Published online Jun 26, 2014. doi: 10.4330/wjc.v6.i6.514
Revised: April 8, 2014
Accepted: May 13, 2014
Published online: June 26, 2014
Processing time: 199 Days and 10.7 Hours
Acute myocardial infarction should be diagnosed as early as possible for the appropriate management to salvage ischemic myocardium. Accurate diagnosis is typically based on the typical symptoms of angina. Headache is an unusual symptom in patients with acute myocardial infraction. We report a patient with ST-segment elevation acute myocardial infarction who presented to the emergency department complaining of severe occipital headache without chest discomfort.
Core tip: The association of headache with myocardial ischemia is unusual and is accompanied by chest discomfort. The only symptom of this patient was occipital headache and this is extremely rare. Owing to the rare occurrence of headache as a symptom of myocardial ischemia, diagnosis may be extremely difficult since a brain computed tomography imaging is important to rule out the possibility of hemorrhage.
- Citation: Asvestas D, Vlachos K, Salachas A, Letsas KP, Sideris A. Headache: An unusual presentation of acute myocardial infraction. World J Cardiol 2014; 6(6): 514-516
- URL: https://www.wjgnet.com/1949-8462/full/v6/i6/514.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i6.514
Atypical symptoms of myocardial infarction may delay the diagnosis, and therefore the proper management to rescue ischemic myocardium. Headache represents a rare symptom of myocardial ischemia[1-5]. We report a patient with ST-segment elevation acute myocardial infarction who presented to the emergency department complaining of headache without chest discomfort.
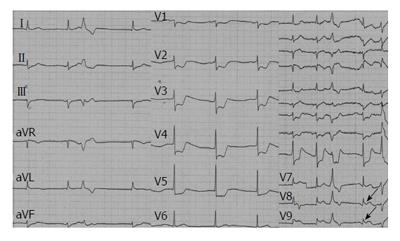
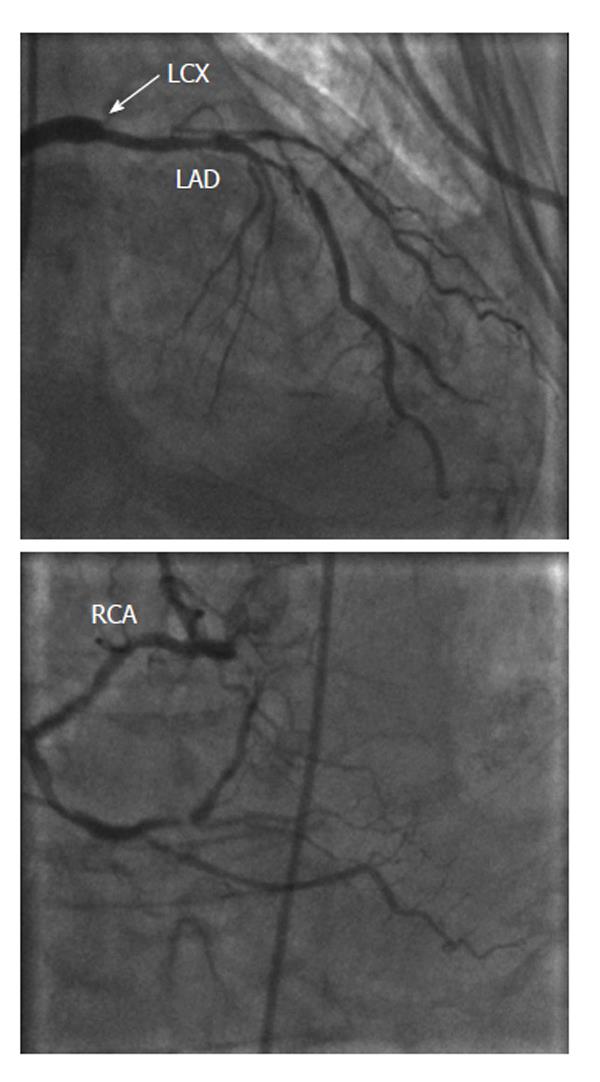
An 86-year-old man with a history of hypertension and tobacco use presented to the emergency department complaining of recent onset severe occipital headache. The patient did not report any chest pain, dyspnea, or other typical symptoms of angina. On admission the patient was pale with tachycardia (100 beats/min), and, while his blood pressure was within normal range (100/60 mmHg). At auscultation, a mild systolic murmur was audible. The electrocardiogram (ECG) showed sinus bradycardia, ST-segment depression in leads V1-V5 and ST-segment elevation in posterior leads (V7-V9) (Figure 1). Transthoracic echocardiography revealed an impaired left ventricular ejection fraction (40%-45%) along with mild mitral valve regurgitation. Initial laboratory examinations showed elevated levels of high-sensitivity cardiac troponin T (250 ng/L). Due to his clinical presentation, a brain computed tomography (CT) imaging was immediately performed. The CT imaging was negative for intracerebral or subarachnoid hemorrhage. Following CT imaging, the patient prepared for cardiac catheterization and received aspirin (500 mg), clopidogrel (600 mg) and unfractionated heparin (70 U/kgr). Coronary angiography was performed 60 min after admission and demonstrated a three-vessel coronary artery disease [the proximal left circumflex artery (LCX) was totally obstructed, the left anterior descending artery (LAD) displayed a severe stenosis and the right coronary artery was also severely diseased] (Figure 2). Proximal LAD lesion was directly stented, while the blood flow was restored in LCX artery revealing a severe stenosis of more than 90%. We attempted to insert the guidewire into the LCX but failed to cross the proximal part of LCX. Following revascularization, the patient was totally asymptomatic without headache, while the ECG was normalized (Figure 3). During the following days, the myocardial enzymes (CK-MB, hs-troponin T) followed the classic rise and fall kinetic pattern. He discharged 6 d later under dual antiplatelet (aspirin, clopidogrel), β-blocker and angiotensin converting enzyme inhibitor therapy.
Myocardial infarction should be diagnosed as early as possible for the appropriate management to salvage ischemic myocardium. Accurate diagnosis is based on both ECG and clinical presentation of the patient. Ischemia and myocardial infarction typically causes chest pain variously radiating elsewhere (shoulders, upper extremities and epigastrium). The association of headaches with myocardial ischemia is unusual and is accompanied by chest discomfort. The only symptom of this patient was occipital headache and this is extremely rare. Owing to the rare occurrence of headache as a symptom of myocardial ischemia, diagnosis may be extremely difficult since a brain CT imaging is important to rule out the possibility of hemorrhage.
The incidence of headache as a symptom of myocardial ischemia may be underestimated[1-5]. Culić et al[6] reported that headache is present (along with other symptoms) in 5.2% of patients with acute myocardial infarction. Moreover, in 3.4% of these patients headache was the primary complaint[6]. Cardiac cephalalgia or headache angina is a recognized phenomenon, but the pathophysiological mechanism is still unclear[7-8]. There is a connection between the central cardiac pathway and the cranial pain afferents. The cardiac sympathetic fibers originate from cervical lymph nodes which also innervate pain sensitive cranial structures[9-10]. Furthermore, it is hypothesized that chemical mediators like bradykinin, serotonin and histamine can induce pain in shoulders, arms, neck and in this case headache. Another mechanism is based on the elevated intracranial pressure associated in the case of decreased cardiac output during myocardial infarction and elevated venous pressure[11,12]. Finally, increased levels of atrial and brain natriuretic peptides may be involved in intracranial pressure regulation[13]. Even though the occurrence of headache as a sole manifestation of angina or myocardial infarction has been previously described, many clinicians ignore this unusual manifestation. The diagnosis of “cardiac headache” is difficult and requires a high degree of suspicion.
An 86-year-old man presented to the emergency department complaining of recent onset severe occipital headache.
The patient was pale with tachycardia and electrocardiogram (ECG) signs suggestive of myocardial infarction.
The differential diagnosis included intracerebral or subarachnoid hemorrhage and myocardial infarction.
Elevated levels of high-sensitivity cardiac troponin T were initially recorded.
Brain computed tomography imaging excluded intracerebral or subarachnoid hemorrhage, while coronary angiography demonstrated a three-vessel coronary artery disease.
Proximal left anterior descending artery lesion was directly stented, while the blood flow was restored in left circumflex artery artery revealing a severe stenosis of more than 90%.
Careful ECG interpretation in the setting of acute headache is of major importance.
Asvestas et al report a rare case of a patient who presented with headache as the sole symptom of an acute myocardial infarction. The mechanisms by which headache is linked to ischemic vascular disease remain uncertain and are likely to be complex. The paper is generally well-written and interesting.
P- Reviewers: Kurisu S, Petix NR, Vermeersch P S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Bowen J, Oppenheim G. Headache as a presentation of angina: reproduction of symptoms during angioplasty. Headache. 1993;33:238-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Korantzopoulos P, Karanikis P, Pappa E, Dimitroula V, Kountouris E, Siogas K. Acute non-ST-elevation myocardial infarction presented as occipital headache with impaired level of consciousness--a case report. Angiology. 2005;56:627-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Chatzizisis YS, Saravakos P, Boufidou A, Parharidou D, Styliadis I. Acute myocardial infarction manifested with headache. Open Cardiovasc Med J. 2010;4:148-150. [PubMed] |
| 4. | Costopoulos C. Acute coronary syndromes can be a headache. Emerg Med J. 2011;28:71-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Falcone C, Bozzini S, Gazzaruso C, Calcagnino M, Ghiotto N, Falcone R, Coppola A, Giustina A, Pelissero G. Primary headache and silent myocardial ischemia in patients with coronary artery disease. Cardiology. 2013;125:133-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Culić V, Mirić D, Eterović D. Correlation between symptomatology and site of acute myocardial infarction. Int J Cardiol. 2001;77:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders. 2nd ed. Cephalalgia. 2004;24 Suppl 1:1-160. |
| 8. | Wang WW, Lin CS. Headache angina. Am J Emerg Med. 2008;26:387.e1-387.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Williams PL, Warwick R, Dyson M, eds . Gray’s anatomy, 37th ed. Livingstone: Edinburgh-Churchill 1989; 1158-1163. |
| 10. | Meller ST, Gebhart GF. A critical review of the afferent pathways and the potential chemical mediators involved in cardiac pain. Neuroscience. 1992;48:501-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 181] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 11. | Guazzi M, Polese A, Fiorentini C, Magrini F, Olivari MT, Bartorelli C. Left and right heart haemodynamics during spontaneous angina pectoris. Comparison between angina with ST segment depression and angina with ST segment elevation. Br Heart J. 1975;37:401-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 96] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Ramadan NM. Headache caused by raised intracranial pressure and intracranial hypotension. Curr Opin Neurol. 1996;9:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Yoshimura M, Yasue H, Morita E, Sakaino N, Jougasaki M, Kurose M, Mukoyama M, Saito Y, Nakao K, Imura H. Hemodynamic, renal, and hormonal responses to brain natriuretic peptide infusion in patients with congestive heart failure. Circulation. 1991;84:1581-1588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 291] [Article Influence: 8.6] [Reference Citation Analysis (0)] |