Published online Jun 26, 2013. doi: 10.4330/wjc.v5.i6.207
Revised: April 19, 2013
Accepted: May 17, 2013
Published online: June 26, 2013
Processing time: 121 Days and 2.8 Hours
We present a rare case of Twiddler’s syndrome diagnosed in an asymptomatic patient on a routine follow up. This case reiterates the need for frequent monitoring of the implanted device. In addition, it was detected 4 years after implantation of an automatic implantable cardioverter defibrillator. This late representation is extremely uncommon.
Core tip: Our case points out few unique points to be remembered in regards to Twiddler’s syndrome: (1) Twiddler’s syndrome can present without any symptoms. Our case was diagnosed with the help of gradually increasing lead impedance. Ours is the first reported case of such a unique presentation; (2) Twiddler’s syndrome, although more common in first few months of implantation, can present very late; and (3) frequent monitoring of permanent pacemaker/automatic implantable cardioverter defibrillator is always needed.
- Citation: Parikh V, Barsoum EA, Morcus R, Azab B, Lafferty J, Kohn J. Unique presentation of Twiddler’s syndrome. World J Cardiol 2013; 5(6): 207-209
- URL: https://www.wjgnet.com/1949-8462/full/v5/i6/207.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i6.207
Twiddler’s syndrome is defined as permanent malfunction of automatic implantable cardioverter defibrillator (AICD) or permanent pacemaker due to conscious or subconscious manipulation of pulse generator within subcutaneous pocket, resulting in dislodgement and/or retraction of leads, leading to loss of device function[1]. First described in 1968, it is one of the rare complications involving a device[1]. Some of the predisposing factors such as female gender, old age, obesity, weight loss, excessive movements of the upper limbs, active manipulation of the generator and large size pockets have been identified[2-5]. However, the exact mechanism behind it remains elusive.
The benefit of the AICD has been established in the primary and secondary prevention of ventricular arrhythmias and sudden cardiac death. Regular monitoring of the AICD is required to ensure normal function. Twiddler’s syndrome, in which the pacemaker is rotated manually repeatedly, has been described as a pacemaker complication by Bayliss et al[1]. The syndrome has been described in the AICD population as well, and has been implicated in device failure leading to various clinical manifestations including sudden cardiac death[6,7]. However, it presented in a unique manner in our case.
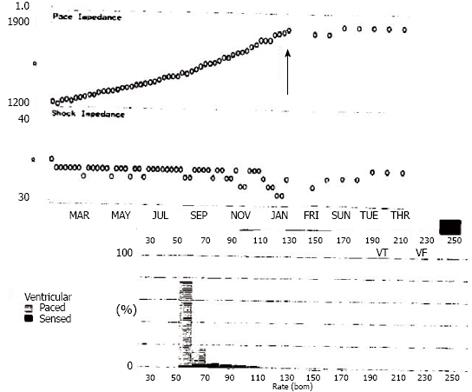
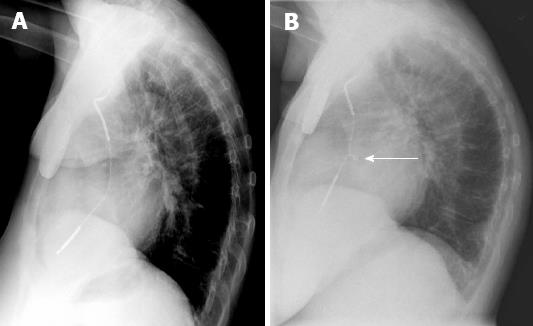
A seventy-three years old woman with history of hypertension, atrial fibrillation and non ischemic cardiomyopathy status post AICD placement for primary prevention 4 years ago, presented to office for routine check-up. Patient denied any palpitation, shortness of breath, fatigue or any other complaints at presentation. Electrocardiogram showed 100% demand ventricular pacing. On routine AICD interrogation, gradually increasing pacing impedance of right ventricular (RV) pace/sense lead over 8 mo, reaching a maximum of 1862 ohms, was found (Figure 1). RV pacing and sensing threshold, and shock parameters were unchanged from last interrogation. A chest X-ray revealed twirling of the ventricular lead (Figure 2). The decision was made to perform a lead revision.
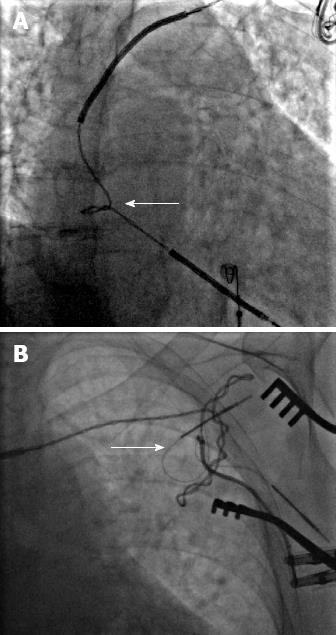
During the procedure, fluoroscopy of the leads confirmed a twist in the lead in the right atrio-ventricular junction. Additionally, there was also significant twisting in the shoulder area, partly intravascular and partly in the pocket (Figure 3). The ventricular lead was tested and showed impedance > 2000 ohms. Due to extensive fibrosis, it was impossible to extract the lead and decision was made to abandon it. A new ventricular lead was placed under fluoroscopic guidance with satisfactory parameters (Figure 4). Since then, the patient is being followed up with no recurrence of this complication or malfunction.
Usually presenting in the first year of implantation, Twiddler’s syndrome causes RV lead malfunction, usually in the pace/sense lead, and more rarely in the high energy coils. As such, it can lead to under or over sensing, loss of capture, and inappropriate AICD shocks. Usually, these cause symptoms of fatigue and lightheadedness. Rarely, it can lead to heart failure, phrenic nerve stimulation and sudden cardiac death[6,7].
In conclusion, our case is a unique presentation of Twiddler’s syndrome in that its initial presentation is in linearly increasing RV lead impedance, without symptoms. We believe this linear increase demonstrates a slowly progressing twist, propagating from the pocket site down the lead to its distal tip. Moreover, our case is unique regarding the site of the twist as well, located in two different locations. With this, we confirm the importance of regular follow up for patients with AICDs.
P- Reviewers Di Bella G, Dodd JD, Liu T, Teragawa H S- Editor Huang XZ L- Editor A E- Editor Yan JL
| 1. | Bayliss CE, Beanlands DS, Baird RJ. The pacemaker-twiddler’s syndrome: a new complication of implantable transvenous pacemakers. Can Med Assoc J. 1968;99:371-373. [PubMed] |
| 2. | Veltri EP, Mower MM, Reid PR. Twiddler’s syndrome: a new twist. Pacing Clin Electrophysiol. 1984;7:1004-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Boyle NG, Anselme F, Monahan KM, Beswick P, Schuger CD, Zebede J, Josephson ME. Twiddler’s syndrome variants in ICD patients. Pacing Clin Electrophysiol. 1998;21:2685-2687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Sidhu GS, Seifi A, Zangiabadi AH, Reinig M. Follow your leads: a case of twiddler’s syndrome. South Med J. 2009;102:871-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Nicholson WJ, Tuohy KA, Tilkemeier P. Twiddler’s Syndrome. N Engl J Med. 2003;348:1726-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Avitall B, Stormo A, Barragry T, Axtel K, Hare J. Sudden cardiac death: Twiddler’s syndrome with an implantable cardioverter defibrillator. Am Heart J. 1994;128:833-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Gasparini M, Regoli F, Ceriotti C, Gardini E. Images in cardiovascular medicine. Hiccups and dysphonic metallic voice: a unique presentation of Twiddler syndrome. Circulation. 2006;114:e534-e535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |