Published online Jan 26, 2025. doi: 10.4330/wjc.v17.i1.100782
Revised: December 6, 2024
Accepted: December 27, 2024
Published online: January 26, 2025
Processing time: 147 Days and 23.9 Hours
The estimated annual incidence of out-of-hospital cardiac arrest (OHCA) is appro
Core Tip: Out-of-hospital cardiac arrest is a major health issue globally with substantial mortality rates. Improvement in overall equipment, adequate training of paramedics in order to initiate cardiopulmonary resuscitation (CPR) on-site rather than prioritizing transport to the Emergency Department, building a strong network in paramedicine and new CPR techniques represent several strategies to facilitate successful resuscitation, increase the probability of return to spontaneous circulation and improve survival to hospital discharge and neurological outcomes. Raising awareness and educating the public could also minimize the delays in recognizing cardiac arrest and initiating CPR.
- Citation: Latsios G, Sanidas E, Velliou M, Nikitas G, Bounas P, Parisis C, Synetos A, Toutouzas K, Tsioufis C. Cardiac arrest: Pre-hospital strategies to facilitate successful resuscitation and improve recovery rates. World J Cardiol 2025; 17(1): 100782
- URL: https://www.wjgnet.com/1949-8462/full/v17/i1/100782.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i1.100782
Out-of-hospital cardiac arrest (OHCA) is a major health issue globally. The estimated annual incidence of emergency medical services (EMS) treated OHCA is 67-170 per 100000 inhabitants in Europe, 47 in the United States, 46 in Asia and 51 in Australia[1,2]. Resuscitation is attempted in about 50%-60% of OHCA cases. The rate of bystander cardiopulmonary resuscitation (CPR) varies from 26% to 86% between countries[3] while the automated external defibrillators (AEDs) are rarely used (range 3.8%-59%)[2].
Worldwide, survival rates after OHCA remain low with a substantial country and geographic region variation[4]. The European Registry of Cardiac Arrest Study number 2 project collected and analyzed data across Europe and revealed that among patients with EMS attempted CPR 25% achieved return of spontaneous circulation (ROSC) before delivery to the Emergency Department (ED), 11% were transferred to the ED with ongoing CPR and 64% did not achieve ROSC and were not transferred to the hospital. Overall survival to hospital discharge was approximately 8% (range 0%-18%)[5]. Surprisingly, in China the survival rate after OHCA is almost 1%[6].
Therefore, interventions aiming to strengthen the “chain of survival” before the ED transfer is crucial in order to facilitate successful resuscitation and increase recovery rates. The purpose of this review is to provide pre-hospital stra
Every minute of conventional CPR decreases rapidly the probability of survival to hospital discharge. Time is crucial in OHCA since the chance of survival increases significantly if CPR initiates immediately within the first 3-5 minutes after collapse. Traditional resuscitation strategies seem to be most effective within the first 10-15 minutes. After 15 minutes, the possibility of good functional recovery falls to 2%. It is almost time to apply innovative strategies in suitable candidates that do not immediately respond to chest compressions, defibrillation or epinephrine[7].
Mechanical CPR (mCPR) represents an appealing alternative of conventional CPR as it can provide uninterrupted chest compressions of optimal quality externally, at the appropriate rate and depth. They are not impaired by human fatigue and free team members for other tasks. In the pre-hospital setting, the lack of personnel and the challenge of continuing CPR in a moving ambulance makes mCPR more attractive[8]. Available devices include the Lund University Cardiopulmonary Assist System (LUCAS), the ZOLL Autopulse Resuscitation System and a piston-based mechanism, known as Thumper. The main disadvantages are the need to stop chest compressions for device deployment and the risk of trau
Nonetheless, large randomized controlled trials have demonstrated that mCPR is not superior to manual CPR in improving survival and achieving ROSC. The Prehospital Assessment of the Role of Adrenaline: Measuring the Effectiveness of Drug Administration in Cardiac Arrest (PARAMEDIC) trial compared LUCAS-2 to conventional CPR and revealed that mCPR did not improve 30-day survival among 4471 patients receiving resuscitation for non-traumatic OHCA[10]. Likewise, the Circulation Improving Resuscitation Care trial showed that both mechanical and manual CPR resulted in equivalent survival to hospital discharge[11]. Hence, current guidelines do not support the routine use of mCPR in the pre-hospital setting[12].
Extracorporeal membrane oxygenation (ECMO) is a mechanical circulation support device that has been utilized following refractory OHCA. Refractory OHCA is defined as the absence of ROSC despite appropriate CPR for 15-30 minutes. The incorporation of ECMO during CPR is referred as extracorporeal CPR (ECPR). ECPR is a complex inter
Data regarding the impact of ECPR in survival among OHCA cases is controversial. The ARREST trial compared the efficacy and safety of early ECMO-facilitated resuscitation to traditional resuscitation in 30 OHCA patients with refractory VF, no ROSC after three shocks, mCPR with LUCAS and estimated transfer time to the ED < 30 minutes. The results revealed that survival to hospital discharge was greater in the ECPR group (43% vs 7%). Only 2 out of 15 patients failed to achieve ROSC in the ECMO-facilitated resuscitation group compared to 13 out of 15 patients in the standard advanced life support (ALS) group. Notably, no serious device-related adverse events were recorded[15]. On the other hand, a prospective registry from France found that survival was almost similar among patients receiving ECPR and those receiving conventional CPR (8% vs 9%) while achieving ROSC was less likely in the ECPR group (26% vs 38%)[16,17]. Likewise, the multicenter, randomized, controlled trial INCEPTION (Early Initiation of Extracorporeal Life Support in Refractory OHCA) from the Netherlands that included patients with refractory OHCA and an initial ventricular arrhythmia showed that the overall success rate of ROSC was 26% in the extracorporeal CPR group vs 31% in the conventional CPR group. The mean interval between the emergency call and ROSC was much lower among OHCA patients receiving conventional CPR (43 minutes ± 20 minutes vs 49 minutes ± 19 minutes). Six-month survival with favorable neurologic outcomes did not differ between the two groups[18]. The 2021 European Resuscitation Council (ERC) Guide
Public access to AED (i.e. casinos, airports, squares, town halls, stadiums etc.) to be used on-site by random bystanders can significantly increase survival in OHCA events to 40%-60%[19-22]. Recommendations to deploy AED in public areas were first published in 1992 by the American Heart Association (AHA) and six years later by the ERC. Since then, several efforts have been made to install AEDs in locations where they are easily visible and accessible[23,24].
During the last decades, additional strategies for public access and early defibrillation have developed. First responder programs including police officers, fire fighters, off-duty healthcare providers and community citizens equipped by AEDs to be dispatched in parallel with paramedics has been suggested as a solution for early CPR and defibrillation, especially in areas not covered by on-site AEDs[25,26]. A recent observational study of 27 European regions showed that areas with dispatching first responders had a significantly higher rate of ROSC (36% vs 24%) and survival (13% vs 5%) compared to regions without[27]. On the other hand, the Swedish AED and Mobile Bystander Activation trial investigated whether a smartphone application, called Heartrunner, could increase the use of AEDs in OHCA. CPR-trained volunteer responders accepted the alert in their phone and then either they were guided to collect the nearest available AED on the way and go directly to the OHCA patient or they received instructions to go directly to the OHCA case and start CPR. The study concluded that these two approaches did not impair the bystander AED use[28]. Possibly, first responder programs might have a better impact in areas with delayed EMS response such as rural areas.
Another solution to improve public access is to deliver the AED by a drone. Drones are promising and innovative tools that fly quickly and cover large and not easily reached regions maximizing bystander access to equipment[25,29]. Investigators from Canada conducted six simulations with AED-equipped drones and found that the response time was 1.8-8.0 minutes faster compared to the ambulance[30]. Another study from Sweden revealed a 92% successful AED delivery rate. Moreover, in 61% of OHCA cases the drones arrived before ambulances with a time benefit of one minute and 61 seconds[31]. Even though AED-equipped drones could improve access to early defibrillation and overcome barriers of spatial distance, drone flights are not allowed in most countries due to safety issues.
In addition, creating an AED Network with an AEDs deployment plan that provides information about AEDs locations and guide bystanders to the nearest accessible device could improve public defibrillation access and recovery rates. A study of 35 OHCA simulations in a university campus showed that the median AED retrieval time was shorter when the bystander received directional assistance[32].
Last but not least, the impedance threshold device (ITD) is a valve connected to a facemask or tracheal tube and prevents respiratory gases to enter the lungs during the recoil phase of chest compressions lowering the intrathoracic pressure in a patient on cardiac arrest. Hence, this device increases the preload and improves the blood flow to brain and other vital organs during CPR[33]. A post hoc analysis of Resuscitation Outcomes Consortium Prehospital Resuscitation Impedance Valve and Early Versus Delayed Analysis (ROC PRIMED) trial showed that an ITD combined with conventional CPR was associated with a greater likelihood of survival to hospital discharge with favorable neurological function compared to traditional resuscitation without an ITD (11.9% vs 7.4%)[34]. Another sub-study of ROC PRIMED trial showed that the quality of CPR represents an important modifier of OHCA clinical outcomes when an ITD is used[35].
Paramedics often work in two-member crews and represent a vital link in the chain or survival as they are in the front line and responsible for initiating CPR on-site in a patient on OHCA[36]. Notably, there is evidence supporting that continued on-scene resuscitation (“stay and play”) increases the chance of survival rather than prioritizing transport to the ED (“load and go”). A sub-analysis of the ROC Cardiac Epidemiologic Registry-Cardiac Arrest OHCA registry showed that among those treated on the scene 40% achieved ROSC and 12.6% survived to hospital discharge. In the group of patients that were transported to the hospital with resuscitation en-route, only 16% achieved ROSC and only 3.8% survived to hospital discharge. In addition, on-site resuscitation was associated with better neurological outcomes compared to intra-arrest transport[37]. A more recent study found that on-scene ALS interventions in traumatic OHCA, such as airway management, vascular access and chest decompression, increased the probability of ROSC before the ED arrival[38]. Therefore, achieving ROSC and survival can be improved if paramedics are adequately trained to initiate resuscitation of good quality on-site in an OHCA patient prior to rapid transport emphasizing on technical and non-technical skills[36].
The use of medical emergency motorcycles could also reduce the response time that is crucial for a patient in cardiac arrest[39]. Even though motorcycles lack patient transport capabilities, the better response time compared to ambulances has been correlated with a greater chance of survival and favorable neurological outcomes. A study from Ljubljana evaluated the impact of a motorcycle paramedic (MP) project on survival among OHCA cases compared to an emergency medical team (EMT) arriving at the scene with a dedicated vehicle. In the MP group, the response time was significantly shorter (7.7 minutes ± 4.1 minutes vs 9.9 minutes ± 6.5 minutes), ROSC was achieved in 16 patients before the EMT arrived and the survival to hospital discharge was higher (18.7% vs 13.0%)[40]. Nevertheless, compared to enclosed ambulance drivers, motorcycle riders are more vulnerable to traffic crashes and weather conditions[41].
Furthermore, the presence of a physician in car ambulances seems to be beneficial for the pre-hospital resuscitation in OHCA. A study from Japan found that ambulance crews staffed with a physician were associated with a higher incidence of ROSC before hospital arrival and a greater 1-month survival[42]. The physician is familiar to advanced procedures such as airway management and electrogram analysis and has also better compliance with guidelines compared to other ambulance personnel[43].
Emergency dispatch centers dedicated to OHCA could provide instructions in lay rescues by phone until professional rescuers assume care[44]. Telecommunicators represent the first responders and are trained to help bystanders to recognize cardiac arrest and start CPR. They coach lay persons to maintain the appropriate rate and depth of chest compressions[45]. Additionally, they have the potential to provide phycological support encouraging the bystanders to remain calm until field personnel arrives[44]. Telephone CPR programs seem to improve survival and functional outcomes[46].
Adrenaline is considered a key component in cardiac resuscitation and ALS algorithms in both shockable and non-shockable rhythms. The PARAMEDIC2 study found that patients in the adrenaline group had a greater chance of achieving ROSC (36.3% vs 11.7%) and ED arrival (50.8% vs 30.7%). However, no significant difference in the rate of favorable neurological outcomes between the two groups was recorded[47]. A meta-analysis of 24 studies showed that the early administration of adrenaline in the pre-hospital setting increased both ROSC and favorable neurological out
Finally, advanced prehospital airway management, including endotracheal intubation and the use of supraglottic airway devices, to secure the airway in OHCA patients remains a controversial subject[51]. Although more advanced airway interventions are performed over the recent years, probably due to the increasing number of physicians in the prehospital care, it is not clear yet the effect on survival and neurological outcomes compared to the conventional bag-valve-mask ventilation[52,53]. A study from Japan showed that advanced airway management performed within 15 minutes after initiating CPR was correlated with better 1-month survival in non-shockable rhythms, but not in shockable rhythms. However, no significant association between this intervention and neurological outcomes was recorded in both shockable and non-shockable rhythms[54,55]. It is encouraged clinicians in the prehospital setting to choose the airway management strategy based on their skills and available resources without delaying other crucial interventions such as high quality chest compressions, rapid defibrillation and management of cardiac arrest reversible causes[56].
In OHCA the role of lay bystander is critical. Bystander CPR is defined as CPR (chest compressions with or without ventilations) provided by any person that is not part of the organized EMS and happens to be near the OHCA patient while emergency personnel is en route. Available data indicates that immediate bystander resuscitation is correlated with increased survival and better neurological outcomes[57,58].
However, only 35%-40% of OHCA cases receive bystander CPR globally. Despite the broad efforts to increase public CPR training, it is estimated that no more that 20% of the general public attends a CPR training seminar at least once in a lifetime[58]. A cross-sectional telephone survey in the United States showed that 18% had been trained in CPR within the past two years and 65% had been trained at some point previously. Older age, lesser educational attainment and lower household income were associated with decreased possibility of training[59].
The aim of CPR training is to prepare each candidate to recognize the signs of cardiac arrest and acquire the knowledge and skills to provide chest compressions and use an AED. As it concerns the length of such a course, there is evidence that a 30-minute CPR and AED training session is as effective as traditional multi-hour courses and trainees can maintain their skills even after a 6-month period[60]. Except the basic life support (BLS) seminars, there are novel approaches for training such as video-based training, virtual CPR and smartphone CPR workshops that show potential to increase the number of bystanders who initiate resuscitation in an OHCA patient[59].
Given that recognizing cardiac arrest is challenging, even for trained citizens, it is essential not only to focus on education, but also to explore the application of advanced technologies to address this issue. In this context, the use of health sensors in wearable devises that measure physiological parameters have emerged as a novel intervention for OHCA detection and alarming, especially in patients with unwitnessed cardiac arrest[61]. The DETECT-1 study deve
In addition, integrating CPR/AED training into school curriculums enables students to learn the lifesaving skills of chest compressions and AED use[63]. In 2015, the World Health Organization endorsed the “Kids-Save-Lives” statement recommending a 2-hour education program in CPR for all school children, beginning at the age of 12 years[64]. In 2020, ERC published a position statement on schoolteachers’ education in CPR in order to become instructors for their schoolchildren. Schoolteachers have experience in teaching children, and they can teach school students as effectively as any healthcare provider[65]. In 2023, a new scientific statement from the International Liaison Committee on Resuscitation, the AHA and the ERC supported that children are highly motivated to learn BLS skills even from the age of four[66].
Although OHCA patients with a shockable rhythm have a greater chance of achieving ROSC compared to patients with a non-shockable rhythm, refractory VF defined as VF despite multiple defibrillation attempts is associated with decreased survival. In such cases, further defibrillation without changing the defibrillation technique is usually ineffective[67].
Double sequential external defibrillation (DSED) and vector-change defibrillation (VCD) represent alternative AED strategies that have been used as last-resort therapeutic options for patients with refractory VF. In DSED approach, two sets of defibrillator patches are placed in different positions (anterior–lateral and anterior–posterior) and the shocks are provided almost simultaneously with a delay of at least 1-2 seconds[67]. In VCD technique, the defibrillation pads are moved from the anterior–lateral to the anterior–posterior position to change the vector of the shock and defibrillate a part of the ventricles that might not be completely defibrillated in the anterior–lateral plane[68].
The current evidence regarding the efficacy of these techniques is still inconclusive. The DOSE VF (DSED for refractory VF) trial aimed at comparing the aforementioned ADE approaches with the standard ADE strategy among 405 OHCA patients with refractory VF. The results revealed that DSED and VCD were associated with greater survival to hospital discharge (DSED: 30.4%, VCD: 21.7%, standard approach: 13.3%). Moreover, in the DSED group more patients had favorable neurological outcomes compared to the standard group[68]. However, a meta-analysis of seven studies showed that survival to ED admission, survival to hospital discharge, ROSC and neurological outcomes were similar irrespective of the defibrillation strategy[69].
The head-up CPR method, in which the head and chest are elevated during CPR, has emerged as a novel resuscitation technique that uses gravity to improve venous drainage, increase blood flow to the brain and lower intracranial pressure. This approach has been correlated with increased survival rates in OHCA patients with non-shockable rhythms[70]. A meta-analysis of seven experimental studies showed that the head-up CPR was associated with better cerebral and coronary perfusion compared to the supine CPR[71]. A prospective observational registry of 227 OHCA patients resuscitated while using an ITD and placed in a device-assisted controlled elevation of the head and thorax showed that ROSC was achieved in 34% of them. The ROSC benefit was time-sensitive and declined by 5.6% for every minute elapsed[72].
Rapid detection of cardiac arrest represents the first step in the chain of survival and delays in recognizing such a patient might contribute to lower recovery rates. A study analyzed bystander perception capabilities on OHCA and found that 50% did not recognize cardiac arrest[73].
Raising public awareness on cardiac arrest through action days and campaigns represent a pre-hospital strategy that can lead to an increase in resuscitation rates by lay persons and improve outcomes[74]. For example, on October 16th every year takes place the European Restart a Heart Day and serves as a reminder of the importance of CPR training in saving lives[75]. The first week of June has been recognized as Cardiac Arrest Awareness Week and events are organized targeting to improve public knowledge on CPR and AED use[74]. Recently, the “Get Trained, Save Lives” CPR campaign from the collaboration between Union of European Football Associations (UEFA) and ERC aimed to encourage football fans to learn resuscitation and received extra attention during EURO 2024 in Germany. The campaign’s message was visible to all EURO fans on LED boards in the stadium and courses were organized to train players, coaches, referees, officials and staff at various UEFA tournaments[76].
Cardiac arrest centers represent well-resourced hospitals with fully trained medical and nursing staff, advanced technology and access to certain facilities such as 24/7 PCI, neuroprognostication, intensive care, targeted temperature management and imaging modalities. According to the 2021 guidelines published by ERC and European Society of Intensive Care Medicine, patients with non-traumatic OHCA should be considered for delivery to a cardiac arrest center[77].
However, there is low certainty of evidence that delivering pre-hospital resuscitated patients in such specialized centers could improve survival and neurological outcomes. A meta-analysis of 17 observational studies revealed that even though post-resuscitation care in a cardiac arrest center increased survival to hospital discharge with favorable neurological outcomes, the likelihood of 30-day survival was similar between specialized centers and other hospitals[78]. Currently, the AREST trial found that transferring patients with ROSC after OHCA to a cardiac arrest center did not affect mortality[79].
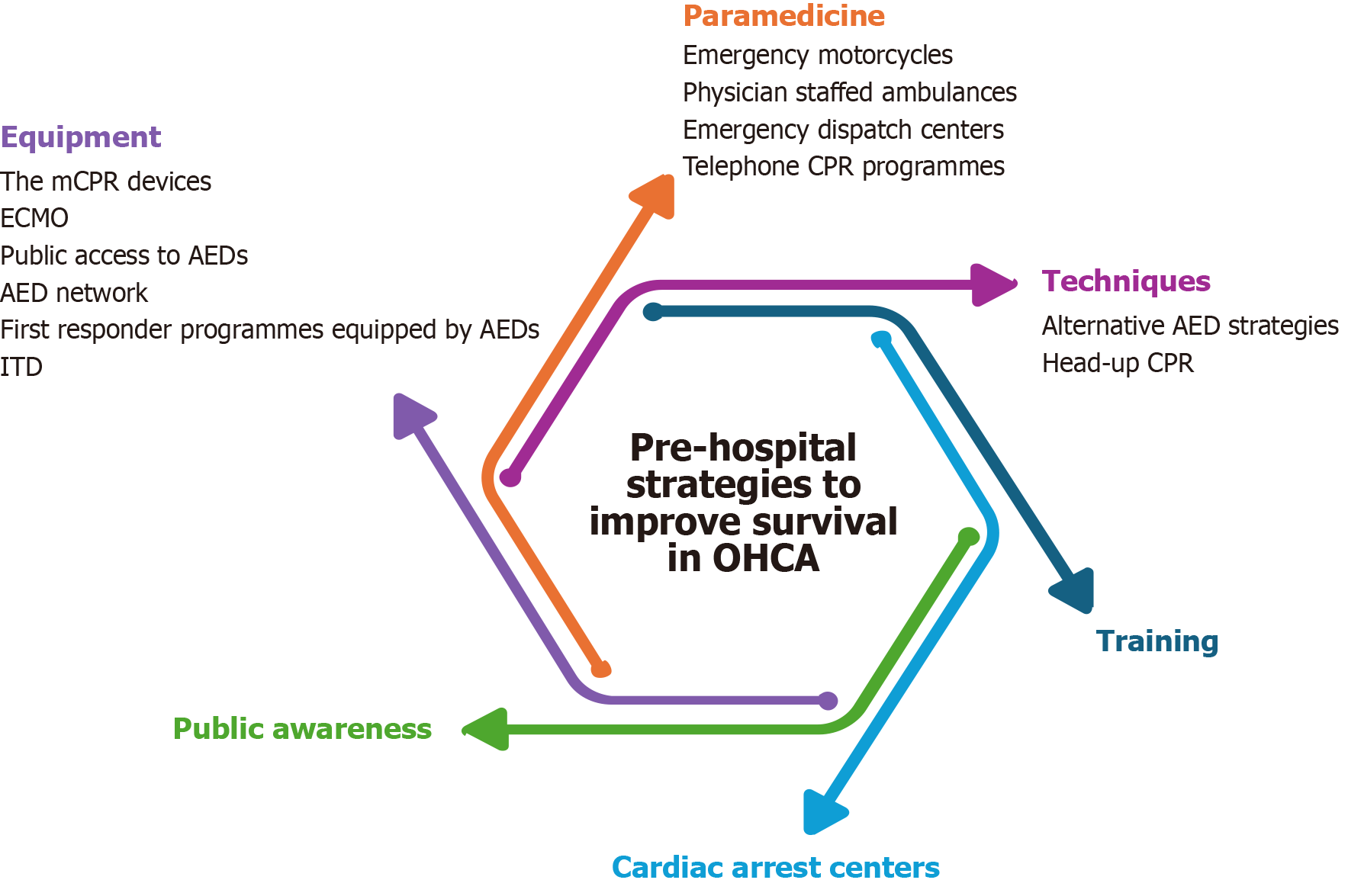
Figure 1 illustrates the main pillars for successful resuscitation and better outcomes among OHCA patients in the pre-hospital setting.
OHCA is a time-sensitive emergency, and every minute of CPR delay decreases the chance of survival and ROSC. Adequate equipment including mCPR devices, ECMO and ITD, an AED network, first responder programs equipped by AEDs and new CPR techniques represent several strategies to facilitate resuscitation and increase survival to hospital discharge in the pre-hospital setting. The presence of a well-functioning pre-hospital EMS is of paramount importance in improving outcomes. Raising awareness and educating the public represent methods to minimize the delays in recog
| 1. | Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81:1479-1487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1588] [Cited by in RCA: 1467] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 2. | Gräsner JT, Herlitz J, Tjelmeland IBM, Wnent J, Masterson S, Lilja G, Bein B, Böttiger BW, Rosell-Ortiz F, Nolan JP, Bossaert L, Perkins GD. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation. 2021;161:61-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 391] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 3. | Kiguchi T, Okubo M, Nishiyama C, Maconochie I, Ong MEH, Kern KB, Wyckoff MH, McNally B, Christensen EF, Tjelmeland I, Herlitz J, Perkins GD, Booth S, Finn J, Shahidah N, Shin SD, Bobrow BJ, Morrison LJ, Salo A, Baldi E, Burkart R, Lin CH, Jouven X, Soar J, Nolan JP, Iwami T. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. 2020;152:39-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 367] [Article Influence: 73.4] [Reference Citation Analysis (0)] |
| 4. | Riess ML. New Developments in Cardiac Arrest Management. Adv Anesth. 2016;34:29-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Gräsner JT, Wnent J, Herlitz J, Perkins GD, Lefering R, Tjelmeland I, Koster RW, Masterson S, Rossell-Ortiz F, Maurer H, Böttiger BW, Moertl M, Mols P, Alihodžić H, Hadžibegović I, Ioannides M, Truhlář A, Wissenberg M, Salo A, Escutnaire J, Nikolaou N, Nagy E, Jonsson BS, Wright P, Semeraro F, Clarens C, Beesems S, Cebula G, Correia VH, Cimpoesu D, Raffay V, Trenkler S, Markota A, Strömsöe A, Burkart R, Booth S, Bossaert L. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 534] [Article Influence: 106.8] [Reference Citation Analysis (0)] |
| 6. | Shao F, Li CS, Liang LR, Li D, Ma SK. Outcome of out-of-hospital cardiac arrests in Beijing, China. Resuscitation. 2014;85:1411-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | Reynolds JC, Frisch A, Rittenberger JC, Callaway CW. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation. 2013;128:2488-2494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 284] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 8. | Latsios G, Leopoulou M, Synetos A, Karanasos A, Papanikolaou A, Bounas P, Stamatopoulou E, Toutouzas K, Tsioufis K. Cardiac arrest and cardiopulmonary resuscitation in "hostile" environments: Using automated compression devices to minimize the rescuers' danger. World J Cardiol. 2023;15:45-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 9. | Mitchell OJL, Shi X, Abella BS, Girotra S. Mechanical Cardiopulmonary Resuscitation During In-Hospital Cardiac Arrest. J Am Heart Assoc. 2023;12:e027726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Perkins GD, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, Lamb SE, Slowther AM, Woollard M, Carson A, Smyth M, Whitfield R, Williams A, Pocock H, Black JJ, Wright J, Han K, Gates S; PARAMEDIC trial collaborators. Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet. 2015;385:947-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 334] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 11. | Wik L, Olsen JA, Persse D, Sterz F, Lozano M Jr, Brouwer MA, Westfall M, Souders CM, Malzer R, van Grunsven PM, Travis DT, Whitehead A, Herken UR, Lerner EB. Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial. Resuscitation. 2014;85:741-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 226] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 12. | Perkins GD, Graesner JT, Semeraro F, Olasveengen T, Soar J, Lott C, Van de Voorde P, Madar J, Zideman D, Mentzelopoulos S, Bossaert L, Greif R, Monsieurs K, Svavarsdóttir H, Nolan JP; European Resuscitation Council Guideline Collaborators. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation. 2021;161:1-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 315] [Article Influence: 78.8] [Reference Citation Analysis (1)] |
| 13. | Wengenmayer T, Tigges E, Staudacher DL. Extracorporeal cardiopulmonary resuscitation in 2023. Intensive Care Med Exp. 2023;11:74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 14. | Richardson ASC, Tonna JE, Nanjayya V, Nixon P, Abrams DC, Raman L, Bernard S, Finney SJ, Grunau B, Youngquist ST, McKellar SH, Shinar Z, Bartos JA, Becker LB, Yannopoulos D, Bˇelohlávek J, Lamhaut L, Pellegrino V. Extracorporeal Cardiopulmonary Resuscitation in Adults. Interim Guideline Consensus Statement From the Extracorporeal Life Support Organization. ASAIO J. 2021;67:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 276] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 15. | Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, Collins G, Zhang L, Kalra R, Kosmopoulos M, John R, Shaffer A, Frascone RJ, Wesley K, Conterato M, Biros M, Tolar J, Aufderheide TP. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396:1807-1816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 668] [Article Influence: 133.6] [Reference Citation Analysis (0)] |
| 16. | Bougouin W, Cariou A, Jouven X. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: do not neglect potential for organ donation! Eur Heart J. 2020;41:3588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Bougouin W, Dumas F, Lamhaut L, Marijon E, Carli P, Combes A, Pirracchio R, Aissaoui N, Karam N, Deye N, Sideris G, Beganton F, Jost D, Cariou A, Jouven X; Sudden Death Expertise Center investigators. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J. 2020;41:1961-1971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 18. | Suverein MM, Delnoij TSR, Lorusso R, Brandon Bravo Bruinsma GJ, Otterspoor L, Elzo Kraemer CV, Vlaar APJ, van der Heijden JJ, Scholten E, den Uil C, Jansen T, van den Bogaard B, Kuijpers M, Lam KY, Montero Cabezas JM, Driessen AHG, Rittersma SZH, Heijnen BG, Dos Reis Miranda D, Bleeker G, de Metz J, Hermanides RS, Lopez Matta J, Eberl S, Donker DW, van Thiel RJ, Akin S, van Meer O, Henriques J, Bokhoven KC, Mandigers L, Bunge JJH, Bol ME, Winkens B, Essers B, Weerwind PW, Maessen JG, van de Poll MCG. Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest. N Engl J Med. 2023;388:299-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 272] [Article Influence: 136.0] [Reference Citation Analysis (0)] |
| 19. | Gantzel Nielsen C, Andelius LC, Hansen CM, Blomberg SNF, Christensen HC, Kjølbye JS, Tofte Gregers MC, Ringgren KB, Folke F. Bystander interventions and survival following out-of-hospital cardiac arrest at Copenhagen International Airport. Resuscitation. 2021;162:381-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 20. | Bækgaard JS, Viereck S, Møller TP, Ersbøll AK, Lippert F, Folke F. The Effects of Public Access Defibrillation on Survival After Out-of-Hospital Cardiac Arrest: A Systematic Review of Observational Studies. Circulation. 2017;136:954-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 148] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 21. | Miyako J, Nakagawa K, Sagisaka R, Tanaka S, Takeuchi H, Takyu H, Tanaka H. Association between bystander intervention and emergency medical services and the return of spontaneous circulation in out-of-hospital cardiac arrests occurring at a train station in the Tokyo metropolitan area: A retrospective cohort study. Resusc Plus. 2023;15:100438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 22. | Miyako J, Nakagawa K, Sagisaka R, Tanaka S, Takeuchi H, Takyu H, Tanaka H. Neurological outcomes of out-of-hospital cardiac arrest occurring in Tokyo train and subway stations. Resusc Plus. 2021;8:100175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 23. | Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part II. Adult basic life support. JAMA. 1992;268:2184-2198. [PubMed] [DOI] [Full Text] |
| 24. | Bossaert L, Handley A, Marsden A, Arntz R, Chamberlain D, Ekström L, Evans T, Monsieurs K, Robertson C, Steen P. European Resuscitation Council guidelines for the use of automated external defibrillators by EMS providers and first responders: A statement from the Early Defibrillation Task Force, with contributions from the Working Groups on Basic and Advanced Life Support, and approved by the Executive Committee. Resuscitation. 1998;37:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Folke F, Shahriari P, Hansen CM, Gregers MCT. Public access defibrillation: challenges and new solutions. Curr Opin Crit Care. 2023;29:168-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 26. | Jonsson M, Berglund E, Müller MP. Automated external defibrillators and the link to first responder systems. Curr Opin Crit Care. 2023;29:628-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 27. | Oving I, de Graaf C, Masterson S, Koster RW, Zwinderman AH, Stieglis R, AliHodzic H, Baldi E, Betz S, Cimpoesu D, Folke F, Rupp D, Semeraro F, Truhlar A, Tan HL, Blom MT; ESCAPE-NET Investigators. European first responder systems and differences in return of spontaneous circulation and survival after out-of-hospital cardiac arrest: A study of registry cohorts. Lancet Reg Health Eur. 2021;1:100004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 28. | Berglund E, Hollenberg J, Jonsson M, Svensson L, Claesson A, Nord A, Nordberg P, Forsberg S, Rosenqvist M, Lundgren P, Högstedt Å, Riva G, Ringh M. Effect of Smartphone Dispatch of Volunteer Responders on Automated External Defibrillators and Out-of-Hospital Cardiac Arrests: The SAMBA Randomized Clinical Trial. JAMA Cardiol. 2023;8:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 29. | Liu X, Yuan Q, Wang G, Bian Y, Xu F, Chen Y. Drones delivering automated external defibrillators: A new strategy to improve the prognosis of out-of-hospital cardiac arrest. Resuscitation. 2023;182:109669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 30. | Cheskes S, McLeod SL, Nolan M, Snobelen P, Vaillancourt C, Brooks SC, Dainty KN, Chan TCY, Drennan IR. Improving Access to Automated External Defibrillators in Rural and Remote Settings: A Drone Delivery Feasibility Study. J Am Heart Assoc. 2020;9:e016687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 31. | Schierbeck S, Hollenberg J, Nord A, Svensson L, Nordberg P, Ringh M, Forsberg S, Lundgren P, Axelsson C, Claesson A. Automated external defibrillators delivered by drones to patients with suspected out-of-hospital cardiac arrest. Eur Heart J. 2022;43:1478-1487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 32. | Johnson AM, Cunningham CJ, Zégre-Hemsey JK, Grewe ME, DeBarmore BM, Wong E, Omofoye F, Rosamond WD. Out-of-Hospital Cardiac Arrest Bystander Defibrillator Search Time and Experience With and Without Directional Assistance: A Randomized Simulation Trial in a Community Setting. Simul Healthc. 2022;17:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Langhelle A, Strømme T, Sunde K, Wik L, Nicolaysen G, Steen PA. Inspiratory impedance threshold valve during CPR. Resuscitation. 2002;52:39-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Sugiyama A, Duval S, Nakamura Y, Yoshihara K, Yannopoulos D. Impedance Threshold Device Combined With High-Quality Cardiopulmonary Resuscitation Improves Survival With Favorable Neurological Function After Witnessed Out-of-Hospital Cardiac Arrest. Circ J. 2016;80:2124-2132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 35. | Yannopoulos D, Aufderheide TP, Abella BS, Duval S, Frascone RJ, Goodloe JM, Mahoney BD, Nadkarni VM, Halperin HR, O'Connor R, Idris AH, Becker LB, Pepe PE. Quality of CPR: An important effect modifier in cardiac arrest clinical outcomes and intervention effectiveness trials. Resuscitation. 2015;94:106-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 36. | Cormack S, Scott S, Stedmon A. Non-Technical Skills in Out-of-Hospital Cardiac Arrest Management: A Scoping Review. AJP. 2020;17:1-8. [DOI] [Full Text] |
| 37. | Grunau B, Kime N, Leroux B, Rea T, Van Belle G, Menegazzi JJ, Kudenchuk PJ, Vaillancourt C, Morrison LJ, Elmer J, Zive DM, Le NM, Austin M, Richmond NJ, Herren H, Christenson J. Association of Intra-arrest Transport vs Continued On-Scene Resuscitation With Survival to Hospital Discharge Among Patients With Out-of-Hospital Cardiac Arrest. JAMA. 2020;324:1058-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 161] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 38. | Smida T, Price BS, Scheidler J, Crowe R, Wilson A, Bardes J. Stay and play or load and go? The association of on-scene advanced life support interventions with return of spontaneous circulation following traumatic cardiac arrest. Eur J Trauma Emerg Surg. 2023;49:2165-2172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 39. | Apiratwarakul K, Phungoen P, Cheung LW, Tiamkao S, Suzuki T, Pearkao C, Ienghong K. Optimizing Operation Time and Travel Distance for Motorcycle Ambulances in Emergency Medical Services. Prehosp Disaster Med. 2023;38:88-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 40. | Škufca Sterle M, Podbregar M. A Motorcycle Paramedic Increases the Survival Rate of Patients after OHCA. Medicina (Kaunas). 2023;59:1708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 41. | Sharwood LN, Kifley A, Craig A, Gopinath B, Jagnoor J, Cameron ID. Comparison of physical and psychological health outcomes for motorcyclists and other road users after land transport crashes: an inception cohort study. BMC Public Health. 2021;21:1983. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Hagihara A, Hasegawa M, Abe T, Nagata T, Nabeshima Y. Physician presence in an ambulance car is associated with increased survival in out-of-hospital cardiac arrest: a prospective cohort analysis. PLoS One. 2014;9:e84424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 43. | Olasveengen TM, Lund-Kordahl I, Steen PA, Sunde K. Out-of hospital advanced life support with or without a physician: effects on quality of CPR and outcome. Resuscitation. 2009;80:1248-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 44. | Yacobis-Cervantes TR, García-Méndez JA, Leal-Costa C, Castaño-Molina MÁ, Suárez-Cortés M, Díaz-Agea JL. Telephone-Cardiopulmonary Resuscitation Guided by a Telecommunicator: Design of a Guiding Algorithm for Telecommunicators. J Clin Med. 2023;12:5884. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 45. | Infinger AE, Vandeventer S, Studnek JR. Introduction of performance coaching during cardiopulmonary resuscitation improves compression depth and time to defibrillation in out-of-hospital cardiac arrest. Resuscitation. 2014;85:1752-1758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | Wu Z, Panczyk M, Spaite DW, Hu C, Fukushima H, Langlais B, Sutter J, Bobrow BJ. Telephone cardiopulmonary resuscitation is independently associated with improved survival and improved functional outcome after out-of-hospital cardiac arrest. Resuscitation. 2018;122:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 47. | Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, Long J, Slowther A, Pocock H, Black JJM, Moore F, Fothergill RT, Rees N, O'Shea L, Docherty M, Gunson I, Han K, Charlton K, Finn J, Petrou S, Stallard N, Gates S, Lall R; PARAMEDIC2 Collaborators. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2018;379:711-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 513] [Article Influence: 73.3] [Reference Citation Analysis (0)] |
| 48. | Ran L, Liu J, Tanaka H, Hubble MW, Hiroshi T, Huang W. Early Administration of Adrenaline for Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2020;9:e014330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 49. | Hansen M, Schmicker RH, Newgard CD, Grunau B, Scheuermeyer F, Cheskes S, Vithalani V, Alnaji F, Rea T, Idris AH, Herren H, Hutchison J, Austin M, Egan D, Daya M; Resuscitation Outcomes Consortium Investigators. Time to Epinephrine Administration and Survival From Nonshockable Out-of-Hospital Cardiac Arrest Among Children and Adults. Circulation. 2018;137:2032-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 133] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 50. | Palatinus HN, Johnson MA, Wang HE, Hoareau GL, Youngquist ST. Early intramuscular adrenaline administration is associated with improved survival from out-of-hospital cardiac arrest. Resuscitation. 2024;201:110266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 51. | Crewdson K, Rehn M, Lockey D. Airway management in pre-hospital critical care: a review of the evidence for a 'top five' research priority. Scand J Trauma Resusc Emerg Med. 2018;26:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 52. | Wang HE, Mann NC, Mears G, Jacobson K, Yealy DM. Out-of-hospital airway management in the United States. Resuscitation. 2011;82:378-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 53. | Diggs LA, Yusuf JE, De Leo G. An update on out-of-hospital airway management practices in the United States. Resuscitation. 2014;85:885-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 54. | Izawa J, Komukai S, Gibo K, Okubo M, Kiyohara K, Nishiyama C, Kiguchi T, Matsuyama T, Kawamura T, Iwami T, Callaway CW, Kitamura T. Pre-hospital advanced airway management for adults with out-of-hospital cardiac arrest: nationwide cohort study. BMJ. 2019;364:l430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 55. | Okubo M, Komukai S, Izawa J, Gibo K, Kiyohara K, Matsuyama T, Iwami T, Callaway CW, Kitamura T. Timing of Prehospital Advanced Airway Management for Adult Patients With Out-of-Hospital Cardiac Arrest: A Nationwide Cohort Study in Japan. J Am Heart Assoc. 2021;10:e021679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 56. | Carlson JN, Colella MR, Daya MR, J De Maio V, Nawrocki P, Nikolla DA, Bosson N. Prehospital Cardiac Arrest Airway Management: An NAEMSP Position Statement and Resource Document. Prehosp Emerg Care. 2022;26:54-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 57. | Bednarz K, Goniewicz K, Al-Wathinani AM, Goniewicz M. Emergency Medicine Perspectives: The Importance of Bystanders and Their Impact on On-Site Resuscitation Measures and Immediate Outcomes of Out-of-Hospital Cardiac Arrest. J Clin Med. 2023;12:6815. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 58. | Dainty KN, Colquitt B, Bhanji F, Hunt EA, Jefkins T, Leary M, Ornato JP, Swor RA, Panchal A. Understanding the Importance of the Lay Responder Experience in Out-of-Hospital Cardiac Arrest: A Scientific Statement From the American Heart Association. Circulation. 2022;145:e852-e867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 55] [Reference Citation Analysis (0)] |
| 59. | Blewer AL, Ibrahim SA, Leary M, Dutwin D, McNally B, Anderson ML, Morrison LJ, Aufderheide TP, Daya M, Idris AH, Callaway CW, Kudenchuk PJ, Vilke GM, Abella BS. Cardiopulmonary Resuscitation Training Disparities in the United States. J Am Heart Assoc. 2017;6:e006124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 60. | Roppolo LP, Pepe PE, Campbell L, Ohman K, Kulkarni H, Miller R, Idris A, Bean L, Bettes TN, Idris AH. Prospective, randomized trial of the effectiveness and retention of 30-min layperson training for cardiopulmonary resuscitation and automated external defibrillators: The American Airlines Study. Resuscitation. 2007;74:276-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 98] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 61. | Hutton J, Lingawi S, Puyat JH, Kuo C, Shadgan B, Christenson J, Grunau B. Sensor technologies to detect out-of-hospital cardiac arrest: A systematic review of diagnostic test performance. Resusc Plus. 2022;11:100277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 62. | Edgar R, Scholte NTB, Ebrahimkheil K, Brouwer MA, Beukema RJ, Mafi-Rad M, Vernooy K, Yap SC, Ronner E, van Mieghem N, Boersma E, Stas PC, van Royen N, Bonnes JL. Automated cardiac arrest detection using a photoplethysmography wristband: algorithm development and validation in patients with induced circulatory arrest in the DETECT-1 study. Lancet Digit Health. 2024;6:e201-e210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 63. | Latsios G, Synetos A, Tsioufis K, Kanakakis J. CPR education in schools: The European "Kids-Save-Lives" initiative and our efforts in Greece. Hellenic J Cardiol. 2023;69:59-60. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 64. | Böttiger BW, Van Aken H. Kids save lives--Training school children in cardiopulmonary resuscitation worldwide is now endorsed by the World Health Organization (WHO). Resuscitation. 2015;94:A5-A7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 139] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 65. | Böttiger BW, Lockey A, Georgiou M, Greif R, Monsieurs KG, Mpotos N, Nikolaou N, Nolan J, Perkins G, Semeraro F, Wingen S. KIDS SAVE LIVES: ERC Position statement on schoolteachers' education and qualification in resuscitation. Resuscitation. 2020;151:87-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 66. | Schroeder DC, Semeraro F, Greif R, Bray J, Morley P, Parr M, Kondo Nakagawa N, Iwami T, Finke SR, Malta Hansen C, Lockey A, Del Rios M, Bhanji F, Sasson C, Schexnayder SM, Scquizzato T, Wetsch WA, Böttiger BW; International Liaison Committee on Resuscitation. KIDS SAVE LIVES: Basic Life Support Education for Schoolchildren: A Narrative Review and Scientific Statement From the International Liaison Committee on Resuscitation. Circulation. 2023;147:1854-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 67. | Park S, Kim JY, Cho YD, Lee E, Shim B, Yoon YH. Successful resuscitation of refractory ventricular fibrillation with double sequence defibrillation. Acute Crit Care. 2021;36:67-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 68. | Cheskes S, Dorian P, Scales DC. Defibrillation Strategies for Refractory Ventricular Fibrillation. Reply. N Engl J Med. 2023;388:861-863. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 69. | Abuelazm MT, Ghanem A, Katamesh BE, Hassan AR, Abdalshafy H, Seri AR, Awad AK, Abdelnabi M, Abdelazeem B. Defibrillation strategies for refractory ventricular fibrillation out-of-hospital cardiac arrest: A systematic review and network meta-analysis. Ann Noninvasive Electrocardiol. 2023;28:e13075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 70. | Bondarenko A, Navolokina A, Kozyk M. The head-up cardiopulmonary resuscitation method: Improving neurological outcomes. Cardiol J. 2023;30:497-498. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 71. | Varney J, Motawea KR, Mostafa MR, AbdelQadir YH, Aboelenein M, Kandil OA, Ibrahim N, Hashim HT, Murry K, Jackson G, Shah J, Boury M, Awad AK, Patel P, Awad DM, Rozan SS, Talat NE. Efficacy of heads-up CPR compared to supine CPR positions: Systematic review and meta-analysis. Health Sci Rep. 2022;5:e644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 72. | Moore JC, Duval S, Lick C, Holley J, Scheppke KA, Salverda B, Rojas-Salvador C, Jacobs M, Nystrom P, Quinn R, Adams PJ, Debaty GP, Hutchison M, Mason C, Martinez E, Mason S, Clift A, Antevy P, Coyle C, Grizzard E, Garay S, Lurie KG, Pepe PE. Faster time to automated elevation of the head and thorax during cardiopulmonary resuscitation increases the probability of return of spontaneous circulation. Resuscitation. 2022;170:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 73. | Breckwoldt J, Schloesser S, Arntz HR. Perceptions of collapse and assessment of cardiac arrest by bystanders of out-of-hospital cardiac arrest (OOHCA). Resuscitation. 2009;80:1108-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 74. | Horriar L, Rott N, Böttiger BW. Improving survival after cardiac arrest in Europe: The synergetic effect of rescue chain strategies. Resusc Plus. 2024;17:100533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 75. | Georgiou M. Restart a Heart Day: a strategy by the European Resuscitation Council to raise cardiac arrest awareness. Resuscitation. 2013;84:1157-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 76. | Lott C, van Goor S, Nikolaou N, Thilakasiri K, Bahtijarević Z. "Get trained. Save lives.": A CPR awareness campaign in football. Resuscitation. 2023;193:110013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 77. | Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, Genbrugge C, Haywood K, Lilja G, Moulaert VRM, Nikolaou N, Mariero Olasveengen T, Skrifvars MB, Taccone F, Soar J. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: Post-resuscitation care. Resuscitation. 2021;161:220-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 459] [Article Influence: 114.8] [Reference Citation Analysis (0)] |
| 78. | Yeung J, Matsuyama T, Bray J, Reynolds J, Skrifvars MB. Does care at a cardiac arrest centre improve outcome after out-of-hospital cardiac arrest? - A systematic review. Resuscitation. 2019;137:102-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 86] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 79. | Patterson T, Perkins GD, Perkins A, Clayton T, Evans R, Dodd M, Robertson S, Wilson K, Mellett-Smith A, Fothergill RT, McCrone P, Dalby M, MacCarthy P, Firoozi S, Malik I, Rakhit R, Jain A, Nolan JP, Redwood SR; ARREST trial collaborators. Expedited transfer to a cardiac arrest centre for non-ST-elevation out-of-hospital cardiac arrest (ARREST): a UK prospective, multicentre, parallel, randomised clinical trial. Lancet. 2023;402:1329-1337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 19.0] [Reference Citation Analysis (0)] |