Published online Jul 26, 2013. doi: 10.4330/wjc.v5.i7.258
Revised: June 17, 2013
Accepted: July 4, 2013
Published online: July 26, 2013
Processing time: 135 Days and 18 Hours
Patients with chronic aortic dissections are at high risk of catheter-induced complications. We report a 41-year-old patient with a type B aortic dissection (Stanford) who underwent successful three-vessel percutaneous coronary intervention via the right radial artery approach following a non-ST elevation myocardial infarction. The patient remained asymptomatic at 6 mo follow-up. Trans-radial approach for coronary interventions can be used safely in patients with Stanford type B aortic dissection without increasing the risk of procedure- related complications in this high-risk group of patients.
Core tip: The case highlights the use of a transradial approach to carry out multivessel percutaneous coronary intervention (PCI) in a patient with a chronic aortic dissection. There is a paucity of literature on this subject. This case discusses the possible mechanisms of dissection propagation with a transfemoral approach and highlights the need for training in both approaches. Decision making in choosing arterial access for PCI in patients with aortic dissection.
- Citation: Hamid T, Choudhury TR, Fraser D. Multi-vessel percutaneous coronary intervention in a patient with a type B aortic dissection-transradial or transfemoral? World J Cardiol 2013; 5(7): 258-260
- URL: https://www.wjgnet.com/1949-8462/full/v5/i7/258.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i7.258
A 41-year-old male patient was admitted with cardiac chest pain and elevated troponin. His 12 lead electrocardiogram showed widespread T wave inversion. A diagnosis of non-ST elevation myocardial infarction (NSTEMI) was made. He was known to have a chronic Stanford type B aortic dissection, extending in the descending aorta from beyond the left subclavian artery down to the abdominal aorta, and was under regular medical surveillance.
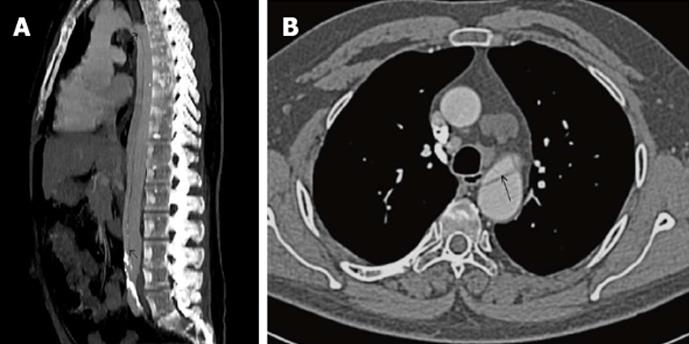
His cardiovascular risk factors included hypertension, hypercholesterolemia and smoking. He had been given standard NSTEMI treatment with dual antiplatelets (aspirin 300 mg and clopidogrel 300 mg) and low-molecular weight heparin (weight adjusted) at admission. While an inpatient, he had further cardiac chest pains and therefore, was transferred to the catheter-lab for cardiac catheterisation. Prior to the procedure, he received further loading with clopidogrel 300 mg. During the procedure, he received weight adjusted unfractionated heparin intravenously. The decision to use standard acute coronary syndrome (ACS) peri-procedural therapy was made in view of the fact that the patient had been stable from his chronic aortic dissection and that his recent electronic computer X-ray tomography technique (CT) of the aorta showed no extension of his dissection (Figure 1). Informed consent was obtained prior to the percutaneous coronary intervention.
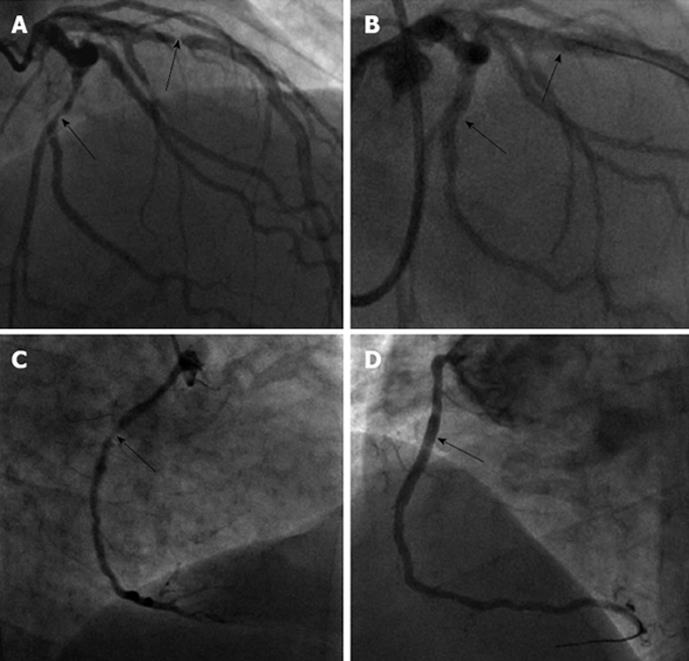
The coronary diagnostic procedure was performed via the right radial artery approach. Five French JR4® and JL 3.5® diagnostic catheters were used for the right and left coronary systems respectively. This confirmed a normal left main stem. The left anterior descending (LAD), left circumflex (LCx) and right coronary artery (RCA) had severe mid-vessel lesions (Figure 2A and C). Due to the complexity of the case, it was decided to treat all three lesions at the same procedure.
A Medtronic Launcher EBU 5.0 (6F)® (Medtronic) guide catheter was used to cannulate the left system. Two 0.014” BMW® guidewires (Abbott Vascular) were advanced to the distal LAD and LCx. The lesion in the LAD was directly stented using a 4.0 mm × 15 mm Resolute Integrity® drug eluting stent (DES) (Medtronic). The LCx lesion was pre-dilated using a 2 mm × 15 mm Maverick Balloon® (Boston Scientific), followed by a 2.75 mm × 22 mm Resolute Integrity® DES.
An Amplatz (AL2) guide catheter was used to cannulate the RCA. A 0.014” BMW® guidewire was advanced to the distal RCA. The lesion was pre-dilated with a 2.0 mm × 15 mm Maverick Balloon® followed by a 3.0 mm × 22 mm Resolute Integrity® DES. Excellent final angiographic results were obtained (Figure 2B and D) A Terumo TR band® (Terumo) was deployed to the radial access site at the end of procedure. There were no peri or post procedure complications. A total of 300 mL contrast (Visipaque®) and 7000 units heparin were given. His repeat blood tests including haemoglobin, urea, creatinine and electrolytes were normal post-procedure. The patient made an uneventful recovery and was discharged a few days later on dual antiplatelets (aspirin 75 mg and clopidogrel 75 mg daily) and standard secondary prevention. He was instructed to continue on dual antiplatelets for 1 year and aspirin for lifelong thereafter.
Aortic dissection can be classified according to the location of the dissection and the relevance to patient management. The commonly used Stanford classification distinguishes aortic dissections by whether the ascending aorta is involved (type A) or not (type B)[1]. The incidence of aortic dissection in the general population is approximately 2.6-3.5 per 100000 person-years[2,3]. In a study by Islamoğlu et al[4], 11 of 76 patients with aortic dissection (acute and chronic) ie 14.5% had concomitant coronary artery disease. However, none of the chronic type B dissection patients who underwent coronary angiography had coronary artery disease. CT angiography allows the fast and reliable detection of aortic dissections and delineation of the dissection flap anatomy.
Since the introduction of trans-radial coronary angioplasty[5], procedural success rates have evolved remarkably and complex coronary artery lesions can be treated with minimal complications. Our patient had a chronic Stanford type B aortic dissection. A transfemoral approach would carry a high risk of complicating the existing dissection. Hildick-Smith et al[6] published a large case series looking at transradial coronary angiography in patients with contraindications to a femoral approach. Of 500 patients in that series, 10 patients had aortic dissection and had a transradial approach. However, there is no series looking solely at patients with aortic dissection and the best approach for PCI. Furthermore, there is a paucity of literature discussing the possible mechanisms of catheter-related complications in relation to aortic dissections in cases similar to ours. Mechanisms would include entry of the catheter tip into the false lumen. Using a femoral approach, this could happen at the exit site of the existing dissection. Continued advancement of the catheter would then risk propagation of the dissection into the ascending aorta as well as rupture of the vessel. Additional risks would include catheter entry into the false lumen via puncturing the wall between the true and false lumens. In our patient, to avoid these potential complications, we safely used the right trans-radial approach for three-vessel PCI without any procedural complications. This would appear to be the ideal approach in patients with Stanford type B aortic dissections as it avoids the descending aorta and thus, the potential to worsen an existing dissection. However, a radial approach is not without risk of aortic dissections. Indeed, there are case reports of iatrogenic aortic dissections due to aggressive catheter manipulation during PCI via a radial approach[7]. Furthermore, in patients with aberrant right subclavian artery (aretria lusoria), PCI via a right radial approach can be extremely difficult and there are reports of iatrogenic aortic dissections during such procedures[8].
This case highlights the importance of choosing the right access approach in patients with a complicated background like ours. It also highlights the importance of training interventionalists in both the transradial and tranfemoral approaches as each has its own merits and is sometimes the only feasible approach in certain patient groups.
In conclusion, trans-radial approach for coronary interventions can be used safely in patients with Stanford type B aortic dissection without increasing the risk of procedure-related complications in this high-risk group of patients.
P- Reviewer Vermeersch P S- Editor Gou SX L- Editor A E- Editor Lu YJ
| 1. | Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg. 1970;10:237-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 786] [Cited by in RCA: 724] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 2. | Mészáros I, Mórocz J, Szlávi J, Schmidt J, Tornóci L, Nagy L, Szép L. Epidemiology and clinicopathology of aortic dissection. Chest. 2000;117:1271-1278. [PubMed] |
| 3. | Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, Evangelista A, Fattori R, Suzuki T, Oh JK. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2417] [Cited by in RCA: 2332] [Article Influence: 93.3] [Reference Citation Analysis (0)] |
| 4. | Islamoğlu F, Atay Y, Can L, Kara E, Ozbaran M, Yüksel M, Büket S. Diagnosis and treatment of concomitant aortic and coronary disease: a retrospective study and brief review. Tex Heart Inst J. 1999;26:182-188. [PubMed] |
| 5. | Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29:1269-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 673] [Cited by in RCA: 628] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 6. | Hildick-Smith DJ, Walsh JT, Lowe MD, Shapiro LM, Petch MC. Transradial coronary angiography in patients with contraindications to the femoral approach: an analysis of 500 cases. Catheter Cardiovasc Interv. 2004;61:60-66. [PubMed] |
| 7. | Noguchi K, Hori D, Nomura Y, Tanaka H. Iatrogenic Acute Aortic Dissection during Percutaneous Coronary Intervention for Acute Myocardial Infarction. Ann Vasc Dis. 2012;5:78-81. [PubMed] |
| 8. | Huang IL, Hwang HR, Li SC, Chen CK, Liu CP, Wu MT. Dissection of arteria lusoria by transradial coronary catheterization: a rare complication evaluated by multidetector CT. J Chin Med Assoc. 2009;72:379-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |