Published online Aug 26, 2012. doi: 10.4330/wjc.v4.i8.260
Revised: September 2, 2011
Accepted: September 9, 2011
Published online: August 26, 2012
Magnetic resonance imaging can be used for preprocedural assessment of complex anatomy for radiofrequency (RF) ablations, e.g., in a univentricular heart. This case report features the treatment of a young patient with a functionally univentricular heart who suffered from persistent sudden onset tachycardia with wide complexes that required RF ablation as treatment.
- Citation: Reiter T, Ritter O, Nordbeck P, Beer M, Bauer WR. MRI-guided ablation of wide complex tachycardia in a univentricular heart. World J Cardiol 2012; 4(8): 260-263
- URL: https://www.wjgnet.com/1949-8462/full/v4/i8/260.htm
- DOI: https://dx.doi.org/10.4330/wjc.v4.i8.260
Patients with a univentricular heart are born with a unique cardiac anatomy, including a wide range of heterogenic morphologies. The heart usually consists of a functionally single main ventricle that is associated with a hypoplastic or rudimentary second ventricular chamber. The anatomy of the outflow and inflow tract can also be altered, for example a double inlet or common atrioventricular canal can exist. Tricuspid or mitral atresia is often found. The clinical presentation depends on the exact anatomic features, but congestive heart failure commonly develops. A possible treatment is a complex surgical procedure, called Fontan’s operation, that ensures patient survival beyond childhood and teenage years. Fontan’s operation forms a total cavopulmonal anastomosis that connects the venae cavae directly to the pulmonary system without participation of the right atrium and ventricle. With increasing age, the patients often develop long-term side effects, the most common being cardiac arrhythmia, hepatic dysfunction and thrombosis[1]. Cardiac arrhythmias can be very resistant to medical treatment, thus requiring ablation therapy. Ablation therapy has been proven to be a very reliable treatment, with high long-term success rates[2]. The unique anatomy can be challenging for this procedure[3-9]. Magnetic resonance imaging (MRI) is a sensitive tool for soft tissue imaging and can be of great help in planning such an intervention.
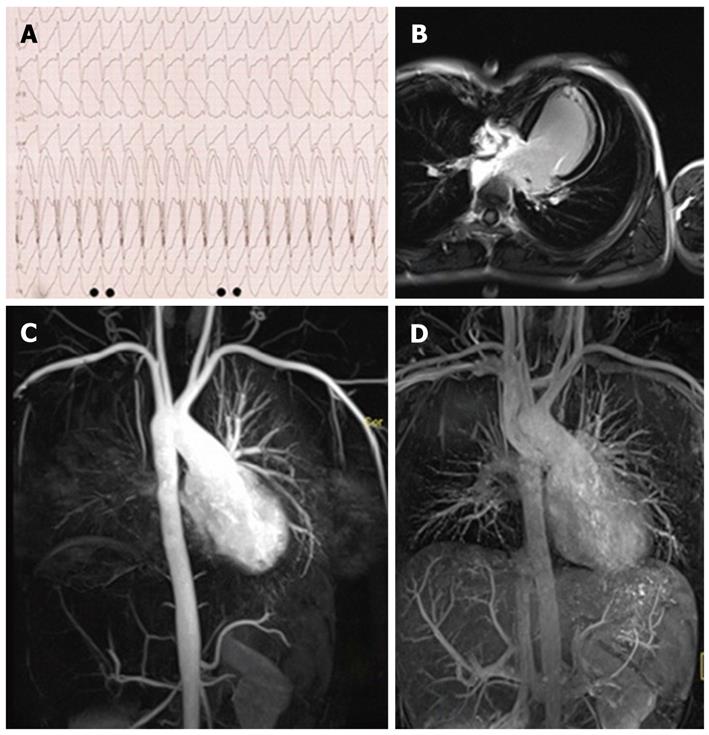
A 17-year-old boy with wide complex tachycardia (heart rate approximately 230 bpm), presented to our emergency room with dizziness and angina (Figure 1A). The tachycardia had been present for more than 3 h at the time of presentation. The patient maintained hemodynamic stability. Acute treatment included administration of adenosine, which had no effect on the tachycardia. Administration of ajmaline successfully terminated the tachycardia. The lack of an effect of adenosine led to the conclusion that supraventricular tachycardia (atrioventricular node reentry or accessory pathway) was very unlikely. The acute treatment was followed up by an invasive electrophysiological (EP) study during the patient’s stay at our hospital.
The patient had been born with a hypoplastic right ventricle and atrium, and atresia of the tricuspid valve. The functionally univentricular heart with a ventricular septal defect and L-malposition of the main arteries had been treated with Fontan’s operation at the age of 4 years. Besides these cardiac conditions, the patient suffered from hypofunction of the thyroid gland and attention deficit hyperactivity disorder. At the time of admission, the patient was treated with medikinet (methylphenidate) and aggrenox (acetylsalicylic acid and dipyridamol).
In this complex case with a univentricular heart and prior cardiac surgery (Fontan’s operation to form a total cavopulmonal anastomosis without participation of the right atrium and ventricle), we chose to examine the patient using MRI before the EP study. There are several advantages of MRI: first, it provides actual information on cardiac anatomy beyond operative notes; second, it offers better anatomical information and, in particular, better soft tissue contrast than echocardiography, which is important for exploring access routes (MR angiography) to the cardiac chambers; and third, contrast-enhanced late enhancement (LE) imaging can indicate intramural scars in contrast to CARTO3 alone, which is dependent on endocardial voltages. Furthermore CARTO3 cannot provide preprocedural information on anatomy.
A 3T Trio (Siemens, Erlangen, Germany) system was used for the MRI studies. 3D-MR angiography demonstrated the dextroposition of the aorta and an anastomosis between the venae cavae and the pulmonary arteries (Figure 1C and D). Steady-state free precession (SSFP true-FISP) imaging (images not shown) revealed a ventricular left-right shunt in the basal area as well as a ventricular septal patch. Septal hypokinetic activity with a remaining ejection fraction of 49% and a cardiac index of 3.3 L/min/m² was documented. After administration of gadolinium-based contrast agent, the LE scan showed a hypoplastic right atrium and right ventricle (Figure 1B). Except for subtle signal enhancement at the site of the septal patch, no left ventricular scar/fibrosis was detected (Figure 2B).
The actual EP study was performed using CARTO3 with a single 7F Navistar Thermocool D-Type/3.5 mm/115 cm catheter (Biosense Webster, Diamond Bar, CA, United States). The arterial access was chosen in accordance with the specific anatomy and the MRI scans showed no direct venous connection to the cardiac main chamber.
During the EP evaluation, all attempts using programmed stimulation to induce the tachycardia failed, even under isoprenaline. However, occasional premature ventricular complexes (PVCs) were detected. Supraventricular stimulation was not possible since the right atrium could not be reached due to anatomical obstacles in the univentricular heart, and the left atrium could not be stimulated in a reliable fashion by retrograde access via the left ventricle.
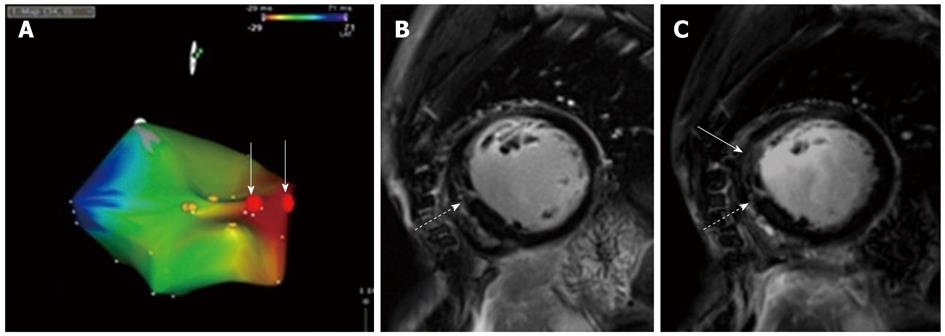
Validation of tachycardia origin was achieved with two approaches. Stimulation of the septal wall showed a QRS morphology similar to the complexes during the tachycardia. Secondly PVCs with electrocardiographic morphology similar to that found during tachycardia were used to create a CARTO3-based 3D-activation map, localizing the origin of earliest activation at the same septal area as the pace map. The PVCs were identical to the documented wide complex tachycardia, suggesting a triggered focus as origin. No areas with low voltage signals were detected which corresponds with the lack of scars/fibrosis in the MRI. His potentials were detected near this focus, indicating close proximity of the bundle (Figure 2A). However, bundle branch reentry tachycardia seemed extremely unlikely, since we had no reproducible induction of the ventricular tachycardia (VT). Since induction of VT failed, we could not see a stable His or bundle branch potential that would have preceded each ventricular activation and which then could indicate a bundle branch reentry[10].
Despite the close proximity of the focus to the bundle of His, radiofrequency (RF) ablation at a sufficient distance from the delicate bundle of His region was feasible. After the ablation, no PVCs were detected. A post-ablational LE MRI scan showed the ablation scar located at the septal wall close to the patch that had been used for closing the ventricular defect (Figure 2C).
In addition to the EP evaluation and ablation, optimization of the patient’s medical treatment was undertaken. Medikinet (methylphenidate) can be pro-arrhythmic[11] and might have contributed to the development of arrhythmias in the univentricular heart after Fontan’s operation. At present, 8 mo after the ablation, the patient is in good health and, to date, there has been no recurrence of the tachycardia.
Patients with a univentricular heart often exhibit very complex heart pathologies even if treated early with Fontan’s operation[12]. After this surgical procedure, heart anatomy and function remain idiosyncratic[13]. A strong association with cardiac arrhythmias has been described, and which might be challenging to treat[1,14]. MRI might offer essential therapeutic help, as it provides a very good insight into the anatomy of these hearts, thus allowing better planning of sometimes necessary EP procedures[15]. MRI can also be used to delineate ablation lesions in patients[2]. As shown in the current case, the synopsis of morphological and structural information and a thorough evaluation of the electrical activities can result in superior guidance and successful ablation in such difficult cases. Written consent for publication was obtained from the patient’s guardian.
Peer reviewers: Brian Olshansky, MD, Professor of Medicine, Cardiac Electrophysiology, University of Iowa Hospitals, 200 Hawkins Drive, Room 4426a JCP, Iowa City, IA 52242, United States; Richard G Trohman, Professor of Medicine, Rush University Medical Center, 1653 West Congress Parkway, Room 983 Jelke, Chicago, IL 60612, United States
S- Editor Cheng JX L- Editor Cant MR E- Editor Zhang DN
| 1. | Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21:28-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1278] [Cited by in RCA: 1361] [Article Influence: 38.9] [Reference Citation Analysis (1)] |
| 2. | Desmet W, Vanhaecke J, Vrolix M, Van de Werf F, Piessens J, Willems J, de Geest H. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J. 1992;13:1637-1640. [PubMed] |
| 3. | Cilliers A, Gewillig M. Fontan procedure for univentricular hearts: have changes in design improved outcome? Cardiovasc J S Afr. 2002;13:111-116. [PubMed] |
| 4. | de Groot NM, Lukac P, Blom NA, van Kuijk JP, Pedersen AK, Hansen PS, Delacretaz E, Schalij MJ. Long-term outcome of ablative therapy of postoperative supraventricular tachycardias in patients with univentricular heart: a European multicenter study. Circ Arrhythm Electrophysiol. 2009;2:242-248. [PubMed] |
| 5. | Giannakoulas G, Dimopoulos K, Yuksel S, Inuzuka R, Pijuan-Domenech A, Hussain W, Tay EL, Gatzoulis MA, Wong T. Atrial tachyarrhythmias late after Fontan operation are related to increase in mortality and hospitalization. Int J Cardiol. 2012;157:221-226. [PubMed] |
| 6. | Kaemmerer H, Bauer U, Pensl U, Oechslin E, Gravenhorst V, Franke A, Hager A, Balling G, Hauser M, Eicken A. Management of emergencies in adults with congenital cardiac disease. Am J Cardiol. 2008;101:521-525. [PubMed] |
| 7. | Khairy P, Fernandes SM, Mayer JE, Triedman JK, Walsh EP, Lock JE, Landzberg MJ. Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation. 2008;117:85-92. [PubMed] |
| 8. | Nürnberg JH, Ovroutski S, Alexi-Meskishvili V, Ewert P, Hetzer R, Lange PE. New onset arrhythmias after the extracardiac conduit Fontan operation compared with the intraatrial lateral tunnel procedure: early and midterm results. Ann Thorac Surg. 2004;78:1979-1988; discussion 1988. [PubMed] |
| 9. | Wolf CM, Seslar SP, den Boer K, Juraszek AL, McGowan FX, Cowan DB, Del Nido P, Triedman JK, Berul CI, Walsh EP. Atrial remodeling after the Fontan operation. Am J Cardiol. 2009;104:1737-1742. [PubMed] |
| 10. | Caceres J, Jazayeri M, McKinnie J, Avitall B, Denker ST, Tchou P, Akhtar M. Sustained bundle branch reentry as a mechanism of clinical tachycardia. Circulation. 1989;79:256-270. [PubMed] |
| 11. | Available from: http: //ch.oddb.org/de; as cited on 2011/06/23. |
| 12. | Gaca AM, Jaggers JJ, Dudley LT, Bisset GS. Repair of congenital heart disease: a primer--Part 2. Radiology. 2008;248:44-60. [PubMed] |
| 13. | Kurotobi S, Sano T, Naito H, Matsushita T, Takeuchi M, Kogaki S, Arisawa J, Matsuda H, Okada S. Regional ventricular systolic abnormalities caused by a rudimentary chamber in patients with univentricular hearts. Am J Cardiol. 1998;82:86-92. [PubMed] |
| 14. | Delacretaz E, Ganz LI, Soejima K, Friedman PL, Walsh EP, Triedman JK, Sloss LJ, Landzberg MJ, Stevenson WG. Multi atrial maco-re-entry circuits in adults with repaired congenital heart disease: entrainment mapping combined with three-dimensional electroanatomic mapping. J Am Coll Cardiol. 2001;37:1665-1676. [PubMed] |
| 15. | Weiss F, Habermann CR, Lilje C, Sasse K, Kühne T, Weil J, Adam G. [MRI in postoperative assessment of univentricular heart disease: correlation with echocardiography and angiography]. Rofo. 2002;174:1537-1543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |