Revised: September 11, 2013
Accepted: December 12, 2013
Published online: January 26, 2014
Processing time: 207 Days and 16.5 Hours
AIM: To investigate the impact of primary reperfusion therapy (RT) on early and late mortality in acute right ventricular infarction (RVI).
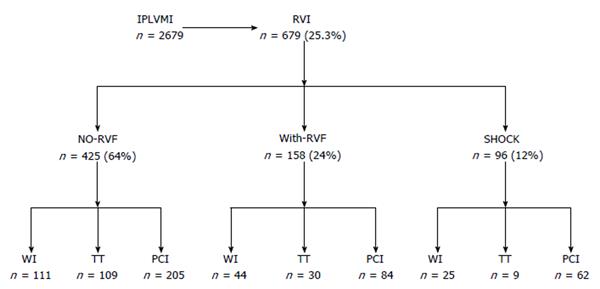
METHODS: RVI patients (n = 679) were prospectively classified as without right ventricular failure (RVF) (class A, n = 425, 64%), with RVF (class B, n = 158, 24%) or with cardiogenic shock (CS) (class C, n = 96, 12%). Of the 679 patients, 148 (21.7%) were considered to be eligible for thrombolytic therapy (TT) and 351 (51.6%) for primary percutaneous coronary intervention (PPCI). TIMI 3-flow by TT was achieved for A, B and C RVI class in 65%, 64% and 0%, respectively and with PPCI in 93%, 91% and 87%, respectively.
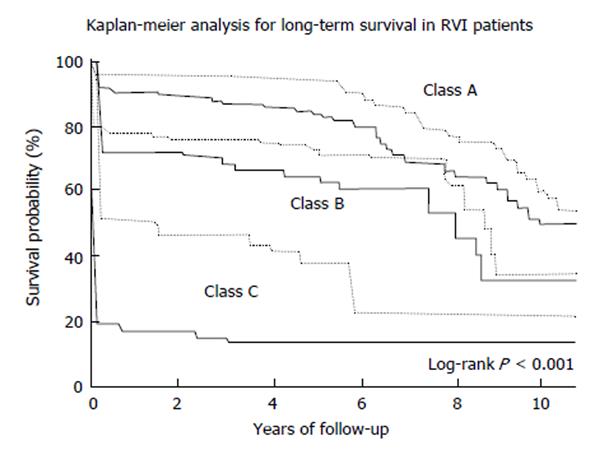
RESULTS: For class A without RT, the mortality rate was 7.9%, with TT was reduced to 4.4% (P < 0.01) and with PPCI to 3.2% (P < 0.01). Considering TT vs PPCI, PPCI was superior (P < 0.05). For class B without RT the mortality was 27%, decreased to 13% with TT (P < 0.01) and to 8.3% with PPCI (P < 0.01). In a TT and PPCI comparison, PPCI was superior (P < 0.01). For class C without RT the in-hospital mortality was 80%, with TT was 100% and with PPCI, the rate decreased to 44% (P < 0.01). At 8 years, the mortality rate without RT for class A was 32%, for class B was 48% and for class C was 85%. When PPCI was successful, the long-term mortality was lower than previously reported for the 3 RVI classes (A: 21%, B: 38%, C: 70%; P < 0.001).
CONCLUSION: PPCI is superior to TT and reduces short/long-term mortality for all RVI categories. RVI CS patients should be encouraged to undergo PPCI at a specialized center.
Core tip: It is, up to our knowledge the largest series of acute right ventricular infarction (RVI) patients where all the clinical RVI spectrum is considered. RVI is analyzed in relation to primary reperfusion procedures, over a study period with a more widespread use of primary percutaneous coronary intervention (PPCI) together with the advent of stents and antiplatelet agents to provide a better insight into reperfusion trends and results in acute RVI. According to our findings, in all RVI hemodynamic scenario PPCI is superior to thrombolytic therapy (TT) and reduces short and long-term mortality for all 3 RVI categories. Patients in cardiogenic shock should be encouraged to undergo PPCI rather than TT at a specialized center.
- Citation: Lupi-Herrera E, González-Pacheco H, Juárez-Herrera &, Espinola-Zavaleta N, Chuquiure-Valenzuela E, Villavicencio-Fernández R, Peña-Duque MA, Ban-Hayashi E, Férez-Santander S. Primary reperfusion in acute right ventricular infarction: An observational study. World J Cardiol 2014; 6(1): 14-22
- URL: https://www.wjgnet.com/1949-8462/full/v6/i1/14.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i1.14
Right ventricular infarction (RVI) is relatively common in patients with acute inferior-posterior left ventricular myocardial infarction (IPLVMI). RVI can depress right ventricular (RV) function, resulting in right ventricular failure (RVF) or cardiogenic shock (CS)[1-5]. There are scarce and somewhat conflicting clinical data concerning the effects of interventions designed to achieve reperfusion of the RV myocardium in acute ischemia. Several investigators have suggested that RV function improves only after successful thrombolytic therapy (TT), whereas others have reported recovery in the absence of early or even any reperfusion of the right coronary artery (RCA)[6]. In a study involving limited number of patients, rapid hemodynamic improvement and excellent clinical outcomes have been reported after successful primary percutaneous coronary intervention (PPCI) of the RCA and its major RV branches[1]. At the most extreme end of the hemodynamic spectrum for RVI, when CS is analyzed in relation to reperfusion, the results can be disappointing, partly due to the time frame of the study (1993-1998), or the results can be better than the outcomes in patients with left ventricular (LV) pump failure in a study from 1984 to 2004[7]. The present study aimed (1) to evaluate the trends and impact of TT and PPCI over time and on early and late mortality in RVI patients with or without RVF; and (2) with CS over a study period with a more widespread use of PPCI together with the advent of stents and potent antiplatelet agents to provide a better insight into reperfusion results in acute RVI.
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. The protocol was approved by the ethics committee of the institution. All patients provided informed written consent.
We prospectively screened 2679 consecutive patients admitted with a first acute (defined as the time from symptom onset to admission of ≤ 48 h) IPLVMI (defined as chest pain with > 1 mm in leads II, III and aVF) from January 1996 to March 2009, and identified 679 (25.3%) patients with infarction extending to the walls of the right ventricle (84% were studied in the last 10 years). Isolated acute RVI, history of valve heart disease, and previous heart or renal failure were exclusion criteria for this study.
The diagnostic criteria for IPLVMI with extension to the walls of the right ventricle, RVF and CS have been published previously[4]. Briefly, in addition to standard electrocardiographic (EKG) leads, a right-sided precordial EKG (leads V3R-V7R) was recorded in all patients immediately after admission. An ST-segment elevation in lead V3R or V4R of greater than 0.1 mV was used to diagnose RVI. The diagnosis of RVI was also based on clinical features that have been described and have been associated with this variety of infarction, and on echocardiographic findings[2]. The diagnosis of RVF was based on clinical features, including persistent systemic hypotension [systemic systolic pressure (SSP) ≤ 100 mmHg, right-sided S3 and S4] without features of shock, echocardiographic evidence of ischemic RVF (RV wall motion abnormalities (WMA) associated with gross RV dilatation), findings that suggest globally depressed RV function and invasive hemodynamic monitoring identifying RVI by a combination of findings that suggest RV dysfunction [low cardiac output (CO) and a disproportionate elevation of the mean right atrial pressure (mRAP) compared to the mean pulmonary wedge pressure (mPWP)][2,8,9]. The diagnosis for shock was made if all of the following criteria were satisfied: SSP persistently ≤ 90 mmHg or vasopressors required to maintain SSP > 90 mmHg; very low CO [cardiac index (CI) < 2.1 L.min/m2]; evidence of end-organ hypoperfusion. We did not include in this category patients with hypotension related to hypovolemia, transient hypotension due to vasodilatation and bradycardia associated with spontaneous reperfusion (Bezold-Jarisch reflex), or hypotension due to atrioventricular block (AVB), cardiac arrhythmias or mechanical complications (ventricular septal or myocardial wall rupture or cardiac tamponade) at admission.
We risk-stratified RVI patients into 3 subsets based on clinical features, echocardiographic findings upon admission and hemodynamic findings as follows: class A (without RVF), comprised of patients without evidence of systemic hypotension (SSP ≥ 100 mmHg) or RVF (by clinical features, echocardiographic and/or hemodynamic findings); class B (with RVF), those with persistent systemic hypotension (SSP < 100 mmHg) or RVF, but without other clinical features of shock; class C, those with CS (Figure 1).
Echocardiograms were analyzed according to previous methods[4]. LV systolic dysfunction was defined as an ejection fraction below 50%. The RV was divided into eight segments; of these segments 3 corresponded to the basal segments, 3 to the middle segments of the anterior, lateral and inferior walls (IWs), and 2 to the apical anterior and inferior segments. The wall movement index (WMI) of both ventricles was obtained by assigning a value to the movement of each wall segments and dividing the sum by the number of segments corresponding to the ventricle in question. A score of 0 was classified to normal movement, 1 as = hypokinesis (diminished thickening), 2 as = akinesis (absence of thickening) and 3 as = dyskinesis (paradoxical systolic movement). The overall score for RV and LV wall motion (LVWM) was calculated as the average score for the segments, and the ratio of the diastolic diameters of the two ventricles diastolic ratio of the two ventricles (RVD/LVD) was also calculated. The echocardiographic evidence of ischemic RV was based on a combination of the following features: right ventricular wall motion abnormalities (RVWMA) and RV dilatation with/without tricuspid regurgitation (TR). Right atrial (RA) ischemia was defined according to the following criteria: akinesis of the RA free wall (FW) despite left atrial contraction, thrombosis at the site of akinesis, presence of spontaneous contrast in the RA, and inversion of the interatrial septal convexity[4].
The location of the culprit lesion was assessed using Bowers criteria[1]. The initial and post-reperfusion flow grades in the coronary artery and in the RV branches were scored from 0 to 3 [thrombolysis in myocardial infarction (TIMI) flow classification]. Successful reperfusion was defined as < 50% residual stenosis and restoration of TIMI grade 3 in the main RCA and its major RV branches (> 1 mm). Coronary collateral blood flow was evaluated according to Rentrop et al[10]. Multivessel disease was defined as a lesion ≥ 50% in ≥ 2 major coronary arteries. We analyzed all of the patients who had a coronary angiogram at admission and a second angiogram after reperfusion. For those who received TT, the second coronary angiogram was performed 90-180 min after the thrombolytic infusion. Information on the coronary arteries was evaluated independent of and blinded to the other study data.
Patients were treated with unfractionated heparin (bolus: 60 IU/kg, maximum 5000 IU; 10 IU/kg per hour, maximum 1000/h) and aspirin (300 mg) in the emergency room and transferred to the coronary care unit or to the catheterization laboratory to undergo coronary angiography, based on the individual’s. Patients who were eligible for reperfusion were consecutively assigned to TT or PPCI. TT was administered intravenously to all of the eligible RVI patients. The inclusion criteria for classes A and B were defined before admission as follows: symptoms of ST elevation myocardial infarction (STEMI) lasting less than 12 h or > 12 h in patients with ongoing ischemia, age ≤ 75 years and absence of other accepted contraindications. TT was performed with either streptokinase (32%) or recombinant tissue plasminogen activator (68%), preceded by heparin. Post-TT consisted of an intravenous heparin dose that was adjusted to maintain TPTa between 60-75 s for 72 h and aspirin. For PPCI, the same inclusion criteria for STEMI symptoms and duration and age were applied; stents were deployed according to standard techniques followed by standard anti-platelet therapy. Stents and glycoprotein IIb/IIIa platelet inhibitors became a standard therapy in eligible patients in 1995 and 1996, respectively. Clopidogrel was used in stented patients with a loading dose of 300 mg or 600 mg and later, a daily dose of 75 mg for ≥ 6 mo in patients treated with bare metal stents and for 6 to 12 mo in patients treated with drug-eluting stents. RVI patients in shock were considered to be candidates for PPCI if age < 75 years and shock developed within ≤ 48 h of the STEMI.
Conservative therapy for A and B class was provided to patients who delayed seeking medical attention, for class C > 75 years of age or those who developed shock > 48 h after the onset of myocardial infarction. Patients underwent PPCI or coronary artery bypass graft surgery (CABGS) only if ischemia recurred despite medical therapy during hospitalization or occurred during a pre-discharge stress test.
The following adverse cardiac events were recorded: hypotension (> 1 h), hypotension necessitating volume infusion (200-400 mL/h), pharmacological hemodynamic support (inotropic agents/vasopressors), or intra-aortic balloon pump (IABP); high grade AVB (> 1 h, need for a transient pacemaker); ventricular arrhythmias requiring treatment; recurrent ischemia (defined as recurrent chest pain with or without new EKG changes or recurrent myonecrosis as indicated by serum biomarkers (increase in creatine kinase level and MB fraction higher than the nadir); death. Urgent target vessel revascularization was defined as the need to repeat PPCI or urgent CABGS for recurrent ischemia or hemodynamic compromise during the hospital stay.
The primary end point was in-hospital cardiac death at 30 d. Follow-up information after hospital discharge was obtained from the hospital records database, which is updated at each patient visit and upon patient death.
We analyzed: (1) the clinical, echocardiographic, angiographic and hemodynamic characteristics of our patients at baseline separately for those in classes A, B, and C; (2) among the 3 RVI classes; (3) within each class, all patients sent for reperfusion were compared to those who were not referred for reperfusion; and (4) within each class, TT vs PPCI was compared.
The continuous data are expressed as the mean ± SD unless otherwise specified. A Student’s t test, 1-way-ANOVA (Bonferroni’s-test for multiple comparisons), χ2, or Fisher exact test was used as appropriate.
Univariate analysis based on the logistic regression model was used to examine the relationship between the selected demographic, medical history, clinical examination, and hemodynamic data to determine the likelihood of overall mortality. After the univariate analysis, any variable that had a univariate test value of P < 0.25 was considered to be a candidate for the multivariate analyses. The results are expressed as odds ratios and 95%CI. The Kaplan-Meier method was used to estimate the overall survival distribution (log-rank test). The analyses were performed using the STATA-9 software.
From all of the RVI patients, echocardiography, invasive hemodynamic evaluation and coronary angiograms were performed in 94.5%, 89% and 73%, respectively. The diagnosis of RVI was made by EKG, echocardiographic, hemodynamic or coronary angiographic criteria in 100% and by 3 criteria (echocardiographic, hemodynamic and angiographic) in 85% of the patients. The RVI subgroups had no differences in their baseline clinical characteristics (Table 1).
| Variables | Class A | Class B | Class C |
| n = 425 | n = 158 | n = 96 | |
| (64%) | (24%) | (12%) | |
| Age (yr) | 59.7 ± 9.4 | 61 ± 10 | 62.4 ± 8.4 |
| Age 64-74 yr | 41.9% | 38.7% | 37.5% |
| Men | 82% | 81% | 83% |
| Pre-IA | 38% | 40% | 41% |
| Peak CK IU/L median (25th-75th percentiles) | 1854 (1654-2490) | 1994 (1214-2634) | 2109 (1532-2812) |
| Peak MB fraction IU/L median (25th-75th percentiles) | 188 (111-350) | 201 (126-312) | 192 (104-333) |
| Diabetes | 26.9% | 27.8% | 30.6% |
| Hypertension | 40.7% | 44.3% | 44.4% |
| Hypercholesterolemia | 23% | 19% | 21% |
| Smoking | 58% | 60% | 55% |
| BMI (kg/m2) | 28.2 ± 4.4 | 26.7 ± 5.2 | 27.2 ± 3.9 |
At baseline, there was evidence of IPLVMI dysfunction in all of the RVI patients (WMI 1.8 ± 0.4). The echocardiographic data at baseline by clinical class was documented as follows. In all of the classes A patients without RV-dilatation, WMA were only found in the IW (LV + RV) = 84% and the FW = 16%. In class B and C patients with RV-dilatation, WMA was not only confined to the IW; TR, and abnormal ventricular septal movement were observed in 78% and 70%, respectively, with abnormal RA wall movement in 18% and 25%, respectively. Abnormal values for the right ventricular motion index were found in all of the patients, with a significant increase in the WMA score classes between A, B and C classes (P < 0.01, respectively). An RVD/LVD of = 1 was most frequently observed in class B, and an RVD/LVD > 1 was observed in C patients (Table 2).
| Variable | Class A | Class B | Class C | Total |
| (n = 396) | (n = 152) | (n = 94) | (n = 642) | |
| RV-dilatation | 0% | 100%b | 100% | 38.3% |
| VWMA | 100% | 100% | 100% | 100% |
| WMA only for IW | 84% | 0% | 0% | 51.7% |
| WMA for IW + OW | 16% | 100%b | 100% | 48% |
| TR | 17% | 100%b | 100% | 48% |
| AVSM | 25% | 78%b | 70% | 43.9% |
| RVMI | 1.9% ± 0.3% | 2.5% ± 0.2%b | 3.4% ± 0.5%d | 2.4% ± 4% |
| RVD/LVD > 1 | 0% | 25%b | 83%d | 18% |
| RVD/LVD = 1 | 0% | 65%b | 17%d | 18% |
| ARAWM | 0% | 18%b | 25% | 8% |
| RA-DPS n (%) | 0 (0) | 19 (70) | 10 (43)d | 29 (58) |
| LVEF < 0.5 | 11% | 22% | 34%d | 16% |
The hemodynamic data according to the RVI class (n = 604, 89%) was documented as follows. In class A patients (n = 350), all of the hemodynamic parameters were within normal limits. In class B patients (n = 158), an elevated mRAP (12.9 ± 3.6 mmHg) and decreased CI (2.4 ± 0.21 L.min/m2) and mean systemic arterial pressure [mSAP (78.7 ± 12.3 mmHg)] were found, with an increased RAP/PWP > 0.8 compared to class A patients.
For class C patients (n = 96), an elevated mRAP (21.4 ± 5.15 mmHg), systolic pulmonary artery pressure [sPAP (36.8 ± 9.3 mmHg)], diastolic PAP (22.2 ± 3.9 mmHg) and mPWP (19.9 ± 9.2 mmHg) and decreased CI (1.67 ± 0.5 L.min/m2) and mSAP (62.7 ± 9.5 mmHg) were found compared to class B patients (Table 3).
| Variable | Class A | Class B | Class C |
| (n = 350) | (n = 158) | (n = 96) | |
| mRAP (mmHg) | 4.6 ± 2.1 | 12.9 ± 3.6b | 21.4 ± 5.15d |
| REVDP (mmHg) | 3.4 ± 1.7 | 11.2 ± 4b | 16 ± 5.4d |
| sPAP (mmHg) | 16.2 ± 4.4 | 16.4 ± 3.9 | 36.8 ± 9.3d |
| dPAP (mmHg) | 9.7 ± 3.7 | 13.4 ± 2.2 | 22.2 ± 3.9d |
| mPWP (mmHg) | 8.6 ± 3.1 | 12.1 ± 1.8 | 19.9 ± 6.2d |
| CI (L.min/m2) | 3.4 ± 0.71 | 2.4 ± 0.21b | 1.67 ± 0.5d |
| mSAP (mmHg) | 108.8 ± 7 | 78.7 ± 12.3b | 62.7 ± 9.5d |
| RAP/PWP ≥ 0.8 | 2% | 96%b | 92% |
The RCA was the infarct-related artery in 95% of the RVI patients. There was severe compromise of RV perfusion, as indicated by the TIMI grade flow (0.7 ± 1).
The culprit RCA lesion was most commonly found proximal in class B and C patient and had a mid location in class A patients. The 3 RVI subgroups had no differences in prevalence of 1 and 2 vessels disease (VD), but 3-VD was more frequently observed in classes B and C. The combination of RCA and significant left anterior descending (LAD > 50% stenosis) disease was most commonly found in C patients (53%), and it was significantly different from A (11%) and B (36%) patients (P < 0.01).
Complete RCA obstruction was found in 240 patients (48%), and 45% of these patients had coronary collaterals. Significant differences in collateral blood flows were found among A, B, and C patients (60%, 47% and 11%, respectively, P < 0.01). None of the class A patients demonstrated an absence of flow to all of the RV or RA branches. For class B and C patients, no flow to all of the RV or RA branches was observed in 57% and 15%, and 92% and 34%, respectively (Table 4).
| Variable | Class A | Class B | Class C | Total |
| (n = 425) | (n = 158) | (n = 96) | ||
| Angiography | 291 (68) | 123 (77) | 85 (88) | 499 (73) |
| PCI | 213 | 93 | 76 | 382 (76.5) |
| TT | 78 | 30 | 9 | 117 (23.4) |
| RCA culprit vessel | 266 (91) | 123 (100) | 85 (100) | 474 (95) |
| RCA CL-location | ||||
| Proximal | 42 (16) | 85 (69)b | 78 (92)d | 205 (43) |
| Mid | 144 (54) | 26 (21)b | 6 (7)d | 176 (37) |
| Distal | 80 (30) | 12 (9)b | 1 (1)d | 93 (19) |
| 1-VD | 144 (54) | 39 (32)b | 11 (14) | 194 (40.9) |
| 2-VD | 96 (36) | 31 (25) | 32 (37) | 159 (33.5) |
| 3-VD | 26 (9) | 53 (43)b | 42 (49) | 121 (25.5) |
| RCA + LAD-D | 29 (11) | 44 (36)b | 45 (53)d | 118 (24.8) |
| 100% RCA-O | 119 (45) | 68 (55) | 53 (62) | 240 (48) |
| Without CCC | 47 (40) | 36 (53) | 47 (89)d | 130 (54) |
| With CCC | 72 (60) | 32 (47) | 6 (11)d | 110 (45) |
| Grade 1 | 9 | 10 | 0 | 19 |
| Grade 2 | 36 | 12 | 0 | 48 |
| Grade 3 | 27 | 10 | 6 | 43 |
| RCA–RVB-RAB flow | ||||
| TIMI grade flow | 0.8 ± 1.4 | 0.7 ± 1 | 0.6 ± 0.7 | 0.7 ± 1 |
| TIMI 3 flow in all RVB | 194 (72) | 0 (0)b | 0 (0) | 194 (40) |
| Impaired flow in 1 RVB | 56 (21) | 11 (8.9)b | 0 (0) | 67 (14) |
| Impaired flow in ≥ 2 | ||||
| RVB | 16 (6) | 41 (33)b | 6 (7)d | 63 (13) |
| No flow in all RVB | 0 (0) | 71 (57)b | 79 (92)d | 150 (31) |
| RAB with no flow | 0 (0) | 19 (15)b | 29 (34)d | 48 (10) |
Of the 679 RVI patients, 148 (21.7%) were eligible for TT and 351 (51.6%) for PPCI. TIMI 3-flow by TT was achieved for 65%, 64%, and 0% for RVI classes A, B, and C. TIMI 3-flow was achieved with PPCI in 93%, 91%, and 87%, respectively. The mean residual coronary artery lesion at 90-180 min for the group RVI patients treated with TT or PPCI was 68% ± 10% and 10% ± 8%, respectively (P < 0.000).
Reversible RVWMA at 24-48 h with successful reperfusion was observed for classes A, B, and C patients in 84%, 78%, and 69%, respectively. Reversible RVF (defined as the normalization of the SSP without volume infusion or inotropic agents and/or improvement or normalization of RVWMA and RV dilatation by echocardiography) was documented for class B in 83% and for CS in 43% (Table 5).
| Variable | Class A | Class B | Class C | Total |
| (n = 425) | (n = 158) | (n = 96) | ||
| Symptoms to admission time (min-max) h | 4.6 (2-23) | 5.5 (3.4-19) | 27 (19-48)d | |
| Medical treatment | 111 (26) | 44 (27) | 25 (26) | 180 (26.5) |
| TT | 109 (25) | 30 (19)b | 9 (9)d | 148 (21.7) |
| Primary PCI | 205 (48) | 84 (53) | 62 (64) | 351 (51.6) |
| Stent use | 182 (88) | 80 (95) | 62 (100) | 324 (92) |
| IIb/IIIa GI use | 49% | 47% | 52% | |
| Inotropes/vasopressors | 0% | 100%b | 100% | |
| Temporary pacemaker | 1.20% | 10.7%b | 29%d | |
| IABP support | 0 | 0 | 73.9%d | |
| MVA | 0 | 0 | 100%d | |
| Median time from MI to reperfusion treatment (min-max) h | 1.9 (1.3-4) | 2.1 (1.4-3.8) | 14 (8-22)d | |
| Door-to-needle time (min) | 42 ± 18 | 48 ± 16 | - | |
| Door-to-balloon time (min) | 93 ± 24 | 89 ± 37 | 198 ± 102d | |
| TIMI 3 flow after PCI | 93% | 91% | 87% | |
| TIMI 3 flow after TT | 65% | 64% | 0%d | |
| RCA-Extensive clot burden | 17% | 22% | 75%d | |
| At 24-48 h reversal of RVWMA with SR | 84% | 78% | 69%d |
Class A: Half of the patients had uneventful clinical courses, although 3.2% developed CS, and 4.4% died. Hemodynamic data recorded at 48-72 h in 134 patients with or without successful reperfusion did not show any significant changes compared to baseline hemodynamics measurements. For those patients who received conservative treatment the mortality rate was 7.9%. With TT or PPCI, decreased rates of bradyarrhythmias, AVB, ventricular arrhythmias and in-hospital mortality were observed. After PPCI, no patient progressed to CS, and significantly fewer patients died compared to those treated with TT (P < 0.01 and P < 0.05, respectively) (Table 6).
| Variable | Class A | Class B | Class C | |||||||||
| NR | TT | PCI | Total | NR | TT | PCI | Total | NR | TT | PCI | Total | |
| (n = 111) | (n = 109) | (n = 205) | (n = 425) | (n = 44) | (n = 30) | (n = 84) | (n = 158) | (n = 25) | (n = 9) | (n = 62) | (n = 96) | |
| AVB+ | 16 (14) | 7 (6)b | 11 (5) | 34 (8) | 14 (31) | 9 (30) | 6 (7)d | 29 (18)h | 22 (88) | 8 (88) | 13 (20) | 43 (45)f |
| SVT/VF+ | 18 (16) | 6 (5)b | 9 (4) | 33 (8) | 18 (40) | 9 (30) | 4 (4.7)d | 31(19.6)h | 14 (56) | 5 (55) | 9 (14)d | 28 (29)f |
| AF/PAT | 4 (3) | 3 (2.7) | 0 (0) | 7 (1.6) | 5 (11) | 6 (20) | 4 (4.7)d | 15 (9.4)h | 4 (16) | 2 (22) | 5 (8) | 11 (11) |
| R-MI+ | 6 (5) | 8 (7.3) | 2 (0.9) | 16 (4) | 4 (9) | 3 (10) | 1 (1) | 8 (5) | 2 (8) | 2 (22) | 3 (4.8) | 7 (7.2) |
| UTVR+ | 6 (5) | 4 (3.6) | 2 (0.9) | 12 (3) | 3 (6) | 1 (3) | 1 (1) | 5 (3) | 2 (8) | 1 (11) | 3 (4.8) | 6 (6) |
| MR/T+ | 0 (0) | 2 (1.8) | 0 (0) | 2 (0.4) | 4 (9) | 2 (6) | 0 (0) | 6 (3.7) | 4 (16) | 2 (22) | 2 (3) | 8 (8.3) |
| ARF | 4 (3) | 3 (2.7) | 2 (0.9) | 9 (2) | 4 (9) | 2 (6) | 4 (4.7) | 10 (6) | 5 (20) | 3 (33) | 10 (16) | 18 (19) |
| SSH+ | 18 (16) | 2 (1)b | 0 (0) | 20 (5) | - | - | - | - | - | - | - | - |
| E-CS+ | 8 (7) | 6 (5) | 0 (0) | 14 (3.2) | 10 (22) | 4 (13)b | 8 (9) | 22 (14)h | - | - | - | - |
| Death | 9 (7.9) | 5 (4.4)a | 5 (3.2)f | 19 (4.4) | 12 (27) | 4 (13)b | 7 (8.3)d | 23 (14.5)h | 20 (80) | 9 (100) | 27 (44)d | 56 (58)f |
Class B: PPCI was associated with a decrease in AVB and ventricular arrhythmias. When reperfusion was successful, the mRAP and right ventricular end diastolic pressure (RVEDP) decreased (although not always to normal), and the CI and mSAP increased. The progression to CS was less frequently observed in patients who underwent TT and PPCI compared to patients who did not receive reperfusion. Without reperfusion therapy (RT) the mortality rate was 27%; with TT the rate was reduced to 13% (P < 0.01) and with PPCI to 8.3% (P < 0.01), with significant differences between the two strategies (P < 0.01) (Table 6).
Class C: When PPCI was successful, decreased ventricular arrhythmias, mRAP, RVEDP, mPWP and sPAP were found to be associated with an increased CI and mSAP. Without RT, the in-hospital mortality rate was 80%. With TT, the rate was 100%, and with PPCI, the rate was reduced to 44% (P < 0.01) (Table 6).
To establish the likelihood of mortality, clinical, echocardiographic and hemodynamic variables were tested. When submitted to stepwise logistic regression analysis, age 64-74 years (OR = 5.1; 95%CI: 1.9-14.1, P < 0.01), age ≥ 75 years (OR = 24.2; 95%CI: 7.1-66.5, P < 0.001), SSP < 100 mmHg (OR = 7.7; 95%CI: 2.4-19.1, P < 0.001) and classes B and C (OR = 38.6; 95%CI: 11.5-97.4, P < 0.01) were independent, significant predictors of mortality in the multivariate model.
A progressive increase in long-term mortality was noted for all of the RVI patients. At 8 years, without primary reperfusion, the mortality rate was 32% in class A patients, 48% in class B patients and 85% in class C patients (solid lines). When PPCI was successful, the mortality rate at 8 years was lower than previously observed for each RVI classes (21% for A, 38% for B, and 70% for C, P < 0.001, dashed lines) (Figure 2).
Our findings indicate that there are significant differences in early outcomes and late mortality among the 3 RVI classes. Thus, our discussion for RVI primary reperfusion treatment will focus on the results of reperfusion procedures in each RVI classes.
This class is the only RVI category in which the following question can be raised: Which is best for treating RVI: TT, PPCI or neither?[6]. The query was based on the supposition that (1) many RCA occlusions do not result in significant necrosis or RV dysfunction; (2) some thrombolytic studies have suggested little or no benefit in the absence of RVF; and (3) there are no controlled trials in any category of RVI with TT or PPCI[1-3,11-21].
Nevertheless, more than 40% of class A RVI patients presented at least one major in-hospital complication. Clinical and life threatening risks of an initially hemodynamically silent RVI can not be dismissed when considering timely RT. Although both reperfusion procedures decreased in-hospital mortality in A class RVI patients, our findings suggest that all patients with a hemodynamically silent RVI should undergo PPCI (when available).
Successful reperfusion of the RCA was associated with near normalization of the mRAP and RVEDP, improvement in the CO and mSAP and reversal of RVWMA/RVF in 78% and 83%. For this category of RVI patients our results demonstrate superior outcomes using PPCI over TT, based on following observations: (1) TIMI 3 RCA flow was obtained with TT in 64% and with PPCI in 91% of the patients; (2) more major complications such as AVB and ventricular arrhythmias, were observed using TT; and (3) mortality was lower in the PPCI treated patients compared to the TT-treated patients (13% vs 9%, P < 0.01).
The higher mortality in CS patients resulted from the substantial myocardial damage reflected by the more severe abnormalities in the RV hemodynamic measurements compared to those for class B patients. These findings are also consistent with the subset of patients who were likely to have suffered concomitant severe RA and RV ischemic dysfunction and, as expected, presented with major cardiac complications [2,3,14,15,22,23].
However, with PPCI we demonstrated a significant reduction in mortality (44%) due to (1) restored perfusion of the RCA and its major branches (TIMI 3 flow: 87%) and reversal of RVWMA (69%); (2) reduced mRAP, RVEDP and mPWP and increased CO and mSAP; and (3) a significant decrease in ventricular arrhythmias.
The mortality with PPCI in our study was lower than that in the SHOCK Registry[14] (53%), but was higher compared to the study by Brodie et al[15] in 30 patients (23%). When we compared Brodie’s[15] results with ours, there are close similarities in age, door-to-balloon time, IABP support, stent use and TIMI grade 3-flow after PPCI. However, two important differences were noted. Although twice as many of our patients were sent for PPCI and could make our population more representative of RVI shock patients, the time from the first symptom to reperfusion was twice as long as Brodie’s[15] study.
In our study, we found that the long-term mortality rate continued to increase after the first year and was different for the 3 RVI classes[4,11,24-27]. The differences in long-term survival after RVI in the 3 classes in our study could be due to coronary artery disease progression to complete RCA obstruction, significant LAD disease and/or poorly developed collateral coronary circulation, conditions that are most frequently observed in class B and C RVI patients. Perhaps the most important factors affecting outcome were the success or failure of the RT[1,3,12,16-18].
The major limitation; this analysis used nonrandomized, prospective surveillance and retrospective analysis; thus identified and unidentified confounders may have influenced the trends in reperfusion over time and clinical outcomes. Therefore, it is only an observational study. Nevertheless, this study reports results of RT over time in a large number of patients in 3 RVI categories and the information should be useful in current clinical practice.
In conclusion, PPCI seems to be superior to TT and reduces short and long-term mortality for all 3 RVI categories. Patients in CS should be encouraged to undergo PPCI rather than TT, as a primary reperfusion procedure; consequently, these patients should be transferred to a primary coronary intervention center to decrease the high morbidity and mortality of RVI class C patients.
We express our thanks to Candace Keirns for her kind review the manuscript.
Right ventricular infarction (RVI) is relatively common in patients with acute inferior-posterior left ventricular myocardial infarction. RVI can depress right ventricular (RV) function, resulting in right ventricular failure (RVF) or cardiogenic shock (CS). There are scarce and somewhat conflicting clinical data concerning the effects of interventions designed to achieve reperfusion of the RV myocardium in acute ischemia.
Several investigators have suggested that RV function improves only after successful thrombolytic therapy (TT), whereas others have reported recovery in the absence of early or even any reperfusion of the right coronary artery (RCA). In a study involving limited number of patients, rapid hemodynamic improvement and excellent clinical outcomes have been reported after successful primary percutaneous coronary intervention (PPCI) of the RCA and its major RV branches. Authors demonstrate that PPCI seems to be superior to TT and reduces short and long-term mortality for all 3 RVI categories. Patients in CS should be encouraged to undergo PPCI rather than TT, as a primary reperfusion procedure.
The findings indicate that there are significant differences in early outcomes and late mortality among the 3 RVI classes. Two important differences were noted. Although twice as many of our patients were sent for PPCI and could make the authors population more representative of RVI shock patients.
They found that the most important factors affecting outcome were the success or failure of the reperfusion. PPCI seems to be superior to TT and reduces short and long-term mortality for all 3 RVI categories. Patients in CS should be encouraged to undergo PPCI rather than TT, as a primary reperfusion procedure; consequently, these patients should be transferred to a primary coronary intervention (PCI) center to decrease the high morbidity and mortality. The authors consider that their findings must be taking into consideration to be included in treatment guidelines for the RVI.
The diagnosis of RVF was based on clinical features, including persistent systemic hypotension (systemic systolic pressure ≤ 100 mmHg, right-sided S3 and S4) without features of shock, echocardiographic evidence of ischemic RVF (RV wall motion abnormalities associated with gross RV dilatation), findings that suggest globally depressed RV function and invasive hemodynamic monitoring identifying RVI by a combination of findings that suggest RV dysfunction (low cardiac output and a disproportionate elevation of the mean right atrial pressure compared to the mean pulmonary wedge pressure).
This study investigated the impact of reperfusion therapy by means of primary PCI on clinical outcomes in acute RV infarction comparing with TT. The authors concluded that primary PCI is superior to TT and reduces the short-and-long-term mortality. The results are interesting and provide important impact on clinical practice.
P- Reviewers: Kurisu S, Satoh S S- Editor: Gou SX L- Editor: A E- Editor: Liu SQ
| 1. | Bowers TR, O’Neill WW, Grines C, Pica MC, Safian RD, Goldstein JA. Effect of reperfusion on biventricular function and survival after right ventricular infarction. N Engl J Med. 1998;338:933-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 166] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Goldstein JA, Barzilai B, Rosamond TL, Eisenberg PR, Jaffe AS. Determinants of hemodynamic compromise with severe right ventricular infarction. Circulation. 1990;82:359-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 138] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Zehender M, Kasper W, Kauder E, Schönthaler M, Geibel A, Olschewski M, Just H. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med. 1993;328:981-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 484] [Cited by in RCA: 410] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 4. | Lupi-Herrera E, Lasses LA, Cosio-Aranda J, Chuquiure-Valenzuela E, Martínez-Sánchez C, Ortiz P, González-Pacheco H, Juárez-Herrera U, Rodriguez Mdel C, Vargas-Barrón J. Acute right ventricular infarction: clinical spectrum, results of reperfusion therapy and short-term prognosis. Coron Artery Dis. 2002;13:57-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Dell’Italia LJ, O’Rourke RA. Right ventricular myocardial infarction. Acute Myocardial Infarction. New York: Chapman & Hall 1996; 385-402. |
| 6. | O’Rourke RA. Treatment of right ventricular infarction: thrombolytic therapy, coronary angioplasty or neither? J Am Coll Cardiol. 1998;32:882-884. [PubMed] |
| 7. | Goldstein JA. Right versus left ventricular shock: a tale of two ventricles. J Am Coll Cardiol. 2003;41:1280-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Dell’Italia LJ, Starling MR, O’Rourke RA. Physical examination for exclusion of hemodynamically important right ventricular infarction. Ann Intern Med. 1983;99:608-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 74] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Lopez-Sendon J, Coma-Canella I, Gamallo C. Sensitivity and specificity of hemodynamic criteria in the diagnosis of acute right ventricular infarction. Circulation. 1981;64:515-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 141] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985;5:587-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1118] [Cited by in RCA: 1164] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 11. | Lupi-Herrera E, Chuquiure-Valenzuela E, González-Pacheco H, Juárez-Herrera U, Martínez-Sánchez C, Gaspar J. A proposed functional clinical classification predicts in-hospital and long-term survival in the setting of acute right ventricular infarction. Arch Cardiol Mex. 2008;78:369-378. [PubMed] |
| 12. | Hanzel GS, Merhi WM, O‘Neill WW, Goldstein JA. Impact of mechanical reperfusion on clinical outcome in elderly patients with right ventricular infarction. Coron Artery Dis. 2006;17:517-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Pfisterer M. Right ventricular involvement in myocardial infarction and cardiogenic shock. Lancet. 2003;362:392-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Jacobs AK, Leopold JA, Bates E, Mendes LA, Sleeper LA, White H, Davidoff R, Boland J, Modur S, Forman R. Cardiogenic shock caused by right ventricular infarction: a report from the SHOCK registry. J Am Coll Cardiol. 2003;41:1273-1279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 163] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Brodie BR, Stuckey TD, Hansen C, Bradshaw BH, Downey WE, Pulsipher MW. Comparison of late survival in patients with cardiogenic shock due to right ventricular infarction versus left ventricular pump failure following primary percutaneous coronary intervention for ST-elevation acute myocardial infarction. Am J Cardiol. 2007;99:431-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Bueno H, López-Palop R, Bermejo J, López-Sendón JL, Delcán JL. In-hospital outcome of elderly patients with acute inferior myocardial infarction and right ventricular involvement. Circulation. 1997;96:436-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Gumina RJ, Murphy JG, Rihal CS, Lennon RJ, Wright RS. Long-term survival after right ventricular infarction. Am J Cardiol. 2006;98:1571-1573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Assali AR, Teplitsky I, Ben-Dor I, Solodky A, Brosh D, Battler A, Fuchs S, Kornowski R. Prognostic importance of right ventricular infarction in an acute myocardial infarction cohort referred for contemporary percutaneous reperfusion therapy. Am Heart J. 2007;153:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Hamon M, Agostini D, Le Page O, Riddell JW, Hamon M. Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: meta-analysis. Crit Care Med. 2008;36:2023-2033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Kaandorp TA, Lamb HJ, Poldermans D, Viergever EP, Boersma E, van der Wall EE, de Roos A, Bax JJ. Assessment of right ventricular infarction with contrast-enhanced magnetic resonance imaging. Coron Artery Dis. 2007;18:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Jensen CJ, Jochims M, Hunold P, Sabin GV, Schlosser T, Bruder O. Right ventricular involvement in acute left ventricular myocardial infarction: prognostic implications of MRI findings. AJR Am J Roentgenol. 2010;194:592-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 22. | Bowers TR, O’Neill WW, Pica M, Goldstein JA. Patterns of coronary compromise resulting in acute right ventricular ischemic dysfunction. Circulation. 2002;106:1104-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | White HD, Aylward PE, Huang Z, Dalby AJ, Weaver WD, Barvik S, Marin-Neto JA, Murin J, Nordlander RO, van Gilst WH. Mortality and morbidity remain high despite captopril and/or Valsartan therapy in elderly patients with left ventricular systolic dysfunction, heart failure, or both after acute myocardial infarction: results from the Valsartan in Acute Myocardial Infarction Trial (VALIANT). Circulation. 2005;112:3391-3399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Wong CK, White HD. Risk stratification of patients with right ventricular infarction: is there a need for a specific risk score? Eur Heart J. 2002;23:1642-1645. [PubMed] |
| 25. | Mehta SR, Eikelboom JW, Natarajan MK, Diaz R, Yi C, Gibbons RJ, Yusuf S. Impact of right ventricular involvement on mortality and morbidity in patients with inferior myocardial infarction. J Am Coll Cardiol. 2001;37:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 263] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 26. | Gumina RJ, Wright RS, Kopecky SL, Miller WL, Williams BA, Reeder GS, Murphy JG. Strong predictive value of TIMI risk score analysis for in-hospital and long-term survival of patients with right ventricular infarction. Eur Heart J. 2002;23:1678-1683. [PubMed] |
| 27. | Shiraki H, Yoshikawa T, Anzai T, Negishi K, Takahashi T, Asakura Y, Akaishi M, Mitamura H, Ogawa S. Association between preinfarction angina and a lower risk of right ventricular infarction. N Engl J Med. 1998;338:941-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 75] [Article Influence: 2.8] [Reference Citation Analysis (0)] |