INTRODUCTION
Coronary artery disease (CAD) is the leading cause of morbidity and mortality in many advanced countries and its prevalence is increasing in developing countries[1,2]. According to recent World Health Organization statistics for 2007, cardiovascular deaths account for 33.7% of all deaths worldwide, whereas cancer represents 29.5%, other chronic diseases 26.5%, injury 7%, and communicable diseases 4.6%[3]. CAD is the leading cause of cardiovascular death throughout the world. In light of the current global focus on healthcare utilization, costs, and quality, it is essential to monitor and understand the magnitude of healthcare delivery and costs, as well as the quality of healthcare delivery in relation to the CAD.
Invasive coronary angiography (ICA) is widely used as a reliable technique to diagnose CAD because of its superior spatial and temporal resolution. However, it is an invasive and expensive procedure with an associated small percentage of morbidity and mortality[4]. As an alternative to ICA, coronary computed tomography (CT) angiography has been increasingly used for the investigation of suspected CAD, and rapid technological developments of multislice CT (MSCT) have led to both improved spatial and temporal resolution[5-7]. Studies have shown that coronary CT angiography has a high diagnostic accuracy for the detection of significant CAD (≥ 50% lumen stenosis) when compared to ICA[8-11], and in selected patients, coronary CT angiography is recommended as a reliable alternative to ICA in the diagnosis of CAD.
Despite promising results having been achieved with coronary CT angiography, it has the disadvantage of high radiation dose, which leads to the concern of radiation-associated risks[12,13]. It is generally agreed that CT is an imaging modality with high radiation exposure, as it contributes up to 70% of the radiation dose of all radiological examinations, although it comprises only 15% of all radiological examinations. Radiation-induced malignancy is a problem that has raised serious concern in the medical field and this has been addressed by the National Research Council of the United States[14]. It is reported that radiation dose from a CT scan has been significantly underestimated by both radiologists and physicians[12,15]. Despite the increased awareness of radiation risk, many clinicians and researchers have not realized the amount of radiation exposure associated with coronary CT angiography, or the possibility of tailoring the scanning protocols to reduce radiation exposure to patients. Thus, the purpose of this article was to investigate the current research directions of coronary CT angiography in CAD, based on a systematic review of the literature published in five main radiology journals over the past 6 years.
RESULTS
General information
One hundred and forty-two studies were identified which met the selection criteria and were included in the analysis. One hundred and thirty seven studies were conducted at a single centre, while three studies were performed at 3 centres and the remaining two studies at 9 and 20 study sites, respectively. The majority of these studies were published in ER with the highest number being 62 articles, and the least number of studies was found in the BJR with only 11 studies being identified. For the remaining three journals, Radiology, AJR and EJR, the corresponding studies were 23, 24 and 22, respectively.
Analysis of author background indicated that most of the studies were performed by radiologists, followed by cardiologists, and other health care professionals such as physicians and medical imaging specialists. Radiologists accounted for 84% of the authors who performed the studies, while cardiologists were in collaboration with radiologists as a research team in all of the studies, except in two studies published in ER, where cardiologists alone conducted the research.
Of 142 studies, 126 were performed on patients (89%), and the remaining 16 studies were conducted on anthropomorphic phantoms with the aim of investigating the effect of heart rate on diagnostic image quality, or radiation dose or high pitch value on image quality. 71 studies (50%) were performed to study the diagnostic value (67 studies) and prognostic value (4 studies) of coronary CT angiography in CAD, while the remaining studies were mainly focused on radiation dose reduction.
Type of MSCT scanners
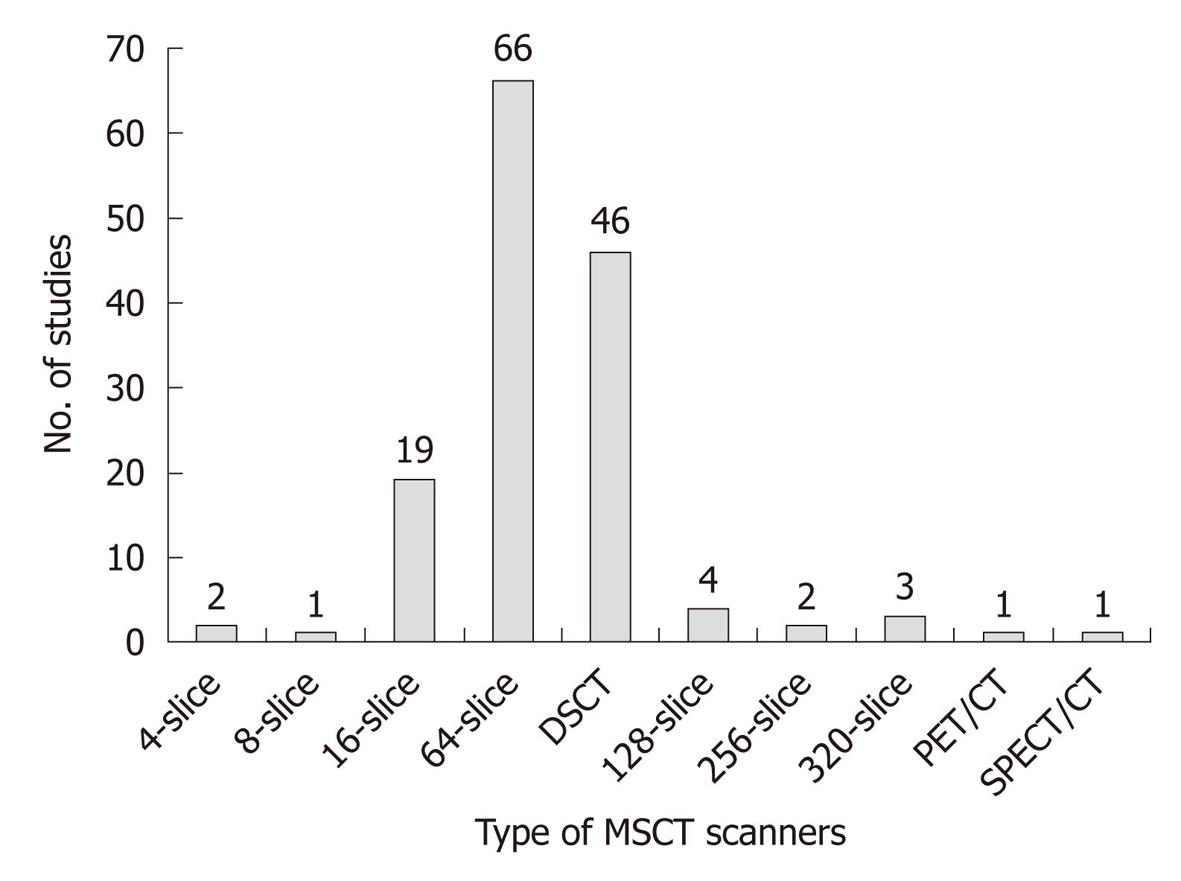
Variable MSCT scanners were used in these studies, with 64- or more slice-scanners representing the majority (85%) of the studies. Figure 1 shows the distribution of different generations of MSCT scanners that were identified in the analysis. Despite rapid technological developments of MSCT scanners, such as the increased availability of 256- and 320-slice CT, single source 64-slice and dual-source CT (DSCT) still dominated 78% of the coronary CT angiography studies. Coronary CT angiography was compared with integrated single photon emission computed tomography/CT and positron emission tomography/CT in two studies to investigate the myocardial perfusion value of coronary CT angiography.
Figure 1 The number of studies performed with different generations of multislice computed tomography scanners.
CT: Computed tomography; DSCT: Dual-source CT; MSCT: Multislice CT; PET: Positron emission tomography; SPECT: Single photon emission computed tomography.
Research directions of coronary CT angiography
The issue of radiation dose has been addressed since 2007 in the publications, Radiology, AJR and BJR, while this has been addressed since 2008 in the EJR publications. In comparison, radiation dose was first reported in some studies published in 2006 in the journal of ER, although more attention has been paid to the issue of dose since 2007. Prior to 2006 and 2007, research was focused on the diagnostic value of coronary CT angiography in CAD, regardless of the studies performed with 8-slice, 16- or 64-slice CT scanners. From 2008, more and more studies started to address radiation dose reduction in these five radiology journals.
Dose-saving strategies
Various dose-saving strategies have been implemented in these studies, and have included adjustments of tube voltage (kVp), tube current (tube current modulation), pitch value, prospective ECG-triggering vs retrospective ECG-gating, addition of padding in patients with high heart rate variability, and application of adaptive statistical iterative reconstruction (ASIR) algorithms for image noise reduction. Radiation dose was reported in 64 studies, representing 45% of the total studies published in the five radiology journals. Of these 64 studies, nearly 50% were published in the journal of ER.
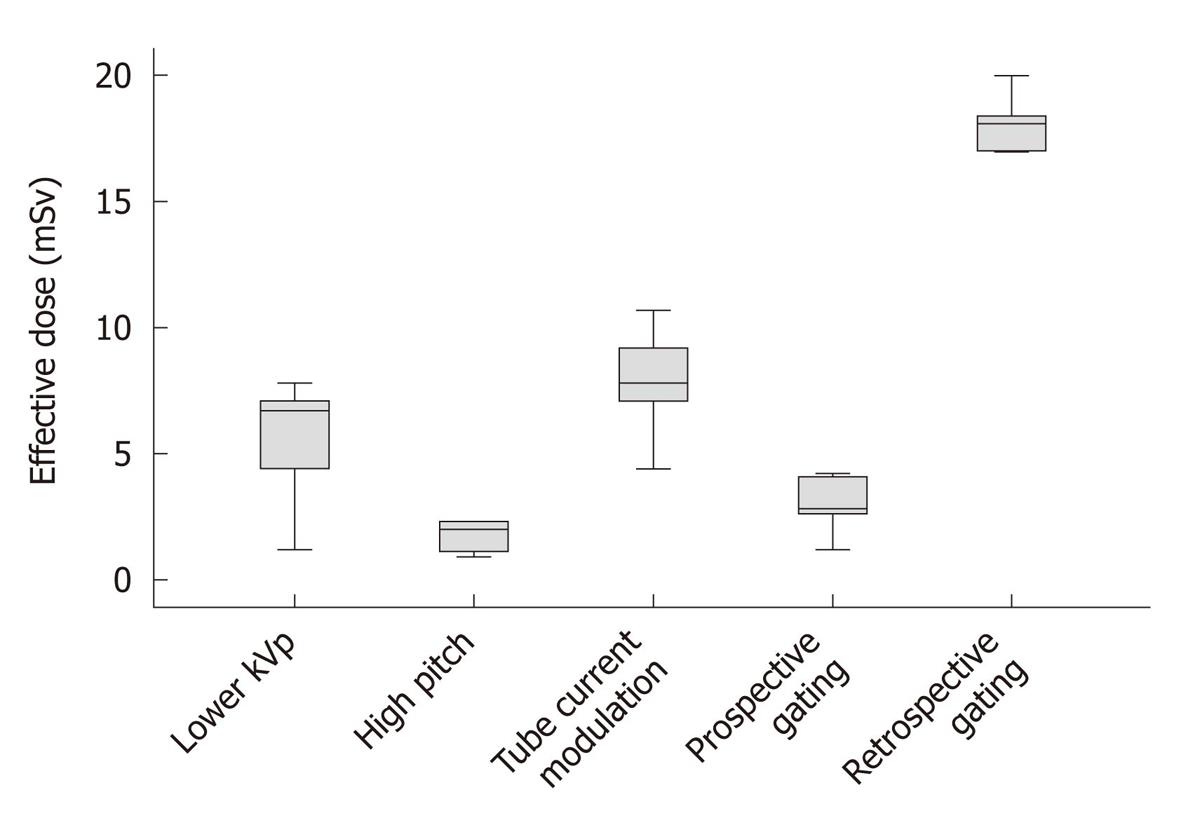
Prospective ECG-triggering was the most commonly applied technique for dose reduction, with 25 studies reported in these five radiology journals. Of these 25 studies, a direct comparison between prospective ECG-triggering and retrospective gating was performed in 16 studies. The mean effective dose was 3.5 ± 1.9 mSv for prospective ECG-triggering, which is significantly lower (P < 0.0001) than that acquired with retrospective ECG-gating, which is 16.3 ± 6.3 mSv.
ECG-controlled tube current modulation was the second most common approach utilized in 22 studies for dose reduction. However, the effective dose value was only reported in 7 studies, with the mean dose being 8.8 ± 2.6 mSv. Application of pitch (up to 3.4) in coronary CT angiography was reported in five studies with the mean effective dose being 1.7 ± 0.6 mSv. Lower kVp of 100 vs the standard 120 kVp was compared in four studies with the resultant mean effective dose of 5.4 ± 2.9 mSv for 100 kVp protocols, and 9.4 ± 5.1 mSv for 120 kVp protocols, leading to a dose reduction of 42%. Figure 2 shows the mean effective dose associated with the above-mentioned commonly used strategies for dose reduction. As shown in the figure, prospective ECG-triggering and high pitch resulted in the lowest doses when compared to other dose-saving strategies.
Figure 2 Box plot shows the mean effective dose associated with different dose-reduction techniques.
Coronary computed tomography angiography with the use of high pitch and prospective electrocardiography-triggering leads to the lowest radiation dose. The boxes indicate the first to third quartiles, and each midline indicates the median (second quartile) and the whiskers represent the maximum and minimum values of effective dose.
ASIR was reported in two studies and the mean effective dose was less than 3.0 mSv. A comparison of radiation dose with use of the International Commission on Radiological Protection (ICRP) 103 and ICRP 60 documents was conducted in two studies with a significant difference observed, indicating that the radiation dose was underestimated if dose calculation is based on the weighting factors that were reported in the ICRP 60.
Radiation dose corresponding to different heart rates was reported in three studies and the analysis shows that DSCT is superior to single-source CT in the diagnosis of CAD in patients with higher heart rates, with resultant lower doses. Padding was applied in one study performed with prospective ECG-gating. The purpose of adding padding is to provide additional phase information to compensate for variations in heart rate by adding time before and after the centre phase of the acquisition. Padding is described in the range of 0-200 ms and is added to both sides of the centre of the acquisition with padding 0 corresponding to a window of 100 ms scanning time and padding 100 corresponding to a window of 200 ms scanning time. In that study, the effective dose was 2.3 mSv for 0 padding, and the dose increased to 3.8 mSv for 1-99 padding and to 5.5 mSv for 100-150 padding.
The remaining study involved the investigation of the effect of adjusting the scan length of coronary CT angiography using the calcium scoring images instead of the scout view with regard to radiation dose. The effective dose associated with the calcium scoring-derived length (9.0 ± 0.6 mSv) was significantly lower than that using the scout view-derived length (10.7 ± 1.2 mSv), corresponding to a radiation dose reduction of 16%.
DISCUSSION
This analysis presents three findings which are considered important for the clinical application of coronary CT angiography in CAD. Firstly, there is a change in research direction with a shift of focus from the previous diagnostic value of coronary CT angiography in CAD to an emphasis on radiation dose reduction. This indicates the increased awareness of radiation dose to patients during coronary CT angiography examinations. Secondly, more dose-saving strategies have been implemented to reduce radiation dose associated with coronary CT angiography while still maintaining diagnostic image quality. Of these strategies, prospective ECG-triggering and high pitch protocols represent the most effective approaches with a significant reduction of radiation dose compared to conventional retrospective gating or other approaches. Thirdly, coronary CT angiography performed with 64-slice CT (single-source or DSCT) dominated the majority of studies that were reviewed, and this indicates that 64-slice CT still plays a key role in the clinical diagnosis of CAD, despite the emergence of 256- and 320-slice CT.
Over the last decade a great deal of interest has been focused on the imaging and diagnosis of CAD using coronary CT angiography, due to its less invasive nature and improved spatial and temporal resolution. Moderate to high diagnostic accuracy was achieved with 64- or more slice CT, owing to further technical improvements[16-20]. These studies have indicated that coronary CT angiography has high accuracy in the diagnosis of CAD and could be used as an effective alternative to ICA in selected patients. However, coronary CT angiography has the disadvantage of high radiation dose which raises concerns for both clinicians and manufacturers. This is reflected in the changing research directions from the early research focus on the diagnostic value of coronary CT angiography in CAD to the increasingly reported studies on dose reduction, as demonstrated in this analysis.
Radiation dose is becoming a major issue for coronary CT angiography, since 64- or more-slice CT shows improved and promising results in the diagnosis of CAD[21-25]. The radiation risks associated with coronary CT angiography have raised serious concerns and have become a hot topic of debate in the literature[12,13,26]. The general view about radiation dose is that CT is associated with a risk of cancer development. Therefore, coronary CT angiography should be performed with dose-saving strategies whenever possible to reduce the radiation dose to patients.
One of the most effective approaches for dose reduction is adjustment of the tube current according to ECG signal, which is defined as ECG-controlled tube current modulation. This approach represents the most significant improvement in minimizing radiation exposure from coronary CT angiography. It has been reported that radiation dose can be reduced by 30%-50% through modulation of the tube current output to decrease the dose given during the systolic phase[27,28]. The estimated radiation dose reduction is similar to or less than that of an ICA examination with use of this dose saving strategy[27,29]. The mean effective dose of ECG-controlled tube current modulation in this analysis was 8.8 mSv, and this was comparable to that of ICA, which was between 3-9 mSv[30].
Prospective ECG-triggering has been confirmed to be another efficient technique for radiation dose reduction in coronary CT angiography[31-33]. Use of prospective ECG-triggering with 64-slice or DSCT has been reported to reduce the effective radiation dose by up to 90% when compared to retrospective ECG-gating, with diagnostic image quality being achieved in more than 90% of cases[34-39]. This was confirmed in this analysis, as the mean effective dose of prospective triggering was 3.5 mSv, which is equivalent to or even lower than that of ICA.
Another effective method currently undertaken in coronary CT angiography to reduce radiation dose is to lower the tube voltage, since radiation dose varies with the square of the kV. Modern CT scanners include tube voltages of 120 or 140 kV, reflecting the settings which most often result in adequate image quality. However, acquisition of cardiac CT images with 100 kV, or even lower, is possible and has been suggested as an effective means to reduce radiation dose in coronary CT angiography[40,41]. Up to 70% dose reduction has been reported in the literature when the X-ray tube voltage is decreased from 120 kVp to 100 kVp or even 80 kVp[42,43]. This analysis showed that a 42% dose reduction was observed in coronary CT angiography with the use of 100 kVp when compared to the routine 120 kVp protocol, and this is consistent with the results reported in the literature. Therefore, tube voltage can be adjusted in cardiac CT angiography without affecting diagnostic image quality, and this should be applied whenever possible in clinical practice[44,45].
For coronary CT angiography, very low pitch values (0.2-0.4) are typically required for coronary data acquisition to ensure continuous z-axis coverage between image stacks reconstructed from consecutive cardiac cycles. The main disadvantage of this approach is higher radiation exposure since the table is advanced by less than one detector width during each gantry rotation, thus, the same anatomic area is exposed to X-ray radiation during consecutive rotations of the gantry. Increasing the pitch to a higher value was made possible by the development of the second generation of DSCT scanners, Siemens Definition Flash, which enabled acquisition of 128 slices simultaneously (flying focal spot)[46-50]. This DSCT mode allows coronary CT angiography to be performed at high pitch values of up to 3.4 with a significant reduction in radiation dose. A high pitch was applied in five studies in this analysis with a mean effective dose of 1.72 mSv, and a radiation dose less than 1.0 mSv was also reported in one study, indicating the effectiveness of this dose-reduction approach. The new scan mode, with a superior temporal resolution of 75 ms, is regarded as an attractive alternative to ICA due to the very low dose and high image quality, although more studies based on a large cohort are required.
Although nearly 50% of the studies in this analysis were conducted with the use of single-source CT, DSCT was used in about one-third of the studies, indicating the increased use of this improved technique. The main limitation of single-source CT coronary angiography is that β-blockers are frequently used to lower the heart rate to less than 65 beats per minute. The introduction of DSCT marked another technological improvement of MSCT in cardiac imaging, as the temporal resolution was further increased from 165 ms to 83 ms, thus eliminating the need to control the heart rate during the scan[43,44,51]. Studies comparing DSCT with single-source CT demonstrated that DSCT maintains high diagnostic accuracy in the diagnostic examination of a wide range of patient subsets, e.g., patients with higher and even irregular heart rates (including atrial fibrillation)[52-54]. Despite slightly lower per-segment evaluability in patients with higher heart rates, DSCT did not show decreased diagnostic accuracy for the detection of coronary stenoses[54,55]. DSCT improves temporal resolution which is vital in patients who cannot have β blockade.
Expansion of MSCT systems from a 64-slice to 256- and 320-slice system has allowed for the accurate assessment of stenosis severity and atherosclerotic plaque composition, or even the acquisition of whole-heart coverage in one gantry rotation, thus, eliminating the restrictions and limitations associated with 64-slice CT scanners[22-24]. Studies performed with 256- and 320-slice CT demonstrated the high diagnostic value of coronary CT angiography for the quantification of coronary lumen stenosis and assessment of plaque morphology and distribution in the coronary arteries[22,56,57]. In patients with atrial fibrillation, 320-slice CT allows for excellent visualization of all coronary segments with sufficient images to enable a diagnosis, and acquisition of images with consistent CT attenuation along the different coronary arteries[23,57]. Despite these advantages, 256- and 320-slice CT has the limitations of reduced gantry speed (270-350 ms), high radiation dose and cone beam effects which need to be addressed in future technical developments.
Some limitations exist in this review. Firstly, our search for references only focused on the five main radiology journals. However, research articles on cardiac CT imaging are also published in cardiac journals such as European Heart Journal, Journal of American College of Cardiology, Circulation, American Journal of Cardiology and International Journal of Cardiovascular Imaging. Therefore, it is possible that some relevant references were not included in this analysis. Secondly, although tube current modulation is one of the most effective methods for radiation dose reduction, a number of studies did not report the actual effective dose, despite the application of this technique in their studies. This emphasises the importance of awareness of radiation exposure to patients by physicians; thus, radiation dose values (effective dose or dose length product) should be recorded in each study to enable the comparison of dose-saving techniques between different studies. Thirdly, we tried to include as many references as possible that were available over the last few years; however, some articles which were accepted for publication were excluded from the analysis. Finally, although this analysis shows that 64-slice CT coronary angiography dominated the majority of the studies, there is no doubt that more and more studies are being performed with the latest models such as 256- and 320-slice CT scanners. Further research to include these studies is necessary.
In conclusion, this systematic review of the literature from five main radiology journals shows that the current research in coronary CT angiography has shifted from the previous focus on diagnostic accuracy in CAD to more emphasis on radiation dose reduction. This review also indicates the increased awareness of radiation dose associated with coronary CT angiography in the literature. Various dose-saving strategies have been undertaken in the past few years to lower radiation exposure to patients undergoing coronary CT angiography. Effective dose reduction has been achieved by employing techniques with a radiation dose of around 10 mSv to as low as 1 mSv in some studies. It is important to note that the current effective doses from coronary CT angiography are at the same level or even lower than those acquired from ICA. Therefore, according to this analysis, the achievements in radiation dose reduction in coronary CT angiography have been tremendous.