Published online Sep 26, 2013. doi: 10.4330/wjc.v5.i9.317
Revised: July 30, 2013
Accepted: August 16, 2013
Published online: September 26, 2013
Processing time: 94 Days and 16.6 Hours
The present review analyses the mechanisms relating heart failure and hyponatremia, describes the association of hyponatremia with the progress of disease and morbidity/mortality in heart failure patients and presents treatment options focusing on the role of arginine vasopressin (AVP)-receptor antagonists. Hyponatremia is the most common electrolyte disorder in the clinical setting and in hospitalized patients. Patients with hyponatremia may have neurologic symptoms since low sodium concentration produces brain edema, but the rapid correction of hyponatremia is also associated with major neurologic complications. Patients with heart failure often develop hyponatremia owing to the activation of many neurohormonal systems leading to decrease of sodium levels. A large number of clinical studies have associated hyponatremia with increased morbidity and mortality in patients hospitalized for heart failure or outpatients with chronic heart failure. Treatment options for hyponatremia in heart failure, such as water restriction or the use of hypertonic saline with loop diuretics, have limited efficacy. AVP-receptor antagonists increase sodium levels effectively and their use seems promising in patients with hyponatremia. However, the effects of AVP-receptor antagonists on hard outcomes in patients with heart failure and hyponatremia have not been thoroughly examined.
Core tip: Patients with heart failure and hyponatremia have increased morbidity and mortality compared with subjects with normal sodium levels. Established treatment options for hyponatremia in heart failure such as fluid restriction or the use of hypertonic saline with loop diuretics have limited efficacy and compliance issues. Arginine vasopressin (AVP)-receptor antagonists increase sodium levels and exhibit beneficial effects on hemodynamic variables in patients with heart failure. However, double-blind, placebo-controlled trials examining the effects of AVP-receptor antagonists on mortality, quality of life and length of hospital stay in patients with heart failure and hyponatremia are missing.
- Citation: Filippatos TD, Elisaf MS. Hyponatremia in patients with heart failure. World J Cardiol 2013; 5(9): 317-328
- URL: https://www.wjgnet.com/1949-8462/full/v5/i9/317.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i9.317
Hyponatremia is defined as a serum sodium concentration lower than 136 mmol/L[1]. It is recognized as the most common electrolyte disorder both in the clinical setting and in hospitalized patients[2,3]. The prevalence of hyponatremia in hospitalized patients varies depending on the sodium level used to define the condition and the patient population[4-13]. Patients with hyponatremia may suffer major neurologic complications since low sodium concentration produces brain edema, but the rapid correction of hyponatremia is also associated with increased morbidity and mortality[14-18]. It should be mentioned that elderly women and subjects who also have hypokalemia are characterized by an increased risk for neurologic complications following rapid correction of hyponatremia[19-24]. The mortality rates associated with hyponatremia range from 5% to 50% depending on severity and acuity of onset[25].
Heart failure is a disabling and growing disease associated, associated with high morbidity and mortality rates and with annually increasing costs[26-29]. Hyponatremia is often encountered in patients with heart failure[30-33]. In a study of our group, 33.7% of patients with congestive heart failure had hyponatremia, which was the most common electrolyte abnormality in the study population[34]. Aim of the present review is to demonstrate the mechanisms relating heart failure and hyponatremia, to present the association of hyponatremia with the progress of disease and morbidity/mortality in heart failure patients and to describe treatment options focusing on the role of arginine-vasopressin (AVP)-receptor antagonists.
A PubMed/Scopus search was performed up to June 2013 using combinations of “heart failure” with the following keywords: sodium, hyponatremia, vasopressin, aldosterone, diuretics, morbidity, mortality, hospital stay, water restriction, vaptans, vasopressin-receptor antagonists, tolvaptan, conivaptan, lixivaptan, electrolyte. Randomised controlled trials, original papers, review articles and case reports are included in the present review. References of these articles were scrutinised for relevant articles.
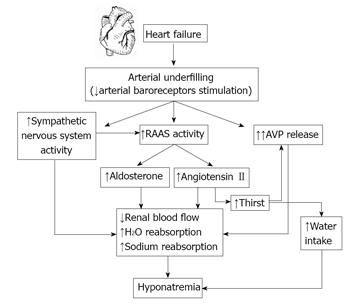
Many factors are implicated in the pathogenesis of hyponatremia in patients with heart failure (Figure 1)[6]. Heart failure reduces cardiac output and results in arterial underfilling, which induces the activation of the sympathetic nervous system (SNS). This leads to peripheral and renal vasoconstriction and decreases glomerular filtration rate, effects that combined with arterial underfilling result in increased reabsorption of sodium and water and induce the activation of the renin-angiotensin-aldosterone system (RAAS)[31,32,35]. The subsequent increase of angiotensin II results in peripheral and renal vasoconstriction and induces aldosterone release from the adrenal gland causing further sodium retention[36-43]. Arterial underfilling and the activation of both SNS and RAAS lead to increased release of AVP. Angiotensin II also stimulates the thirst center of the brain and increases water intake and the release of AVP[44-46]. AVP binds to the vasopressin-2 (V2) receptor subtype and increases the number of aquaporin-2 water channels, leading to increased permeability of water in the collecting duct and enhanced free water retention[47-50]. Aquaporin water channels consist of six membrane-spanning domains that form water channels within collecting duct membranes[50-52].
In agreement with the above mechanisms patients with heart failure and hyponatremia have higher levels of plasma renin, angiotensin II, aldosterone, epinephrine, norepinephrine, and dopamine compared with patients with normal sodium levels[40,53,54]. It has been shown that heart failure patients exhibit increased AVP production and generally a dysregulation of AVP characterised by an elevation of its levels despite the presence of volume overload, atrial distension and low plasma osmolality[55-61]. Furthermore, the urinary excretion of aquaporin-2 is increased in heart failure patients with elevated AVP[48]. Notably, the elevated plasma AVP levels are not appropriately reduced even with acute water loading in hyponatremic patients with advanced heart failure[62]. These observations led to the hypothesis that hyponatremia may be a marker of neurohormonal activation that reflects the severity of heart failure[63].
AVP plays an important role in the development of hyponatremia in heart failure but unfortunately it cannot reliably determined by the current laboratory methods. Copeptin, the C-terminal part of the AVP precursor peptide, is secreted in an equimolar ratio to AVP and is a sensitive and stable surrogate marker for its release[64]. Copeptin levels have been used as a prognostic marker in patients with acute diseases such as lower respiratory tract infection, heart disease and stroke. Copeptin is also a promising marker in the differential diagnosis of hyponatremia[64]. In a study plasma copeptin and N-terminal pro-B-type natriuretic peptide were evaluated in 340 patients with left ventricular systolic dysfunction, who were divided into 3 groups according to copeptin tertiles and followed for 55 mo[65]. Copeptin, although it did not predict the future development of hyponatremia, was a significant predictor of hospitalization or death (HR = 1.4, 95%CI: 1.1-1.9, P < 0.019) even after adjustment for plasma sodium, loop diuretic dose, and N-terminal pro-B-type natriuretic peptide levels[65]. However, a secondary analysis of three prospective studies of patients with lower respiratory tract infections and acute cerebrovascular events showed that plasma copeptin levels did not add significant information to the investigation of sodium imbalance states in hospitalized patients[66]. It should be mentioned that this analysis was based on a small sample size and did not focus on patients with heart failure[66].
Another molecule that may play role in the development of hyponatremia in patients with heart failure is apelin, which is an endogenous ligand of the orphan APJ receptor. Apelin has a wide tissue distribution and is implicated in the regulation of body fluid homeostasis, cardiovascular functions, glucose homeostasis, cell proliferation, and angiogenesis[67]. Apelin has diuretic properties and it has been shown that it is regulated in opposite directions with AVP to maintain body fluid homeostasis[67,68]. There is evidence of apelin dysregulation in patients with cardiac failure since it has been shown that the observed increase in plasma apelin cannot compensate for the higher levels of AVP and may contribute to the corresponding water metabolism defect[69].
Diuretics are one of the most common causes of drug-induced hyponatremia[70,71]. The great majority of cases of diuretic-induced hyponatremia are caused by thiazide diuretics, which act solely in the distal tubules and do not interfere with urinary concentration and the ability of AVP to promote water retention[24,70,72,73]. Thiazide-induced hyponatremia is usually mild, but acute severe hyponatremia is occasionally developed as an idiosyncratic reaction[70,72,74].
It should also be mentioned that the hydrochlorothiazide and amiloride combination appears to increase the risk of hyponatremia. This increment is probably because of the direct effect of amiloride on the collecting tubule increasing sodium loss[75-77]. Moreover, amiloride spares potassium and, hence, aggravates thiazide-induced hyponatremia as a consequence of potassium retainment by exchanging it for sodium in the distal tubule. Indapamide administration has also been associated with hyponatremia[78-80].
A large number of clinical studies have confirmed the association of hyponatremia with increased morbidity and mortality in patients hospitalized for heart failure or outpatients with chronic heart failure[10,11,42,81-94]. A recent meta-analysis that included 14766 patients from 22 studies and used as endpoint the death from any cause at 3 years showed that the risk of death is linearly increasing with serum sodium levels < 140 mmol/L[95]. Moreover, hyponatremia was predictive of death in both patients with reduced or preserved ejection fraction[95]. Another recent study, which enrolled 1000 consecutive patients with heart failure of any cause and severity for a median duration of 5.1 years, showed that hyponatremia was associated with a significantly increased mortality risk (HR = 2.10, 95%CI: 1.60-2.77)[96]. Notably, it was shown that serum sodium within the reference range has a U-shaped association with mortality risk; specifically, sodium levels of 135-139 mmol/L indicated an increased mortality risk, whereas sodium levels of 140-145 mmol/L were associated with the best prognosis[96]. Hyponatremia has also been found to be an important predictor of survival in several risk models in patients with heart failure[83,84,97-101].
Hyponatremia is associated with increased rate of re-hospitalization[102], increased length of stay[10,84,103], increased hospital resource use[104], increased complications[81,105] and increased costs[106-108]. Furthermore, the presence of hyponatremia in patients with acute ST-elevation myocardial infarction is associated with the development of acute heart failure and with in-hospital adverse outcomes[109]. Moreover, the risk of in-hospital mortality was associated with the severity of hyponatremia in patients with acute ST-elevation myocardial infarction[109,110].
Recent studies have also shown the role of copeptin in the prognosis of heart failure. In the Biomarkers in Acute Heart Failure trial, which enrolled 1641 patients with acute dyspnea, of whom 557 patients had acute heart failure, copeptin concentrations in the highest quartile were associated with increased 90-d mortality (HR = 3.85, P < 0.001)[111]. The combination of elevated copeptin and hyponatremia was associated with a higher risk of 90-d mortality (HR = 7.36, P < 0.001). Of note, no correlation was found between copeptin and sodium concentration[111]. Similarly, marked elevations of copeptin were independent predictors of poor outcomes in a cohort of 157 patients with class III or IV heart failure prospectively evaluated for 2 years[112]. Furthermore, the combination of increased copeptin levels with hyponatremia was a stronger predictor[112].
In acute symptomatic hyponatremia serum sodium concentrations decrease rapidly resulting in the appearance of neurologic symptoms[25,113]. These neurologic symptoms are due to brain edema resulting from fluid shifts from the hypotonic extracellular fluid into the more hypertonic brain[1]. In acute symptomatic hyponatremia with severe neurologic symptoms (for example seizures and/or obtundation) immediate treatment is required to reduce the risk of neurologic complications[1,114]. The proposed treatment for symptomatic hyponatremia is the infusion of hypertonic saline to increase serum sodium by 1-2 mEq/L per hour until symptoms subside[54]. After this emergency intervention, the treatment should continue with the measures that are analysed below for the correction of chronic hyponatremia. Notably, in any case the rate of sodium correction should not exceed the recommended limit of 8 mEq/L in any 24-h period.
In patients with chronic hyponatremia the rate of correction of sodium levels should not exceed the rate of 8 mEq/L per day in any 24-h period[115,116]. A more rapid correction increases the danger of central pontine myelinolysis[1,117,118]. Central pontine myelinolysis is a neurological disease caused by the rapid rise in serum sodium levels during treatment in individuals with hyponatremia. It is characterised by severe damage of the myelin sheath of nerve cells in the pons area in the brainstem, leading to confusion, horizontal gaze paralysis, spastic quadriplegia, dysphagia, dysarthria and other neurological symptoms. The neurologic deterioration occurs 48-72 h after the rapid correction of hyponatremia. Death is common, but if the patient survives chronic neurologic deficits including locked-in syndrome and spastic quadriparesis are usually observed[117-120]. Brain magnetic resonance imaging is used to reveal the demyelination in the brainstem pons[121,122].
Fluid is restricted to amounts less than 800-1000 mL/d in order to achieve a negative water balance[54]. It is the least expensive treatment option. In a randomized study, patients with hyponatremia (serum sodium ≤ 137 mg/dL) received usual care (n = 26) or 1000 mL/d fluid restriction (n = 20) at discharge[123]. After 60 d patients in the group of fluid restriction had significantly better scores of symptom burden, total symptoms and overall quality of life. In this study there were no differences in thirst or adherence to fluid restriction between groups[123]. However, many patients with heart failure have increased thirst, which reduces the compliance in fluid restriction[54].
The use of diuretics is the mainstay of treatment in patients with heart failure with fluid overload. Loop diuretics are preferred because they increase electrolyte-free water clearance[71]. It has been shown that the addition of a loop diuretic to an angiotensin-converting enzyme inhibitor reversed hyponatremia in heart failure patients[124]. Furthermore, a study of our group showed that the combination of angiotensin-converting enzyme inhibitors with furosemide improves sodium concentration in heart failure patients with hyponatremia[125]. Specifically, six patients with congestive heart failure and serum sodium of 125-128 mmol/L treated with furosemide received captopril in progressively increasing doses. The addition of captopril resulted in clinical improvement and induced a significant increase in serum sodium levels, which was associated with a rise in the diluting ability of the kidney[125].
It has also been shown that the infusion of hypertonic saline combined with high-dose diuretics was associated with increase in serum sodium levels and a potential improvement in outcomes in heart failure patients[126,127]. One study enrolled 60 patients with New York Heart Association Class IV heart failure, who received infusion of furosemide (500 to 1000 mg) plus hypertonic saline (150 mL 1.4%-4.6% NaCl) in 30 min for 6 to 12 d. The combination of furosemide and hypertonic saline increased serum sodium levels and decreased length of stay and re-admissions compared with furosemide infusion alone[126]. In a larger study, which enrolled 107 patients with heart failure, the infusion of furosemide plus hypertonic saline was associated with improvement in symptoms and reduction of re-admissions and mortality[127].
AVP has three different receptor subtypes[128]. V1A receptors are found in vascular smooth muscle and cardiac myocytes causing vasoconstriction and hypertrophy, as well as in platelets and hepatocytes regulating platelet aggregation and glycogen metabolism[129-135]. V1B receptors are found in the anterior pituitary gland and are associated with adrenocorticotropic hormone and b-endorphin release[136]. Interestingly, these receptor subtypes have been also linked to the regulation of glucose homeostasis[137]. V2 receptors are found on the renal collecting ducts and cause free-water reabsorption leading to increased water retention[50,51,138]. V2 receptors are mainly linked to the development of hyponatremia in heart failure patients.
The central role of AVP in hyponatremia is targeted with the AVP-receptor antagonists (vaptans) conivaptan, tolvaptan and lixivaptan, which differ in their affinity for the V1A and V2 receptor[139].
Tolvaptan: Tolvaptan is an orally active, selective V2-receptor blocker. It is recommended to initiate the drug in hospital for safety reasons, although patients have been receiving tolvaptan safely as long as 3 years[140].
Tolvaptan has been extensively studied in patients with heart failure. The administration of tolvaptan at a single oral dose (15, 30 or 60 mg) in 181 patients with advanced heart failure on standard therapy resulted in favourable changes in filling pressures and a significant increase in urine output[141]. The low-dose (7.5 mg/d) tolvaptan for seven days improved hemodynamic parameters and resulted in significant fluid removal in 22 patients with chronic heart failure[142]. Tolvaptan administration for 7 consecutive days reduced body weight and improved symptoms compared with placebo in patients with heart failure and volume overload despite the use of conventional diuretics[143,144]. Tolvaptan administration in 254 stable patients with heart failure decreased body weight and increased urine volume[145]. Similarly, in the Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Congestive Heart Failure (ACTIV in CHF) trial tolvaptan administration in hospitalized patients with systolic heart failure (n = 319) resulted in a significant decrease in body weight at 24 h without any changes in heart rate or blood pressure or increase in the rates of hypokalemia or worsening renal function[146]. Of note, a lower 60-d mortality was observed in post hoc analyses in patients with renal dysfunction or severe systemic congestion[146,147]. In the Multicenter Evaluation of Tolvaptan Effect on Remodeling (METEOR) study tolvaptan for 54 wk did not show any beneficial or detrimental effects on remodeling compared with placebo in 240 patients with stable systolic heart failure[148]. Moreover, tolvaptan administration prevented the worsening of renal function compared with conventional therapy in patients with acute decompensated heart failure and high risk of renal failure[149].
The larger trial of tolvaptan is the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST), which enrolled 4133 patients hospitalized with systolic heart failure. A significant reduction in body weight on day 7 after discharge was demonstrated[150]. During a median follow-up of 9.9 mo a significant increase in sodium levels was observed in patients with hyponatremia[151]. However, tolvaptan had no effect on long-term mortality or heart failure-related morbidity. Specifically, 537 patients (25.9%) in the tolvaptan group and 543 (26.3%) in the placebo group died (HR = 0.98, 95%CI: 0.87-1.11, P = 0.68). The composite of cardiovascular death or hospitalization for heart failure occurred in 42% of patients receiving tolvaptan and 40.2% of patients receiving placebo (HR = 1.04, 95%CI: 0.95-1.14, P = 0.55)[151]. It should be mentioned that EVEREST did not enrol solely patients with heart failure and hyponatremia, who in theory could benefit from the administration of tolvaptan. A recent analysis of patients with hyponatremia from the EVEREST trial (n = 475) showed that tolvaptan was associated with greater likelihood of normalization of serum sodium, greater weight reduction and greater relief of dyspnea at discharge than placebo (all P < 0.05)[152]. Tolvaptan did not reduce long-term outcomes compared with placebo among all patients with hyponatremia. However, the administration of tolvaptan in patients with pronounced hyponatremia (< 130 mEq/L; n = 92) resulted in a significant reduction in cardiovascular morbidity and mortality after discharge (P = 0.04)[152].
A recent study showed that the use of a single dose tolvaptan in pediatric patients with heart failure (n = 28) significantly increased serum sodium concentration (P < 0.001)[153]. Furthermore, urine output was significantly increased at 24 h (P < 0.001).
Lixivaptan: Lixivaptan is an oral, highly selective V2-receptor antagonist[154]. The administration of lixivaptan in 42 patients with mild to moderate heart failure was associated with significant increases in urine volume and solute-free water excretion without any significant change in plasma renin, norepinephrine, aldosterone, atrial natriuretic peptide and endothelin-1 levels[155]. Treatment with lixivaptan 100 mg/d for 8 wk (in addition to standard therapy) in outpatients with heart failure and volume overload significantly reduced body weight and improved dyspnea and orthopnea[156]. Lixivaptan was generally well tolerated but thirst and polyuria occurred more frequently in the active drug group compared with the placebo group[156].
The effectiveness and safety of lixivaptan for 60 d in patients with heart failure and hyponatremia are being evaluated in a double-blind, placebo-controlled study, the Treatment of Hyponatremia Based on Lixivaptan in NYHA Class III/IV Cardiac Patient Evaluation (BALANCE) study[157]. Primary endpoint is the effect of lixivaptan on serum sodium in patients hospitalized with worsening heart failure (target n = 650), signs of congestion and serum sodium concentrations < 135 mEq/L. Other endpoints include assessment of dyspnea, body weight, cognitive function and days of hospital-free survival[157].
Conivaptan: Conivaptan is both a V1A- and a V2-receptor blocker; the aquaretic effect is due to antagonism of the V2 receptor[158-161]. The drug is a substrate and potent inhibitor of the cytochrome P450 isoenzyme CYP3A4 and may result in significant drug-drug interactions[158]. The drug is given only intravenously (20 mg bolus, then continuous infusion 20-40 mg/24 h) over up to 4 d in hospital[139]. It has been shown that volume status or the presence of congestive heart failure do not alter the pharmacokinetics of conivaptan 20 or 40 mg/d[162].
The effects of conivaptan in hyponatremia of various origin were evaluated in 3 randomized double-blind, controlled studies which showed significant improvement in serum sodium levels[163-165]. The acute hemodynamic effects of conivaptan (single intravenous dose of 10, 20 or 40 mg) in heart failure were examined in 142 patients with symptomatic heart failure (New York Heart Association class III and IV)[166]. The administration of conivaptan resulted in favourable changes in hemodynamic variables and urine output without affecting blood pressure or heart rate[166]. In a double-blind trial, which randomised 170 patients hospitalized for worsening heart failure receiving standard therapy to conivaptan (20 mg loading dose followed by 2 successive 24-h continuous infusions of 40, 80, or 120 mg/d) or placebo, conivaptan significantly increased urine output at 24 h compared with placebo (1-1.5 L difference, P≤ 0.02 for all doses)[167]. Body weight was decreased with the 40 and 80 mg/d dose in parallel with the increase in urine output but this reduction was not significant. Global and respiratory status at 48 h did not differ significantly between conivaptan and placebo groups. Conivaptan was well tolerated with the most common adverse events being infusion-site reactions[167]. Another study assessed the role of conivaptan, furosemide or their combination in 8 patients with chronic stable heart failure on standard medical treatment[168]. Both conivaptan and furosemide monotherapy increased urine volume, but the combination treatment significantly augmented this effect. Although conivaptan did not increase urinary sodium excretion compared with furosemide, the combination led to a greater urinary sodium excretion compared with furosemide monotherapy. There were no significant effects of conivaptan, furosemide or their combination on heart rate, arterial pressure, systemic vascular resistance, cardiac output, glomerular filtration rate, renal blood flow, plasma catecholamines, renin activity, AVP and B-type natriuretic peptide levels[168].
Other considerations: Fluid should not be restricted in patients with hyponatremia who start AVP-receptor antagonists and serum sodium concentration should be monitored every 6-8 h in order to avoid rapid correction of sodium levels[139]. Although osmotic demyelination has not been reported with the use of AVP-receptor antagonists in studies with heart failure patients, a warning letter was recently published concerning the occurrence of neurological sequelae in some patients treated with tolvaptan in whom the correction of serum sodium exceeded the suggested rate[169].
AVP-receptor antagonists should not be used in patients with hypovolemic hyponatremia, who should instead be treated with isotonic saline. Adverse effects of AVP-receptor antagonists include dry mouth, thirst and increased urination in most patients. These agents may not be effective in patients with advanced acute or chronic renal failure[139]. Furthermore, the United States Food and Drug Administration based on a recent large clinical trial of tolvaptan in patients with autosomal dominant polycystic kidney disease[170] has recently determined that tolvaptan should not administrated for more than 30 d or in patients with underlying liver disease, because of the danger of significant liver injury, potentially leading to liver transplant or death[171].
Many patients with heart failure have decreased sodium levels due to neurohormonal mechanisms. Patients with heart failure and hyponatremia have increased morbidity and worse prognosis compared with subjects with normal sodium levels. Treatment options for hyponatremia in heart failure such as fluid restriction or the use of hypertonic saline with loop diuretics have limited efficacy and compliance issues. AVP-receptor antagonists increase effectively sodium levels and their use seems promising in patients with hyponatremia. However, it is not clear whether normalization of serum sodium also leads to an improved prognosis. Furthermore, the effects of AVP-receptor antagonists on the mortality, quality of life and length of hospital stay, as well as their cost-effectiveness, have not been thoroughly examined in double-blind, placebo-controlled trials in patients with heart failure and hyponatremia.
P- Reviewers Esposito P, Giuffre M, Liu T S- Editor Wen LL L- Editor A E- Editor Wang CH
| 1. | Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1255] [Cited by in RCA: 1106] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 2. | Siragy HM. Hyponatremia, fluid-electrolyte disorders, and the syndrome of inappropriate antidiuretic hormone secretion: diagnosis and treatment options. Endocr Pract. 2006;12:446-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Milionis HJ, Liamis GL, Elisaf MS. The hyponatremic patient: a systematic approach to laboratory diagnosis. CMAJ. 2002;166:1056-1062. [PubMed] |
| 4. | Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119:S30-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 495] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 5. | Oren RM. Hyponatremia in congestive heart failure. Am J Cardiol. 2005;95:2B-7B. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Bettari L, Fiuzat M, Felker GM, O’Connor CM. Significance of hyponatremia in heart failure. Heart Fail Rev. 2012;17:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Janicic N, Verbalis JG. Evaluation and management of hypo-osmolality in hospitalized patients. Endocrinol Metab Clin North Am. 2003;32:459-81, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 97] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Hawkins RC. Age and gender as risk factors for hyponatremia and hypernatremia. Clin Chim Acta. 2003;337:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 257] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 9. | Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122:857-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 499] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 10. | Gheorghiade M, Abraham WT, Albert NM, Gattis Stough W, Greenberg BH, O’Connor CM, She L, Yancy CW, Young J, Fonarow GC. Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J. 2007;28:980-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 464] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 11. | Tavazzi L, Maggioni AP, Lucci D, Cacciatore G, Ansalone G, Oliva F, Porcu M. Nationwide survey on acute heart failure in cardiology ward services in Italy. Eur Heart J. 2006;27:1207-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 171] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 12. | Cleland JG, Swedberg K, Follath F, Komajda M, Cohen-Solal A, Aguilar JC, Dietz R, Gavazzi A, Hobbs R, Korewicki J. The EuroHeart Failure survey programme-- a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J. 2003;24:442-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 963] [Cited by in RCA: 902] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 13. | Filippatos TD, Milionis HJ, Elisaf MS. Alterations in electrolyte equilibrium in patients with acute leukemia. Eur J Haematol. 2005;75:449-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain damage after elective surgery in healthy women. N Engl J Med. 1986;314:1529-1535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 353] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 15. | Arieff AI, Llach F, Massry SG. Neurological manifestations and morbidity of hyponatremia: correlation with brain water and electrolytes. Medicine (Baltimore). 1976;55:121-129. [PubMed] |
| 16. | Gross P, Palm C. Thiazides: do they kill? Nephrol Dial Transplant. 2005;20:2299-2301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Reynolds RM, Seckl JR. Hyponatraemia for the clinical endocrinologist. Clin Endocrinol (Oxf). 2005;63:366-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Gross SG, Bell RD. Central pontine myelinolysis and rapid correction of hyponatremia. Tex Med. 1982;78:59-60. [PubMed] |
| 19. | Verbalis JG, Martinez AJ. Neurological and neuropathological sequelae of correction of chronic hyponatremia. Kidney Int. 1991;39:1274-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 90] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Ayus JC, Arieff AI. Hyponatremia and myelinolysis. Ann Intern Med. 1997;127:163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Ayus JC, Krothapalli RK, Arieff AI. Treatment of symptomatic hyponatremia and its relation to brain damage. A prospective study. N Engl J Med. 1987;317:1190-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 262] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 22. | Lohr JW. Osmotic demyelination syndrome following correction of hyponatremia: association with hypokalemia. Am J Med. 1994;96:408-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 120] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 23. | Lien YH. Role of organic osmolytes in myelinolysis. A topographic study in rats after rapid correction of hyponatremia. J Clin Invest. 1995;95:1579-1586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 60] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Liamis G, Milionis H, Elisaf M. Blood pressure drug therapy and electrolyte disturbances. Int J Clin Pract. 2008;62:1572-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Fall PJ. Hyponatremia and hypernatremia. A systematic approach to causes and their correction. Postgrad Med. 2000;107:75-82; quiz 179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 971] [Cited by in RCA: 956] [Article Influence: 79.7] [Reference Citation Analysis (0)] |
| 27. | Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:188-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 912] [Cited by in RCA: 950] [Article Influence: 73.1] [Reference Citation Analysis (0)] |
| 28. | Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46-e215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2338] [Cited by in RCA: 2613] [Article Influence: 174.2] [Reference Citation Analysis (0)] |
| 29. | Filippatos TD, Mikhailidis DP. Statins and heart failure. Angiology. 2008;59:58S-61S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Fried LF, Palevsky PM. Hyponatremia and hypernatremia. Med Clin North Am. 1997;81:585-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 31. | Farmakis D, Filippatos G, Parissis J, Kremastinos DT, Gheorghiade M. Hyponatremia in heart failure. Heart Fail Rev. 2009;14:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 32. | Sica DA. Hyponatremia and heart failure--pathophysiology and implications. Congest Heart Fail. 2005;11:274-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Klein L, O’Connor CM, Leimberger JD, Gattis-Stough W, Piña IL, Felker GM, Adams KF, Califf RM, Gheorghiade M. Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation. 2005;111:2454-2460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 413] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 34. | Milionis HJ, Alexandrides GE, Liberopoulos EN, Bairaktari ET, Goudevenos J, Elisaf MS. Hypomagnesemia and concurrent acid-base and electrolyte abnormalities in patients with congestive heart failure. Eur J Heart Fail. 2002;4:167-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Schrier RW. Water and sodium retention in edematous disorders: role of vasopressin and aldosterone. Am J Med. 2006;119:S47-S53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 162] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 36. | Hasking GJ, Esler MD, Jennings GL, Burton D, Johns JA, Korner PI. Norepinephrine spillover to plasma in patients with congestive heart failure: evidence of increased overall and cardiorenal sympathetic nervous activity. Circulation. 1986;73:615-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 665] [Cited by in RCA: 633] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 37. | DiBona GF, Herman PJ, Sawin LL. Neural control of renal function in edema-forming states. Am J Physiol. 1988;254:R1017-R1024. [PubMed] |
| 38. | Schrier RW, Abraham WT. Hormones and hemodynamics in heart failure. N Engl J Med. 1999;341:577-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 876] [Cited by in RCA: 814] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 39. | Schuster VL, Kokko JP, Jacobson HR. Angiotensin II directly stimulates sodium transport in rabbit proximal convoluted tubules. J Clin Invest. 1984;73:507-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 245] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 40. | Lilly LS, Dzau VJ, Williams GH, Rydstedt L, Hollenberg NK. Hyponatremia in congestive heart failure: implications for neurohumoral activation and responses to orthostasis. J Clin Endocrinol Metab. 1984;59:924-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 41. | Dzau VJ, Packer M, Lilly LS, Swartz SL, Hollenberg NK, Williams GH. Prostaglandins in severe congestive heart failure. Relation to activation of the renin--angiotensin system and hyponatremia. N Engl J Med. 1984;310:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 281] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 42. | Lee WH, Packer M. Prognostic importance of serum sodium concentration and its modification by converting-enzyme inhibition in patients with severe chronic heart failure. Circulation. 1986;73:257-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 418] [Cited by in RCA: 377] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 43. | Weber KT. Aldosterone in congestive heart failure. N Engl J Med. 2001;345:1689-1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 537] [Cited by in RCA: 495] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 44. | Brooks VL, Keil LC, Reid IA. Role of the renin-angiotensin system in the control of vasopressin secretion in conscious dogs. Circ Res. 1986;58:829-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 45. | Mitchell LD, Barron K, Brody MJ, Johnson AK. Two possible actions for circulating angiotensin II in the control of vasopressin release. Peptides. 1982;3:503-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 46. | Sica DA. Pharmacotherapy in congestive heart failure: angiotensin II and thirst: therapeutic considerations. Congest Heart Fail. 2001;7:325-328. [PubMed] |
| 47. | Schrier RW, Berl T, Anderson RJ. Osmotic and nonosmotic control of vasopressin release. Am J Physiol. 1979;236:F321-F332. [PubMed] |
| 48. | Funayama H, Nakamura T, Saito T, Yoshimura A, Saito M, Kawakami M, Ishikawa SE. Urinary excretion of aquaporin-2 water channel exaggerated dependent upon vasopressin in congestive heart failure. Kidney Int. 2004;66:1387-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 49. | Kumar S, Rubin S, Mather PJ, Whellan DJ. Hyponatremia and vasopressin antagonism in congestive heart failure. Clin Cardiol. 2007;30:546-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Nielsen S, Kwon TH, Christensen BM, Promeneur D, Frøkiaer J, Marples D. Physiology and pathophysiology of renal aquaporins. J Am Soc Nephrol. 1999;10:647-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 51. | Kwon TH, Hager H, Nejsum LN, Andersen ML, Frøkiaer J, Nielsen S. Physiology and pathophysiology of renal aquaporins. Semin Nephrol. 2001;21:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 52. | Nielsen S. Renal aquaporins: an overview. BJU Int. 2002;90 Suppl 3:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 53. | Packer M, Medina N, Yushak M. Relation between serum sodium concentration and the hemodynamic and clinical responses to converting enzyme inhibition with captopril in severe heart failure. J Am Coll Cardiol. 1984;3:1035-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 87] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 54. | Ghali JK, Tam SW. The critical link of hypervolemia and hyponatremia in heart failure and the potential role of arginine vasopressin antagonists. J Card Fail. 2010;16:419-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 55. | Anderson RJ, Chung HM, Kluge R, Schrier RW. Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med. 1985;102:164-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 395] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 56. | Lee CR, Watkins ML, Patterson JH, Gattis W, O’connor CM, Gheorghiade M, Adams KF. Vasopressin: a new target for the treatment of heart failure. Am Heart J. 2003;146:9-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 150] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 57. | Kalra PR, Anker SD, Coats AJ. Water and sodium regulation in chronic heart failure: the role of natriuretic peptides and vasopressin. Cardiovasc Res. 2001;51:495-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 72] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 58. | Isnard R, Pousset F, Trochu J, Chafirovskaïa O, Carayon A, Golmard J, Lechat P, Thomas D, Bouhour J, Komajda M. Prognostic value of neurohormonal activation and cardiopulmonary exercise testing in patients with chronic heart failure. Am J Cardiol. 2000;86:417-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 59. | Francis GS, Benedict C, Johnstone DE, Kirlin PC, Nicklas J, Liang CS, Kubo SH, Rudin-Toretsky E, Yusuf S. Comparison of neuroendocrine activation in patients with left ventricular dysfunction with and without congestive heart failure. A substudy of the Studies of Left Ventricular Dysfunction (SOLVD). Circulation. 1990;82:1724-1729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 981] [Cited by in RCA: 947] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 60. | Goldsmith SR. Congestive heart failure: potential role of arginine vasopressin antagonists in the therapy of heart failure. Congest Heart Fail. 2002;8:251-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 61. | Goldsmith SR, Francis GS, Cowley AW, Levine TB, Cohn JN. Increased plasma arginine vasopressin levels in patients with congestive heart failure. J Am Coll Cardiol. 1983;1:1385-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 365] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 62. | Goldsmith SR, Francis GS, Cowley AW. Arginine vasopressin and the renal response to water loading in congestive heart failure. Am J Cardiol. 1986;58:295-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 83] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 63. | De Luca L, Klein L, Udelson JE, Orlandi C, Sardella G, Fedele F, Gheorghiade M. Hyponatremia in patients with heart failure. Am J Cardiol. 2005;96:19L-23L. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 64. | Nickel CH, Bingisser R, Morgenthaler NG. The role of copeptin as a diagnostic and prognostic biomarker for risk stratification in the emergency department. BMC Med. 2012;10:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 65. | Balling L, Kistorp C, Schou M, Egstrup M, Gustafsson I, Goetze JP, Hildebrandt P, Gustafsson F. Plasma copeptin levels and prediction of outcome in heart failure outpatients: relation to hyponatremia and loop diuretic doses. J Card Fail. 2012;18:351-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 66. | Nigro N, Müller B, Morgenthaler N, Fluri F, Schütz P, Neidert S, Stolz D, Bingisser R, Tamm M, Christ-Crain M. The use of copeptin, the stable peptide of the vasopressin precursor, in the differential diagnosis of sodium imbalance in patients with acute diseases. Swiss Med Wkly. 2011;141:w13270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 67. | Galanth C, Hus-Citharel A, Li B, Llorens-Cortès C. Apelin in the control of body fluid homeostasis and cardiovascular functions. Curr Pharm Des. 2012;18:789-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 68. | Llorens-Cortes C, Moos F. Apelin and vasopressin: two work better than one. J Neuroendocrinol. 2012;24:1085-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 69. | Blanchard A, Steichen O, De Mota N, Curis E, Gauci C, Frank M, Wuerzner G, Kamenicky P, Passeron A, Azizi M. An abnormal apelin/vasopressin balance may contribute to water retention in patients with the syndrome of inappropriate antidiuretic hormone (SIADH) and heart failure. J Clin Endocrinol Metab. 2013;98:2084-2089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 70. | Liamis G, Milionis H, Elisaf M. A review of drug-induced hyponatremia. Am J Kidney Dis. 2008;52:144-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 300] [Article Influence: 17.6] [Reference Citation Analysis (2)] |
| 71. | Chow KM, Szeto CC, Wong TY, Leung CB, Li PK. Risk factors for thiazide-induced hyponatraemia. QJM. 2003;96:911-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 98] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 72. | Spital A. Diuretic-induced hyponatremia. Am J Nephrol. 1999;19:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 77] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 73. | Miltiadous G, Mikhailidis DP, Elisaf M. Acid-base and electrolyte abnormalities observed in patients receiving cardiovascular drugs. J Cardiovasc Pharmacol Ther. 2003;8:267-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 74. | Liamis G, Christidis D, Alexandridis G, Bairaktari E, Madias NE, Elisaf M. Uric acid homeostasis in the evaluation of diuretic-induced hyponatremia. J Investig Med. 2007;55:36-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 75. | van Assen S, Mudde AH. Severe hyponatraemia in an amiloride/hydrochlorothiazide-treated patient. Neth J Med. 1999;54:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 76. | Fidler HM, Goldman J, Bielawska CA, Rai GS, Hoffbrand BI. A study of plasma sodium levels in elderly people taking amiloride or triamterene in combination with hydrochlorothiazide. Postgrad Med J. 1993;69:797-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 77. | Strykers PH, Stern RS, Morse BM. Hyponatremia induced by a combination of amiloride and hydrochlorothiazide. JAMA. 1984;252:389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 78. | Hypokalaemia and hyponatraemia due to indapamide. Prescrire Int. 2002;11:183. [PubMed] |
| 79. | Chapman MD, Hanrahan R, McEwen J, Marley JE. Hyponatraemia and hypokalaemia due to indapamide. Med J Aust. 2002;176:219-221. [PubMed] |
| 80. | Mathew TH, Boyd IW, Rohan AP. Hyponatraemia due to the combination of hydrochlorothiazide and amiloride (Moduretic): Australian spontaneous reports 1977-1988. Med J Aust. 1990;152:308-309. [PubMed] |
| 81. | Chin MH, Goldman L. Correlates of major complications or death in patients admitted to the hospital with congestive heart failure. Arch Intern Med. 1996;156:1814-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 104] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 82. | Chen MC, Chang HW, Cheng CI, Chen YH, Chai HT. Risk stratification of in-hospital mortality in patients hospitalized for chronic congestive heart failure secondary to non-ischemic cardiomyopathy. Cardiology. 2003;100:136-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 83. | Felker GM, Leimberger JD, Califf RM, Cuffe MS, Massie BM, Adams KF, Gheorghiade M, O’Connor CM. Risk stratification after hospitalization for decompensated heart failure. J Card Fail. 2004;10:460-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 243] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 84. | Lee DS, Austin PC, Rouleau JL, Liu PP, Naimark D, Tu JV. Predicting mortality among patients hospitalized for heart failure: derivation and validation of a clinical model. JAMA. 2003;290:2581-2587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 980] [Cited by in RCA: 1023] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 85. | Packer M, Lee WH, Kessler PD, Medina N, Yushak M, Gottlieb SS. Identification of hyponatremia as a risk factor for the development of functional renal insufficiency during converting enzyme inhibition in severe chronic heart failure. J Am Coll Cardiol. 1987;10:837-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 86. | Velavan P, Khan NK, Goode K, Rigby AS, Loh PH, Komajda M, Follath F, Swedberg K, Madeira H, Cleland JG. Predictors of short term mortality in heart failure - insights from the Euro Heart Failure survey. Int J Cardiol. 2010;138:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 87. | Wong PS, Davidsson GK, Timeyin J, Warren A, Watson DJ, Vincent R, Davidson C. Heart failure in patients admitted to hospital: mortality is still high. Eur J Intern Med. 2002;13:304-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 88. | Bettari L, Fiuzat M, Shaw LK, Wojdyla DM, Metra M, Felker GM, O’Connor CM. Hyponatremia and long-term outcomes in chronic heart failure--an observational study from the Duke Databank for Cardiovascular Diseases. J Card Fail. 2012;18:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 89. | Schou M, Valeur N, Torp-Pedersen C, Gustafsson F, Køber L. Plasma sodium and mortality risk in patients with myocardial infarction and a low LVEF. Eur J Clin Invest. 2011;41:1237-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 90. | Gheorghiade M, Rossi JS, Cotts W, Shin DD, Hellkamp AS, Piña IL, Fonarow GC, DeMarco T, Pauly DF, Rogers J. Characterization and prognostic value of persistent hyponatremia in patients with severe heart failure in the ESCAPE Trial. Arch Intern Med. 2007;167:1998-2005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 310] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 91. | Baldasseroni S, Urso R, Orso F, Bianchini BP, Carbonieri E, Cirò A, Gonzini L, Leonardi G, Marchionni N, Maggioni AP. Relation between serum sodium levels and prognosis in outpatients with chronic heart failure: neutral effect of treatment with beta-blockers and angiotensin-converting enzyme inhibitors: data from the Italian Network on Congestive Heart Failure (IN-CHF database). J Cardiovasc Med (Hagerstown). 2011;12:723-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 92. | Sato N, Gheorghiade M, Kajimoto K, Munakata R, Minami Y, Mizuno M, Aokage T, Asai K, Sakata Y, Yumino D. Hyponatremia and in-hospital mortality in patients admitted for heart failure (from the ATTEND registry). Am J Cardiol. 2013;111:1019-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 93. | Lee SE, Choi DJ, Yoon CH, Oh IY, Jeon ES, Kim JJ, Cho MC, Chae SC, Ryu KH, Oh BH. Improvement of hyponatraemia during hospitalisation for acute heart failure is not associated with improvement of prognosis: an analysis from the Korean Heart Failure (KorHF) registry. Heart. 2012;98:1798-1804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 94. | Kearney MT, Fox KA, Lee AJ, Brooksby WP, Shah AM, Flapan A, Prescott RJ, Andrews R, Batin PD, Eckberg DL. Predicting sudden death in patients with mild to moderate chronic heart failure. Heart. 2004;90:1137-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 95. | Rusinaru D, Tribouilloy C, Berry C, Richards AM, Whalley GA, Earle N, Poppe KK, Guazzi M, Macin SM, Komajda M. Relationship of serum sodium concentration to mortality in a wide spectrum of heart failure patients with preserved and with reduced ejection fraction: an individual patient data meta-analysis(†): Meta-Analysis Global Group in Chronic heart failure (MAGGIC). Eur J Heart Fail. 2012;14:1139-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 96. | Deubner N, Berliner D, Frey A, Güder G, Brenner S, Fenske W, Allolio B, Ertl G, Angermann CE, Störk S. Dysnatraemia in heart failure. Eur J Heart Fail. 2012;14:1147-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 97. | Aaronson KD, Schwartz JS, Chen TM, Wong KL, Goin JE, Mancini DM. Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation. 1997;95:2660-2667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 770] [Cited by in RCA: 788] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 98. | Kearney MT, Nolan J, Lee AJ, Brooksby PW, Prescott R, Shah AM, Zaman AG, Eckberg DL, Lindsay HS, Batin PD. A prognostic index to predict long-term mortality in patients with mild to moderate chronic heart failure stabilised on angiotensin converting enzyme inhibitors. Eur J Heart Fail. 2003;5:489-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 99. | Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD, Cropp AB, Anand I, Maggioni A, Burton P, Sullivan MD. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation. 2006;113:1424-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1435] [Cited by in RCA: 1572] [Article Influence: 82.7] [Reference Citation Analysis (0)] |
| 100. | Vazquez R, Bayes-Genis A, Cygankiewicz I, Pascual-Figal D, Grigorian-Shamagian L, Pavon R, Gonzalez-Juanatey JR, Cubero JM, Pastor L, Ordonez-Llanos J. The MUSIC Risk score: a simple method for predicting mortality in ambulatory patients with chronic heart failure. Eur Heart J. 2009;30:1088-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 152] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 101. | O’Connor CM, Hasselblad V, Mehta RH, Tasissa G, Califf RM, Fiuzat M, Rogers JG, Leier CV, Stevenson LW. Triage after hospitalization with advanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J Am Coll Cardiol. 2010;55:872-878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 199] [Cited by in RCA: 227] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 102. | Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1611] [Cited by in RCA: 1581] [Article Influence: 52.7] [Reference Citation Analysis (0)] |
| 103. | Krumholz HM, Chen YT, Bradford WD, Cerese J. Variations in and correlates of length of stay in academic hospitals among patients with heart failure resulting from systolic dysfunction. Am J Manag Care. 1999;5:715-723. [PubMed] |
| 104. | Amin A, Deitelzweig S, Christian R, Friend K, Lin J, Lowe TJ. Healthcare resource burden associated with hyponatremia among patients hospitalized for heart failure in the US. J Med Econ. 2013;16:415-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 105. | Konishi M, Haraguchi G, Ohigashi H, Sasaoka T, Yoshikawa S, Inagaki H, Ashikaga T, Isobe M. Progression of hyponatremia is associated with increased cardiac mortality in patients hospitalized for acute decompensated heart failure. J Card Fail. 2012;18:620-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 106. | Callahan MA, Do HT, Caplan DW, Yoon-Flannery K. Economic impact of hyponatremia in hospitalized patients: a retrospective cohort study. Postgrad Med. 2009;121:186-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 107. | Shea AM, Hammill BG, Curtis LH, Szczech LA, Schulman KA. Medical costs of abnormal serum sodium levels. J Am Soc Nephrol. 2008;19:764-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 108. | Zilberberg MD, Exuzides A, Spalding J, Foreman A, Jones AG, Colby C, Shorr AF. Epidemiology, clinical and economic outcomes of admission hyponatremia among hospitalized patients. Curr Med Res Opin. 2008;24:1601-1608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 131] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 109. | Tada Y, Nakamura T, Funayama H, Sugawara Y, Ako J, Ishikawa SE, Momomura S. Early development of hyponatremia implicates short- and long-term outcomes in ST-elevation acute myocardial infarction. Circ J. 2011;75:1927-1933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 110. | Tang Q, Hua Q. Relationship between hyponatremia and in-hospital outcomes in Chinese patients with ST-elevation myocardial infarction. Intern Med. 2011;50:969-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 111. | Maisel A, Xue Y, Shah K, Mueller C, Nowak R, Peacock WF, Ponikowski P, Mockel M, Hogan C, Wu AH. Increased 90-day mortality in patients with acute heart failure with elevated copeptin: secondary results from the Biomarkers in Acute Heart Failure (BACH) study. Circ Heart Fail. 2011;4:613-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 112. | Miller WL, Grill DE, Struck J, Jaffe AS. Association of hyponatremia and elevated copeptin with death and need for transplantation in ambulatory patients with chronic heart failure. Am J Cardiol. 2013;111:880-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 113. | Goh KP. Management of hyponatremia. Am Fam Physician. 2004;69:2387-2394. [PubMed] |
| 114. | Fraser CL, Arieff AI. Epidemiology, pathophysiology, and management of hyponatremic encephalopathy. Am J Med. 1997;102:67-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 161] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 115. | Assadi F. Hyponatremia: a problem-solving approach to clinical cases. J Nephrol. 2012;25:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 116. | Pfennig CL, Slovis CM. Sodium disorders in the emergency department: a review of hyponatremia and hypernatremia. Emerg Med Pract. 2012;14:1-26. [PubMed] |
| 117. | Karp BI, Laureno R. Pontine and extrapontine myelinolysis: a neurologic disorder following rapid correction of hyponatremia. Medicine (Baltimore). 1993;72:359-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 117] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 118. | Kumar S, Fowler M, Gonzalez-Toledo E, Jaffe SL. Central pontine myelinolysis, an update. Neurol Res. 2006;28:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 119. | Laureno R, Karp BI. Myelinolysis after correction of hyponatremia. Ann Intern Med. 1997;126:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 210] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 120. | Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 2004;75 Suppl 3:iii22-iii28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 209] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 121. | Graff-Radford J, Fugate JE, Kaufmann TJ, Mandrekar JN, Rabinstein AA. Clinical and radiologic correlations of central pontine myelinolysis syndrome. Mayo Clin Proc. 2011;86:1063-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 122. | Hart BL, Eaton RP. Images in clinical medicine. Osmotic myelinolysis. N Engl J Med. 1995;333:1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 123. | Albert NM, Nutter B, Forney J, Slifcak E, Tang WH. A randomized controlled pilot study of outcomes of strict allowance of fluid therapy in hyponatremic heart failure (SALT-HF). J Card Fail. 2013;19:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 124. | Dzau VJ, Hollenberg NK. Renal response to captopril in severe heart failure: role of furosemide in natriuresis and reversal of hyponatremia. Ann Intern Med. 1984;100:777-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 90] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 125. | Elisaf M, Theodorou J, Pappas C, Siamopoulos K. Successful treatment of hyponatremia with angiotensin-converting enzyme inhibitors in patients with congestive heart failure. Cardiology. 1995;86:477-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 126. | Paterna S, Di Pasquale P, Parrinello G, Amato P, Cardinale A, Follone G, Giubilato A, Licata G. Effects of high-dose furosemide and small-volume hypertonic saline solution infusion in comparison with a high dose of furosemide as a bolus, in refractory congestive heart failure. Eur J Heart Fail. 2000;2:305-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 90] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 127. | Licata G, Di Pasquale P, Parrinello G, Cardinale A, Scandurra A, Follone G, Argano C, Tuttolomondo A, Paterna S. Effects of high-dose furosemide and small-volume hypertonic saline solution infusion in comparison with a high dose of furosemide as bolus in refractory congestive heart failure: long-term effects. Am Heart J. 2003;145:459-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 183] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 128. | Thibonnier M, Conarty DM, Preston JA, Wilkins PL, Berti-Mattera LN, Mattera R. Molecular pharmacology of human vasopressin receptors. Adv Exp Med Biol. 1998;449:251-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 79] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 129. | Wallace AW, Tunin CM, Shoukas AA. Effects of vasopressin on pulmonary and systemic vascular mechanics. Am J Physiol. 1989;257:H1228-H1234. [PubMed] |
| 130. | Xu YJ, Gopalakrishnan V. Vasopressin increases cytosolic free [Ca2+] in the neonatal rat cardiomyocyte. Evidence for V1 subtype receptors. Circ Res. 1991;69:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 67] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 131. | Goldsmith SR. The role of vasopressin in congestive heart failure. Cleve Clin J Med. 2006;73 Suppl 3:S19-S23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 132. | Nakamura Y, Haneda T, Osaki J, Miyata S, Kikuchi K. Hypertrophic growth of cultured neonatal rat heart cells mediated by vasopressin V(1A) receptor. Eur J Pharmacol. 2000;391:39-48. [PubMed] |
| 133. | Fukuzawa J, Haneda T, Kikuchi K. Arginine vasopressin increases the rate of protein synthesis in isolated perfused adult rat heart via the V1 receptor. Mol Cell Biochem. 1999;195:93-98. [PubMed] |
| 134. | Thibonnier M, Coles P, Thibonnier A, Shoham M. The basic and clinical pharmacology of nonpeptide vasopressin receptor antagonists. Annu Rev Pharmacol Toxicol. 2001;41:175-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 110] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 135. | Howl J, Ismail T, Strain AJ, Kirk CJ, Anderson D, Wheatley M. Characterization of the human liver vasopressin receptor. Profound differences between human and rat vasopressin-receptor-mediated responses suggest only a minor role for vasopressin in regulating human hepatic function. Biochem J. 1991;276:189-195. [PubMed] |
| 136. | Tanoue A, Ito S, Honda K, Oshikawa S, Kitagawa Y, Koshimizu TA, Mori T, Tsujimoto G. The vasopressin V1b receptor critically regulates hypothalamic-pituitary-adrenal axis activity under both stress and resting conditions. J Clin Invest. 2004;113:302-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 137. | Nakamura K, Aoyagi T, Hiroyama M, Kusakawa S, Mizutani R, Sanbe A, Yamauchi J, Kamohara M, Momose K, Tanoue A. Both V(1A) and V(1B) vasopressin receptors deficiency result in impaired glucose tolerance. Eur J Pharmacol. 2009;613:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 138. | Xu DL, Martin PY, Ohara M, St John J, Pattison T, Meng X, Morris K, Kim JK, Schrier RW. Upregulation of aquaporin-2 water channel expression in chronic heart failure rat. J Clin Invest. 1997;99:1500-1505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 215] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 139. | Schrier RW, Sharma S, Shchekochikhin D. Hyponatraemia: more than just a marker of disease severity? Nat Rev Nephrol. 2013;9:37-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 140. | Berl T, Quittnat-Pelletier F, Verbalis JG, Schrier RW, Bichet DG, Ouyang J, Czerwiec FS. Oral tolvaptan is safe and effective in chronic hyponatremia. J Am Soc Nephrol. 2010;21:705-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 239] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 141. | Udelson JE, Orlandi C, Ouyang J, Krasa H, Zimmer CA, Frivold G, Haught WH, Meymandi S, Macarie C, Raef D. Acute hemodynamic effects of tolvaptan, a vasopressin V2 receptor blocker, in patients with symptomatic heart failure and systolic dysfunction: an international, multicenter, randomized, placebo-controlled trial. J Am Coll Cardiol. 2008;52:1540-1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 131] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 142. | Watanabe K, Dohi K, Sugimoto T, Yamada T, Sato Y, Ichikawa K, Sugiura E, Kumagai N, Nakamori S, Nakajima H. Short-term effects of low-dose tolvaptan on hemodynamic parameters in patients with chronic heart failure. J Cardiol. 2012;60:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 143. | Matsuzaki M, Hori M, Izumi T, Fukunami M. Efficacy and safety of tolvaptan in heart failure patients with volume overload despite the standard treatment with conventional diuretics: a phase III, randomized, double-blind, placebo-controlled study (QUEST study). Cardiovasc Drugs Ther. 2011;25 Suppl 1:S33-S45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 144. | Fukunami M, Matsuzaki M, Hori M, Izumi T. Efficacy and safety of tolvaptan in heart failure patients with sustained volume overload despite the use of conventional diuretics: a phase III open-label study. Cardiovasc Drugs Ther. 2011;25 Suppl 1:S47-S56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 145. | Gheorghiade M, Niazi I, Ouyang J, Czerwiec F, Kambayashi J, Zampino M, Orlandi C. Vasopressin V2-receptor blockade with tolvaptan in patients with chronic heart failure: results from a double-blind, randomized trial. Circulation. 2003;107:2690-2696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 312] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 146. | Gheorghiade M, Gattis WA, O’Connor CM, Adams KF, Elkayam U, Barbagelata A, Ghali JK, Benza RL, McGrew FA, Klapholz M. Effects of tolvaptan, a vasopressin antagonist, in patients hospitalized with worsening heart failure: a randomized controlled trial. JAMA. 2004;291:1963-1971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 482] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 147. | Rossi J, Bayram M, Udelson JE, Lloyd-Jones D, Adams KF, Oconnor CM, Stough WG, Ouyang J, Shin DD, Orlandi C. Improvement in hyponatremia during hospitalization for worsening heart failure is associated with improved outcomes: insights from the Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Chronic Heart Failure (ACTIV in CHF) trial. Acute Card Care. 2007;9:82-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 113] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 148. | Udelson JE, McGrew FA, Flores E, Ibrahim H, Katz S, Koshkarian G, O’Brien T, Kronenberg MW, Zimmer C, Orlandi C. Multicenter, randomized, double-blind, placebo-controlled study on the effect of oral tolvaptan on left ventricular dilation and function in patients with heart failure and systolic dysfunction. J Am Coll Cardiol. 2007;49:2151-2159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 127] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 149. | Matsue Y, Suzuki M, Seya M, Iwatsuka R, Mizukami A, Nagahori W, Ohno M, Matsumura A, Hashimoto Y. Tolvaptan reduces the risk of worsening renal function in patients with acute decompensated heart failure in high-risk population. J Cardiol. 2013;61:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 78] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 150. | Gheorghiade M, Konstam MA, Burnett JC, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J. Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials. JAMA. 2007;297:1332-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 655] [Cited by in RCA: 690] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 151. | Konstam MA, Gheorghiade M, Burnett JC, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial. JAMA. 2007;297:1319-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1225] [Cited by in RCA: 1232] [Article Influence: 68.4] [Reference Citation Analysis (0)] |
| 152. | Hauptman PJ, Burnett J, Gheorghiade M, Grinfeld L, Konstam MA, Kostic D, Krasa HB, Maggioni A, Ouyang J, Swedberg K. Clinical course of patients with hyponatremia and decompensated systolic heart failure and the effect of vasopressin receptor antagonism with tolvaptan. J Card Fail. 2013;19:390-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 153. | Regen RB, Gonzalez A, Zawodniak K, Leonard D, Quigley R, Barnes AP, Koch JD. Tolvaptan increases serum sodium in pediatric patients with heart failure. Pediatr Cardiol. 2013;34:1463-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 154. | Ghali JK, Zmily HD, Farah JO, Daifallah S. Lixivaptan, a non-peptide vasopressin V2 receptor antagonist for the potential oral treatment of hyponatremia. IDrugs. 2010;13:782-792. [PubMed] |
| 155. | Abraham WT, Shamshirsaz AA, McFann K, Oren RM, Schrier RW. Aquaretic effect of lixivaptan, an oral, non-peptide, selective V2 receptor vasopressin antagonist, in New York Heart Association functional class II and III chronic heart failure patients. J Am Coll Cardiol. 2006;47:1615-1621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 156. | Ghali JK, Orlandi C, Abraham WT. The efficacy and safety of lixivaptan in outpatients with heart failure and volume overload: results of a multicentre, randomized, double-blind, placebo-controlled, parallel-group study. Eur J Heart Fail. 2012;14:642-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 157. | Abraham WT, Aranda JM, Boehmer JP, Elkayam U, Gilbert EM, Gottlieb SS, Hasenfuss G, Kukin M, Lowes BD, O’Connell JB. Rationale and design of the treatment of hyponatremia based on lixivaptan in NYHA class III/IV cardiac patient evaluation (THE BALANCE) study. Clin Transl Sci. 2010;3:249-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 158. | Ali F, Raufi MA, Washington B, Ghali JK. Conivaptan: a dual vasopressin receptor v1a/v2 antagonist [corrected]. Cardiovasc Drug Rev. 2007;25:261-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 159. | Yatsu T, Tomura Y, Tahara A, Wada K, Kusayama T, Tsukada J, Tokioka T, Uchida W, Inagaki O, Iizumi Y. Cardiovascular and renal effects of conivaptan hydrochloride (YM087), a vasopressin V1A and V2 receptor antagonist, in dogs with pacing-induced congestive heart failure. Eur J Pharmacol. 1999;376:239-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 160. | Verbalis JG, Zeltser D, Smith N, Barve A, Andoh M. Assessment of the efficacy and safety of intravenous conivaptan in patients with euvolaemic hyponatraemia: subgroup analysis of a randomized, controlled study. Clin Endocrinol (Oxf). 2008;69:159-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 161. | Chatterjee K. Hyponatremia in heart failure. J Intensive Care Med. 2009;24:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 162. | Mao ZL, Stalker D, Keirns J. Pharmacokinetics of conivaptan hydrochloride, a vasopressin V(1A)/V(2)-receptor antagonist, in patients with euvolemic or hypervolemic hyponatremia and with or without congestive heart failure from a prospective, 4-day open-label study. Clin Ther. 2009;31:1542-1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 163. | Zeltser D, Rosansky S, van Rensburg H, Verbalis JG, Smith N. Assessment of the efficacy and safety of intravenous conivaptan in euvolemic and hypervolemic hyponatremia. Am J Nephrol. 2007;27:447-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 140] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 164. | Annane D, Decaux G, Smith N. Efficacy and safety of oral conivaptan, a vasopressin-receptor antagonist, evaluated in a randomized, controlled trial in patients with euvolemic or hypervolemic hyponatremia. Am J Med Sci. 2009;337:28-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 165. | Ghali JK, Koren MJ, Taylor JR, Brooks-Asplund E, Fan K, Long WA, Smith N. Efficacy and safety of oral conivaptan: a V1A/V2 vasopressin receptor antagonist, assessed in a randomized, placebo-controlled trial in patients with euvolemic or hypervolemic hyponatremia. J Clin Endocrinol Metab. 2006;91:2145-2152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 171] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 166. | Udelson JE, Smith WB, Hendrix GH, Painchaud CA, Ghazzi M, Thomas I, Ghali JK, Selaru P, Chanoine F, Pressler ML. Acute hemodynamic effects of conivaptan, a dual V(1A) and V(2) vasopressin receptor antagonist, in patients with advanced heart failure. Circulation. 2001;104:2417-2423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 241] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 167. | Goldsmith SR, Elkayam U, Haught WH, Barve A, He W. Efficacy and safety of the vasopressin V1A/V2-receptor antagonist conivaptan in acute decompensated heart failure: a dose-ranging pilot study. J Card Fail. 2008;14:641-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 168. | Goldsmith SR, Gilbertson DT, Mackedanz SA, Swan SK. Renal effects of conivaptan, furosemide, and the combination in patients with chronic heart failure. J Card Fail. 2011;17:982-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 169. | Available from: http://www.cbg-meb.nl/NR/rdonlyres/BC53C10C-62AF-44B3-A43A-CE7A39A231B4/0/120326DHPCSamscaEN.pdf. Accessed at 08-06-2013. |
| 170. | Torres VE, Chapman AB, Devuyst O, Gansevoort RT, Grantham JJ, Higashihara E, Perrone RD, Krasa HB, Ouyang J, Czerwiec FS. Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2012;367:2407-2418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1179] [Cited by in RCA: 1145] [Article Influence: 88.1] [Reference Citation Analysis (0)] |