INTRODUCTION
Resting heart rate (HR) is an easily accessible clinical parameter. The initiation of the HR by spontaneous sinoatrial node depolarization is determined by voltage-sensitive membrane currents, particularly the hyperpolarization activated pacemaker current If, and by calcium release from the sarcoplasmic reticulum, leading to diastolic depolarization through activation of the sodium-calcium exchanger current[1].
Experimental data and clinical observations support the notion of the importance of HR in the pathophysiology of atherosclerosis and plaque rupture[2]. An elevated HR enhances mechanical arterial wall stress and it prolongs the exposure of the coronary endothelium to systolic low and oscillatory shear stress. All these processes induce structural and functional changes in endothelial cells, which accumulate over time in atherosclerosis-prone regions, promoting atherosclerosis[2]. Furthermore, elevated HR caused by mechanical stress may promote weakening of the fibrous cap, ultimately increasing the risk of plaque disruption and the onset of an acute coronary syndrome[3].
Ivabradine, a selective inhibitor of the If channel, reduces resting and exercise HR without affecting cardiac contractility or blood pressure[4-6]. Clinical trials have revealed an improved exercise tolerance, an increased time to exercise-induced ischemia, and a reduced frequency of ambient angina attacks after If channel inhibition[7,8]. This editorial summarizes the possible role of ivabradine on atherosclerosis.
THE ROLE OF HR IN CARDIOVASCULAR DISEASE
A large number of studies in healthy and asymptomatic subjects as well as in patients with already established coronary artery disease (CAD) have demonstrated that HR is a very important and major independent cardiovascular risk factor for prognosis[9]. In the general population, life expectancy is associated inversely with elevated HR[10-12]. This association is independent of gender and genetic background. An increase in risk is derived from data comparing individuals with HR < 60 beats per minute with those with HR of 90-99 beats per minute[13]. In particular, there is an increase in CAD mortality and there is also an increase in sudden cardiac death[11]. The contribution of HR reduction to the clinical effects of β-blockers and calcium-channel blockers has been analyzed in several studies[14,15].
In the Framingham study, cardiovascular and coronary mortality increased progressively with resting HR in a cohort of 5070 subjects free from cardiovascular disease at the time of entry into the study. The effect of HR on mortality was independent of traditional cardiovascular risk factors[2,16-18].
The analysis of a pre-specified subgroup of the BEAUTIFUL (morbidity-mortality evaluation of the If inhibitor ivabradine in patients with coronary disease and left-ventricular dysfunction) trial demonstrated that, in patients with CAD and left ventricular systolic dysfunction, a resting HR > 70 beats per minute is associated with an increased cardiovascular mortality as well as increased risk for hospitalization due to heart failure, myocardial infarction, or the need for coronary revascularization[19]. Recently, the systolic heart failure treatment with If inhibitor ivabradine trial, demonstrated that patients with HR ≥ 87 beats per minute, had a two-fold higher risk of the primary composite endpoint (cardiovascular death or hospital admission for worsening heart failure) than patients with the lowest HR (70 to < 72 beats per minute). The risk of primary composite endpoint events increased by 3% with every beat increase from baseline HR, and 16% for every 5 beats per minute increase. Thus, the authors conclude that high HR is a risk factor in heart failure and therefore, it should be an important target for treatment of heart failure[20]. Taken together, there is compelling epidemiologic evidence that elevated resting HR is predictive of cardiovascular risk, independently of the other currently accepted risk factors.
ATHEROSCLEROSIS, INCREASED HR AND IVABRADINE
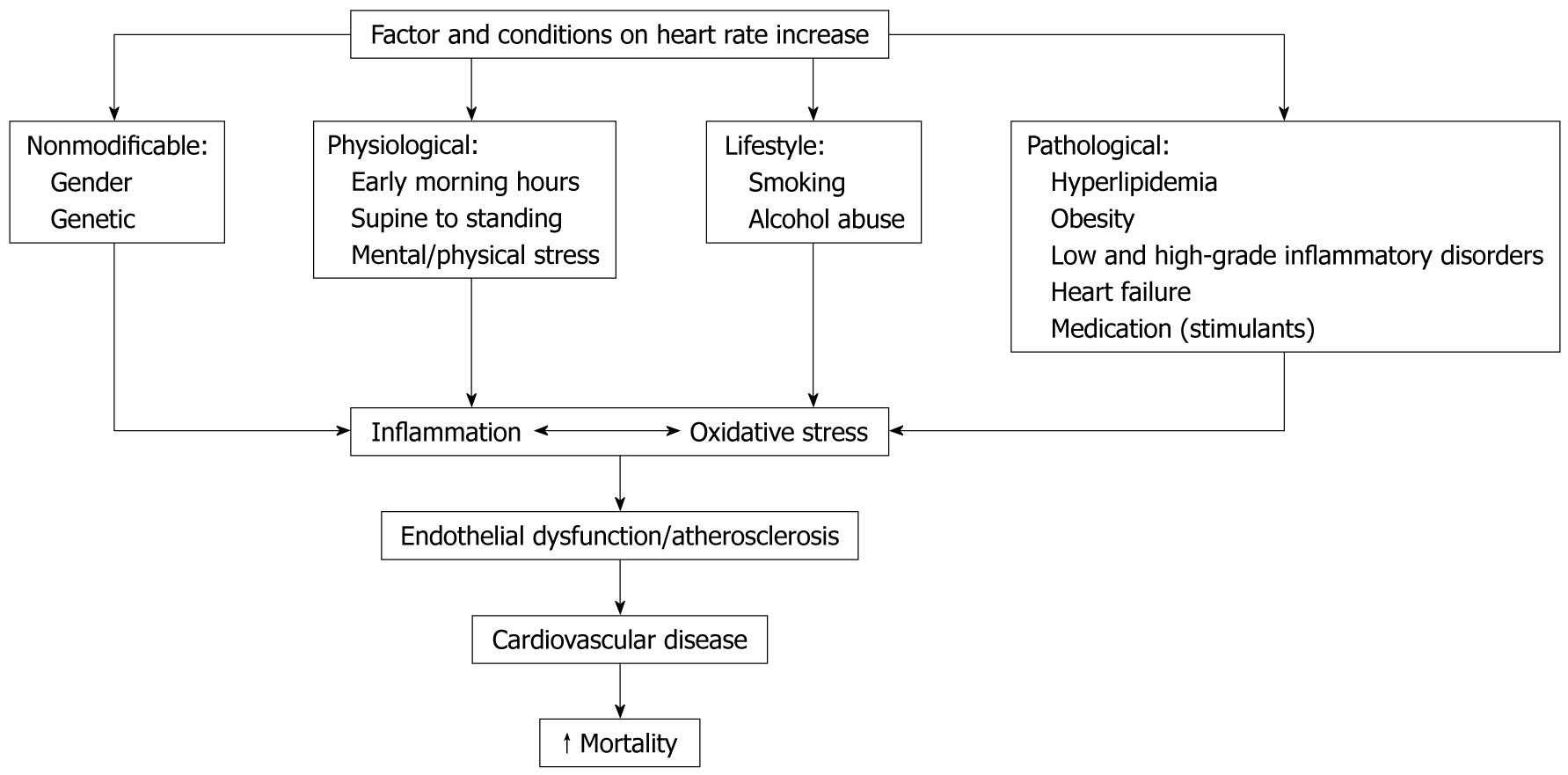
HR is influenced by a variety of physiological processes mainly via effects on the balance of sympathetic and vagal tone. The factors and conditions which influence HR are summarized in Figure 1. The importance of an increased HR in cardiovascular prognosis can be explained by its relationship with major pathophysiological determinants: (1) greater myocardial oxygen consumption; (2) decreased myocardial perfusion; (3) increased severity and progression of coronary atherosclerosis; (4) less development of collaterals; (5) increased risk of coronary plaque disruption; (6) increased arterial rigidity; and (7) a marker and possible mediator of sympathetic overactivity[21].
Figure 1 The role of heart rate in the pathophysiology of cardiovascular disease.
Experimental and clinical evidence also suggests that sustained elevations in HR may also play a direct role in the pathogenesis of coronary atherosclerosis and its complications[2]. Accelerated atherogenesis resulting from increased HR may be due to both mechanical and metabolic factors. Increased vascular wall stress may contribute to endothelial injury, potentially promoting the complex cascade of events leading to increased atherosclerosis[21]. Experimental data also show that a reduction in HR can delay the progression of coronary atherosclerosis in monkeys[22]. Additionally, in young patients with myocardial infarction, there is a strong positive relationship between higher HR and the extent of atherosclerotic coronary lesions[23].
In apolipoprotein E knockout mice, cholesterol-induced atherosclerosis was inhibited by HR reduction with ivabradine[24]. In this study, ivabradine also markedly reduced vascular oxidative stress, nicotinamide adenine dinucleotide phosphate oxidase activity, superoxide production, and lipid peroxidation[24]. Ivabradine also prevented atherogenesis when given simultaneously with a high cholesterol diet, but it was also effective in reducing plaques size when given to animals 4 wk after initiation of a high-cholesterol diet[25]. Presumably, therefore, mechanical load on the vessel wall caused by higher HR might lead to endothelial dysfunction, increased oxidative stress, and enhanced plaque formation, which can be reversed or prevented by the inhibition of If channels and consequent HR reduction with ivabradine[26].
Subclinical inflammation and the concentration of inflammatory markers have shown in many studies to correlate strongly with cardiovascular mortality and morbidity in both healthy subjects and in subjects with known CAD[27,28]. Two population-based studies reported a positive correlation between increased resting HR and markers of inflammation in apparently healthy subjects[29,30]. Thus, increased HR may contribute to endothelial dysfunction by upregulation of inflammatory cytokines[2]. In summary, the data show an association of HR with circulating markers of vascular inflammation.
These observations support the rationale for HR reduction with ivabradine as an intervention to improve endothelial function and to attenuate the progression of atherosclerosis and cardiovascular event prevention[2]. In this respect, the RIVIERA study (randomized, double-blind, placebo-controlled trial of ivabradine in patients with acute coronary syndrome: effects of the If current inhibitor ivabradine on reduction of inflammation markers in patients with acute coronary syndrome), is the first opportunity to investigate whether a pure HR-lowering agent reduces vascular inflammatory stress in patients with acute coronary syndrome[31]. The importance of this study will explore potentially new cardiovascular effects of ivabradine that may be useful for management of these patients. In addition, the use of ivabradine can be further expanded by investigating its mechanism of action in high grade inflammatory disorders in models of inflammation-induced accelerated atherosclerosis leading to a substantial cardiovascular burden[32].
Likewise, the effect of ivabradine had been demonstrated in various clinical trials. In the international trial on the treatment of angina with ivabradine vs atenolol (INITIATIVE), ivabradine was compared with atenolol in a double-blind trial in 939 patients with stable angina randomized to receive ivabradine 5 mg bid for 4 wk and then either 7.5 or 10 mg bid for 12 wk or atenolol 50 mg od for 4 wk and then 100 od for 12 wk. Patients underwent treadmill exercise tests at randomization and after 4 and 16 wk of treatment. Increases in total exercise duration and other exercise test parameters at trough of drug activity were not inferior with ivabradine, suggesting that ivabradine is as effective as atenolol in patients with stable angina[7].
The ASSOCIATE (evaluation of the antianginal efficacy and safety of the association of the If current inhibitor ivabradine with a β-blocker) study was an international, double blind, placebo-controlled trial which investigated the effects of ivabradine in patients with stable angina receiving atenolol[33]. This study clearly demonstrates that ivabradine in patients with stable angina receiving the β-blocker atenolol had a significant long-term improvement in total exercise duration in standardized Bruce protocol exercise testing.
Regarding ivabradine-associated adverse effects, the most frequently encountered (sinus bradycardia and visual disturbances) are related to the drug’s mechanism of action; e.g. inhibition of sinus node If channels and inhibition of h channels in retinal rods and cones, though their density is low[19]. In BEAUTIFUL, the incidence of symptomatic sinus bradycardia was 3%. The rate of visual symptoms (phosphenes, blurred vision, and visual disturbances) was also very low and led to discontinuation in only 0.5% of patients receiving ivabradine vs 0.2% of patients receiving placebo[19].