Published online Oct 26, 2014. doi: 10.4330/wjc.v6.i10.1131
Revised: July 12, 2014
Accepted: August 27, 2014
Published online: October 26, 2014
Processing time: 157 Days and 4.7 Hours
Kounis syndrome seems to be not a rare disease but a rarely diagnosed disorder. Multiple causes can join forces and trigger the development of this syndrome. We report the first case of Kounis syndrome manifesting as myocardial infarction with cardiovascular collapse that occurred in the dialysis room following an allergic reaction. The dialysis apparatus material of polyurethane, polyamide, polycarbonate, silicon rubber and polypropylene were incriminated causes. Physicians should be aware of the causality and existence of this disorder in order to achieve early and correct diagnosis and apply the appropriate therapeutic measures.
Core tip: This is the first report of Kounis syndrome occurring in the dialysis room in a patient using a new dialysis machine. The apparatus components acting as allergens are incriminated since subsequent hemodialysis sessions with the apparatus used before the anaphylactic reaction were without any sequelae. Materials such as polyurethane, polyamide, polycarbonate, silicon rubber and polypropylene acting as allergens might prove risky in sensitive patients during hemodialysis. Atopic patients should be always interrogated about allergies and patch testing concerning the apparatus components should be performed in such patients.
- Citation: Mazarakis A, Bardousis K, Almpanis G, Mazaraki I, Ouzounis A, Kounis NG. Anaphylactic cardiovascular collapse during hemodialysis: Kounis syndrome in the dialysis room. World J Cardiol 2014; 6(10): 1131-1134
- URL: https://www.wjgnet.com/1949-8462/full/v6/i10/1131.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i10.1131
Kounis syndrome is hypersensitivity-associated acute coronary syndrome manifesting as acute myocardial infarction, coronary spasm or even stent thrombosis[1]. It is caused by numerous drugs, materials, metals, environmental exposures and conditions associated with mast cell activation. During mast cell activation the released mediators can induce either coronary artery spasm which can progress to acute myocardial infarction or atheromatous plaque erosion or rupture culminating to coronary thrombosis. Kounis syndrome is ubiquitous disease affecting patients of any age, from 2-year-old to octagenarians, involving numerous and continuously increasing causes, with broadening clinical manifestations[2,3]. The following report concerns of a patient who developed this syndrome during hemodialysis. To our knowledge this is the first case of Kounis syndrome occurring in the dialysis room.
A 75-year-old diabetic, hypertensive man having history of coronary artery disease with acute myocardial infarction 12 years ago and stent implantation in the left anterior descending coronary artery and undergoing hemodialysis thrice a week for the last 3 years due to diabetic chronic kidney disease, was transferred to the emergency department after an episode of loss of consciousness accompanied by chest discomfort during dialysis.
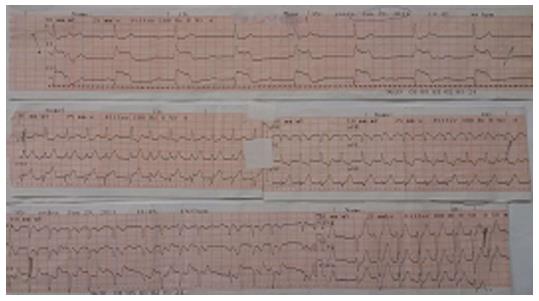
He was asymptomatic until he had been connected to the hemodialysis machine in the renal unit for his routine dialysis session. The staff of the unit confirmed changing of the hemodialysis apparatus before the current session with an older brand due to unavailability of the previously used machine. The new apparatus consisted of polyamix membrane, potting material made from polyurethane, housing caps made from polycarbonate, protective plugs made from polypropylene and o-ring made from silicon. Five minutes following the connection with the new dialysis apparatus the patient developed an erythematous rash that covered his trunk and complained of feeling “burning” in his face, chest pain, dyspnea, palpitations and suddenly lost consciousness. Α severe anaphylactic reaction associated with Kounis syndrome probably due to the new dialyzer- was suspected and immediate cardiopulmonary resuscitation was started with chest compressions, antihistamines, hydrocortisone intravenously and adrenaline intramuscular doses of 0.2-0.5 mg (1:1000). His blood pressure was 60/40 mmHg and the electrocardiogram revealed complete heart block with cardiac rate of 40 beats per minute and 5-7mm ST elevation in leads II and III, AVF. Within 3 min the patient was alerted but confused. His blood pressure was raised to 85/60 mmHg, electrocardiogram revealed atrial fibrillation with rapid ventricular response 135 beat per minute and ST elevation 1-2 mm in leads II, III and aVF and ST depression 1 mm in leads I, aVL, V1-V3 (Figure 1). He was then transferred to our coronary care unit for further treatment and evaluation.
Upon arrival to the unit the patient was alert, complaining of mild retrosternal chest pain and Killip class II dyspnea. His blood pressure was 90/50 mmHg, the heart rate was 120 bpm regular and his temperature was 36.0 C. The oxygen saturation, while breathing in the room air was 93%, the electrocardiogram revealed sinus tachycardia with 122 bpm and minimal 0.5-1 mm ST elevation in leads II, III and aVF and 1mm horizontal-downsloping ST depression in leads I, aVL, V1-V6.
Treatment started with 300 mg clopidogrel and 4000IU of low molecular weight heparin. He was not aspirin naïve because of his previous myocardial infarction, so no oral loading dose of aspirin was administered. Peak high sensitivity troponin I levels were 0.350 ng/mL, eosinophils 8%, IgEs were elevated to 170 IU/mL (normal levels < 110 IU/mL) but specific IgEs for the dialysis apparatus were not detected. Transthoracic echocardiographic study showed hypokinesis of basal and mid portions of the infero-posterior wall of the left ventricle with an estimated ejection fraction of 50%. Skin prick tests were not performed on ethical grounds.
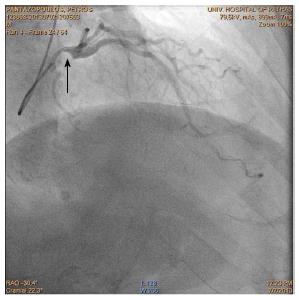
The patient remained hemodynamically and electrically stable, asymptomatic and afebrile. Coronary angiography revealed severe stenosis of the left main artery and 70% stenosis of the first segment of right coronary artery and patent previous stent (Figure 2). The patient underwent successful coronary artery bypass surgery. Subsequent hemodialysis sessions with the apparatus used before the anaphylactic reaction were re-started and were without any sequelae.
The described patient developed severe anaphylaxis associated with myocardial infarction and cardiovascular collapse in the hemodialysis room soon after changing the dialysis apparatus. He was found to have increased IgEs and eosinophil count suggesting hypersensitivity reaction and was diagnosed as type II variant of Kounis syndrome. All 4 components of the used apparatus namely polyamix membrane, potting material made from polyurethane, housing caps made from polycarbonate, protective plugs made from polypropylene and o-ring made from silicon rubber have been incriminated to induce hypersensitivity reactions. Polyamix membrane is made from a polymer blend of polyarylethersulfone, polyvinylpyrrolidone and polyamide all of which are sensitizers[4]. Polyurethane chemicals are produced by the reaction of isocyanates and they may cause allergic contact dermatitis or precipitate asthma attacks[5]. Polycarbonate can induced allergic reactions especially in dental procedures[6]. Polypropylene is able to induce irritant contact dermatitis[7] and silicon rubber has induced hypersensitivity reactions known as “latex-fruit syndrome”[8]. These materials have been incriminated to induce hypersensitivity reactions by activating high and low affinity IgE receptors known as FCγRI, FCγRII, FCεRI and FCεRII receptors situated on both mast cell and platelet surface[9].
Therefore the described patient was exposed to 5 antigens. Indeed, clinical studies indicate that sensitive patients simultaneously exposed to several allergens can have more symptoms than mono-sensitized individuals[10]. This could be an explanation for the patient’s immediate cardiovascular collapse. On the other hand, immunoglobulin E (IgE) antibodies with different specificities can have additive effects and small, even subthreshold numbers of them can join forces and trigger the cells to release their mediators. This can occur when the patient is simultaneously exposed to the corresponding antigens[11]. The initiation of allergic inflammation takes place when allergens cross-bridge their corresponding, receptor bound, IgE antibodies on the mast cell or basophil cell surface. These cells degranulate and release their mediators when the critical number of bridged IgE antibodies reaches the order of 2000 out of maximal number of some 500000-1000000 IgE antibodies on the cell surface[12]. A total of approximately 1000 bridges are necessary to induced mast cell degranulation.
Kounis syndrome seems to be not a rare disease but a rarely diagnosed disorder. Multiple and combined causes can trigger the development of this syndrome. Physicians should be aware of its pathophysiology and existence in order to apply predictive, preventive, diagnostic and appropriate therapeutic measures.
A 75-year-old diabetic, hypertensive man suffering from coronary artery disease and renal failure developed anaphylactic cardiac collapse soon after been connected with the dialysis apparatus.
The appearance of erythematous rash that covered his trunk together with feeling “burning” in his face, chest pain, dyspnea, palpitations, sudden loss of consciousness, electrocardiophic changes, increased cardiac enzymes, increased eosinophils and IgEs were suggestive of type II variant of hypersensitivity-associated Kounis syndrome.
The differential diagnosis included anaphylactic shock and acute myocardial infarction but their combination is classical with Kounis acute associated with hypersensitity coronary syndrome.
Serial electrocardiographic changes of complete heart block, atrial fibrillation, ST segment elevation, increased cardiac enzymes and troponin I, increased eosinophils, increased IgEs and hypokinetic basal and mid portions of the infero-posterior wall of the left ventricle were observed.
Coronary angiography revealed severe stenosis of the left main artery and 70% stenosis of the first segment of right coronary artery but patent previous stent that had been implanted in the left anterior descending artery 12 years previously.
Neither pathological examination nor skin biopsy for the erythematous rash was thought necessary to be performed.
The patient was treated initially with chest compressions, antihistamines, hydrocortisone intravenously and adrenaline intramuscular doses followed by clopidogrel and of low molecular weight heparin and finally underwent successful coronary artery bypass surgery. Subsequent hemodialysis sessions with the apparatus used before the anaphylactic reaction were re-started and were without any sequelae.
No related reports are available and this case of Kounis syndrome is the first in the world literature.
This case of Kounis type II variant syndrome is characterized as unique.
Kounis syndrome is not a rare disease but a rarely diagnosed disorder caused by multiple and combined causes. Therefore physicians should be aware of its pathophysiology and existence in order to apply predictive, preventive, diagnostic and appropriate therapeutic measures.
This is a very interesting report of the case of Kounis syndrome occuring in the dialysis room.
P- Reviewer: Kounis GN, Xiong XJ S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Kounis NG. Coronary hypersensitivity disorder: the Kounis syndrome. Clin Ther. 2013;35:563-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 221] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 2. | Parent B, Wearden P, Kounis NG, Chrysostomou C. Kounis syndrome or allergic coronary vasospasm in a two-year-old. Congenit Heart Dis. 2011;6:499-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Biteker M, Duran NE, Biteker FS, Civan HA, Kaya H, Gökdeniz T, Yildiz M, Ozkan M. Allergic myocardial infarction in childhood: Kounis syndrome. Eur J Pediatr. 2010;169:27-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Situm M, Lugović-Mihić L, Bulat V, Peternel R, Vojniković B, Martinis M, Toth I. Dermatological aspects of contact dermatitis from eyeglass frames and optical materials. Coll Antropol. 2013;37 Suppl 1:19-24. [PubMed] |
| 5. | Turan H, Saricaoğlu H, Turan A, Tunali S. Polyurethane toilet seat contact dermatitis. Pediatr Dermatol. 2011;28:731-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Tanoue N, Nagano K, Matsumura H. Use of a light-polymerized composite removable partial denture base for a patient hypersensitive to poly(methyl methacrylate), polysulfone, and polycarbonate: a clinical report. J Prosthet Dent. 2005;93:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Patiwael JA, Wintzen M, Rustemeyer T, Bruynzeel DP. Airborne irritant contact dermatitis due to synthetic fibres from an air-conditioning filter. Contact Dermatitis. 2005;52:126-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Ricci G, Piccinno V, Calamelli E, Giannetti A, Pession A. Latex-fruit syndrome in Italian children and adolescents with natural rubber latex allergy. Int J Immunopathol Pharmacol. 2013;26:263-268. [PubMed] |
| 9. | Kounis NG, Mazarakis A, Tsigkas G, Giannopoulos S, Goudevenos J. Kounis syndrome: a new twist on an old disease. Future Cardiol. 2011;7:805-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 146] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 10. | MacGlashan DW, Bochner BS, Adelman DC, Jardieu PM, Togias A, McKenzie-White J, Sterbinsky SA, Hamilton RG, Lichtenstein LM. Down-regulation of Fc(epsilon)RI expression on human basophils during in vivo treatment of atopic patients with anti-IgE antibody. J Immunol. 1997;158:1438-1445. [PubMed] |
| 11. | Nopp A, Johansson SG, Lundberg M, Oman H. Simultaneous exposure of several allergens has an additive effect on multisensitized basophils. Allergy. 2006;61:1366-1368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Wickman M. When allergies complicate allergies. Allergy. 2005;60 Suppl 79:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |