Published online Mar 26, 2025. doi: 10.4330/wjc.v17.i3.101709
Revised: January 27, 2025
Accepted: February 21, 2025
Published online: March 26, 2025
Processing time: 178 Days and 3.1 Hours
Transcatheter aortic valve replacement (TAVR) can be performed through multiple access sites with the preferred approach being transfemoral. In patients with severe peripheral arterial disease and previous grafts, the safety of transfemoral access via direct graft puncture, especially when performed twice within a short period, remains unclear compared to alternative access methods. We present a case demonstrating the safety and efficacy of direct graft puncture for transfemoral access during balloon aortic valvuloplasty (BAV) and TAVR.
An 82-year-old man presented with dyspnea on exertion. Echocardiogram was significant for severe aortic stenosis. Following a heart team discussion, the patient was scheduled for a balloon valvuloplasty followed by staged TAVR. Based on pre-TAVR computed tomography angiogram, the aortobifemoral graft was deemed as an appropriate access site. Micropuncture needle was used to access the right femoral artery graft, and the sheath was upscaled to 10 Fr. He underwent successful intervention to ostial left anterior descending and left circumflex arteries, and BAV with 22 mm Vida BAV balloon. Hemostasis was achieved using Perclose. For TAVR, an 8 Fr sheath was inserted via the right femoral bypass graft. The arteriotomy was pre-closed with two Perclose ProGlides and access was upsized to 18F Gore DrySeal. A 5Fr sheath was used for left femoral bypass graft access. Patient underwent successful TAVR with 29 mm CoreValve. Hemostasis was successfully achieved using 2 Perclose for right access site and one Perclose for left side with no postoperative bleeding complications.
BAV and TAVR are feasible and safe through a direct puncture of the aortofe
Core Tip: This case report focuses on the safety and efficacy of a direct puncture of an aortofemoral graft for transfemoral access to perform balloon aortic valvuloplasty and a staged transcatheter aortic valve replacement (TAVR) within a short time frame in a patient with severe peripheral arterial disease. While alternative non-femoral access approaches are reasonable, we chose direct graft puncture as the ideal access based on multi-detector computed tomography imaging. This demonstrates the safety of obtaining large-bore catheter access twice through an aortofemoral graft. Our case adds to the literature by exploring the short-term outcomes of puncturing an avascular structure during TAVR in a complex patient. This transfemoral approach may be considered in patients with aortofemoral grafts when general anesthesia or alternative access methods are less desirable.
- Citation: Mustafa A, Wei C, Cinelli M, Khan S, Khan D, Tamburrino F, Maniatis G, Spagnola J. Balloon valvuloplasty and transcatheter aortic valve replacement via aortofemoral bypass grafts: A case report and review of literature. World J Cardiol 2025; 17(3): 101709
- URL: https://www.wjgnet.com/1949-8462/full/v17/i3/101709.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i3.101709
Transcatheter aortic valve replacement (TAVR) is a widely recognized procedure used to treat severe aortic stenosis for high surgical risk patients and can be performed through multiple access sites with the preferred approach being transfemoral. In patients with prior lower limb bypass, few case reports have reported the usefulness and safety of direct graft puncture for transfemoral access[1]. The concerns associated with direct graft puncture include challenges in achieving post-procedural hemostasis leading to hematoma formation, disruption of the anastomosis with subsequent development of pseudoaneurysm, and the risk of graft site infection requiring surgical intervention. However, when performed diligently with proper imaging guidance, accessing a vascular graft for intervention can be achieved with minimal complications. Additionally, femoral hemostasis in patients with femoral grafts using vascular closure devices have been reported to be safe and effective[2,3]. There are several types of vascular closure devices- clip-based, suture-based, disc-based, and plug-based[4]. The use of certain plug-based devices such as Angio-Seal and Mantra, and suture based devices has been published in the literature. Herein, we report a case of successful balloon aortic valvuloplasty (BAV), followed by staged TAVR, both performed via an aortobifemoral bypass graft.
An 82-year-old man presented to ambulatory clinic for dyspnea with exertion for past 5-6 months.
His dyspnea was progressively worsening without any relieving factors and had begun to significantly impair his daily functioning. His symptoms were consistent with New York Heart Association Class III.
His past medical history included hypertension, diabetes mellitus, chronic diastolic heart failure, hyperlipidemia, chronic kidney disease stage 3, coronary artery disease with a drug eluting stent (DES) placed in the proximal left anterior descending (LAD) artery nine years ago, and peripheral arterial disease. His past surgical history includes an aortobifemoral bypass for peripheral arterial disease with polytetrafluoroethylene graft in 1985.
For medications, the patient was taking metoprolol tartrate 50 mg twice daily, aspirin 81 mg daily, amlodipine 5 mg daily, spironolactone 25 mg daily, atorvastatin 40 mg once daily, and 1.5 mg of Soliqua 100/33 subcutaneous injection daily. He was not taking any herbal medication and was adherent to his medications. He had no known allergies. He had no significant family history. He was a former tobacco smoker. He reported smoking three packs of cigarettes daily for five years before quitting 40 years ago. He was a retired engineer and lived with his son and grandchildren. He reported being consistent with a low-salt and low-fat diet.
Physical examination was unremarkable with the exception of 1+ lower extremity edema and grade 3/5 systolic murmur.
His hepatic function was normal (aspartate aminotransferase/alanine aminotransferase were 17 U/L and 18 U/L respectively). His renal function was decreased with a baseline creatinine level of 1.5 mg/dL. Besides the laboratory values listed above, he also had an elevated pro-BNP level of 3093 pg/mL.
An echocardiogram was performed which showed severe aortic stenosis with a peak velocity of 4.0 m/s, mean aortic gradient of 44 mmHg and an aortic valve area of 0.96 cm2. Other findings included a normal ejection fraction of 65%, trace aortic regurgitation, trace mitral regurgitation, and trace tricuspid regurgitation.
Based on the patient’s medical historyand and imaging findings, a diagnosis of severe aortic stenosis was confirmed.
Following a heart team discussion, it was recommended that the patient would need his aortic valve replaced. Subsequently, the patient underwent left heart catheterization (LHC) as part of a TAVR workup. LHC showed 2-vessel coronary artery disease with a 70% ostial LAD lesion, hemodynamically significant by instantaneous wave-free ratio with a value of 0.88. He also had 95% distal left circumflex (LCx) lesion. His society of thoracic surgeons score was 4.361%, and he had Frailty Index of 1. The case was discussed with the cardiothoracic surgery team and considering multiple comor
Computed tomography angiography (CTA) TAVR protocol was performed which showed patency of the aortobife
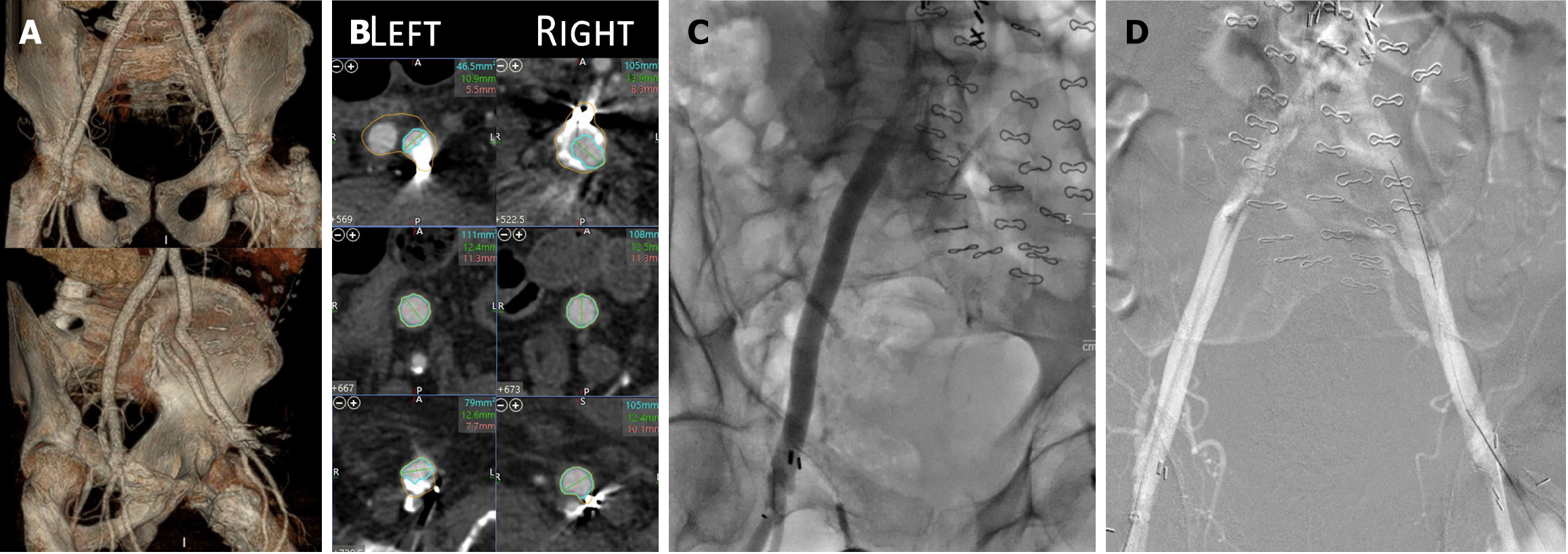
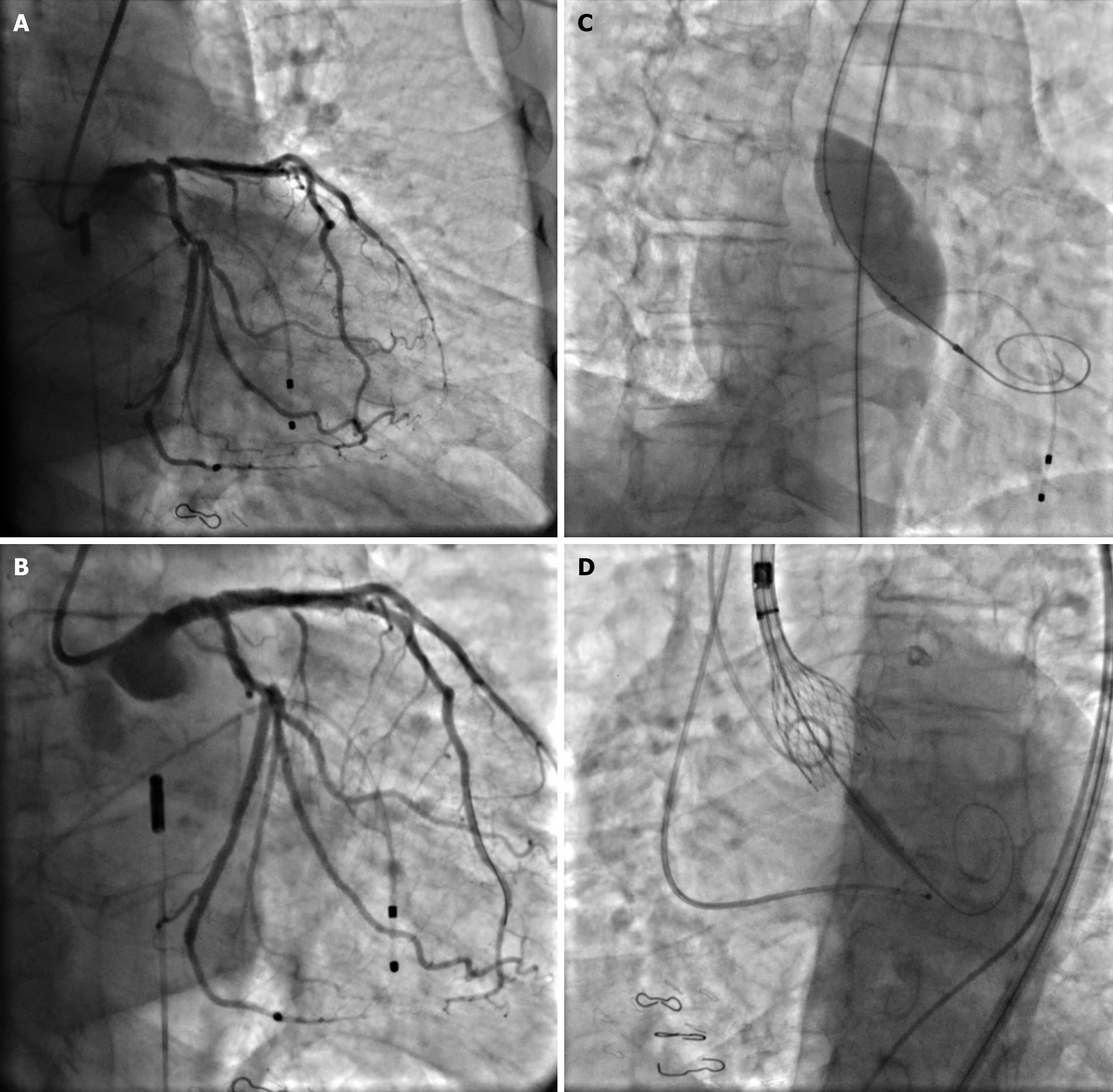
He was scheduled for a complex high-risk and indicated percutaneous coronary intervention (PCI) with intra-aortic balloon pump for mechanical circulatory support and BAV. Based on the pre-TAVR CTA, the aortobifemoral graft was deemed an appropriate access site (Figure 1A and B). Micro puncture needle was used to access the right femoral artery graft at the level of the femoral head using ultrasound and fluoroscopic guidance, and a femoral angiogram was per
Three weeks later, the patient was scheduled for TAVR. Graft patency was assessed using color Doppler on the ultrasound. Ultrasound and fluoroscopic-guided access of the graft was obtained using a micro puncture needle at the level of the femoral head. A femoral angiogram was performed using a micro puncture sheath and an 8 Fr sheath was advanced over the wire. Over Supra Core wire, the arteriotomy was pre-closed with two Perclose ProGlides and access was upsized to 18 Fr Gore Dry Seal after passing serial dilators. A 5Fr sheath was used for left femoral arterial access (Figure 1D). Heparin was administered during the procedure for anticoagulation. The patient underwent a successful TAVR with 29 mm Core Valve (Figure 2D) with post-deployment echocardiogram demonstrating no significant paraval
Following high-risk PCI and BAV, the patient was monitored in the CCU as per standard institutional protocol and remained without any postoperative complications. He was discharged on postoperative day 1. Following TAVR, the post-deployment echocardiogram demonstrated no significant paravalvular leak and low peak and mean gradients across the aortic valve. Postoperative course in the CTU was uneventful with no signs of access site-related complications. On outpatient follow-up, the patient reported significant improvement in symptoms, and no complications were noted at the access site. Follow-up echocardiogram demonstrated findings consistent with the postoperative study, with no significant paravalvular leak and low peak and mean gradients across the aortic valve.
We present a case of high-risk PCI with BAV and staged TAVR being successfully performed using transfemoral access through a direct puncture of an aortobifemoral bypass graft in both procedures. Hemostasis was successfully achieved using Perclose without having postoperative bleeding complications.
In cases with previous aortofemoral grafts, careful pre-TAVR planning is of paramount importance[6]. Multi-detector computed tomography (MDCT) imaging is considered the standard of care and helps with evaluating graft diameter, degree of vessel calcification, and tortuosity[7]. In patients with history of aortofemoral grafts, MDCT can help in determining patency and dimensions of the graft. The minimal graft dimension in our case did not limit the delivery of the sheaths[1]. Furthermore, ultrasound-guided access is the standard of care at our institution and should be used especially in cases with aortofemoral grafts to reduce complications[8].
Multiple studies have highlighted the pros and cons of alternative access for TAVR when transfemoral access is not permissible. Transfemoral access is utilized in at least 85% of TAVRs, as it is the preferred approach because the femoral artery typically provides an adequate diameter for the insertion of the required equipment[9-11]. In both the PARTNER Trial using the Edwards SAPIEN valve and the United States CoreValve Trial using CoreValve, the devices require large bore access, either through transfemoral or the transapical access[12-14]. In addition to transfemoral access, other accesses include transaxillary, transcaval, trans-subclavian, or transcarotid[9,10,15-20]. Each alternative access has their advantages and disadvantages and is limited by the vessel diameter requirement of each device. Transaxillary access was first introduced in 2011 and has become the most frequent alternative access route, alongside transcarotid access[16,21]. In a network meta-analysis, trans-subclavian approaches had more risk for stroke and life-threatening bleeds compared to transfemoral access and transcaval access had the highest rate of major vascular complications compared to transfemoral access[20].
Few case reports describe the usefulness and safety of direct graft puncture of an aortobifemoral grafts (Table 1)[1,22]. Direct graft puncture used to be unpopular due to multiple concerns including inability to achieve hemostasis post-procedure with subsequent hematoma, disruption of the anastomosis and subsequent pseudoaneurysm, and graft site infection necessitating surgical intervention because of the avascular nature of the graft[22]. However, studies have reported complication rates ranging from 0-20% with direct endovascular graft puncture[23,24]. Hence direct graft puncture for arterial access is now presumed to be safe and feasible[22]. In a case study describing two patients with aortofemoral graft undergoing TAVR, no postoperative complications were observed after direct puncture of the graft[1]. Our case is unique for demonstrating that direct graft puncture remains a safe and viable approach even after accessing the same site with a large-bore catheter twice within a short interval between the BAV and the staged TAVR.
| Ref. | Type of graft | Closure devices | Complications |
| Rosseel et al[1] | Two patients had aortobifemoral bypass grafts | Both patients used the same technique- 2. Perclose devices and 1 additional 6Fr Angioseal (Terumo, Shibuya, Tokyo, Japan) | None |
| Wu et al[3] | Aortobifemoral bypass graft | 14F MANTA vascular closure device (Teleflex, Wayne, United States) and 4 Perclose devices | None |
| Ezeh et al[26] | Aortobifemoral bypass graft | 2 Perclose devices | None |
| Geyer et al[27] | Aortobifemoral bypass graft | 18F MANTA vascular closure device (Teleflex, Wayne, United States) | None |
Repeat imaging of the vascular access after a BAV and before TAVR can be reasonable in certain situations. If there is suspicion of pseudoaneurysm or hematoma at the vascular access site, ultrasound imaging would be useful as an initial test. CT imaging is particularly useful in cases where bleeding is suspected, especially if the patient has hemodynamic compromise after the procedure[25]. Without any obvious signs of complication, a repeat imaging is unlikely to have clinical significance.
Multiple steps can be taken to prevent post-operative complications from direct graft puncture for arterial access. The use of ultrasound guidance for access has been shown to help minimize trauma to the graft and ensure graft patency prior to access[24]. After the procedure was finished, a vascular closure device was used to suture the arteriotomy. Vascular closure devices, such as Perclose, have been deemed to be not only as effective as manual compression but also safer with slightly fewer complications. They have proven to be safe alternatives for closing femoral artery puncture sites and prosthetic grafts after TAVR[1,3,26-29].
In case of uncontrolled bleeding, certain bail-out options are available. Similar to routine transfemoral access, an additional Perclose or a collagen-plug vascular closure device such as AngioSeal or Manta can be used[3,27,29-32]. If hemostasis is still unsuccessful, a covered stent or a surgical cutdown can be considered[29,33].
BAV and TAVR are feasible and safe through a direct puncture of the aortobifemoral bypass graft with successful hemostasis using Perclose.
| 1. | Rosseel L, Degrieck I, De Bruyne B, Søndergaard L, De Backer O. Percutaneous Transfemoral TAVR With Direct Puncture and Successful Closure of Aortobifemoral Bypass Graft. CJC Open. 2020;2:34-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Essibayi MA, Cloft H, Savastano LE, Brinjikji W. Safety and efficacy of Angio-Seal device for transfemoral neuroendovascular procedures: A systematic review and meta-analysis. Interv Neuroradiol. 2021;27:703-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Wu MS, Oyetunji S, Don CW. Use of the MANTA Device in Percutaneous Closure of Graft Puncture. J Soc Cardiovasc Angiogr Interv. 2023;2:100565. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Robertson L, Andras A, Colgan F, Jackson R. Vascular closure devices for femoral arterial puncture site haemostasis. Cochrane Database Syst Rev. 2016;3:CD009541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Veenis L, Holierook M, Vis MM, Baan J, Henriques JP. Periprocedural Antibiotic Prophylaxis for Transfemoral Transcatheter Aortic Valve Replacement: A Nationwide Survey in the Netherlands. Struct Heart. 2021;5:328-329. [DOI] [Full Text] |
| 6. | Saadi RP, Tagliari AP, Saadi EK, Miglioranza MH, Polanczyck CA. Preoperative TAVR Planning: How to Do It. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 7. | Bleakley C, Monaghan MJ. The Pivotal Role of Imaging in TAVR Procedures. Curr Cardiol Rep. 2018;20:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Rashid MK, Sahami N, Singh K, Winter J, Sheth T, Jolly SS. Ultrasound Guidance in Femoral Artery Catheterization: A Systematic Review and a Meta-Analysis of Randomized Controlled Trials. J Invasive Cardiol. 2019;31:E192-E198. [PubMed] |
| 9. | Abusnina W, Machanahalli Balakrishna A, Ismayl M, Latif A, Reda Mostafa M, Al-Abdouh A, Junaid Ahsan M, Radaideh Q, Haddad TM, Goldsweig AM, Ben-Dor I, Mamas MA, Dahal K. Comparison of Transfemoral versus Transsubclavian/Transaxillary access for transcatheter aortic valve replacement: A systematic review and meta-analysis. Int J Cardiol Heart Vasc. 2022;43:101156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Dahle TG, Kaneko T, McCabe JM. Outcomes Following Subclavian and Axillary Artery Access for Transcatheter Aortic Valve Replacement: Society of the Thoracic Surgeons/American College of Cardiology TVT Registry Report. JACC Cardiovasc Interv. 2019;12:662-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 132] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 11. | Ramlawi B, Anaya-Ayala JE, Reardon MJ. Transcatheter aortic valve replacement (TAVR): access planning and strategies. Methodist Debakey Cardiovasc J. 2012;8:22-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S; PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5086] [Cited by in RCA: 5506] [Article Influence: 367.1] [Reference Citation Analysis (1)] |
| 13. | Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, Bajwa T, Heiser JC, Merhi W, Kleiman NS, Askew J, Sorajja P, Rovin J, Chetcuti SJ, Adams DH, Teirstein PS, Zorn GL 3rd, Forrest JK, Tchétché D, Resar J, Walton A, Piazza N, Ramlawi B, Robinson N, Petrossian G, Gleason TG, Oh JK, Boulware MJ, Qiao H, Mugglin AS, Reardon MJ; Evolut Low Risk Trial Investigators. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019;380:1706-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2802] [Cited by in RCA: 2663] [Article Influence: 443.8] [Reference Citation Analysis (0)] |
| 14. | Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ; PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187-2198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4547] [Cited by in RCA: 4933] [Article Influence: 352.4] [Reference Citation Analysis (0)] |
| 15. | Chamandi C, Abi-Akar R, Rodés-Cabau J, Blanchard D, Dumont E, Spaulding C, Doyle D, Pagny JY, DeLarochellière R, Lafont A, Paradis JM, Puri R, Karam N, Maes F, Rodriguez-Gabella T, Chassaing S, Le Page O, Kalavrouziotis D, Mohammadi S. Transcarotid Compared With Other Alternative Access Routes for Transcatheter Aortic Valve Replacement. Circ Cardiovasc Interv. 2018;11:e006388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 16. | Harloff MT, Percy ED, Hirji SA, Yazdchi F, Shim H, Chowdhury M, Malarczyk AA, Sobieszczyk PS, Sabe AA, Shah PB, Kaneko T. A step-by-step guide to trans-axillary transcatheter aortic valve replacement. Ann Cardiothorac Surg. 2020;9:510-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Lederman RJ, Greenbaum AB, Khan JM, Bruce CG, Babaliaros VC, Rogers T. Transcaval Access and Closure Best Practices. JACC Cardiovasc Interv. 2023;16:371-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 18. | Munguti C, Ndunda PM, Abukar A, Jawad MA, Vindhyal MR, Fanari Z. Transcarotid versus transfemoral transcatheter aortic valve replacement: A systematic review and meta-analysis. Cardiovasc Revasc Med. 2024;68:92-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 19. | Olivier ME, Di Cesare A, Poncet A, Brasselet C, Metz D, Biancari F, Ruggieri VG; Reims Heart Team Group. Transfemoral versus transcarotid access for transcatheter aortic valve replacement. JTCVS Tech. 2022;15:46-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Yokoyama Y, Sakata T, Mikami T, Misumida N, Scotti A, Takagi H, Sugiura T, Kuno T, Latib A. Vascular access for transcatheter aortic valve replacement: A network meta-analysis. J Cardiol. 2023;82:227-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Gleason TG, Schindler JT, Hagberg RC, Deeb GM, Adams DH, Conte JV, Zorn GL 3rd, Hughes GC, Guo J, Popma JJ, Reardon MJ. Subclavian/Axillary Access for Self-Expanding Transcatheter Aortic Valve Replacement Renders Equivalent Outcomes as Transfemoral. Ann Thorac Surg. 2018;105:477-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 93] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 22. | Eisenberg RL, Mani RL, McDonald EJ. The complication rate of catheter angiography by direct puncture through aorto-femoral bypass grafts. AJR Am J Roentgenol. 1976;126:814-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Cowling MG, Belli AM, Buckenham TM. Evaluation and complications of direct graft puncture in thrombolysis and other interventional techniques. Cardiovasc Intervent Radiol. 1996;19:82-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Katoh H, Nozue T, Michishita I. Direct puncture of the prosthetic bypass graft in the treatment of critical limb ischemia patient undergoing prior axillo-femoral bypass. Cardiovasc Interv Ther. 2013;28:123-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Mach M, Okutucu S, Kerbel T, Arjomand A, Fatihoglu SG, Werner P, Simon P, Andreas M. Vascular Complications in TAVR: Incidence, Clinical Impact, and Management. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 26. | Ezeh E, Amro M, Akhigbe E, Hamilton M, Maru M. Achieving Hemostasis Posttranscatheter Aortic Valve Replacement in a Patient with Aortobifemoral Bypass Graft Using Perclose Device: A Novel Technique. Case Rep Cardiol. 2021;2021:4253570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 27. | Geyer M, Tamm AR, Oberhoffer M, Kreidel F, El Beyrouti H, Münzel T, von Bardeleben RS. Percutaneous puncture of an aorto-bifemoral bypass graft and successful closure with MANTA(®) device in transfemoral TAVR. Echocardiography. 2021;38:506-507. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Lee WA, Brown MP, Nelson PR, Huber TS, Seeger JM. Midterm outcomes of femoral arteries after percutaneous endovascular aortic repair using the Preclose technique. J Vasc Surg. 2008;47:919-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 135] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 29. | Basman C, Kodra A, Mustafa A, Wang D, Cinelli M, Onyebeke K, Rutkin B, Mehla P, Maniatis G, Pirelli L, Goldberg Y, Liu S, Uttar S, Wilson S, Kalimi R, Brinster D, Gandotra P, Koss E, Meraj P, Mihelis E, Supariwala A, Hartman A, Scheinerman SJ, Kliger C; Northwell TAVR Investigators. Collagen-Based Bailout Compared to Suture-Mediated Vascular Closure Alone During Transcatheter Aortic Valve Replacement. J Soc Cardiovasc Angiogr Interv. 2024;3:101929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 30. | Bazarbashi N, Ahuja K, Gad MM, Sammour YM, Kaur M, Karrthik A, Saad AM, Khubber S, Dhaliwal K, Mick SL, Navia JL, Puri R, Reed GW, Krishnaswamy A, Kapadia SR. The utilization of single versus double Perclose devices for transfemoral aortic valve replacement access site closure: Insights from Cleveland Clinic Aortic Valve Center. Catheter Cardiovasc Interv. 2020;96:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Boussofara A, Godin M, Canville A, Baala B, Berland J, Koning R, Landolff Q. Assessment of the MANTA closure device in real-life transfemoral transcatheter aortic valve replacement: A single-centre observational study. Catheter Cardiovasc Interv. 2024;103:650-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 32. | Fan J, Lane W, Lawrence M, Mixon T. Adjunctive use of Angio-Seal closure device following transcatheter aortic valve implantation via percutaneous transfemoral approach with incomplete hemostasis after modified Perclose ProGlide preclosure technique. Proc (Bayl Univ Med Cent). 2019;32:34-36. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 33. | Schahab N, Kavsur R, Mahn T, Schaefer C, Kania A, Fimmers R, Nickenig G, Zimmer S. Endovascular management of femoral access-site and access-related vascular complications following percutaneous coronary interventions (PCI). PLoS One. 2020;15:e0230535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |