of the SPECTACL study. JACC Cardiovasc Imaging. 2009;2:858-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 196] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 53. | Bjork Ingul C, Rozis E, Slordahl SA, Marwick TH. Incremental value of strain rate imaging to wall motion analysis for prediction of outcome in patients undergoing dobutamine stress echocardiography. Circulation. 2007;115:1252-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 54. | Korosoglou G, Gitsioudis G, Voss A, Lehrke S, Riedle N, Buss SJ, Zugck C, Giannitsis E, Osman NF, Katus HA. Strain-encoded cardiac magnetic resonance during high-dose dobutamine stress testing for the estimation of cardiac outcomes: comparison to clinical parameters and conventional wall motion readings. J Am Coll Cardiol. 2011;58:1140-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 55. | Katus HA, Remppis A, Neumann FJ, Scheffold T, Diederich KW, Vinar G, Noe A, Matern G, Kuebler W. Diagnostic efficiency of troponin T measurements in acute myocardial infarction. Circulation. 1991;83:902-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 511] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 56. | Korosoglou G, Labadze N, Hansen A, Selter C, Giannitsis E, Katus H, Kuecherer H. Usefulness of real-time myocardial perfusion imaging in the evaluation of patients with first time chest pain. Am J Cardiol. 2004;94:1225-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 57. | Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Katus HA, Lindahl B, Morrow DA, Clemmensen PM. Third universal definition of myocardial infarction. Circulation. 2012;126:2020-2035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2200] [Cited by in RCA: 2477] [Article Influence: 190.5] [Reference Citation Analysis (0)] |
| 58. | Korosoglou G, Lehrke S, Mueller D, Hosch W, Kauczor HU, Humpert PM, Giannitsis E, Katus HA. Determinants of troponin release in patients with stable coronary artery disease: insights from CT angiography characteristics of atherosclerotic plaque. Heart. 2011;97:823-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 153] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 59. | Laufer EM, Mingels AM, Winkens MH, Joosen IA, Schellings MW, Leiner T, Wildberger JE, Narula J, Van Dieijen-Visser MP, Hofstra L. The extent of coronary atherosclerosis is associated with increasing circulating levels of high sensitive cardiac troponin T. Arterioscler Thromb Vasc Biol. 2010;30:1269-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 60. | Andrassy M, Volz HC, Igwe JC, Funke B, Eichberger SN, Kaya Z, Buss S, Autschbach F, Pleger ST, Lukic IK. High-mobility group box-1 in ischemia-reperfusion injury of the heart. Circulation. 2008;117:3216-3226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 514] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 61. | Andrassy M, Volz HC, Riedle N, Gitsioudis G, Seidel C, Laohachewin D, Zankl AR, Kaya Z, Bierhaus A, Giannitsis E. HMGB1 as a predictor of infarct transmurality and functional recovery in patients with myocardial infarction. J Intern Med. 2011;270:245-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 62. | Andrassy M, Volz HC, Schuessler A, Gitsioudis G, Hofmann N, Laohachewin D, Wienbrandt AR, Kaya Z, Bierhaus A, Giannitsis E. HMGB1 is associated with atherosclerotic plaque composition and burden in patients with stable coronary artery disease. PLoS One. 2012;7:e52081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 63. | Voros S, Joshi P, Qian Z, Rinehart S, Vazquez-Figueroa JG, Anderson H, Elashoff M, Murrieta L, Karmpaliotis D, Kalynych A. Apoprotein B, small-dense LDL and impaired HDL remodeling is associated with larger plaque burden and more noncalcified plaque as assessed by coronary CT angiography and intravascular ultrasound with radiofrequency backscatter: results from the ATLANTA I study. J Am Heart Assoc. 2013;2:e000344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 64. | Nakazato R, Gransar H, Berman DS, Cheng VY, Lin FY, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ. Relationship of low- and high-density lipoproteins to coronary artery plaque composition by CT angiography. J Cardiovasc Comput Tomogr. 2013;7:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 65. | Zhang YX, Cliff WJ, Schoefl GI, Higgins G. Coronary C-reactive protein distribution: its relation to development of atherosclerosis. Atherosclerosis. 1999;145:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 137] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 66. | Clapp BR, Hirschfield GM, Storry C, Gallimore JR, Stidwill RP, Singer M, Deanfield JE, MacAllister RJ, Pepys MB, Vallance P. Inflammation and endothelial function: direct vascular effects of human C-reactive protein on nitric oxide bioavailability. Circulation. 2005;111:1530-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 137] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 67. | Koike T, Kitajima S, Yu Y, Nishijima K, Zhang J, Ozaki Y, Morimoto M, Watanabe T, Bhakdi S, Asada Y. Human C-reactive protein does not promote atherosclerosis in transgenic rabbits. Circulation. 2009;120:2088-2094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 81] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 68. | Blaha MJ, Rivera JJ, Budoff MJ, Blankstein R, Agatston A, O’Leary DH, Cushman M, Lakoski S, Criqui MH, Szklo M. Association between obesity, high-sensitivity C-reactive protein ≥2 mg/L, and subclinical atherosclerosis: implications of JUPITER from the Multi-Ethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol. 2011;31:1430-1438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 69. | Hamirani YS, Pandey S, Rivera JJ, Ndumele C, Budoff MJ, Blumenthal RS, Nasir K. Markers of inflammation and coronary artery calcification: a systematic review. Atherosclerosis. 2008;201:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 70. | Duivenvoorden R, Mani V, Woodward M, Kallend D, Suchankova G, Fuster V, Rudd JH, Tawakol A, Farkouh ME, Fayad ZA. Relationship of serum inflammatory biomarkers with plaque inflammation assessed by FDG PET/CT: the dal-PLAQUE study. JACC Cardiovasc Imaging. 2013;6:1087-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 71. | Andreini D, Pontone G, Mushtaq S, Bartorelli AL, Bertella E, Antonioli L, Formenti A, Cortinovis S, Veglia F, Annoni A. A long-term prognostic value of coronary CT angiography in suspected coronary artery disease. JACC Cardiovasc Imaging. 2012;5:690-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 154] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 72. | Hadamitzky M, Distler R, Meyer T, Hein F, Kastrati A, Martinoff S, Schömig A, Hausleiter J. Prognostic value of coronary computed tomographic angiography in comparison with calcium scoring and clinical risk scores. Circ Cardiovasc Imaging. 2011;4:16-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 73. | Motoyama S, Sarai M, Harigaya H, Anno H, Inoue K, Hara T, Naruse H, Ishii J, Hishida H, Wong ND. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54:49-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1024] [Cited by in RCA: 1079] [Article Influence: 67.4] [Reference Citation Analysis (0)] |
| 74. | Bamberg F, Sommer WH, Hoffmann V, Achenbach S, Nikolaou K, Conen D, Reiser MF, Hoffmann U, Becker CR. Meta-analysis and systematic review of the long-term predictive value of assessment of coronary atherosclerosis by contrast-enhanced coronary computed tomography angiography. J Am Coll Cardiol. 2011;57:2426-2436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |