Revised: December 20, 2011
Accepted: December 27, 2011
Published online: January 26, 2012
AIM: To study a cohort of consecutive patients undergoing transcatheter aortic valve implantation (TAVI) and compare the outcomes of atrial fibrillation (AF) patients vs patients in sinus rhythm (SR).
METHODS: All consecutive patients undergoing TAVI in our hospital were included. The AF group comprised patients in AF at the time of TAVI or with history of AF, and were compared with the SR group. Procedural, echocardiographic and follow-up variables were compared. Likewise, the CHA2DS2-VASC stroke risk score and HAS-BLED bleeding risk score and antithrombotic treatment at discharge in AF patients were compared with that in SR patients.
RESULTS: From a total of 34 patients undergoing TAVI, 17 (50%) were allocated to the AF group, of whom 15 (88%) were under chronic oral anticoagulation. Patients in the AF group were similar to those in the SR group except for a trend (P = 0.07) for a higher logistic EuroSCORE (28% vs 19%), and a higher prevalence of hypertension (82% vs 53%) and chronic renal failure (17% vs 0%). Risk of both stroke and bleeding was high in the AF group (mean CHA2DS2-VASC 4.3, mean HAS-BLED 2.9). In the AF group, treatment at discharge included chronic oral anticoagulation in all except one case, and in association with an antiplatelet drug in 57% of patients. During a mean follow-up of 11 mo (maximum 32), there were only two strokes, none of them during the peri-procedural period: one in the AF group at 30 mo and one in the SR group at 3 mo. There were no statistical differences in procedural success, and clinical outcome (survival at 1 year 81% vs 74% in AF and SR groups, respectively, P = NS).
CONCLUSION: Patients in AF undergoing TAVI show a trend to a higher surgical risk. However, in our cohort, patients in AF did not have a higher stroke rate compared to the SR group, and the prognosis was similar in both groups.
- Citation: Salinas P, Moreno R, Calvo L, Jiménez-Valero S, Galeote G, Sánchez-Recalde A, López-Fernández T, Garcia-Blas S, Iglesias D, Riera L, Moreno-Gómez I, Mesa JM, Plaza I, Ayala R, Gonzalez R, López-Sendón JL. Clinical and prognostic implications of atrial fibrillation in patients undergoing transcatheter aortic valve implantation. World J Cardiol 2012; 4(1): 8-14
- URL: https://www.wjgnet.com/1949-8462/full/v4/i1/8.htm
- DOI: https://dx.doi.org/10.4330/wjc.v4.i1.8
Degenerative aortic stenosis (AS) is currently the most prevalent acquired valvular heart disease, occurring in 4.6% of adults ≥ 75 years old[1]. The classic treatment for symptomatic severe AS is surgical aortic valve replacement (SAVR), which modifies the natural history of the disease and has improved survival in historical comparisons[2-4]. Unfortunately, one third of patients who are recognized to need surgery are rejected, generally because of unacceptably high surgical risk[5]. Transcatheter aortic valve implantation (TAVI) has had successful and constant development during the last few years to become a real alternative for these high-risk patients[6].
With more than 10 000 implants in Europe, the TAVI technique has reached maturity with implantation success in ≥ 95% and 30 d mortality < 10% in transfemoral procedures and < 20% in transapical procedures[7-9]. In the randomized Placement of Aortic TraNscatheter Valve Trial (PARTNER), cohort B proved superiority of TAVI compared with medical treatment (including aortic valvuloplasty) in inoperable patients, with an outstanding 20% absolute decrease in mortality at 1 year[10]. In the recently reported results of PARTNER cohort A, the TAVI procedure met non-inferiority criteria compared with SAVR in a high-risk population, thus becoming an alternative to surgery for patients accepted for surgery but with a high surgical risk[11].
One of the limitations, however, of TAVI in the PARTNER cohort A trial was a significantly higher incidence of stroke in comparison with SAVR. In this elderly, high surgical risk population, stroke is one of the biggest concerns a clinician may have because of the associated disability and mortality. Stroke rates after SAVR are reported to be around 5% in a high-risk population[12], and they are associated with aortic cross-clamping and hypoperfusion during cardiopulmonary by-pass. TAVI procedures have reported stroke rates below 5%, albeit with a subclinical incidence of 70%-80% in magnetic resonance studies (40%-50% for similar studies in SAVR)[7,13,14]. It is attributed to manipulation of large catheters in atherosclerotic and calcified aortas and to embolization after valvuloplasty or valve implantation. However, apart from these technical reasons for stroke in patients undergoing TAVI, atrial fibrillation (AF) is a potential confounding factor in the relationship between aortic replacement and stroke, and little has been reported to date on this issue. AF is a well-known risk factor for stroke (approximately 1 in 5 strokes are caused by AF), and is very prevalent in old patients (5%-15% in ≥ 80-year-old patients)[15]. It is also a common comorbid condition in the late stages of aortic valve disease. This study aimed to determine the influence of AF in the TAVI population, on procedure complications and on long-term prognosis, as well as to analyze the antithrombotic treatment at discharge.
At our center, a total of 34 implants have been performed (31 transfemoral and 3 transapical). All TAVI patients were excluded from conventional SAVR because of high surgical risk in a ‘heart team’ meeting composed of clinical cardiologists, interventional cardiologists, anesthesiologists and cardiac surgeons. In a dedicated prospective database we recorded data from all evaluated patients, implantations and follow-up. Variables included were basal characteristics of the patients, symptoms and intervention indication, EuroSCORE, echocardiographic data, procedural characteristics and complications during the procedure, following the published recommendations[16].
TAVI procedures were performed in a catheterization laboratory under general anesthesia, with most of the patients being extubated before leaving the laboratory. All cases were implanted with the Edwards-SAPIEN transcatheter valve system (Edwards Lifesciences, Irvine, United States)[17]. Vascular access was obtained by surgical cutdown of the femoral artery, and closure was secured by direct suture of the femoral artery. The prosthesis delivery and implantation process has been previously described[18,19]. If significant coronary artery disease was found in the preliminary study, percutaneous coronary revascularization was performed approximately 1 mo prior to the procedure.
For this paper, we divided our implanted population in two groups: those in AF or with a previous history of AF (AF group) and those in sinus rhythm (SR) without a history of AF (SR group). We calculated previously validated CHA2DS2VASC and HAS-BLED scores to assess the stroke and bleeding risk, respectively; and the suitability of antithrombotic treatment[15,20,21]. As for the HAS-BLED score, we defined major bleeding as any bleeding requiring hospitalization and/or causing a decrease in hemoglobin of more than 2 g/L and/or requiring blood transfusion, which was not a hemorrhagic stroke[21]. Chronic renal failure was defined as serum creatinine levels ≥ 200 mmol/L (cut-off value of EuroSCORE risk score). Left ventricular ejection fraction was estimated by the biplanar Simpson method. We also recorded treatment at discharge of all patients. Recommended medical treatment after TAVI is aspirin plus 75 mg clopidogrel for 3-6 mo, and only aspirin afterwards, but final treatment at discharge was open to the clinician’s preference. If warfarin was used, target INR values were 2.0-3.0. Patients without AF before TAVI but developing AF during or after the procedure were maintained in the SR group for statistical comparisons, but received special attention and will be described in detail.
Clinical follow-up was obtained in all patients by clinical visits, and/or telephone interview. The following clinical end-points were determined: death, myocardial infarction, stroke, aortic valve surgery, hospitalization because of heart failure, and the combination of all of them (MACE, major adverse cardiac events).
Also, several echocardiographic studies were performed at follow-up (at discharge, at 6 mo, 1 year, and every year subsequently) to evaluate prosthetic function (maximum and mean trans-aortic pressure gradients, aortic valve area, aortic valve regurgitation, and left ventricular function).
Statistical analysis was performed with PASW version 17.0 (SPSS Inc, Chicago, IL). Categorical variables are expressed as proportions (percentages) and continuous variables as mean ± standard deviation unless otherwise specified. Comparisons between groups were performed with the Student t test (comparison of 2 means) or Chi-square test (comparison of proportions). Comparative survival analysis was performed with the Kaplan-Meier curves and log-rank test. Associations with a P value < 0.05 were considered statistically significant, although all P values are provided.
Main characteristics of both AF and non-AF groups are shown in Table 1. There were significant differences only in the ‘prior warfarin use’ item, but there was a trend (P = 0.068) towards a higher prevalence of hypertension and chronic renal failure as well as a higher mean EuroSCORE in the AF group. Echocardiographic features of the valve disease and other coexistent heart diseases were also similar between both groups. All patients had symptomatic AS, with no differences in the accompanying symptoms: similar proportion of heart failure (76.4% in AF patients vs 88.2% in SR patients, P = 0.37); a numerically but not statistically higher rate of angina in the AF group (43.8% vs 17.7%, P = 0.1); and 4 patients with syncope in each group.
| AF group | SR group | P | |
| Male gender | 6 (35.3) | 7 (41.2) | 0.72 |
| Age (yr) | 81.3 | 83.9 | 0.15 |
| Diabetes | 8 (47.1) | 6 (35.3) | 0.49 |
| Hypertension | 14 (82.4) | 9 (52.9) | 0.07 |
| Peripheral vascular disease | 4 (23.5) | 1 (5.9) | 0.15 |
| Significant coronary disease | 6 (35.3) | 10 (58.8) | 0.17 |
| Prior stroke | 3 (17.7) | 2 (11.8) | 0.63 |
| Chronic respiratory failure | 2 (11.8) | 4 (23.5) | 0.37 |
| Chronic renal failure | 3 (17.7) | 0 | 0.07 |
| Hemodialysis | 2 (11.8) | 0 | 0.14 |
| Prior warfarin use | 15 (88.2) | 0 | < 0.01 |
| Logistic euroSCORE (mean) | 27.9 | 18.7 | 0.07 |
| Baseline echocardiogram features | |||
| Aortic valve area (cm2, mean) | 0.66 | 0.72 | 0.35 |
| Peak gradient (mmHg, mean) | 76.9 | 71.4 | 0.42 |
| Mean gradient (mmHg, mean) | 44.2 | 41.8 | 0.60 |
| LVEF (mean) | 55.9% | 57.5% | 0.66 |
Average CHA2DS2-VASC score for the whole AF group was 4.3 (range, 2-7) whereas the average HAS-BLED bleeding score was 2.9 (range, 2-5).
Procedural and in-hospital outcomes of both groups are shown in Table 2. There were no significant differences in any of the peri-procedural outcomes. There were 2 deaths in the AF group: one patient died because of coronary obstruction, myocardial infarction and shock, and the other because of respiratory complications attributed to previous pulmonary fibrosis and severe pulmonary hypertension (no prosthesis dysfunction). There were 2 deaths in the SR group: one transfemoral procedure complicated by perforation with the temporary pacemaker lead, and one transapical procedure with post-procedural severe bleeding at the site of ventricular puncture 48 h after the procedure. Only 2 patients (6%) had new onset AF during TAVI admission. One patient from the SR group had new onset AF 2 d after TAVI and was discharged under warfarin plus clopidogrel (this patient was kept in SR group “per protocol”, as described in methods). The other patient from the AF group was in SR at the start of TAVI, but developed AF during the procedure and was discharged with AF under warfarin treatment. None of these patients had events in the follow-up.
| AF group | Non-AF group | P | |
| Valve size (mm) | 0.27 | ||
| 23 | 13 (76.5) | 10 (58.8) | |
| 26 | 4 (23.5) | 7 (41.2) | |
| Access | 0.55 | ||
| Transfemoral | 16 (94.1) | 15 (88.2) | |
| Transapical | 1 (5.9) | 2 (11.8) | |
| Procedural success | 16 (94.1) | 17 (100) | 0.31 |
| Any peri-procedural complication | 7 (41.2) | 7 (41.2) | 1.00 |
| Death | 2 (11.8) | 2 (11.8) | 1 |
| Emergent heart surgery | 0 | 1 (5.9) | 0.31 |
| Orotracheal intubation > 24 h | 0 | 1 (5.9) | 0.31 |
| Proshtesis embolization | 0 | 0 | - |
| Endocarditis | 0 | 0 | - |
| New onset AF | 1 (5.9) | 1 (5.9) | 1.00 |
| Coronary obstruction | 1 (5.9) | 1 (5.9) | 1.00 |
| Myocardial infarction | 1 (5.9) | 1 (5.9) | 1.00 |
| Stroke | 0 | 0 | - |
| Renal failure requiring hemodialysis | 0 | 0 | - |
| New pacemaker implantation | 2 (11.8) | 1 (5.9) | 0.55 |
| Major access site complications | 0 | 2 (11.8) | 0.14 |
| Minor access site complications | 2 (11.8) | 4 (23.5) | 0.37 |
| Transfusion | 5 (29.4) | 2 (11.8) | 0.20 |
| Post-procedural stay (mean days) | 14.4 | 10.2 | 0.22 |
During hospitalization (and at 30-d follow-up), 4 patients died: one after transapical and 3 after transfemoral procedures. Therefore, survival at 30 d was 88.2% in the overall study population, 90.3% in patients undergoing trans-femoral TAVI, and 66.7% in those undergoing trans-apical TAVI. Thus, 30 patients were discharged alive: 15 from SR group and 15 from AF group. All patients in the SR group were treated after valve implantation with aspirin 100 mg/d plus clopidogrel 75 mg/d for 3-6 mo. AF patients were treated according to the clinical cardiologist’s preference, as shown in Table 3. The most common treatment at discharge was warfarin alone, followed by warfarin plus aspirin.
| Patient | Age | Gender | CHA2DS2-VASC | HAS-BLED | Treatment at discharge | Follow up (mo) | Non-fatal events | Follow up (mo) | Survival |
| 1 | 87 | Female | 6 | 5 | Warfarin | 2 | None | 2 | Alive |
| 2 | 76 | Male | 4 | 4 | Aspirin | 32 | None | 32 | Alive |
| 3 | 81 | Female | 5 | 3 | Warfarin + Aspirin | 7 | None | 7 | Alive |
| 4 | 80 | Female | 4 | 3 | Warfarin | 1 | None | 1 | Alive |
| 5 | 90 | Female | 6 | 2 | Warfarin | 26 | None | 26 | Alive |
| 6 | 77 | Female | 5 | 3 | Warfarin | 23 | None | 23 | Alive |
| 7 | 68 | Female | 2 | 2 | Aspirin + Clopidogrel | 10 | None | 10 | Alive |
| 8 | 83 | Male | 7 | 4 | Warfarin + Aspirin | 3 | None | 3 | Death, non-cardiac |
| 9 | 80 | Female | 3 | 2 | Warfarin | 19 | None | 19 | Alive |
| 10 | 79 | Female | 5 | 3 | Warfarin + Aspirin | 30 | Stroke | 31 | Death, non-cardiac |
| 11 | 84 | Female | 5 | 3 | Warfarin + Clopidogrel | 1 | Heart failure admission | 31 | Alive |
| 12 | 87 | Female | 4 | 2 | Warfarin + Aspirin | 6 | None | 6 | Alive |
| 13 | 83 | Female | 3 | 2 | Warfarin | 5 | None | 5 | Alive |
| 14 | 82 | Male | 3 | 3 | Warfarin + Aspirin | 2 | None | 2 | None |
| 15 | 68 | Male | 3 | 2 | Warfarin + Clopidogrel | 1 | Heart failure admission | 3 | Alive |
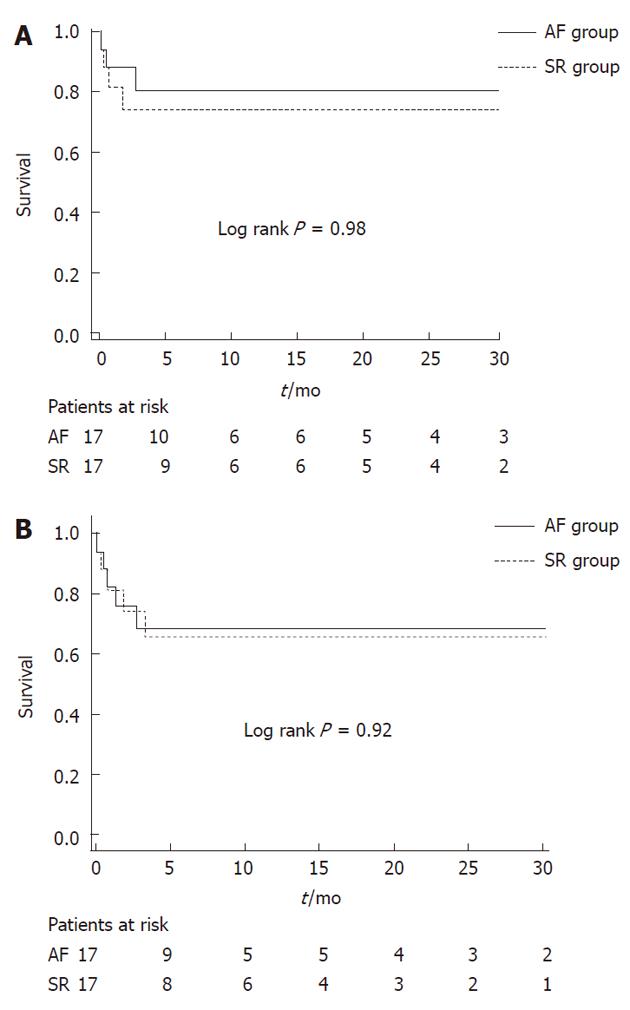
Clinical follow-up was completed in 100% of the patients. Mean follow-up for the whole cohort was 10.4 mo, with a maximum of 32 mo. Kaplan-Meier curves for survival are shown in Figure 1A. Mean survival was similar in both groups: 23.8 mo in the SR group vs 25.6 mo in the AF group (log-rank, Mantel-Cox: P = 0.98; hazard ratio (HR), 0.99; 95% confidence interval (CI), 0.26-3.75). Survival at 30 d was 81.4% in the SR group vs 88.2% in the AF group. Survival at 1 year was 74% in the SR group vs 80.9% in the AF group. Figure 1B depicts survival free from a composite MACE endpoint (death, stroke, myocardial infarction, aortic valve surgery, heart failure admission, and prosthesis failure). Survival free from MACE was similar: 21.4 mo in SR vs 21.7 mo in AF (log-rank, Mantel-Cox: P = 0.92; HR, 0.94; 95% CI, 0.29-3.11). Survival at 30 d was 81.4% in the SR group vs 82.4% in the AF group; whereas survival at 1 year was 65.8% in the SR group vs 68.4% in the AF group.
Importantly, there were 2 strokes in the follow up. One took place in the AF group at 30.3 mo (a patient treated with aspirin and warfarin), and contributed to the patient’s death due to respiratory complications. The other happened at 3.3 mo in the SR group (aspirin), and was classified as atherosclerotic with the patient remaining in SR, and the patient was discharged with mild sequelae. There were no documented major bleedings either in AF or non-AF patients in the entire follow-up.
Follow-up echocardiography was performed at 6 mo, 1 year, and every year subsequently. For this study we selected the longest available echocardiographic follow-up, with a mean of 14.7 mo. There were no differences between AF and non-AF patients in any of the echocardiographic items during the follow-up (Table 4). There were no cases of prosthesis thrombosis, or prosthesis failure.
| AF group | SR group | P | |
| Aortic valve area (cm2, mean) | 1.66 | 2.05 | 0.18 |
| Peak gradient (mmHg, mean) | 18.6 | 19.3 | 0.86 |
| Mean gradient (mmHg, mean) | 9.5 | 11.0 | 0.51 |
| LVEF (mean) | 59% | 62.9% | 0.14 |
| Valvular aortic regurgitation | |||
| No | 70% | 66.7% | - |
| Mild | 30% | 33.3% | - |
| Moderate | 0% | 0% | - |
| Severe | 0% | 0% | - |
| Paravalvular aortic regurgitation | |||
| No | 10% | 55.6% | - |
| Mild | 70% | 44.4% | - |
| Moderate | 20% | 0% | - |
| Severe | 0% | 0% | - |
The PARTNER trial cohort A results have lifted the TAVI procedure from “alternative procedure” to “non-inferior” compared to surgery in patients acceptable for surgery but with a relatively high risk. However, a new concern appeared, as stroke rates were significantly higher in the TAVI arm compared to the SAVR group (8.3% vs 4.3% at 1 year, P = 0.04)[11]. This was not totally unexpected, because 3-5% of patients undergoing cardiac surgery suffer a periprocedural stroke[22], and prior studies with TAVI had described similar or even higher subclinical brain ischemic events[13,14].
We analyzed the potential influence that AF, a first-line risk factor for stroke, could have in the stroke rate of the TAVI population. Our cohort had a slightly higher prevalence of AF compared to PARTNER population (50% vs 41% in the PARTNER TAVI arm), and interestingly AF patients had higher risk compared to non-AF patients (logistic EuroSCORE 27.9 vs 18.7), with otherwise no relevant differences in baseline characteristics. However, this higher risk did not translate into differences in TAVI procedure complications, with only a trend toward a longer hospital stay (14 d vs 10 d, P = 0.22) and a more frequent need of transfusion in the AF group (29% vs 12%, P = 0.2). In our cohort, we had no strokes during admission and the stroke rate in the follow-up was as low as 6%, with no differences among groups. The fact that the 2 strokes occurred during follow-up after discharge and not in the peri-operative period does not support the use of embolic protection devices during TAVI, that has been proposed by some groups[23].
Survival and other long-term events were also similar between patients with and without AF before TAVI, as well as prosthesis hemodynamics. The follow-up estimated valve area was higher (non-significantly) in the non-AF group, but that was probably due to the lower number of patients with 26 mm valves in the AF group. This is supported also by the similar gradients found in both groups (Table 4).
In spite of the long experience with bioprosthesis, treatment at discharge of patients with aortic bioprostheses is still controversial, and the recommendations after TAVI are based only on expert consensus. Guidelines for the management of patients with valvular heart disease published by the American Heart Association and the European Society of Cardiology all recommend the prescribing of aspirin to all recipients of bioprosthetic heart valves (Class I, Level of evidence C) as well as the consideration of warfarin use during the first 3 mo, notwithstanding the lack of evidence[4,24]. Some studies have found no advantage of 3-mo warfarin treatment in patients with no other indication for anticoagulation[25,26].
Our AF cohort received antithrombotic treatment according to stroke and bleeding scores, as recommended in the AF guidelines and irrespective of the presence of the aortic bioprosthesis[27,28]. This led to similar rates of stroke, major hemorrhage and MACE events, supporting this management.
The main limitation of this paper was the small study population that could make some differences among groups non-significant. Nevertheless this is somewhat balanced with a long-term follow up of the patients, that showed similar survival and event-free survival curves. We performed no routine brain imaging, assuming the under-detection of clinically silent cerebral events, but focused on clinically evident strokes that were of major relevance to the clinician. All treatment data was observational, so it should only be used for hypothesis-generating purposes, with limited value due to the heterogeneity of therapeutic strategies.
In the absence of specific guidelines or previous literature to choose a specific antithrombotic treatment after TAVI in AF patients, the treatment at discharge was tailored to each patient, according to both bleeding and stroke scores. This treatment obtained similar rates of stroke, bleeding or MACE events during follow-up. In our cohort, AF patients undergoing TAVI had similar prognosis despite the trend toward a higher risk compared with the non-AF patients.
Transcatheter aortic valve implantation (TAVI) has become a safe and effective alternative for high surgical risk aortic stenosis patients. Stroke rates in a recent randomized trial were found to be superior in the TAVI group than in the surgical group. Atrial fibrillation (AF) is a potential confounding factor as it is related to age and stroke, and has not been studied in this setting. Furthermore, there are no specific recommendations for antithrombotic treatment in the TAVI population, and its influence in the follow-up
Stroke rates in patients undergoing TAVI procedures are a major concern for the clinician, and the influence of AF in this setting has not been addressed. Antithrombotic treatment of AF patients after TAVI implantation is not well established.
Clinically relevant strokes after TAVI were globally low, and there are no differences among AF and sinus rhythm (SR) patients. Antithrombotic treatment after TAVI tailored according to stroke and bleeding risks, and irrespective of the presence of the transcatheter valve obtained similar stroke rates to SR patients in the follow-up.
The study suggest tailoring the long-term antithrombotic treatment of AF patients undergoing TAVI to the stroke and bleeding risks, irrespective of the presence of the transcatheter valve. Future studies with larger population should verify this hypothesis and confirm the finding of similar stroke rates in this setting.
The paper investigated the potential influence of AF on the stroke rate in a consecutive TAVI collection. Herein, they found no strokes during admission and no differences between the AF- and non-AF-group in the follow up.
Dr. Salinas receives an educational grant from Cordis Corp. and the Spanish Society of Cardiology. To Dr. Filgueiras and Dr. Dobarro who contributed to the database and the selection of patients for TAVI.
Peer reviewer: Dirk Skowasch, MD, Department of Cardiology, University of Bonn, Sigmund-Freud-Strasse 25, 53105 Bonn, Germany
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
| 1. | Aronow WS, Kronzon I. Prevalence and severity of valvular aortic stenosis determined by Doppler echocardiography and its association with echocardiographic and electrocardiographic left ventricular hypertrophy and physical signs of aortic stenosis in elderly patients. Am J Cardiol. 1991;67:776-777. [PubMed] |
| 2. | Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008;118:e523-e661. [PubMed] |
| 3. | Lester SJ, Heilbron B, Gin K, Dodek A, Jue J. The natural history and rate of progression of aortic stenosis. Chest. 1998;113:1109-1114. [PubMed] |
| 4. | Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, Filippatos G, Flachskampf F, Hall R, Iung B, Kasprzak J. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J. 2007;28:230-268. [PubMed] |
| 5. | Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24:1231-1243. [PubMed] |
| 6. | Webb J, Cribier A. Percutaneous transarterial aortic valve implantation: what do we know? Eur Heart J. 2011;32:140-147. [PubMed] |
| 7. | Salinas P, Moreno R, Lopez-Sendon JL. Transcatheter aortic valve implantation: Current status and future perspectives. World J Cardiol. 2011;3:177-185. [PubMed] |
| 8. | Moreno R, Dobarro D, López de Sá E, Prieto M, Morales C, Calvo Orbe L, Moreno-Gomez I, Filgueiras D, Sanchez-Recalde A, Galeote G. Cause of complete atrioventricular block after percutaneous aortic valve implantation: insights from a necropsy study. Circulation. 2009;120:e29-e30. [PubMed] |
| 9. | Moreno R, Calvo L, Salinas P, Dobarro D, Santiago JV, Sanchez-Recalde A, Galeote G, Riera L, Moreno-Gomez I, Mesa J. Causes of peri-operative mortality after transcatheter aortic valve implantation: a pooled analysis of 12 studies and 1223 patients. J Invasive Cardiol. 2011;23:180-184. [PubMed] |
| 10. | Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597-1607. [PubMed] |
| 11. | Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187-2198. [PubMed] |
| 12. | Thourani VH, Ailawadi G, Szeto WY, Dewey TM, Guyton RA, Mack MJ, Kron IL, Kilgo P, Bavaria JE. Outcomes of surgical aortic valve replacement in high-risk patients: a multiinstitutional study. Ann Thorac Surg. 2011;91:49-55; discussion 55-56. [PubMed] |
| 13. | Ghanem A, Müller A, Nähle CP, Kocurek J, Werner N, Hammerstingl C, Schild HH, Schwab JO, Mellert F, Fimmers R. Risk and fate of cerebral embolism after transfemoral aortic valve implantation: a prospective pilot study with diffusion-weighted magnetic resonance imaging. J Am Coll Cardiol. 2010;55:1427-1432. [PubMed] |
| 14. | Knipp SC, Matatko N, Schlamann M, Wilhelm H, Thielmann M, Forsting M, Diener HC, Jakob H. Small ischemic brain lesions after cardiac valve replacement detected by diffusion-weighted magnetic resonance imaging: relation to neurocognitive function. Eur J Cardiothorac Surg. 2005;28:88-96. [PubMed] |
| 15. | Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31:2369-2429. |
| 16. | Leon MB, Piazza N, Nikolsky E, Blackstone EH, Cutlip DE, Kappetein AP, Krucoff MW, Mack M, Mehran R, Miller C. Standardized endpoint definitions for Transcatheter Aortic Valve Implantation clinical trials: a consensus report from the Valve Academic Research Consortium. J Am Coll Cardiol. 2011;57:253-269. [PubMed] |
| 17. | Moreno R, Calvo L, Filgueiras D, López T, Sánchez-Recalde A, Jiménez-Valero S, Galeote G, López-Sendón JL. [Percutaneous implantation of aortic valve prosthesis in patients with symptomatic severe aortic stenosis rejected for surgical valve replacement]. Rev Esp Cardiol. 2008;61:1215-1219. [PubMed] |
| 18. | Lichtenstein SV, Cheung A, Ye J, Thompson CR, Carere RG, Pasupati S, Webb JG. Transapical transcatheter aortic valve implantation in humans: initial clinical experience. Circulation. 2006;114:591-596. [PubMed] |
| 19. | Webb JG, Chandavimol M, Thompson CR, Ricci DR, Carere RG, Munt BI, Buller CE, Pasupati S, Lichtenstein S. Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation. 2006;113:842-850. [PubMed] |
| 20. | Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263-272. [PubMed] |
| 21. | Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093-1100. [PubMed] |
| 22. | Salazar JD, Wityk RJ, Grega MA, Borowicz LM, Doty JR, Petrofski JA, Baumgartner WA. Stroke after cardiac surgery: short- and long-term outcomes. Ann Thorac Surg. 2001;72:1195-1201; discussion 1201-1202. [PubMed] |
| 23. | Nietlispach F, Wijesinghe N, Gurvitch R, Tay E, Carpenter JP, Burns C, Wood DA, Webb JG. An embolic deflection device for aortic valve interventions. JACC Cardiovasc Interv. 2010;3:1133-1138. [PubMed] |
| 24. | Bonow RO, Carabello BA, Kanu C, de Leon AC, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006;114:e84-231. [PubMed] |
| 25. | Gherli T, Colli A, Fragnito C, Nicolini F, Borrello B, Saccani S, D'Amico R, Beghi C. Comparing warfarin with aspirin after biological aortic valve replacement: a prospective study. Circulation. 2004;110:496-500. [PubMed] |
| 26. | Jamieson WR, Moffatt-Bruce SD, Skarsgard P, Hadi MA, Ye J, Fradet GJ, Abel JG, Janusz MT, Cheung A, Germann E. Early antithrombotic therapy for aortic valve bioprostheses: is there an indication for routine use? Ann Thorac Surg. 2007;83:549-556; discussion 556-557. [PubMed] |
| 27. | Wann LS, Curtis AB, Ellenbogen KA, Estes NA, Ezekowitz MD, Jackman WM, January CT, Lowe JE, Page RL, Slotwiner DJ. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on Dabigatran): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;123:1144-1150. [PubMed] |
| 28. | Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31:2369-2429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3227] [Cited by in RCA: 3335] [Article Influence: 222.3] [Reference Citation Analysis (0)] |