Revised: December 10, 2011
Accepted: December 17, 2011
Published online: February 26, 2012
AIM: To study the interobserver variability between a cardiologist and vascular medicine specialist in the screening of the abdominal aorta during transthoracic echocardiography (TTE).
METHODS: Consecutive patients, > 55 years of age, underwent abdominal aortic imaging following standard TTE. Two cardiologists and one vascular medicine specialist performed a blinded review of the images. Interobserver agreement of abdominal aortic size was determined by the correlation coefficient and paired t test. Interobserver reliability for each cardiologist was assessed using Bland-Altman plots.
RESULTS: Ninety patients were studied. The mean age of patients was 72 ± 10 years and 48% were male. The mean aortic diameter was 2.31 ± 0.50 cm and 5 patients (5.5%) had an abdominal aortic aneurysm (AAA). The additional time required for the abdominal aortic images was 4.4 ± 0.9 min per patient. Interobserver agreement between the 2 cardiologist interpreters and the vascular medicine specialist was excellent (P > 0.05 for all comparisons). On Bland-Altman analysis of interobserver reliability, the 95% lower and upper limits for measurement by the cardiologists were 84% and 124% of that of the vascular specialist.
CONCLUSION: The assessment of the abdominal aorta during a routine TTE performed by a cardiologist is accurate in comparison to that of a vascular medicine specialist. In selected patients undergoing TTE, the detection rate of AAA is significant. Additional time and effort required to perform imaging of the abdominal aorta after TTE is less than 5 min.
- Citation: Navas EV, McCalla-Lewis A, Fernandez Jr BB, Pinski SL, Novaro GM, Asher CR. Abdominal aortic aneurysm screening during transthoracic echocardiography: Cardiologist and vascular medicine specialist interpretation. World J Cardiol 2012; 4(2): 31-35
- URL: https://www.wjgnet.com/1949-8462/full/v4/i2/31.htm
- DOI: https://dx.doi.org/10.4330/wjc.v4.i2.31
Abdominal aortic aneurysms (AAA) affect approximately 5% of elderly men at risk factors of cardiovascular disease[1,2]. Most AAA are not detectable on physical examination and remain silent until discovered during radiologic testing for other reasons or when complications occur. The recommendation for abdominal aortic ultrasound screening for AAA by the United States Preventive Services Task Force in select populations (men, age > 64 years, history of tobacco use) and by several Vascular Societies are supported by evidence demonstrating a reduction in aneurysm-related mortality[3-6]. However, AAA screening has not been widely adopted due to differing criteria for screening and uncertainty about costs and insurance coverage[7-10]. Transthoracic echocardiography (TTE) is frequently performed in patients with atherosclerotic vascular disease who may be at risk for the development of AAA. Although not commonly appreciated, the equipment used for TTE is similar to that used for abdominal aortic ultrasound, and imaging of the abdominal aorta can easily be performed as an adjunct to a standard echocardiographic examination.
The prevalence of AAA detected during TTE is estimated as 0.8%-6.5% depending on the demographic characteristics of the population screened[11-17]. Furthermore, the additional time required for AAA screening after TTE is generally less than 5 min. However, little data is available on who should interpret the study. Therefore, we designed a protocol for screening the abdominal aorta during TTE with the primary objective of comparing the interobserver variability between a cardiologist and vascular medicine specialist (i.e., the “gold standard”).
We prospectively evaluated 90 consecutive patients (age > 55 years old) scheduled for a clinically indicated TTE at the Cleveland Clinic Florida between November 1, 2005 and April 1, 2006. The study was approved by the Institutional Review Board. Clinical and demographic data were extracted from the electronic medical record. It was not known to the sonographer or the investigators at the time of the study whether the patient had a history of AAA. The same sonographer, licensed in both cardiac and vascular imaging performed all studies. Patient data were recorded with patient identifier numbers for confidentiality, and a database was secured with access only to the principal investigator and co-investigators.
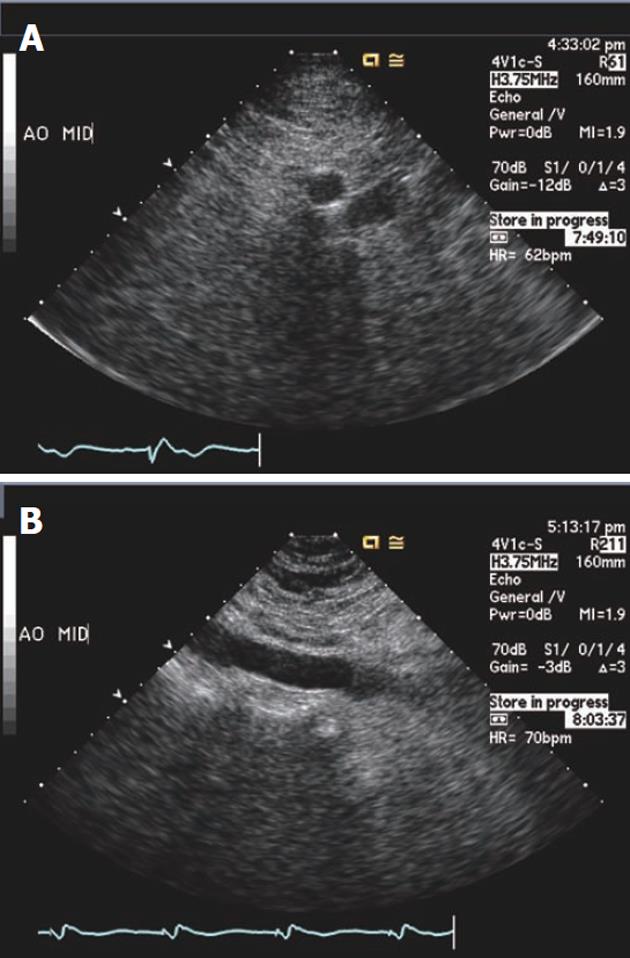
An ancillary aortic ultrasound was performed in all patients after the routine TTE images were completed and immediately after the subcostal images were obtained. A standard ultrasound machine with harmonic imaging mode and cardiac presets was utilized (Philips iE33; Philips Medical System, Andover MA or Sequoia C512; Acuson, Mountain View, CA). The transducer probe and frequency were not changed. Images of the proximal, mid and distal abdominal aorta in transverse and longitudinal planes were obtained (Figure 1). Images were digitally clipped and stored for future review and labeled with a study number. In a subgroup of 19 patients, the time taken to perform the additional abdominal aortic images was recorded.
Two staff cardiologists (Novaro GM, Asher CR) and one vascular medicine specialist (Fernandez Jr BB) made off-line measurements of the abdominal aorta. Measurements were made in 10 patients (30 segments) using the outer-edge to outer edge convention of the proximal, mid and distal aortic transverse projection. The readers were blinded to patient information. For the purpose of the study, AAA was defined as a diameter ≥ 3 cm.
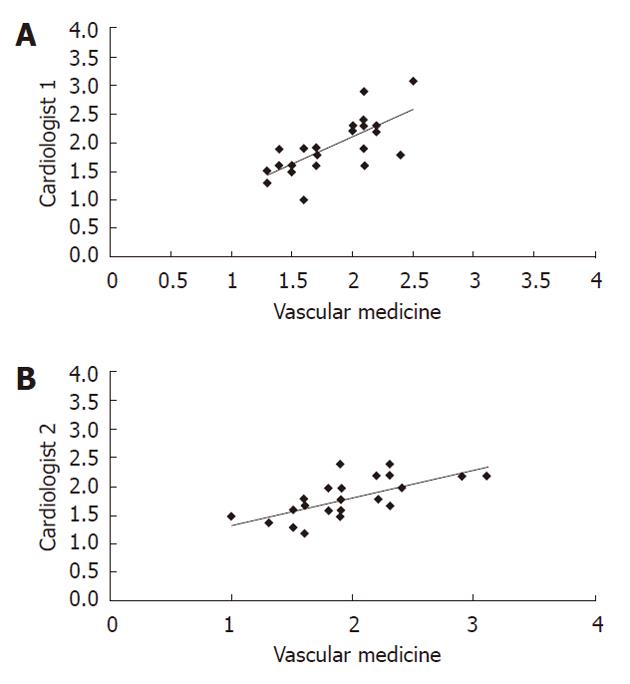
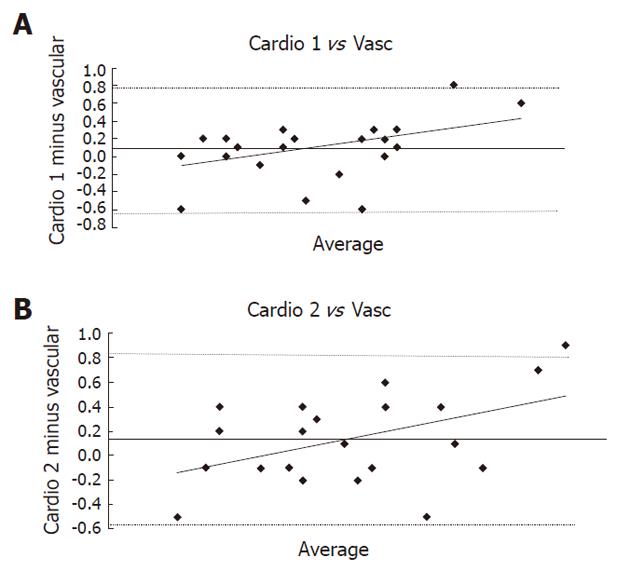
Comparisons were made between the cardiologists and vascular medicine specialist using paired t tests and Pearson’s coefficient of correlation (r). Bland-Altman difference plots were constructed to evaluate interobserver agreement between each Cardiologist’s interpretation compared with that of the vascular medicine specialist. These plots depict the mean of the aortic measurements on the x-axis, and the difference and 95% limit of agreement on the y-axis. P < 0.05 was considered statistically significant. We used SAS 9.1 (Cary, NC) and R 2.6.1 for all statistical analysis.
The study group comprised 90 patients, 43 men (48%), with an average age of 72 ± 10 years and body mass index (kg/m2) of 26.4 ± 5.6, 57 (63%) hypertensive, 51 (57%) smokers, 29 (32%) with coronary artery disease and 16 (18%) with diabetes. All abdominal aorta segments (proximal, mid and distal) were visualized adequately for measurement in 77% of patients. The infrarenal segment was seen in 93%, with the distal abdominal aorta least often well seen. The mean aortic diameter was 2.31 ± 0.50 cm. Five patients (5.5%) had abdominal aortic aneurysms (defined as a diameter ≥ 3.0 cm) ranging from 3.4 to 5.1 cm. Among the 5 patients with AAA, 2 were known and comparison computed tomography within 6 mo showed similar sizes (one patient had an AAA of 5.3 cm measured by computed tomography and of 5.1 cm measured by TTE and one patient had an AAA of 3.6 cm measured by computed tomography and of 3.9 cm measured by TTE). In 2 patients with small AAA, no confirmation was obtained due to advanced age and comorbid conditions. The additional time required for the abdominal aortic images was 4.4 ± 0.9 min per patient.
Interobserver agreement between the 2 cardiologist interpreters and the vascular medicine specialist was excellent (P > 0.05 for all comparisons; cardiologist 1 vs cardiologist 2, P = 0.531; cardiologist 1 vs vascular medicine, P = 0.728; cardiologist 2 vs vascular medicine, P = 0.432; Figure 2). Linear regression analysis showed a strong correlation at all 3 levels of aortic diameters. On Bland-Altman analysis of interobserver reliability, the 95% lower and upper limits for measurement by cardiologist 1 were 84.4% and 123.8% of that of the vascular medicine specialist and for cardiologist 2 they were 88.9% and 124.8% of that of the vascular medicine specialist. These differences were clinically insignificant with most measurements within 7 mm of the “gold standard” measurement (Figure 3).
In our study, we demonstrate that the interpretation of the abdominal aorta performed by a cardiologist during a TTE is accurate compared with that by a vascular medicine specialist. We found a similar prevalence of AAAs (5.5%) in a select group of patients 55 years of age and older as reported by previous studies and a limited (< 5 min) additional time required for abdominal imaging after a standard TTE.
AAA occur in 1-2% of the general population, most often in elderly man with a prior history of tobacco use or hypertension[1,2]. Current guidelines from the United States Preventive Services Task Force, Societies of Vascular Surgery and Medicine and Medicare recommend and support screening for AAA in selected groups of at-risk patients on the basis that screening is cost-effective and reduces aneurysm-related mortality[3-7]. Screening is underutilized because of the lack of consensus criteria and uncertain reimbursement[10]. Therefore, since the population of patients with cardiovascular disease undergoing TTE and those who are at risk for AAA have similar risk factors, abdominal aortic imaging during TTE is appealing and increasingly studied. Echocardiography continues to be a widely performed and reimbursable test particularly in patients with cardiovascular diseases such as coronary artery disease, hypertension, valvular heart disease and thoracic aortic disease.
The prevalence of AAA detected during supplementary imaging during TTE ranges from 0.8%-6.5%[11-17]. These studies have included both unselected and selected populations of patients chosen for screening undergoing routine TTE examinations. Confirmatory testing has shown favorable accuracy for TTE screening compared with a gold standard test (computed tomography, magnetic resonance imaging or abdominal aortic ultrasound). Several studies have also demonstrated that imaging of the abdominal aorta can be performed with the same equipment and in limited time for most patients, usually less than 5 min[14,16].
Most studies on AAA screening during TTE do not identify the training of the sonographer performing the examinations or the background of the interpreting physician. Although, cardiologists routinely make measurements of the ascending aorta during TTE, they do no usually evaluate the abdominal aorta. Conventions for measuring the ascending aorta vary, including inner edge to inner edge and leading edge to leading edge techniques, differing from standard measurements made by vascular medicine specialists. In addition, the abdominal aorta has considerably more atheroma than the ascending aorta, which confounds measuring the outer edge of a blood vessel. Therefore, it is important to establish that cardiologists without vascular training can accurately measure the abdominal aorta and detect AAA. We utilized a sonographer with training in both cardiac and vascular imaging. It cannot be expected that a cardiac sonographer without vascular training can image the abdominal aorta with similar quality.
We did not systematically compare the measurement of the aorta made by TTE to a gold standard test and therefore sensitivity and specificity cannot be determined. Intraobserver variability was not performed.
The assessment of the abdominal aorta during a routine TTE performed by a cardiologist is accurate in comparison to that of a vascular medicine specialist. In selected patients that fit the criteria for AAA screening, TTE detection of AAA is significant. Additional time and effort required to perform imaging of the abdominal aorta after TTE is less than 5 min.
Most abdominal aorta aneurysm (AAA) are not detectable on physical examination and remain silent until discovered during radiologic testing for other reasons or when complications occur. Transthoracic echocardiography (TTE) is frequently performed in patients with atherosclerotic vascular disease who may be at risk for the development of AAA. Although not commonly appreciated, the equipment used for TTE is similar to that used for abdominal aortic ultrasound, and imaging of the abdominal aorta can easily be done as an adjunct to a standard echocardiographic examination. Furthermore, the additive time required for AAA screening after TTE is generally less than 5 min. However, little data is available on who should interpret the study.
Most studies on AAA screening during TTE do not identify the training of the sonographer performing the examinations or the background of the interpreting physician. Although, cardiologists routinely make measurements of the ascending aorta during TTE they do no usually evaluate the abdominal aorta. Conventions for measuring the ascending aorta vary including inner edge to inner edge and leading edge to leading edge techniques, differing from standard measurements made by vascular medicine specialists. In addition, the abdominal aorta has considerably more atheroma than the ascending aorta which confounds measuring the outer edge of a blood vessel. Therefore, it is important to establish that cardiologists without vascular training can accurately measure the abdominal aorta and detect AAA. This research utilized a sonographer with training in both cardiac and vascular imaging.
In this study, authors investigated interobserver variability in the evaluation of TTE to assess the AAA. Two cardiologists and one specialist of vascular medicine were compared for their ability to accurately assess the TTE findings to diagnose AAA, since TTE is routinely used. They conclude that the diagnosis of AAA by routine TTE is as accurately done by a cardiologist as compared with a vascular medicine specialist.
The assessment of the abdominal aorta during a routine TTE performed by a cardiologist is accurate in comparison to a Vascular Medicine specialist. In selected patients that fit criteria for AAA screening, TTE detection of AAA is significant.
This is an important work and it is well performed. The manuscript is well written and sufficiently well illustrated.
Peer reviewers: Yuri V Bobryshev, PhD, Associate Professor, School of Medical Sciences, Faculty of Medicine University of New South Wales, Kensington NSW 2052, Australia; Prashanth Panduranga, Department of Cardiology, Royal Hospital, PB 1331, Muscat 111, Oman
S- Editor Cheng JX L- Editor Cant MR E- Editor Li JY
| 1. | Bickerstaff LK, Hollier LH, Van Peenen HJ, Melton LJ, Pairolero PC, Cherry KJ. Abdominal aortic aneurysms: the changing natural history. J Vasc Surg. 1984;1:6-12. [PubMed] |
| 2. | Scott RA, Ashton HA, Kay DN. Abdominal aortic aneurysm in 4237 screened patients: prevalence, development and management over 6 years. Br J Surg. 1991;78:1122-1125. [PubMed] |
| 3. | Screening for abdominal aortic aneurysm: recommendation statement. Ann Intern Med. 2005;142:198-202. [PubMed] |
| 4. | Kent KC, Zwolak RM, Jaff MR, Hollenbeck ST, Thompson RW, Schermerhorn ML, Sicard GA, Riles TS, Cronenwett JL. Screening for abdominal aortic aneurysm: a consensus statement. J Vasc Surg. 2004;39:267-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 137] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 5. | Ashton HA, Buxton MJ, Day NE, Kim LG, Marteau TM, Scott RA, Thompson SG, Walker NM. The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet. 2002;360:1531-1539. [PubMed] |
| 6. | Wilmink AB, Quick CR, Hubbard CS, Day NE. Effectiveness and cost of screening for abdominal aortic aneurysm: results of a population screening program. J Vasc Surg. 2003;38:72-77. [PubMed] |
| 7. | Multicentre aneurysm screening study (MASS): cost effectiveness analysis of screening for abdominal aortic aneurysms based on four year results from randomised controlled trial. BMJ. 2002;325:1135. [PubMed] |
| 8. | Lindholt JS, Juul S, Fasting H, Henneberg EW. Hospital costs and benefits of screening for abdominal aortic aneurysms. Results from a randomised population screening trial. Eur J Vasc Endovasc Surg. 2002;23:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 119] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 9. | Wood S. Proposed Medicare reimbursement for aortic aneurysm screening gains momentum and Congress support. Available From: URL: www.theheart.org [Heartwire > News]. Mar 29 2004; . |
| 10. | Federman DG, Carbone VG, Kravetz JD, Kancir S, Kirsner RS, Bravata DM. Are screening guidelines for abdominal aortic aneurysms being implemented within a large VA primary health care system? Postgrad Med. 2009;121:132-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Schwartz KV, Rashkow AM, Akella MS. Detection of Abdominal Aortic Aneurysm During Routine Echocardiography. Echocardiography. 1996;13:71-74. [PubMed] |
| 12. | Spittell PC, Ehrsam JE, Anderson L, Seward JB. Screening for abdominal aortic aneurysm during transthoracic echocardiography in a hypertensive patient population. J Am Soc Echocardiogr. 1997;10:722-727. [PubMed] |
| 13. | Seelig MH, Malouf YL, Klingler PJ, Oldenburg WA, Atkinson EJ. Clinical utility of routine screening for abdominal aortic aneurysm during echocardiography. Vasa. 2000;29:265-268. [PubMed] |
| 14. | Giaconi S, Lattanzi F, Orsini E, Prosperi R, Tartarini G. Feasibility and accuracy of a rapid evaluation of the abdominal aorta during routine transthoracic echocardiography. Ital Heart J Suppl. 2003;4:332-336. [PubMed] |
| 15. | Bekkers SC, Habets JH, Cheriex EC, Palmans A, Pinto Y, Hofstra L, Crijns HJ. Abdominal aortic aneurysm screening during transthoracic echocardiography in an unselected population. J Am Soc Echocardiogr. 2005;18:389-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Ruggiero M, Lenti ML, Cavallari D, Dicillo CP, Mascolo AR, Musci S, Tota F, Sabato G, Tortorella C, Damiani D. Screening for abdominal aortic aneurysm during transthoracic echocardiography. A prospective study in 1202 consecutive patients at high risk: incidence, correlation with risk factors, feasibility, diagnostic accuracy, and increase in echocardiography time. G Ital Cardiol (Rome). 2006;7:217-223. [PubMed] |
| 17. | Roshanali F, Mandegar MH, Yousefnia MA, Mohammadi A, Baharvand B. Abdominal aorta screening during transthoracic echocardiography. Echocardiography. 2007;24:685-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |