Published online Jun 26, 2014. doi: 10.4330/wjc.v6.i6.424
Revised: January 27, 2014
Accepted: April 9, 2014
Published online: June 26, 2014
Processing time: 189 Days and 7.9 Hours
Primary percutaneous coronary intervention (PPCI) is the preferred reperfusion therapy for patients presenting with ST-segment elevation myocardial infarction (STEMI) when it can be performed expeditiously and by experienced operators. In spite of excellent clinical results this technique is associated with longer delays than thrombolysis and this fact may nullify the benefit of selecting this therapeutic option. Several strategies have been proposed to decrease the temporal delays to deliver PPCI. Among them, prehospital diagnosis and direct transfer to the cath lab, by-passing the emergency department of hospitals, has emerged as an attractive way of diminishing delays. The purpose of this review is to address the effect of direct transfer on time delays and clinical events of patients with STEMI treated by PPCI.
Core tip: Primary angioplasty has emerged as the preferred reperfusion modality for patients with ST-segment elevation myocardial infarction. However, this treatment is associated with longer delays. Several strategies have been proposed to overcome these drawbacks. This review aimed to highlight the effect of a direct transfer strategy on time delays reduction and in the prognosis of this subgroup of patients.
- Citation: Estévez-Loureiro R, López-Sainz &, Pérez de Prado A, Cuellas C, Calviño Santos R, Alonso-Orcajo N, Salgado Fernández J, Vázquez-Rodríguez JM, López-Benito M, Fernández-Vázquez F. Timely reperfusion for ST-segment elevation myocardial infarction: Effect of direct transfer to primary angioplasty on time delays and clinical outcomes. World J Cardiol 2014; 6(6): 424-433
- URL: https://www.wjgnet.com/1949-8462/full/v6/i6/424.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i6.424
Primary percutaneous coronary intervention (PPCI) is the current preferred strategy to treat ST-segment elevation myocardial infarction (STEMI) when performed in a timely-fashion and by experienced operators. This technique has yielded superior results over thrombolytic therapy even when long transfer distances are accomplished[1-6].
It has been demonstrated a relevant prognostic role of reperfusion delays in STEMI and both door-to-balloon and total ischemic time have been linked to increasing mortality[7-9]. Current guidelines recommend that door-to-balloon delay must be inferior to 90-120 min[10,11]. However, time delays to deliver PPCI are usually longer than recommended in practice guidelines[12,13] and this may nullify the advantages of mechanical reperfusion over lysis[14,15]. To overcome this problem, several strategies have been proposed[16-18] and national efforts have been claimed to address all organizational issues either in United States or in Europe[19,20].
Among these strategies, direct transfer from the field, bypassing the emergency department, to the catheterization laboratory has emerged as a safe and effective protocol for minimizing PPCI-related delays[21-28]. We aimed to review the current evidence regarding the effect of DT on time delays and on clinical outcomes.
Experimental models have clearly shown that there is a close relationship between the extension of myocardial necrosis and the time elapsed since the coronary artery occlusion[29-31]. The myocardial damage extends as a “wavefront phenomenon” from the subendocardium to the subepicardium and the amount of muscle that can be saved by reperfusion is related to the time that flow can be restored[32].
In the clinical setting, this relationship was evident in the first studies where a reperfusion method was tested: the thrombolytic therapy. The GISSI trial compared the use of streptokinase against placebo in patients with STEMI and less than 12 h from symptom onset. The overall results showed a net clinical benefit of the thrombolytic therapy[33]. But when results were divided between time delay categories the significant benefit was observed only in those patients that received the lytic in the first 6 h since the start of the symptoms. This finding was subsequently confirmed in the fibrinolytic therapy trialists’ analyses where all studies including > 1000 STEMI patients and randomized to thrombolytic or placebo were included[34]. This metaanalysis showed that there was a linear relationship between the time to lytic therapy and the benefit in terms of mortality. The benefit was greater in the first hour (35 lives saved/1000 patients treated) and progressively decline every hour until 12 h since symptom onset. It was calculated that the loss of benefit of every hour of delay was 1.6 lives per every 1000 patients treated. No survival benefit was observed for those patients randomized after 12 h. However, this concept was challenged in a similar analysis but with more studies included by Boersma et al[35] (22 studies, every study with > 100 patients randomized). Authors showed that this time-survival relationship with lytics was better represented by a non-linear regression curve. Survival benefit was maximal in the first two h and thereafter it suffered a steep decline, maintaining the benefit until 12 h of delay.
The relationship between time delays and mortality was as well observed in the setting of PPCI. To assess this association two time intervals have been defined: time to treatment (TTT, interval elapsed between symptom onset and mechanical reperfusion) and door-to-balloon (DTB, time from arrival to interventional hospital and mechanical reperfusion). Both time intervals have been linked to mortality in STEMI patients treated by PPCI. De Luca et al[9] showed that every 30 min of delay in the delivery of PPCI increased the mortality by 7.5%. Cannon et al[7] analyzing the data from the NRMI-2 registry demonstrated as well that the DTB interval was associated with an increasing mortality, above all when it was greater than 120 min. This fact was confirmed subsequently in a more contemporary analysis of the NRMI-3 and 4 registries, noting that a DTB interval > 90 min was associated with worse prognosis[8]. However, several publications have addressed the issue that the time delay effect is related to the risk profile of the patients. In this sense, those patients exhibiting high risk features [anterior wall myocardial infarction (MI), previous MI, advanced Killip class, data of hemodynamic instability], those presenting very early after symptom onset (< 2-3 h) and those in cardiogenic shock, time delays play a key role in their prognosis. On the other hand, those patients of low risk or presenting late are less affected by the delays in reperfusion[36-39].
The aforementioned data allowed the establishment in the practice guidelines the recommended time intervals to deliver PPCI: a DTB time of ≤ 90-120 min[10,40,41]. If mechanical reperfusion cannot be achieved in this time frame, then a selection of thrombolytic therapy might be advisable. However, with the growing evidence of PPCI being superior to lytic therapy in terms of mortality and cardiac events, this mode of reperfusion rapidly gained adoption in the medical community[1]. Notwithstanding, it was rapidly pointed out that the widespread use of PPCI was translated into the fact that most of the patients received their reperfusion treatment out of the time schedule proposed by guidelines. In an analysis of the NRMI-4 registry, Nallamothu et al[12] showed that only 4.2% of patients treated by means of PPCI had a DTB time of less than 90 min. In a more recent analysis by Chakrabarti, including as well transferred patients form non-PPCI hospitals, only 9.9% of patients were into the boundaries of practice guidelines[13]. In Europe, even with a more organized system, delays are as well longer than suggested. Moreover, the retardation induced by the system of care is an independent factor associated with worse prognosis[42]. Several retrospectives studies have tried to elucidate the exact delay with PPCI which will nullify the clinical benefit compared to thrombolysis[14,15,43,44]. This time frame has varied from 60 to 120 min, but all studies have limitations inherent to post-hoc analysis and registries. Therefore, the exact delay assumable is still elusive and, moreover, it may depend on the risk profile of the individual patient[43,45]. Given the evidence supporting the benefit of PPCI over thrombolysis (even though when the patient should be transferred from a non-PPCI facility[6], and likely related to a more stable effect of reperfusion[46,47]) most of efforts of national societies is to implement STEMI networks well organized and strategies in order to minimize delays for a timely PPCI[19,20,48-50].
Taking the previous information into account, several efforts have been claimed to reduce the delays involved in the delivery of PPCI and there have been conducted studies to address the strategies associated with the greater reductions in time delays performing PPCI. Most of these studies have been conducted in United States through surveys to hospitals across the country and through analysis of how top hospitals develop their programs of PPCI[16,17,51-53]. The most comprehensive analysis of all studies published has been reported by Bradley et al[18]. Authors conducted a survey in 365 hospitals of United States trying to identify the independent predictors of lower DTB time. In their results 6 strategies were significantly associated with faster door-to-balloon interval: (1) Having an emergency physician activating the catheterization laboratory; (2) Having a single call to a central page operator activate the laboratory; (3) Having the emergency department activate the catheterization laboratory while the patient is en route to the hospital; (4) Expecting staff to arrive in the catheterization laboratory within 20 min after being paged; (5) Having an attending cardiologist always on site; and (6) Having staff in the emergency department and the catheterization laboratory use real-time data feedback.
Interestingly, the use of prehospital electrocardiogram (ECG) was not associated with lower delays in the overall population. However, this strategy was associated with significantly lower time intervals if the emergency medical system activated the cath lab team while the patient was on route to the hospital. Simply diagnosing STEMI in the prehospital setting, activate the interventional team and move the patient directly to the catheterization theater avoiding the emergency department or the coronary care unit is what we call direct transfer strategy (DT).
In recent years there have been several studies that have investigated the association of DT for PPCI with shorter time delays in the delivery of reperfusion. The publications differ in their geographic location, method of ECG interpretation, distance between the reference point and the cath lab and the definitions of the different intervals analyzed[21-26,28,54-63]. Furthermore, it is noteworthy that there is no randomized study on the subject and the evidence that we have rests on observational studies. That is why the results are heterogeneous and difficult to compare.
The results of the main studies regarding the effect of DT on time delays in PPCI are summarized in Table 1.
| n | DTB | TTT | FP | Staff | Ref. |
| 161 (DT 13) | 87 vs 168 | - | 14% | Physician | [24] |
| 658 (DT 25.2) | - | 146 vs 191 | - | Physician | [25] |
| 401 (DT 59.9) | 124 vs 154 (group PPCI) | - | - | Paramedics | [55] |
| 301 (DT 35.8) | 74 vs 116 | 150 vs 203 | 7% | Paramedics (teletransmission) | [28] |
| 344 (DT 39.2) | 69 vs 123 | 158 vs 230 | - | Paramedics | [21] |
| 1437 (DT 42.9) | 83 vs 103 | 150 vs 200 | - | Paramedics (teletransmission) | [26] |
| 581 (DT 78) | 69 vs 118 | 149 vs 219 | - | Paramedics (computed algorithm) | [61] |
| 1194 (DT 21) | 102 vs 125 | 189 vs 259 | 4.7% | Physician | [27] |
| 1859 (DT 23) | 105 vs 122 | 185 vs 255 | - | Physician | [67] |
The most relevant publications in terms of number of patients, methodology and results are those published by Le May et al[21], Pedersen et al [26], Dieker et al[61] and our group[27] . Le May et al[21] analyzed the effect of DT in 344 patients with STEMI treated in the metropolitan area of Ottawa. The farthest distance to the PPCI hospital was 59.5 km. In this publication 39.2% of patients were directly transferred to the catheterization laboratory. Notably, for various reasons 2% received fibrinolytic therapy. DT significantly shortened the time delays, with median DTB of 69 min compared to 123 min in the standard admission. A significant reduction in total ischemic time (median 158 min vs 230 min, P < 0.001) was also observed. Ambulances were handled by paramedics. Pedersen et al[26] analyzed their records of STEMI from 2005 to 2008 and included in the analysis 1437 patients of whom 42.9% were transferred directly to the catheterization laboratory. The study region covers a large population nucleus but investigators stress that the maximum transfer distance was 10 km and 90% within 60 min of the interventional hospital. For DTB interval definition the first medical contact instead of the arrival to the interventional hospital was selected. This is in accordance with the new recommendations for measuring these intervals when transferred patients from non-PCI facilities are included[64]. Direct transfer patients consistently showed less delay compared to the conventional admission strategy in the DTB interval (median 83 min vs 103 min, P < 0.001) and in the TTT time (median 150 min vs 200 min, P < 0.001). Sixty-one percent of patients were in the range of DTB < 90 min recommended by the guidelines. In this study, ambulances were equipped with ECG teletransmission and were staffed by paramedics. Dieker et al[61] analyzed 581 patients from a region of Holland with transport distance of 77 km. DT was associated with lower time delays and a higher proportion of patients in the recommended time frame of guidelines (82% vs 23%, P < 0.001). In the publication by our group[27], we studied the role of DT in 1194 patients with STEMI who underwent PPCI at our regional STEMI program. From that group, 255 (21%) experienced DT from the field. It must be stressed that our network has its farthest point of reference located 154 km from the PPCI-hospital. Our data showed that DT was as well associated with lower DTB and total ischemic time compared to those referred through emergency department route. And this finding was consistent for both patients form the catchment area of the PPCI-hospital and for that form catchment areas of non-PPCI hospitals. Furthermore, the longer the distance to the PPCI the greater the time saved by this strategy. Our results confirm and expand the previous observations to those regions with a STEMI network involving large transfer distances.
While it is clear that DT reduces temporal delays, it is still more debatable if this strategy is associated with better clinical outcomes. Since the overall ischemic time is diminished a greater myocardial salvage is expected and this should impact prognosis of patients. However, we must take into account that publications of DT are retrospective and observational and the association between DT and clinical events may be biased. Moreover, in the early publications of the topic DT was associated with a negative impact on survival. In the publication of So et al[55] DT group showed significantly higher mortality (13.3% vs 5%, P = 0.001) despite having less delay to reperfusion. But, we should highlight that these figures of mortality are unadjusted and DT patients presented cardiogenic shock more frequently and had higher percentage of intracranial hemorrhage. And even in 2009 a systematic review of studies published to that date with 980 patients concluded that there was still insufficient evidence to confirm that DT improved prognosis[65]. However, this meta-analysis did not include the most recent studies and pooled together trials where fibrinolytic therapy and primary angioplasty were used. These features may explain why this meta-analysis failed to show benefit of DT on prognosis.
However, the most contemporary researches have changed this tendency and consistently pointed to a net clinical benefit with this strategy. In the study by Steg et al[57], avoiding the emergency department was associated with lower early mortality (4.9% vs 8.6%, P = 0.01), being the Emergency service use a factor associated with a worse prognosis (OR = 1.67). At one year there was still benefit in mortality in the direct admission group (11.5% vs 15.6%, P < 0.05). In a post-hoc analysis of the On-Time trial[23] patients in the DT group had a significant improvement in ejection fraction, less ventricular dysfunction [left ventricular ejection fraction (LVEF) < 40%] and lower 30-d mortality (1% vs 3.2%), although this finding was not statistically significant (P = 0.2). However at 1 year, DT was associated with lower mortality (2.1% vs 5.6%, P = 0.04), being direct admission an independent predictor of better clinical outcome (OR = 0.3). Pedersen et al[26] were the first researchers to report an independent clinical benefit of DT. Authors showed a significant reduction in the composite endpoint of death or non-fatal myocardial infarction at 1 year (HR = 0.67). On the other hand, this study present the limitation that the individual figures of the clinical variables were not provided and they found no decrease in both “end points” individually. In the ACTION registry[62] , a registry regarding the use of prehospital ECG, which included patients not undergoing PPCI, a trend towards lower adjusted hospital mortality in prehospital diagnosis group was as well observed (6.7% vs 9.5%, OR = 0.80, P = 0.06). Dieker et al[61] observed a lower mortality in the group of DT (7% vs 13%, P = 0.03). However the mortality reported was unadjusted and DT group were younger, with less diabetes mellitus and lower percentage of previous myocardial infarctions. In a novel study by Le May et al[66] DT strategy was analyzed in 1389 patients. Death at 180 days occurred in 5.0% of patients transferred directly from the field, and in 11.5% of patients transported from the field to a non-PPCI-capable hospital (P < 0.0001). After adjusting for baseline characteristics mortality remained lower among DT group (OR = 0.52, 95%CI: 0.31-0.88, P = 0.01).
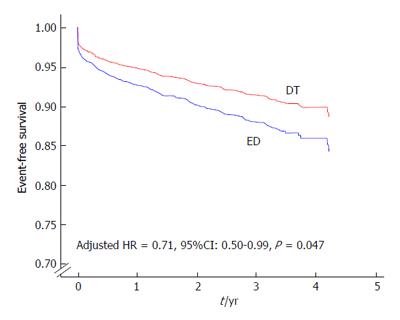
The most exhaustive analysis of the effect of DT on mortality was carried out by our group in two separate reports analyzing short (30-d) and long-term mortality (after a median follow-up of 2.4 years)[27,67]. In the first study, we analyzed the effect of DT on 30-d mortality in 1194 patients. Patients transported directly had lower 30-d mortality (2.7% vs 6.8%, P = 0.017). After adjustment in a multivariable logistic regression analysis, DT remained as an independent predictor for improved outcome (OR = 0.33, 95%CI: 0.12-0.92). Subsequently we reported the effect of DT in a larger cohort and with the longest follow-up in the literature. In a multivariable Cox regression model the DT strategy persisted as an independent variable associated with a better prognosis (HR = 0.71, 95%CI: 0.50-0.99) (Figure 1).
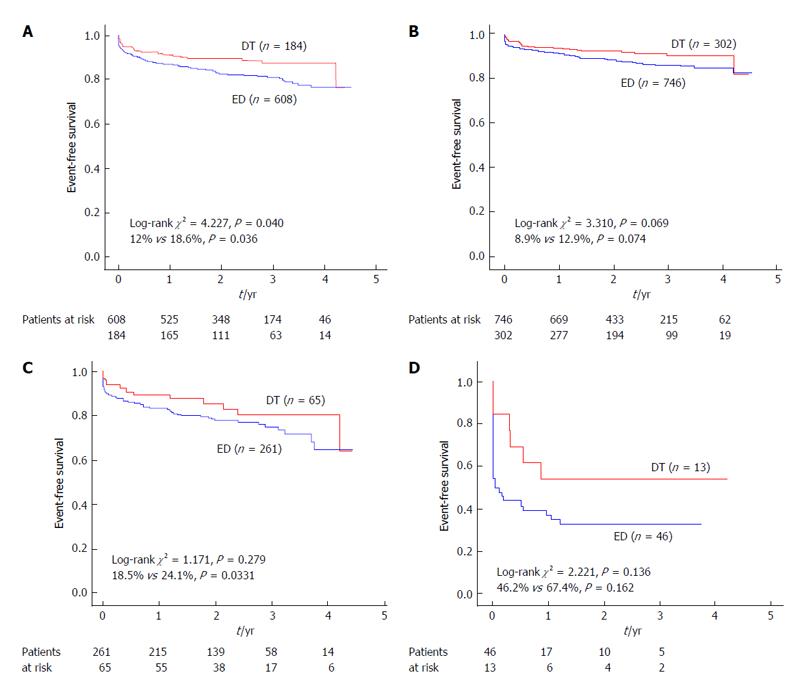
And finally, as we previously stated, the effect of time delays may be related to risk profile of patients. Therefore, the effect of DT on mortality might be influenced as well by some of the baseline characteristics. In this sense, Ortolani found a positive effect on survival of patients with cardiogenic shock who experienced direct transfer[25,59] and our group found a suggested better outcomes in those patients with cardiogenic shock, diabetes mellitus, anterior wall myocardial infarction and those presenting ≤ 2 h from symptom onset (Figure 2)[67]. The evidence of the effect of DT on clinical events is summarized in Table 2.
| n | Short-term mortality | Late mortality | Adjusted mortality | Ref. |
| 401 (DT 59.9) | 13.3% vs 5%, P = 0.001 | - | - | [55] |
| 1204 (DT 66.9) | 4.9% vs 8.6%, P = 0.01 | 11.5% vs 15.6%, P < 0.05 | OR = 1.67 use ED | [57] |
| 467 (DT 44.7) | 1% vs 3.2%, P = NS | 2.1% vs 5.6%, P = 0.04 | OR = 0.3 if DT | [23] |
| 344 (DT 39.2) | 3.7% vs 5.7%, P = 0.3 | 6% vs 7.7%, P = 0.67 | - | [21] |
| 1437 (DT 42.9) | - | - | HR = 0.67 at 1 yr for death/reMI in DT | [26] |
| 7098 (DT 27.4) | 6.7% vs 9.5%, P = NS | - | OR = 0.80, P = NS in DT | [62] |
| 581 (DT 78) | 7% vs 13%, P = 0.03 | - | - | [61] |
| 1389 (DT 59.2) | 3% vs 8.1%, P > 0.001 | 5% vs 11.5%, P < 0.001 | OR = 0.52 at 180 d | [66] |
| 1194 (DT 21) | 2.7% vs 6.8%, P = 0.017 | 9% vs 16%, P = 0.005 | OR = 0.33 at 30 d | [27] |
| 1859 (DT 23) | 3% vs 6%, P = 0.049 | 9.4% vs 14.4%, P = 0.008 at a median 2.4 yr | HR = 0.71 at 2.4 yr | [67] |
There are various reasons that may explain this survival benefit. First, patients have an earlier contact with the system, which provides a higher possibility of being in contact with staff that can deliver cardiac defibrillation and resuscitation if necessary, since it has been estimated that 50% of deaths occur in the prehospital phase[68]. It is pertinent to recall that it has been observed consistently in the literature that the time from onset of symptoms to the contact with medical system is lower in DT group. It is possible that the DT group may represent a lower risk profile than those who come or are derived through emergency departments. They usually are younger, probably with clearer symptoms and possibly with a more definite ECG. This fact was shown previously[69] and it is for this reason that when the effect of DT on mortality is assessed, it must be adjusted by this and other relevant variables. Despite this adjustment, the DT is still significantly associated with lower mortality. Second, it is clear that this strategy consistently reduces time delays and following the aphorism that “time is muscle” it is logical to find a prognostic benefit in these patients. The benefit of reperfusion regarding myocardial salvage is maximal in the first h of STEMI[70] and this strategy allows greater diagnosis and treatment in the early stages, therefore driving to a more preserved LVEF. Moreover, the earlier treatment of patients with STEMI has been linked to a better degree of “myocardial blush”[71] and has also reported to significantly increase the percentage of thrombolysis in myocardial infarction 3 flow after PPCI[61], both facts associated with improvement in LV function and prognosis. A recent publication has challenged the concept that lower DTB times are associated with lower in-hospital mortality[72]. However, the retrospective nature of the study, the exclusion of transferred patients, the short DTB times and follow-up and the unadjustment for time from symptom onset to presentation may have affected the results. Since DT decreases all temporal delays in PPCI and not only DTB, we believe that this fact impacts positively the prognosis of patients. In addition, the prehospital diagnosis allows early initiation of antiplatelet and antithrombotic treatment. Drugs such as aspirin, clopidogrel, heparin and IIb/IIIa inhibitors have been associated with an increased permeability of the infarct related artery preangioplasty[73-76], a fact that has been associated with a better prognosis[77].
This strategy, although in our view of enormous clinical benefit, has several limitations. First, it can only be applied in areas where a well-organized STEMI network is present. Second, despite having shown that the prehospital diagnosis by emergency medical system (EMS) ambulances and subsequent activation of the interventional cardiology team reduces delays, the use of these resources is underutilized. The main reason is probably related to the difficulty of general population awareness to call the EMS when there is a case of chest pain suggestive of myocardial infarction. Third, despite activating the EMS ambulances, not all of them have the capability to perform and transmit an ECG. In the ACTION registry[62] done on more than 12000 patients, only 58.7% of the patients analyzed had contacted the EMS and only 27.4% had a prehospital ECG available. And together with the low frequency of prehospital ECG there is still the problem of its interpretation, raising the possibility of false activations of the cath lab with the consumption of unnecessary resources. In the literature false positive activations of the PPCI team with DT strategy have ranged from 0% to as high as 17%[54]. However, when a STEMI network is well organized the false positive referrals from the EMS ambulances performing DT do not differ from those observed in the PPCI-hospitals and it is not associated with an increase in mortality[78]. And finally, it is remarkable that, despite the benefits demonstrated and that is recommended in practice guidelines[41], this strategy is underutilized in most of angioplasty networks. In a recent study in Canada[79], and more than 15000 paramedics surveyed, only 18% (95%CI: 10%-25%) of EMS operators had protocols allowing the bypass of emergency departments in case of STEMI. We must work to increase the use of a technique that can offer prognostic benefits.
PPCI is the preferred reperfusion strategy in patients experiencing STEMI. On the other hand, it is associated with longer time delays and most of patients do not meet the DTB limit recommended in practice guidelines. DT has emerged as a strategy that has consistently proved to reduce time delays and that is associated with an improved survival. However, it is still underutilized in most STEMI networks, so efforts must be done to increase the percentage of utilization.
P- Reviewers: Dominguez-Rodriguez A, Liu PY, Lee TM S- Editor: Gou SX L- Editor: A E- Editor: Liu SQ
| 1. | Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2931] [Cited by in RCA: 2776] [Article Influence: 126.2] [Reference Citation Analysis (1)] |
| 2. | Widimský P, Groch L, Zelízko M, Aschermann M, Bednár F, Suryapranata H. Multicentre randomized trial comparing transport to primary angioplasty vs immediate thrombolysis vs combined strategy for patients with acute myocardial infarction presenting to a community hospital without a catheterization laboratory. The PRAGUE study. Eur Heart J. 2000;21:823-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 320] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 3. | Andersen HR, Nielsen TT, Rasmussen K, Thuesen L, Kelbaek H, Thayssen P, Abildgaard U, Pedersen F, Madsen JK, Grande P. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349:733-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 915] [Cited by in RCA: 858] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 4. | Widimský P, Budesínský T, Vorác D, Groch L, Zelízko M, Aschermann M, Branny M, St’ásek J, Formánek P. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Final results of the randomized national multicentre trial--PRAGUE-2. Eur Heart J. 2003;24:94-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 525] [Cited by in RCA: 479] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 5. | Grines CL, Westerhausen DR, Grines LL, Hanlon JT, Logemann TL, Niemela M, Weaver WD, Graham M, Boura J, O’Neill WW. A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction: the Air Primary Angioplasty in Myocardial Infarction study. J Am Coll Cardiol. 2002;39:1713-1719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 247] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 6. | Dalby M, Bouzamondo A, Lechat P, Montalescot G. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: a meta-analysis. Circulation. 2003;108:1809-1814. [PubMed] |
| 7. | Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941-2947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 855] [Cited by in RCA: 871] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 8. | McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, Peterson ED, Blaney M, Frederick PD, Krumholz HM. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180-2186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 544] [Cited by in RCA: 599] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 9. | De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223-1225. [PubMed] |
| 10. | Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909-2945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1468] [Cited by in RCA: 1425] [Article Influence: 83.8] [Reference Citation Analysis (0)] |
| 11. | Kushner FG, Hand M, Smith SC, King SB, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205-2241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 958] [Cited by in RCA: 926] [Article Influence: 61.7] [Reference Citation Analysis (0)] |
| 12. | Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation. 2005;111:761-767. [PubMed] |
| 13. | Chakrabarti A, Krumholz HM, Wang Y, Rumsfeld JS, Nallamothu BK. Time-to-reperfusion in patients undergoing interhospital transfer for primary percutaneous coronary intervention in the U.S: an analysis of 2005 and 2006 data from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2008;51:2442-2443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol. 2003;92:824-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 246] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 15. | Betriu A, Masotti M. Comparison of mortality rates in acute myocardial infarction treated by percutaneous coronary intervention versus fibrinolysis. Am J Cardiol. 2005;95:100-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Bradley EH, Roumanis SA, Radford MJ, Webster TR, McNamara RL, Mattera JA, Barton BA, Berg DN, Portnay EL, Moscovitz H. Achieving door-to-balloon times that meet quality guidelines: how do successful hospitals do it? J Am Coll Cardiol. 2005;46:1236-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 136] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Bradley EH, Curry LA, Webster TR, Mattera JA, Roumanis SA, Radford MJ, McNamara RL, Barton BA, Berg DN, Krumholz HM. Achieving rapid door-to-balloon times: how top hospitals improve complex clinical systems. Circulation. 2006;113:1079-1085. [PubMed] |
| 18. | Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355:2308-2320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 600] [Cited by in RCA: 573] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 19. | Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline-Rogers E, Stern AF, Byrd JR, Brush JE. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008;1:97-104. [PubMed] [DOI] [Full Text] |
| 20. | Knot J, Widimsky P, Wijns W, Stenestrand U, Kristensen SD, Van’ T Hof A, Weidinger F, Janzon M, Nörgaard BL, Soerensen JT. How to set up an effective national primary angioplasty network: lessons learned from five European countries. EuroIntervention. 2009;5:299, 301-309. [PubMed] |
| 21. | Le May MR, So DY, Dionne R, Glover CA, Froeschl MP, Wells GA, Davies RF, Sherrard HL, Maloney J, Marquis JF. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2008;358:231-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 306] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 22. | Dorsch MF, Greenwood JP, Priestley C, Somers K, Hague C, Blaxill JM, Wheatcroft SB, Mackintosh AF, McLenachan JM, Blackman DJ. Direct ambulance admission to the cardiac catheterization laboratory significantly reduces door-to-balloon times in primary percutaneous coronary intervention. Am Heart J. 2008;155:1054-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | van ‘t Hof AW, Rasoul S, van de Wetering H, Ernst N, Suryapranata H, Hoorntje JC, Dambrink JH, Gosselink M, Zijlstra F, Ottervanger JP. Feasibility and benefit of prehospital diagnosis, triage, and therapy by paramedics only in patients who are candidates for primary angioplasty for acute myocardial infarction. Am Heart J. 2006;151:1255.e1-1255.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Terkelsen CJ, Lassen JF, Nørgaard BL, Gerdes JC, Poulsen SH, Bendix K, Ankersen JP, Gøtzsche LB, Rømer FK, Nielsen TT. Reduction of treatment delay in patients with ST-elevation myocardial infarction: impact of pre-hospital diagnosis and direct referral to primary percutanous coronary intervention. Eur Heart J. 2005;26:770-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 163] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 25. | Ortolani P, Marzocchi A, Marrozzini C, Palmerini T, Saia F, Serantoni C, Aquilina M, Silenzi S, Baldazzi F, Grosseto D. Clinical impact of direct referral to primary percutaneous coronary intervention following pre-hospital diagnosis of ST-elevation myocardial infarction. Eur Heart J. 2006;27:1550-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Pedersen SH, Galatius S, Hansen PR, Mogelvang R, Abildstrom SZ, Sørensen R, Davidsen U, Galloe A, Abildgaard U, Iversen A. Field triage reduces treatment delay and improves long-term clinical outcome in patients with acute ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. J Am Coll Cardiol. 2009;54:2296-2302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Estévez-Loureiro R, Calviño-Santos R, Vázquez-Rodríguez JM, Marzoa-Rivas R, Barge-Caballero E, Salgado-Fernández J, Aldama-López G, Barreiro-Díaz M, Varela-Portas J, Freire-Tellado M. Direct transfer of ST-elevation myocardial infarction patients for primary percutaneous coronary intervention from short and long transfer distances decreases temporal delays and improves short-term prognosis: the PROGALIAM Registry. EuroIntervention. 2010;6:343-349. [PubMed] |
| 28. | Carstensen S, Nelson GC, Hansen PS, Macken L, Irons S, Flynn M, Kovoor P, Soo Hoo SY, Ward MR, Rasmussen HH. Field triage to primary angioplasty combined with emergency department bypass reduces treatment delays and is associated with improved outcome. Eur Heart J. 2007;28:2313-2319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 29. | Jennings RB, Ganote CE, Reimer KA. Ischemic tissue injury. Am J Pathol. 1975;81:179-198. [PubMed] |
| 30. | Jennings RB, Steenbergen C, Reimer KA. Myocardial ischemia and reperfusion. Monogr Pathol. 1995;37:47-80. [PubMed] |
| 31. | Antman EM. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52:1216-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 32. | Reimer KA, Jennings RB, Tatum AH. Pathobiology of acute myocardial ischemia: metabolic, functional and ultrastructural studies. Am J Cardiol. 1983;52:72A-81A. [PubMed] |
| 33. | Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico (GISSI). Lancet. 1986;1:397-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group. Lancet. 1994;343:311-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1935] [Cited by in RCA: 1630] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 35. | Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 774] [Cited by in RCA: 736] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 36. | Antoniucci D, Valenti R, Migliorini A, Moschi G, Trapani M, Buonamici P, Cerisano G, Bolognese L, Santoro GM. Relation of time to treatment and mortality in patients with acute myocardial infarction undergoing primary coronary angioplasty. Am J Cardiol. 2002;89:1248-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 111] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 37. | Brodie BR, Stuckey TD, Muncy DB, Hansen CJ, Wall TC, Pulsipher M, Gupta N. Importance of time-to-reperfusion in patients with acute myocardial infarction with and without cardiogenic shock treated with primary percutaneous coronary intervention. Am Heart J. 2003;145:708-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 38. | De Luca G, Suryapranata H, Zijlstra F, van ‘t Hof AW, Hoorntje JC, Gosselink AT, Dambrink JH, de Boer MJ. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42:991-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 320] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 39. | Brodie BR, Hansen C, Stuckey TD, Richter S, Versteeg DS, Gupta N, Downey WE, Pulsipher M. Door-to-balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol. 2006;47:289-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 166] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 40. | Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51:210-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 629] [Cited by in RCA: 577] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 41. | Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569-2619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3540] [Cited by in RCA: 3704] [Article Influence: 284.9] [Reference Citation Analysis (0)] |
| 42. | Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763-771. [PubMed] [DOI] [Full Text] |
| 43. | Pinto DS, Kirtane AJ, Nallamothu BK, Murphy SA, Cohen DJ, Laham RJ, Cutlip DE, Bates ER, Frederick PD, Miller DP. Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation. 2006;114:2019-2025. [PubMed] |
| 44. | Pinto DS, Frederick PD, Chakrabarti AK, Kirtane AJ, Ullman E, Dejam A, Miller DP, Henry TD, Gibson CM. Benefit of transferring ST-segment-elevation myocardial infarction patients for percutaneous coronary intervention compared with administration of onsite fibrinolytic declines as delays increase. Circulation. 2011;124:2512-2521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 45. | Tarantini G, Razzolini R, Napodano M, Bilato C, Ramondo A, Iliceto S. Acceptable reperfusion delay to prefer primary angioplasty over fibrin-specific thrombolytic therapy is affected (mainly) by the patient’s mortality risk: 1 h does not fit all. Eur Heart J. 2010;31:676-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 46. | Schömig A, Ndrepepa G, Mehilli J, Schwaiger M, Schühlen H, Nekolla S, Pache J, Martinoff S, Bollwein H, Kastrati A. Therapy-dependent influence of time-to-treatment interval on myocardial salvage in patients with acute myocardial infarction treated with coronary artery stenting or thrombolysis. Circulation. 2003;108:1084-1088. [PubMed] |
| 47. | Zijlstra F, Patel A, Jones M, Grines CL, Ellis S, Garcia E, Grinfeld L, Gibbons RJ, Ribeiro EE, Ribichini F. Clinical characteristics and outcome of patients with early (< 2 h), intermediate (2-4 h) and late (> 4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J. 2002;23:550-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 191] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 48. | Jacobs AK, Antman EM, Ellrodt G, Faxon DP, Gregory T, Mensah GA, Moyer P, Ornato J, Peterson ED, Sadwin L. Recommendation to develop strategies to increase the number of ST-segment-elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation. 2006;113:2152-2163. [PubMed] |
| 49. | Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation. 2007;116:217-230. [PubMed] |
| 50. | Bradley EH, Nallamothu BK, Stern AF, Cherlin EJ, Wang Y, Byrd JR, Linnander EL, Nazem AG, Brush JE, Krumholz HM. The door-to-balloon alliance for quality: who joins national collaborative efforts and why? Jt Comm J Qual Patient Saf. 2009;35:93-99. [PubMed] |
| 51. | Bradley EH, Herrin J, Wang Y, McNamara RL, Radford MJ, Magid DJ, Canto JG, Blaney M, Krumholz HM. Door-to-drug and door-to-balloon times: where can we improve? Time to reperfusion therapy in patients with ST-segment elevation myocardial infarction (STEMI). Am Heart J. 2006;151:1281-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 52. | Bradley EH, Nallamothu BK, Curtis JP, Webster TR, Magid DJ, Granger CB, Moscucci M, Krumholz HM. Summary of evidence regarding hospital strategies to reduce door-to-balloon times for patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Crit Pathw Cardiol. 2007;6:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 53. | McNamara RL, Herrin J, Bradley EH, Portnay EL, Curtis JP, Wang Y, Magid DJ, Blaney M, Krumholz HM. Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J Am Coll Cardiol. 2006;47:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 160] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 54. | Le May MR, Davies RF, Dionne R, Maloney J, Trickett J, So D, Ha A, Sherrard H, Glover C, Marquis JF. Comparison of early mortality of paramedic-diagnosed ST-segment elevation myocardial infarction with immediate transport to a designated primary percutaneous coronary intervention center to that of similar patients transported to the nearest hospital. Am J Cardiol. 2006;98:1329-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 55. | So DY, Ha AC, Turek MA, Maloney JP, Higginson LA, Davies RF, Ryan SC, Le May MR. Comparison of mortality patterns in patients with ST-elevation myocardial infarction arriving by emergency medical services versus self-transport (from the prospective Ottawa Hospital STEMI Registry). Am J Cardiol. 2006;97:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 56. | Gross BW, Dauterman KW, Moran MG, Kotler TS, Schnugg SJ, Rostykus PS, Ross AM, Weaver WD. An approach to shorten time to infarct artery patency in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2007;99:1360-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 57. | Steg PG, Cambou JP, Goldstein P, Durand E, Sauval P, Kadri Z, Blanchard D, Lablanche JM, Guéret P, Cottin Y. Bypassing the emergency room reduces delays and mortality in ST elevation myocardial infarction: the USIC 2000 registry. Heart. 2006;92:1378-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 58. | van de Loo A, Saurbier B, Kalbhenn J, Koberne F, Zehender M. Primary percutaneous coronary intervention in acute myocardial infarction: direct transportation to catheterization laboratory by emergency teams reduces door-to-balloon time. Clin Cardiol. 2006;29:112-116. [PubMed] |
| 59. | Ortolani P, Marzocchi A, Marrozzini C, Palmerini T, Saia F, Baldazzi F, Silenzi S, Taglieri N, Bacchi-Reggiani ML, Gordini G. Usefulness of prehospital triage in patients with cardiogenic shock complicating ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Am J Cardiol. 2007;100:787-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 60. | de Villiers JS, Anderson T, McMeekin JD, Leung RC, Traboulsi M. Expedited transfer for primary percutaneous coronary intervention: a program evaluation. CMAJ. 2007;176:1833-1838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 61. | Dieker HJ, Liem SS, El Aidi H, van Grunsven P, Aengevaeren WR, Brouwer MA, Verheugt FW. Pre-hospital triage for primary angioplasty: direct referral to the intervention center versus interhospital transport. JACC Cardiovasc Interv. 2010;3:705-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 62. | Diercks DB, Kontos MC, Chen AY, Pollack CV, Wiviott SD, Rumsfeld JS, Magid DJ, Gibler WB, Cannon CP, Peterson ED. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol. 2009;53:161-166. [PubMed] [DOI] [Full Text] |
| 63. | Qiu JP, Zhang Q, Lu JD, Wang HR, Lin J, Ge ZR, Zhang RY, Shen WF. Direct ambulance transport to catheterization laboratory reduces door-to-balloon time in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: the DIRECT-STEMI study. Chin Med J (Engl). 2011;124:805-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 64. | Krumholz HM, Anderson JL, Bachelder BL, Fesmire FM, Fihn SD, Foody JM, Ho PM, Kosiborod MN, Masoudi FA, Nallamothu BK. ACC/AHA 2008 performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST-elevation and non-ST-elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine. Circulation. 2008;118:2596-2648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 156] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 65. | Brooks SC, Allan KS, Welsford M, Verbeek PR, Arntz HR, Morrison LJ. Prehospital triage and direct transport of patients with ST-elevation myocardial infarction to primary percutaneous coronary intervention centres: a systematic review and meta-analysis. CJEM. 2009;11:481-492. [PubMed] |
| 66. | Le May MR, Wells GA, So DY, Glover CA, Froeschl M, Maloney J, Dionne R, Marquis JF, O’Brien ER, Dick A. Reduction in mortality as a result of direct transport from the field to a receiving center for primary percutaneous coronary intervention. J Am Coll Cardiol. 2012;60:1223-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 67. | Estévez-Loureiro R, Calviño-Santos R, López-Sainz A, Vázquez-Rodríguez JM, Soler-Martín MR, Prada-Delgado O, Barge-Caballero E, Salgado-Fernández J, Aldama-López G, Piñón-Esteban P. Long-term prognostic benefit of field triage and direct transfer of patients with ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention. Am J Cardiol. 2013;111:1721-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 68. | Dean NC, Haug PJ, Hawker PJ. Effect of mobile paramedic units on outcome in patients with myocardial infarction. Ann Emerg Med. 1988;17:1034-1041. [PubMed] |
| 69. | Canto JG, Zalenski RJ, Ornato JP, Rogers WJ, Kiefe CI, Magid D, Shlipak MG, Frederick PD, Lambrew CG, Littrell KA. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106:3018-3023. [PubMed] |
| 70. | Gersh BJ, Stone GW, White HD, Holmes DR. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA. 2005;293:979-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 298] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 71. | De Luca G, van ‘t Hof AW, de Boer MJ, Ottervanger JP, Hoorntje JC, Gosselink AT, Dambrink JH, Zijlstra F, Suryapranata H. Time-to-treatment significantly affects the extent of ST-segment resolution and myocardial blush in patients with acute myocardial infarction treated by primary angioplasty. Eur Heart J. 2004;25:1009-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 164] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 72. | Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 503] [Cited by in RCA: 555] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 73. | Zijlstra F, Ernst N, de Boer MJ, Nibbering E, Suryapranata H, Hoorntje JC, Dambrink JH, van ‘t Hof AW, Verheugt FW. Influence of prehospital administration of aspirin and heparin on initial patency of the infarct-related artery in patients with acute ST elevation myocardial infarction. J Am Coll Cardiol. 2002;39:1733-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 74. | Montalescot G, Borentain M, Payot L, Collet JP, Thomas D. Early vs late administration of glycoprotein IIb/IIIa inhibitors in primary percutaneous coronary intervention of acute ST-segment elevation myocardial infarction: a meta-analysis. JAMA. 2004;292:362-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 183] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 75. | Vlaar PJ, Svilaas T, Damman K, de Smet BJ, Tijssen JG, Hillege HL, Zijlstra F. Impact of pretreatment with clopidogrel on initial patency and outcome in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review. Circulation. 2008;118:1828-1836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 76. | De Luca G, Gibson CM, Bellandi F, Murphy S, Maioli M, Noc M, Zeymer U, Dudek D, Arntz HR, Zorman S. Early glycoprotein IIb-IIIa inhibitors in primary angioplasty (EGYPT) cooperation: an individual patient data meta-analysis. Heart. 2008;94:1548-1558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 77. | Stone GW, Cox D, Garcia E, Brodie BR, Morice MC, Griffin J, Mattos L, Lansky AJ, O’Neill WW, Grines CL. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation. 2001;104:636-641. [PubMed] |
| 78. | Barge-Caballero E, Vázquez-Rodríguez JM, Estévez-Loureiro R, Barge-Caballero G, Rodríguez-Vilela A, Calviño-Santos R, Salgado-Fernández J, Aldama-López G, Piñón-Esteban P, Campo-Pérez R. Prevalence, etiology and outcome of catheterization laboratory false alarms in patients with suspected ST-elevation myocardial infarction. Rev Esp Cardiol. 2010;63:518-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |