Published online Jul 26, 2024. doi: 10.4330/wjc.v16.i7.385
Revised: June 26, 2024
Accepted: July 9, 2024
Published online: July 26, 2024
Processing time: 36 Days and 12.2 Hours
A number of publications have claimed that Mobitz type II atrioventricular block (AVB) may occur during sleep. None of the reports defined type II AVB and representative electrocardiograms were either misinterpreted or missing. Relatively benign Wenckebach type I AVB is often misdiagnosed as Mobitz type II which is an indication for a pacemaker. Review of the published reports indicates that Mobitz type II AVB does not occur during sleep when it is absent in the awake state. Conclusion: There is no proof that sleep is associated with Mobitz type II AVB.
Core Tip: A number of publications have claimed that Mobitz type II atrioventricular block (AVB) may occur during sleep. None of the reports defined it and representative electrocardiograms were either misinterpreted or missing. Sleep-induced relatively benign narrow QRS-Mobitz type I AVB must be differentiated from serious Mobitz type II AVB. This depends solely on strict electrocardiograms definitions and behavior of the sinus rate where slowing rules out Mobitz type II AVB even if all the PR intervals are constant. Mobitz type II AVB does not occur solely during sleep when it is absent in the awake state.
- Citation: Barold SS. Misinterpretation of sleep-induced second-degree atrioventricular block. World J Cardiol 2024; 16(7): 385-388
- URL: https://www.wjgnet.com/1949-8462/full/v16/i7/385.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i7.385
Second-degree and third-degree atrioventricular block (AVB) not uncommonly occur during ordinary sleep and sleep apnea. They are caused by enhanced vagal tone and generally considered benign. During sleep, second-degree AVB can be manifested by Wenckebach type I AVB block, 2:1 AVB or high grade AVB almost always with a narrow QRS complex. A number of publications have claimed that Mobitz type II AVB may also occur during sleep[1-5]. These reports have been largely discredited because none of the reports defined type II AVB and representative electrocardiograms (ECG) were either misinterpreted or missing[6]. Vagally-induced type I second-degree AVB during sleep occurs in the atrioventricular (AV) node and is reversible. Mobitz type II second-degree AVB is far more serious and irreversible because it is caused by structural changes in the His-Purkinje conduction system of the heart. Therefore, type II AVB is often associated with a broad QRS complex. It is therefore important especially for sleep-health care workers to be familiar with the strict definitions of the various manifestations of second-degree AVB to avoid diagnostic or even therapeutic errors.
Type I AVB is defined as intermittent failure of AV conduction in which a single blocked sinus P wave is preceded by prolongation of conduction time relative to the first conducted P wave after the block. There must be at least two consecutive conducted P waves (i.e., 3:2 AV block), thereby ruling out 2:1 AVB. This definition accommodates all forms of typical and atypical type I block and is valid with variations of the sinus rate[7,8]. Narrow QRS-type I AVB is almost always localized in the AV node.
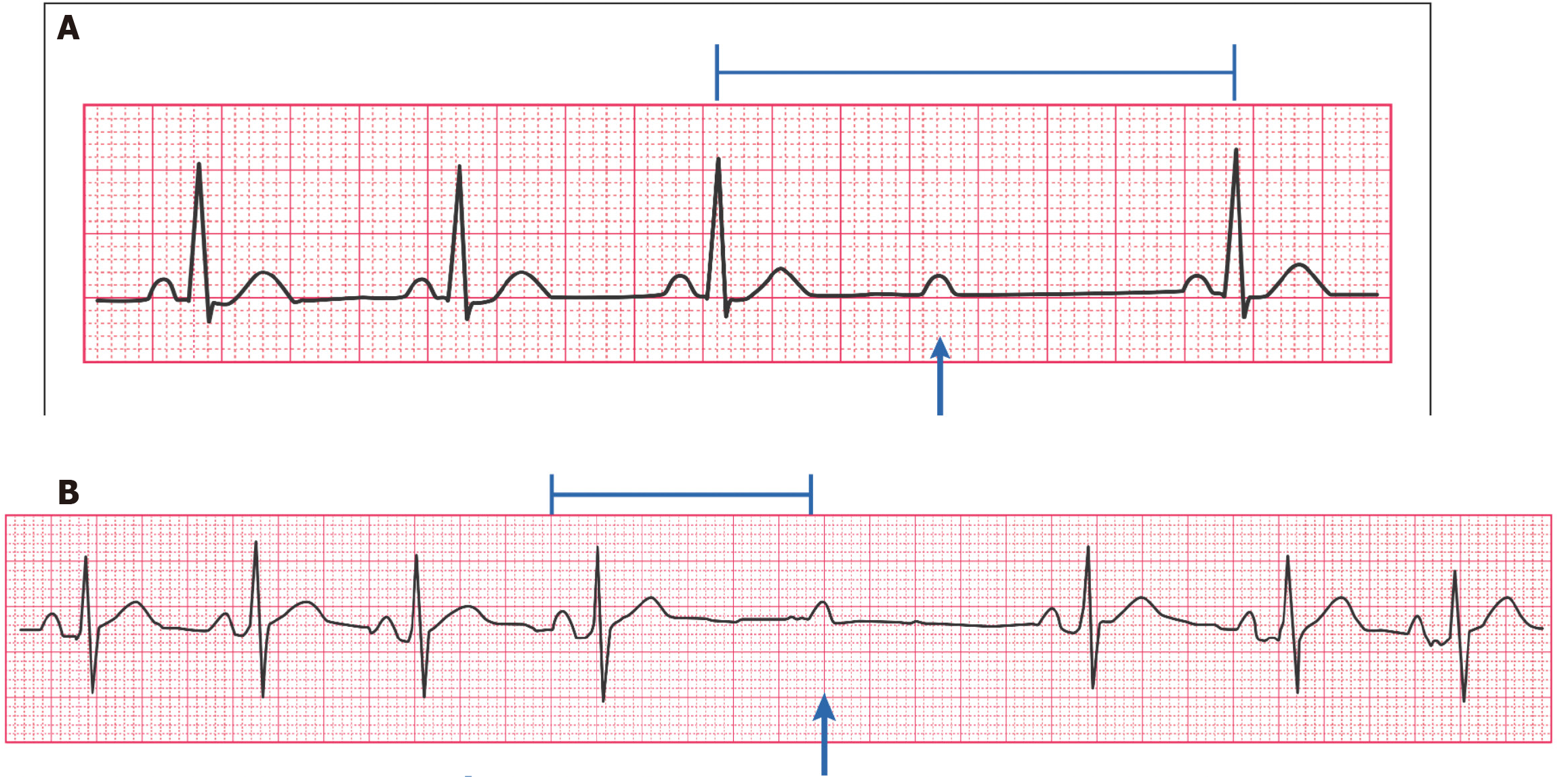
Mobitz type II second-degree AVB is defined as the occurrence of a single non-conducted sinus P wave associated with constant PR intervals before and after the blocked impulse, provided the sinus rate or the P-P interval is constant and there are at least two consecutive conducted P waves (i.e., 3:2 AVB) to determine behavior of the PR intervals[7-10]. Therefore, type II block appears to represent an all-or-none phenomenon (Figure 1A). Mobitz type II AVB is always localized in the His-Purkinje conduction system and is an indication for a permanent pacemaker[9,11]. Stability of the sinus rate is an important criterion of type II AVB. A vagal surge causing type I AVB by simultaneously slowing of the sinus rate and depression of AV nodal conduction can superficially resemble type II AVB especially when the PR interval before the block is equal to that of the first conducted beat after the block[12,13] (Figure 1B).
Two to one AVB or higher degrees of AVB cannot be classified into Wenckebach type I or Mobitz type II AVB. A common mistake is to equate 2:1 and higher degree of AVB with type II infranodal block when block can be either in the AV node or the His-Purkinje system.
First, ignoring the presence of a vagal surge with sinus slowing that may be subtle (at least 0.04 second) either before and/or after the block of a single blocked P wave. Vagally-induced AVB may sometimes present with an ECG pattern that superficially resembles type II block because the PR interval(s) before and after the block are constant (Figure 1B). Note that only the behavior of the sinus rate differentiates Figure 1A (type II AVB) from Figure 1B (type I AVB).
Second, in the presence of 2:1 or higher degrees of AV block.
Third, when narrow QRS- type I block exhibits miniscule increments, a situation mimicking type II block. This pattern may be seen during ECG monitoring or Holter recordings and is associated with sinus slowing which rules out type II block. Furthermore, repeated ECGs or further monitoring should reveal more obvious runs of type I AVB. In this situation, type II AVB can then be safely excluded because type I and II blocks almost never occur together in a single ECG recording or one done at separate times.
Fourth, less commonly during stable sinus rhythm when there is a string of constant PR intervals before the block of a single P wave and the PR interval of the first conducted beat is shorter.
Szajerska-Kurasiewicz et al[5] recently warned that sleep-disordered breathing is a risk factor for unnecessary pacemaker implantation based on a study involving 207 patients hospitalized in a general cardiology ward. Paradoxically, about 5% of patients exhibited so called type II block but none received a pacemaker. As type II is rare, their reported incidence is excessive and suggests an incorrect diagnosis.
In conclusion, the separate diagnosis of relatively benign narrow QRS- type I AVB from that of serious type II AVB depends solely on strict ECG definitions and behavior of the sinus rate. A suspected diagnosis of true type II AVB during sleep mandates a detailed cardiology evaluation. As a rule, type II AVB does not occur solely during sleep when it is absent in the awake state.
| 1. | Colicchio S, Della Marca G, Vollono C, Quatrale M, Janiri L. Sleep-related modification of atrioventricular block: from first-degree to second-degree, Mobitz type II. Sleep Med. 2015;16:1091-1093. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Koehler U, Fus E, Grimm W, Pankow W, Schäfer H, Stammnitz A, Peter JH. Heart block in patients with obstructive sleep apnoea: pathogenetic factors and effects of treatment. Eur Respir J. 1998;11:434-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 101] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Mann A, Jean, Fleischman J, Mrejen-Shakin K. Bradyarrhythmias Associated with the Obstructive Sleep Apnoea Syndrome: A Precursor to Life-threatening Arrhythmias? Br J Med Practitioners. 2012;5:a511. |
| 4. | Gula LJ, Krahn AD, Skanes AC, Yee R, Klein GJ. Clinical relevance of arrhythmias during sleep: guidance for clinicians. Heart. 2004;90:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Szajerska-Kurasiewicz A, Loboda D, Roleder T, Stepanik M, Durmala J, Golba KS. Sleep-disordered breathing as a risk factor for unnecessary pacemaker implantation. Kardiol Pol. 2022;80:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Barold SS. Mobitz type II second-degree atrioventricular block during sleep: true or false? Herzschrittmacherther Elektrophysiol. 2023;34:226-228. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 7. | Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ, Gorgels A, Hancock EW, Josephson M, Kligfield P, Kors JA, Macfarlane P, Mason JW, Mirvis DM, Okin P, Pahlm O, van Herpen G, Wagner GS, Wellens H; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2009;119:e241-e250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 301] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 8. | Definition of terms related to cardiac rhythm. Am Heart J. 1978;95:796-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 55] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Barold SS, Hayes DL. Second-degree atrioventricular block: a reappraisal. Mayo Clin Proc. 2001;76:44-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Barold SS. Problematic definitions of Mobitz type II second degree AV block: Historical aspects. J Electrocardiol. 2023;79:122-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, Goldschlager NF, Hamilton RM, Joglar JA, Kim RJ, Lee R, Marine JE, McLeod CJ, Oken KR, Patton KK, Pellegrini CN, Selzman KA, Thompson A, Varosy PD. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. Circulation. 2019;140:e333-e381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Massie B, Scheinman MM, Peters R, Desai J, Hirschfeld D, O'Young J. Clinical and electrophysiologic findings in patients with paroxysmal slowing of the sinus rate and apparent Mobitz type II atrioventricular block. Circulation. 1978;58:305-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Alboni P, Holz A, Brignole M. Vagally mediated atrioventricular block: pathophysiology and diagnosis. Heart. 2013;99:904-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 14. | Barold DC, Barold SS. ECG Simplified. Facts You will Never Forget. San Marcos: Conductivity Press, 2022. |