Published online Sep 26, 2013. doi: 10.4330/wjc.v5.i9.355
Revised: August 14, 2013
Accepted: August 20, 2013
Published online: September 26, 2013
Processing time: 74 Days and 9.7 Hours
We are reporting a case of 71-year old lady with a dual chamber demand pacemaker, who developed acute pulmonary edema due to an acute left ventricular (LV) dysfunction and worsening in mitral valve regurgitation after atrioventricular nodal ablation for uncontrolled atrial fibrillation. This was attributed to right ventricular apical pacing leading to LV dyssynchronization. Patient dramatically improved within 12-24 h after upgrading her single chamber pacemaker to biventricular pacing. Our case demonstrates that biventricular pacing can be an effective modality of treatment of acute congestive heart failure. In particular, it can be used when it is secondary to LV dysfunction and severe mitral regurgitation attributed to significant dyssynchrony created by right ventricular pacing in patients with atrioventricular nodal ablation for chronic atrial fibrillation.
Core tip: Our case demonstrates that biventricular pacing (cardiac resynchronization therapy pacemaker, CRT-P) can be an effective modality of treatment in acute congestive heart failure. In particular, it can be used when it is secondary to left ventricular dysfunction and severe mitral regurgitation attributed to significant dyssynchrony created by right ventricular pacing in patients with atrioventricular (AV) nodal ablation for chronic atrial fibrillation. our case matches recent update to guidelines that CRT can be useful in patients with atrial fibrillation and left ventricular ejection fraction (LVEF) ≤ 35% if AV nodal ablation will allow ventricular pacing with CRT except our patient has LVEF > 35%.
- Citation: Barsoum EA, Bhat T, Asti D, Kowalski M, Vazzana T. Cardiac resynchronization therapy in acute pulmonary edema: A case report. World J Cardiol 2013; 5(9): 355-358
- URL: https://www.wjgnet.com/1949-8462/full/v5/i9/355.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i9.355
The detrimental effects of right ventricular apical (RVA) pacing on left ventricular (LV) hemodynamics have been well documented and a higher incidence of heart failure hospitalizations or death in patients with chronic RVA pacing has been attributed to the ventricular dyssynchronization[1,2]. Theoretically, acute RVA pacing could induce discrepancy between electric and mechanical ventricular synchronization resulting in asynchronous left ventricular contraction and relaxation. However, the exact mechanisms of acute LV dysfunction after RVA pacing are not fully understood.
Biventricular pacing (BVP) in chronic heart failure patients within the New York Heart Association (NYHA) functional class III or IV with LV dysfunction and prolonged QRS duration have led to improvement in both morbidity and mortality[3-8]. In addition, cardiac resynchronization therapy (CRT) became the innovative treatment of congestive heart failure, and its use has been extended to patients with NYHA functional class I or II[9-11].
In our case report, we address the benefit and therapeutic role of CRT pacing in patients who developed acute ventricular dysfunction and worsening in mitral regurgitation due to RVA pacing after atrio-ventricular node ablation for refractory atrial fibrillation.
A 71-year old woman presented to the emergency department with a chief complaint of worsening dyspnea and orthopnea for three days (NYHA class IV), she had an atrioventricular (AV) nodal ablation for refractory atrial fibrillation five days prior to presentation. Patient had a history of atrial fibrillation, mild mitral regurgitation, hypothyroidism, hypertension, hypercholesterolemia, chronic obstructive pulmonary disease, obstructive sleep apnea, chronic kidney disease, primary biliary cirrhosis. She had a history of permanent dual chamber pacemaker that was inserted two years ago for symptomatic bradycardia secondary to sick sinus syndrome after atrial fibrillation cardioversion.
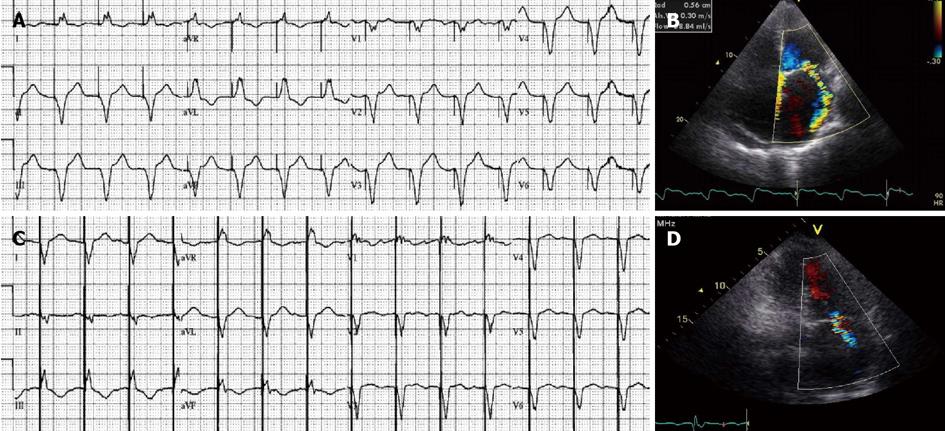
On admission she was orthopneic, tachycardiac and hypoxic that partially improved by using bi-level positive airway pressure. Physical exam revealed positive S1 and S2 heart sounds with a summation gallop, a grade 4/6 apical systolic murmur and a left parasternal systolic murmur that accentuates with inspiration. There was a jugular venous distention up to jaw line. On lung auscultation, there were bibasilar crackles heard. The patient also had bilateral pedal edema. An electrocardiogram (EKG) showed ventricular pacing with a rate of 90 beats per minute (bpm) and QRS duration of 200 ms with positive R in Lead I (Figure 1A). Echocardiographic examination demonstrated decreased left ventricular function (40%), a LV end-diastolic volume (LVEDV) of 97 mL, markedly dilated left atrium (6.1 cm). There were moderate to severe mitral regurgitation (Figure 1B) and moderate to severe tricuspid regurgitation. Pacemaker interrogation showed that the pacemaker was programmed in a DDD mode with lower rate of 60 bpm and upper tracking rate of 120 bpm.
The patient was diagnosed as pulmonary edema and was admitted to the coronary care unit (CCU). She was placed on maximal medical therapy for five days without improvement. Acute ischemic event was ruled out by serial cardiac enzymes. The worsening symptoms and LV dysfunction were attributed to RVA pacing, which then was leading to dyssynchrony and worsening mitral regurgitation.
We decided to upgrade her pacemaker to biventricular (cardiac resynchronization therapy pacemaker, CRT-P), by adding new lead through the coronary sinus to accomplish left ventricular pacing. The old right atrial and right ventricular leads were connected to the CRT pacemaker. Immediately post operatively, the patient reported feeling better and her symptoms improved (NYHA class III). Follow up EKG showed ventricular pacing with a rate of 90 bpm with reduction in QRS duration to 156 ms with negative R in Lead I (Figure 1C). Forty-eight hours after surgery echocardiography demonstrated improvement in LV function (45%) with a reduction in LVEDV to 88 mL and improvement in mitral regurgitation (Figure 1D). The patient was discharged without complication from CCU.
Since the introduction of cardiac pacing five decades ago as an effective treatment for symptomatic bradyacardia, scientists have pursued the goal of better approximating the normal cardiac physiology leading to more highly sophisticated devices[12,13]. BVP has been found to resynchronize ventricular contraction in heart failure patients with wide QRS complexes, leading not only to reversal of LV remodeling over time but also increased functional capacity with an improvement in mortality and quality of life[14,15].
The main indication for CRT is congestive heart failure patients with wide QRS and left ventricular dysfunction (ejection fraction ≤ 35%), who are symptomatic even while on maximal medical therapy. Also, CRT can be useful in patients with atrial fibrillation and left ventricular ejection fraction ≤ 35% if AV nodal ablation will allow ventricular pacing with CRT[16]. According to recent guidelines from the European Society of Cardiology, CRT can be an alternative to traditional right ventricular pacing in patients with heart failure and LV dysfunction who have a standard indication for pacing[17].
Although, biventricular pacing can reverse the dyssynchronization induced by RVA pacing and trials have shown the benefit of biventricular pacing in patients with symptomatic atrial fibrillation after AV nodal ablation[18-20]. A recent meta-analysis of four trials did not demonstrate improvement in mortality with BVP in comparison with RVA pacing[21].
Mitral regurgitation is common in patient with left ventricular dysfunction that negatively affect the survival of patients with congestive heart failure[22], but CRT has been shown to reduce functional mitral regurgitation by optimizing the force balance acting on the mitral valve[23].
Our patient developed acute pulmonary edema after two days of atrio-ventricular node ablation, mostly secondary to left ventricular dyssynchrony, which led to worsening of her mitral regurgitation. This in turn caused pulmonary edema. Despite optimization of medical treatment, her symptoms didn’t improve for five days in CCU, the patient dramatically improved within hours of changing the right ventricular pacemaker to CRT-P. This improvement included a reduction in severity of the status of her mitral regurgitation as well as an alleviation of her symptoms.
Our case demonstrates that biventricular pacing (CRT-P) can be an effective modality of treatment of acute congestive heart failure. In particular, it can be used when it is secondary to LV dysfunction and severe mitral regurgitation attributed to significant dyssynchrony created by right ventricular pacing in patients with AV nodal ablation for chronic atrial fibrillation.
P- Reviewers Chawla M, Durandy Y, Liu T, Petix N, Vermeersch P, Xanthos T S- Editor Gou SX L- Editor A E- Editor Wang CH
| 1. | Tops LF, Schalij MJ, Holman ER, van Erven L, van der Wall EE, Bax JJ. Right ventricular pacing can induce ventricular dyssynchrony in patients with atrial fibrillation after atrioventricular node ablation. J Am Coll Cardiol. 2006;48:1642-1648. [PubMed] |
| 2. | Tse HF, Yu C, Wong KK, Tsang V, Leung YL, Ho WY, Lau CP. Functional abnormalities in patients with permanent right ventricular pacing: the effect of sites of electrical stimulation. J Am Coll Cardiol. 2002;40:1451-1458. [PubMed] |
| 3. | Sutton MG, Plappert T, Hilpisch KE, Abraham WT, Hayes DL, Chinchoy E. Sustained reverse left ventricular structural remodeling with cardiac resynchronization at one year is a function of etiology: quantitative Doppler echocardiographic evidence from the Multicenter InSync Randomized Clinical Evaluation (MIRACLE). Circulation. 2006;113:266-272. [PubMed] |
| 4. | Young JB, Abraham WT, Smith AL, Leon AR, Lieberman R, Wilkoff B, Canby RC, Schroeder JS, Liem LB, Hall S. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA. 2003;289:2685-2694. [PubMed] |
| 5. | Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, Kocovic DZ, Packer M, Clavell AL, Hayes DL. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346:1845-1853. [PubMed] |
| 6. | Cazeau S, Leclercq C, Lavergne T, Walker S, Varma C, Linde C, Garrigue S, Kappenberger L, Haywood GA, Santini M. Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med. 2001;344:873-880. [PubMed] |
| 7. | Auricchio A, Stellbrink C, Sack S, Block M, Vogt J, Bakker P, Huth C, Schöndube F, Wolfhard U, Böcker D. Long-term clinical effect of hemodynamically optimized cardiac resynchronization therapy in patients with heart failure and ventricular conduction delay. J Am Coll Cardiol. 2002;39:2026-2033. [PubMed] |
| 8. | Higgins SL, Hummel JD, Niazi IK, Giudici MC, Worley SJ, Saxon LA, Boehmer JP, Higginbotham MB, De Marco T, Foster E. Cardiac resynchronization therapy for the treatment of heart failure in patients with intraventricular conduction delay and malignant ventricular tachyarrhythmias. J Am Coll Cardiol. 2003;42:1454-1459. [PubMed] |
| 9. | Linde C, Abraham WT, Gold MR, St John Sutton M, Ghio S, Daubert C. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and previous heart failure symptoms. J Am Coll Cardiol. 2008;52:1834-1843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 860] [Cited by in RCA: 922] [Article Influence: 54.2] [Reference Citation Analysis (0)] |
| 10. | Tang AS, Wells GA, Talajic M, Arnold MO, Sheldon R, Connolly S, Hohnloser SH, Nichol G, Birnie DH, Sapp JL. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med. 2010;363:2385-2395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1322] [Cited by in RCA: 1382] [Article Influence: 92.1] [Reference Citation Analysis (0)] |
| 11. | Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, Estes NA, Foster E, Greenberg H, Higgins SL. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009;361:1329-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2231] [Cited by in RCA: 2308] [Article Influence: 144.3] [Reference Citation Analysis (0)] |
| 12. | Jeffrey K, Parsonnet V. Cardiac pacing, 1960-1985: a quarter century of medical and industrial innovation. Circulation. 1998;97:1978-1991. [PubMed] |
| 13. | Trohman RG, Kim MH, Pinski SL. Cardiac pacing: the state of the art. Lancet. 2004;364:1701-1719. [PubMed] |
| 14. | Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, DeMets D, White BG. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140-2150. [PubMed] |
| 15. | Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539-1549. [PubMed] |
| 16. | Tracy CM, Epstein AE, Darbar D, Dimarco JP, Dunbar SB, Estes NA, Ferguson TB, Hammill SC, Karasik PE, Link MS. 2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2012;60:1297-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 257] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 17. | McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3411] [Cited by in RCA: 3554] [Article Influence: 273.4] [Reference Citation Analysis (0)] |
| 18. | Leclercq C, Cazeau S, Lellouche D, Fossati F, Anselme F, Davy JM, Sadoul N, Klug D, Mollo L, Daubert JC. Upgrading from single chamber right ventricular to biventricular pacing in permanently paced patients with worsening heart failure: The RD-CHF Study. Pacing Clin Electrophysiol. 2007;30 Suppl 1:S23-S30. [PubMed] |
| 19. | Orlov MV, Gardin JM, Slawsky M, Bess RL, Cohen G, Bailey W, Plumb V, Flathmann H, de Metz K. Biventricular pacing improves cardiac function and prevents further left atrial remodeling in patients with symptomatic atrial fibrillation after atrioventricular node ablation. Am Heart J. 2010;159:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 20. | Doshi RN, Daoud EG, Fellows C, Turk K, Duran A, Hamdan MH, Pires LA. Left ventricular-based cardiac stimulation post AV nodal ablation evaluation (the PAVE study). J Cardiovasc Electrophysiol. 2005;16:1160-1165. [PubMed] |
| 21. | Chatterjee NA, Upadhyay GA, Ellenbogen KA, Hayes DL, Singh JP. Atrioventricular nodal ablation in atrial fibrillation: a meta-analysis of biventricular vs. right ventricular pacing mode. Eur J Heart Fail. 2012;14:661-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Trichon BH, Felker GM, Shaw LK, Cabell CH, O’Connor CM. Relation of frequency and severity of mitral regurgitation to survival among patients with left ventricular systolic dysfunction and heart failure. Am J Cardiol. 2003;91:538-543. [PubMed] |
| 23. | Solis J, McCarty D, Levine RA, Handschumacher MD, Fernandez-Friera L, Chen-Tournoux A, Mont L, Vidal B, Singh JP, Brugada J. Mechanism of decrease in mitral regurgitation after cardiac resynchronization therapy: optimization of the force-balance relationship. Circ Cardiovasc Imaging. 2009;2:444-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |