INTRODUCTION
Coronary artery disease is a leading cause of mortality worldwide and associated with significant morbidity. Nonetheless, studies have shown that up to two thirds of patients who exhibit anginal symptoms have non-obstructive coronary arteries during coronary angiography but have demonstratable ischemia, an entity known as ischemia with non-obstructive coronary arteries[1]. Of these, half of the patients have coronary microvascular disease (CMD) or coronary vasospasm[2]. CMD refers to a spectrum of functional and structural changes at the level of coronary microcirculation, impairing the coronary blood flow leading to myocardial ischemia[3]. It is one of the common causes of chest pain, is more prevalent in women and is a predictor for increased major adverse cardiac events[4,5]. The invasive diagnosis requires special tools or equipment, which is not universally available in catheterization laboratory or hospitals and so the entity is infrequently diagnosed, and no tailored therapy is offered to these patients. The methods include CMD assessment via Doppler technique (Combowire XT or Flowire) or thermodilution method using a pressure-temperature sensor guidewire (Pressurewire X). Invasive assessment of CMD is indicated for the patients with symptoms suggestive of angina and signs of myocardial ischemia at noninvasive testing in the absence of significant epicardial stenosis on coronary or computed tomographic angiography. These patients continue to have recurrent angina with impaired quality of life, unnecessary cardiac testing in multiple settings, and adverse outcomes regardless of the presence of coronary artery stenosis[2,6]. Lately, there is data emerging that the entity may be associated with cancer therapy-related cardiovascular toxicities[7]. The recently updated 2024 European Society of Cardiology (ESC) chronic coronary syndrome guidelines have upgraded the recommendation to class I [level of evidence (LOE): B] from class IIa (LOE: B) in 2019 for invasive assessment of CMD in patients with persistent symptoms, who have either normal or hemodynamically non-significant moderate stenosis of coronary arteries[8,9]. Also, the updated 2023 American College of Cardiology (ACC) and American Heart Association (AHA) guidelines for chronic coronary disease provide class IIa (LOE: B) recommendation for invasive coronary physiologic guided medical therapy to improve angina severity and quality of life[10].
PATHOPHYSIOLOGY
The endothelium plays an important role in the physiological tone of coronary vasculature through release of several vasodilators including nitric oxide (NO) and endothelium-derived hyperpolarizing factor. The underlying pathophysiology of CMD is complex and heterogenous and related to intrinsic vascular and endothelial dysfunction. The molecular mechanism include alteration in the cellular milieu, and overproduction of reactive oxygen species (ROS) resulting in inflammatory response. The changes at the mitochondrial level are believed to be initiated by a proapoptotic protein(p66shc) that stimulates nicotinamide adenine dinucleotide phosphate oxidases, and activates the vicious cycle of ROS production[11,12]. This in turn promotes uncoupling of endothelial NO synthetase, altering its activity of NO-mediated vasodilation with enhancement of vasoconstricting thromboxane and endothelin-1 activity via RhoA/Rho-kinase pathway[13]. Furthermore, in presence of endothelial dysfunction, acetylcholine binds to the muscarinic receptor on vascular smooth muscle cell and, leading to unopposed vasoconstriction[14]. The hypercontraction of vascular smooth muscle cell via impairment of calcium sensitivity modulation, phosphorylation of contractile myofilaments and increased ROS synthesis, plays a crucial role in increasing the susceptibility of coronary vessels to spasm[15].
The endothelium independent mechanisms are comparatively less studied and include diminished vasodilator response of vascular smooth muscle cell to adenosine or papaverine. Besides this, other variables such as blood pressure, heart rate, diastolic time also influence functional responsiveness of coronary microcirculation[15]. Moreover, structural alterations associated with CMD include luminal narrowing of arterioles and capillaries, perivascular fibrosis, and capillary diminution in setting of left ventricular hypertrophy[3].
INVASIVE ASSESSMENT OF CMD
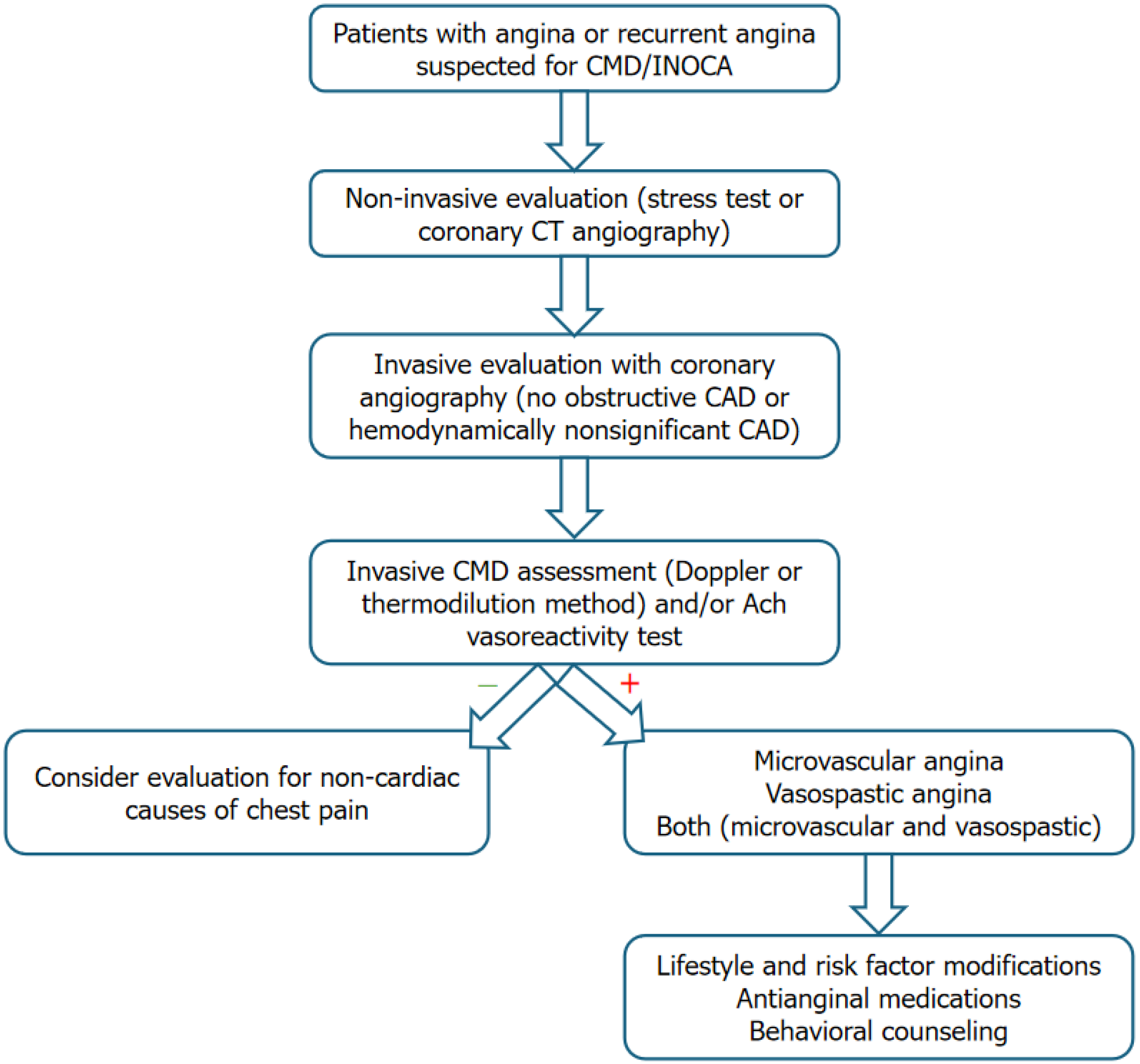
Invasive assessment of CMD is indicated for the patients with symptoms suggestive of angina and signs of myocardial ischemia at noninvasive testing in the absence of significant epicardial stenosis on coronary or computed tomographic angiography[6]. The options include CMD assessment via Doppler technique (Combowire XT or Flowire, Philips Volcano corporation, San Diego, CA) or thermodilution method using a pressure-temperature sensor guidewire (Pressurewire X, Abbott, Santa Clara, CA, United States). An algorithm highlighting the recommended approach to a patient with suspected CMD is depicted in Figure 1.
Figure 1 An algorithm for coronary microvascular disease assessment.
CAD: Coronary artery disease; CMD: Coronary microvascular disease; CT: Computed tomography; INOCA: Ischemia with non-obstructive coronary arteries.
Using the combowire XT, doppler flow velocity, aortic pressure, and distal coronary pressure and the electrocardiographic signals are recorded using the ComboMap system (Philips, Eindhoven)[16]. Then steady state hyperemia is induced using adenosine (140 μg/kg/minute) for endothelium-independent vasodilation[17]. Coronary flow reserve (CFR) is calculated using doppler flow velocity (hyperemic flow velocity divided by resting flow velocity) and hyperemic myocardial velocity resistance (HMR) (HMR by dividing intracoronary pressure by hyperemic flow velocity)[16]. The doppler value of CFR ≤ 2.5 is considered prognostically significant[6]. Prior studies have shown HMR > 1.9 was an independent predictor of recurrence of symptoms and HMR ≥ value of 2.5 mmHg/cm/second provided adequate sensitivity and specificity for predicting CMD[18].
The thermodilution test is based on the dilution theory “Stewart-Hamilton equation” principle, which implies that the flow is inversely proportional to the temperature of the saline solution mixed with blood in the distal part of the vessel[19]. The CMD assessment can either be done by injecting saline at room temperature (colder than body temperature) as a bolus (bolus method) or continuous infusion at a fixed rate (continuous method). In a study of 102 patients comparing bolus and continuous methods of thermodilution, continuous thermodilution demonstrated higher reproducibility than bolus method[20].
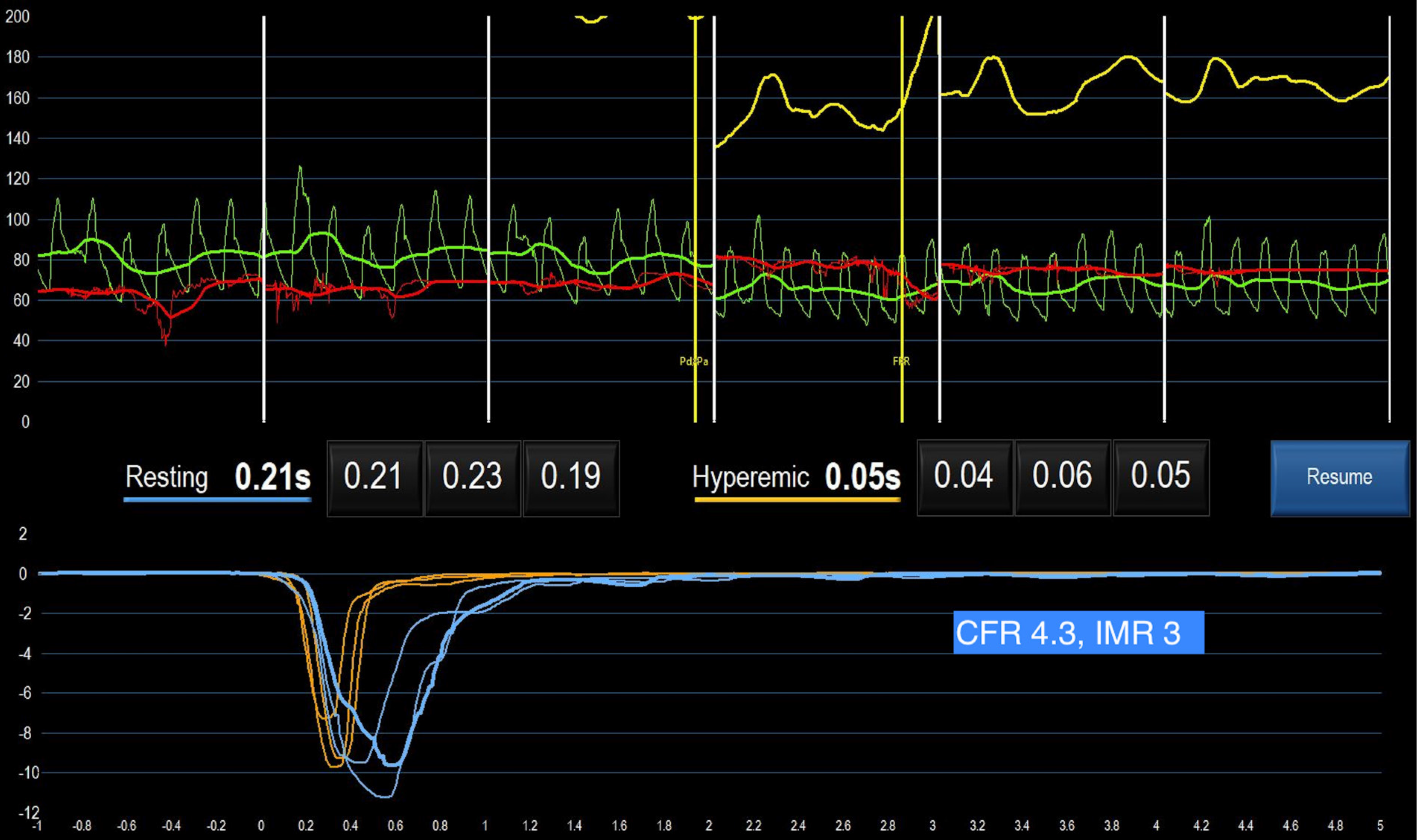
In bolus method, standard practice to inject bolus of 3 mL to 4 mL of saline from a 6 French guiding catheter and a V-shaped temperature change curve (fast descending limb and slow ascending limb) is recorded in the distal part of coronary artery using pressure wire X, and readings are repeated in setting of hyperemia using intravenous adenosine (Figure 2) and intracoronary papaverine[21]. The flow (Q) in mL/second is calculated using equation, Q = I (quantity of indicator) divided by ∫0∞c(t)dtwhich is time-dependent surface area under the thermodilution. If the exact volume of saline is not known (possibility of spillover into the aorta), Q can be estimated by dividing the vascular volume (in mL) by the mean transit time of the saline (Tmn; in secs). CFR via this method is calculated as the ratio between resting and hyperemic Tmn[22]. CFR interrogates the flow status in both epicardial vessels and microcirculation, while index of microcirculatory resistance (IMR) calculation is based on the analogy of Ohm’s law for electric resistance, that evaluates microvascular resistance, independent of epicardial stenoses. It is defined as distal coronary pressure (Pd) divided by the inverse of the Tmn during maximal hyperemia and thus IMR = Pd x Tmn at hyperemia[23]. According to thermodilution methods, CFR < 2.0 is considered prognostically significant and IMR value of ≥ 25 is representative of microvascular dysfunction[5].
Figure 2 A case study of coronary microvascular disease using bolus thermodilution method with normal coronary flow reserve.
CFR: Coronary flow reserve; IMR: Index of microcirculatory resistance.
Continuous thermodilution method directly measures absolute coronary blood flow (Q; mL/minute) as well as absolute microvascular resistance [Rμ; wood units (WU)]. In addition to pressurewire X, this method requires a monorail infusion microcatheter with four external side holes and two internal side holes (RayFlow, Hexacath) that enables instantaneous mixing of saline solution and blood in the very proximal part of the vessel and a regular power injector to infuse saline solution at a steady rate. Ideally, the monorail infusion microcatheter and pressurewire X are parked in the proximal and distal segments of the vessel to be examined, respectively[21]. The power injector is automated to infuse at the rate of 10 mL/minute for resting phase and 20 mL/minute for the hyperemic measurements. The absolute coronary blood flow is calculated as Q (mL/minute) = 1.08 × (T/Ti) x Qi, where Tiis the temperature of the saline when it enters the coronary artery (°C), T is temperature of mixed saline blood measured in the distal segment of the artery (°C), 1.08 is constant for the densities and specific heat of blood and normal saline and Qi is saline infusion rate (mL/minute). First, T is measured after complete mixing of blood with saline and once steady state for T is achieved, then temperature sensor of wire is pulled back to the tip of infusion catheter for measuring Ti. Absolute microvascular resistance is computed as Rμ (WU) as a ratio of distal coronary pressure (Pd) and absolute coronary blood flow (Q). CFRabsolute is calculated by dividing Qhyperemia by Qrest and value < 2.0 is abnormal. Microvascular resistance reserve (MRR) is calculated as: MRR = CFR/FFR × Parest/Pahyperemia, where Pa is aortic pressure and FFR is fractional flow reserve. MRR > 2.7 essentially excludes the presence of CMD, while MRR < 2.1 confirms CMD[24].
Lastly, vasoreactivity testing by intracoronary infusion of acetylcholine is recommended. A standardized method involves successive infusion of acetylcholine at concentrations of 10−6 moL/L, 10−5 moL/L, and 10−4 moL/L, respectively[6,25]. Vasospastic angina is diagnosed when there is ≥ 90% diameter reduction of coronary vessel, plus presence of ischemic electrocardiographic changes and angina[6].
MANAGEMENT
A patient-centered multidisciplinary approach should be considered for the management of CMD. Currently there is no evidence-based treatment available for CMD as most of prior studies were small and heterogeneous[26]. Lifestyle modifications including directing at addressing risk factors (hypertension, dyslipidemia, and diabetes), reduce symptoms and behavioral interventions including smoking cessation are warranted[10]. Blood pressure control can reduce the frequency and intensity of anginal symptoms[27]. Patients with microvascular angina with reduced CFR and increased IMR can be benefited from beta-blockers (carvedilol, nebivolol, bisoprolol), calcium channel blockers (CCB) and or angiotensin-converting enzyme inhibitors (ACEis). In patients with epicardial or microvascular spasm with acetylcholine testing, CCBs are first line medications of choice. In patients with hypertensive microvascular angina, ACEis have shown improve hyperemic myocardial blood flow and decrease angina frequency[28,29]. The recent 2023 ACC/AHA guidelines recommend beta-blockers as a first line agent, followed by CCBs as a second line therapy if beta-blockers are ineffective or not well tolerated[10]. CORonary MICrovascular Angina trial demonstrated that a stratified medical therapy approach of an interventional diagnostic procedure with linked therapy was associated with reduction in angina frequency and better quality of life at 6 months and 1 year[30,31]. Nicorandil, a potassium channel activator with coronary microvascular dilatory effect may be an effective alternative for some patients[32]. Ranolazine, an inhibitor of late sodium current in cardiomyocytes, have shown mixed results in various studies[33,34]. Trimetazidine, which increases cellular tolerance to ischemia is recommended by ESC in patients who are intolerant to medications for angina[8]. Few patients remain refractory to medications and with the gaps in the knowledge and lack of evidence-based treatment, large future studies are warranted. Women's Ischemia Trial to Reduce Events in Non-Obstructive CAD trial is a multicenter, prospective, randomized, blinded outcome trial (NCT03417388) currently in phase 4, is investigating intensive medical treatment versus usual care in 4422 symptomatic women patients with signs and symptoms of ischemia but no obstructive CAD.
CONCLUSION
CMD is a common cause of angina, often overlooked and underdiagnosed resulting in recurrent angina, multiple unnecessary cardiac testing and associated with adverse outcomes. This editorial intends to increase the awareness of CMD among the primary physicians and cardiologist to keep low threshold for referral or considering further testing in suspected patients having recurrent angina or angina with no obstructive coronary artery. Undoubtedly, future research is warranted to investigate it further including availability of evidence-based treatment options and most importantly, to improve diagnostic awareness and relieve patient sufferings.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country of origin: India
Peer-review report’s classification
Scientific Quality: Grade B, Grade B
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade C
Scientific Significance: Grade B, Grade B
P-Reviewer: Xue HM S-Editor: Luo ML L-Editor: A P-Editor: Zhao YQ