Published online May 26, 2024. doi: 10.4330/wjc.v16.i5.260
Revised: February 19, 2024
Accepted: April 12, 2024
Published online: May 26, 2024
Processing time: 143 Days and 16.3 Hours
Coronavirus is an important pathogen causing disease in humans and animals. At the end of 2019, an investigation into an increase in pneumonia cases in Wuhan, Hubei Province, China, found that the cause was a new coronavirus. This disease, which spread rapidly across China and caused an outbreak worldwide, resulted in a pandemic. Although this virus has previously been referred to as 2019-nCoV, which causes coronavirus disease 2019 (COVID-19), later it was named severe acute respiratory syndrome coronavirus 2. Children were usually asymptomatic and rarely severely affected. In April 2020, reports from the United Kingdom indicated that children may have Kawasaki disease or a clinical condition similar to toxic shock syndrome. This clinical picture was later defined as multisystem inflammatory syndrome in children. Since then, similarly affected children as well as cases with other cardiac complications have been reported in other parts of the world. In this review, we aimed to evaluate COVID-19 in terms of cardiac invol
Core Tip: In April 2020, reports from the United Kingdom indicated that children may have Kawasaki disease or a clinical condition similar to toxic shock syndrome. This clinical picture was later defined as multisystem inflammatory syndrome in children. Since then, similarly affected children as well as cases with other cardiac complications have been reported in other parts of the world. In this review, we aimed to evaluate coronavirus disease 2019 in terms of cardiac involvement by reviewing the literature.
- Citation: Güneş M, Özdemir Ö. COVID-19 and cardiac complications: Myocarditis and multisystem inflammatory syndrome in children. World J Cardiol 2024; 16(5): 260-268
- URL: https://www.wjgnet.com/1949-8462/full/v16/i5/260.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i5.260
Multisystem inflammatory syndrome in children (MIS-C) caused by coronavirus disease 2019 (COVID-19) in children can lead to death, if not diagnosed early. After it was first identified in the United Kingdom in April 2020, similar cases were reported in Europe and America[1-5]. Polymerase chain reaction (PCR) tests or antibodies were found to be positive in most of these children and were associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Various forms of cardiac involvement have been reported in the literature during MIS-C disease. These forms may affect the course of the disease. After the World Health Organization defined the picture as MIS-C in May 2020, guidelines on diagnosis and treatment have been continuously updated[6]. In this review, cardiac involvement that may occur during COVID-19 and MIS-C are discussed in light of the current literature.
The mechanisms of myocardial damage in COVID-19 are not clearly defined. Different variants of the virus may cause myocardial damage in children by various mechanisms. One theory suggests that entry of the virus into the host cell is facilitated by the binding of the spike protein to the angiotensin converting enzyme (ACE) 2 receptor. The virus causes a local inflammatory reaction with T-cell infiltration and B lymphocytes[7]. Permanent cell damage may lead to fibrosis formation and finally to the development of dilated cardiomyopathy[7,8]. Postmortem histological examination revealed local inflammation and the presence of a viral genome in the myocardial tissue. Accordingly, the negativity of markers indicating systemic inflammation in blood indicated the presence of direct damage caused by the virus itself[9].
In another study, researchers suggested that the cause of myocardial damage in adults was due to ischemia in the coronaries leading to a weakening of the blood supply to the heart muscle[10]. The main sign of myocardial damage in COVID-19 is thought to be endothelial inflammation leading to bleeding, thrombosis, and necrosis in intramural arteries. There is no correlation between markers of inflammation and myocarditis and no evidence that the virus directly triggers myocarditis. As a result, the theory that immune damage to the endothelium and microthrombosis formation play a role in the pathogenesis of myocarditis has been strengthened[11].
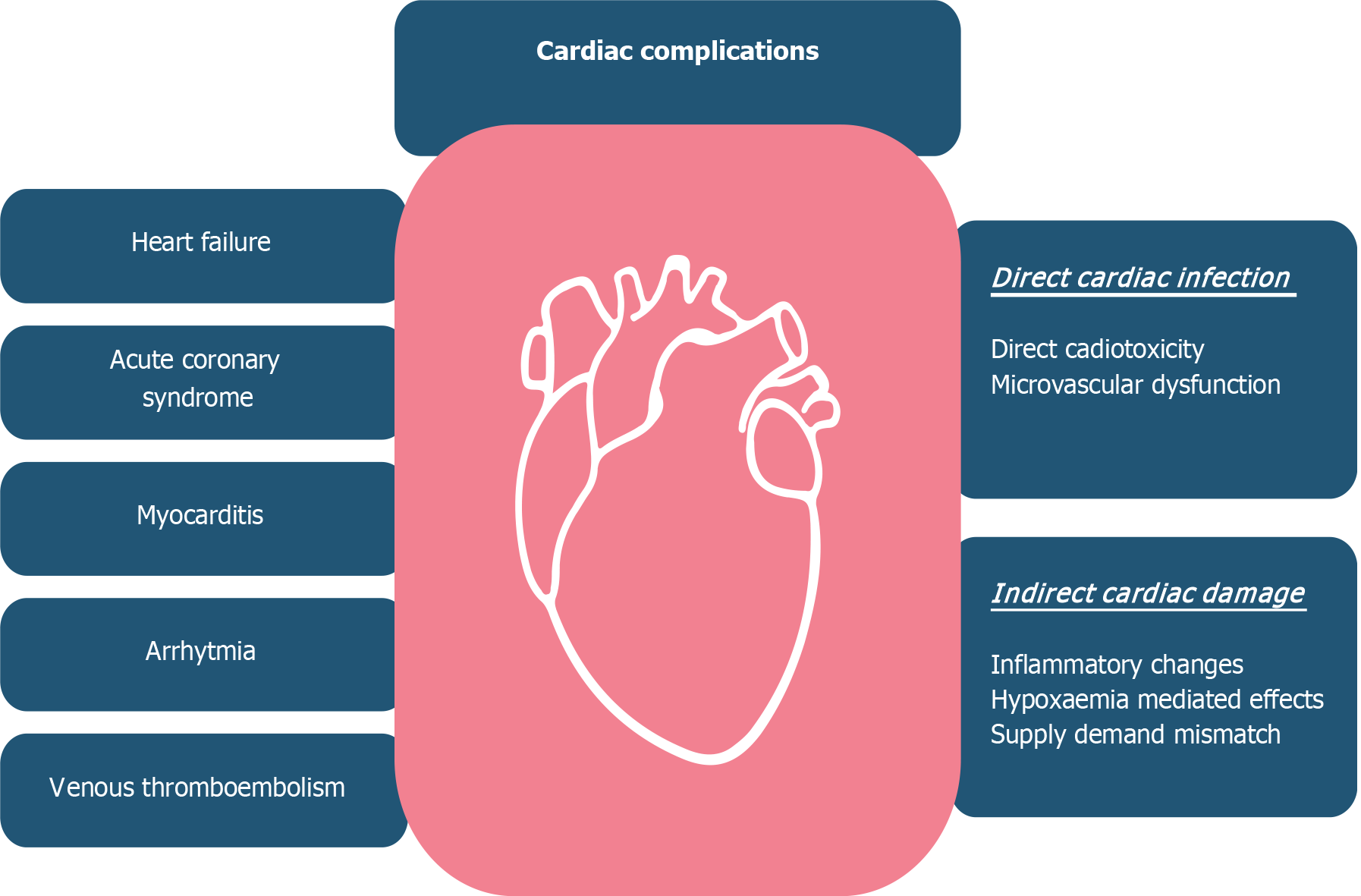
However, the etiology of heart failure due to COVID-19 is multifactorial. (1) Virus-induced infiltration of the myo
COVID-19 usually proceeds with mild respiratory symptoms in children[12]. As with other viral agents, COVID-19 has the potential to cause myocarditis. The prevalence of myocarditis due to COVID-19 is not yet known. The approach in COVID-19 patients presenting with acute myocarditis is not different to other classical viral myocarditis. All types of rhythm disturbances can be seen in acute myocarditis cases. In a case presented by Kohli et al[9], atrial fibrillation developed, and cardioversion was required[13].
Unlike adults, cases of acute fulminant myocarditis due to SARS-CoV-2 infection with left ventricular dysfunction are rarely seen[14]. Recently, rare cases of acute fulminant myocarditis have been reported and these patients required treatment in intensive care units. In these patients, acute myocarditis develops before respiratory symptoms develop[9,13]. Extracorporeal membrane oxygenation (ECMO) was applied in an infant with fulminant myocarditis with a fatal course reported by Kesici et al[14], but the patient died[9]. In the cases of acute fulminant myocarditis presented in the literature, adolescents presenting with chest pain, fever, palpitations, weakness, and pallor, as well as infants presenting with fever, vomiting, pallor, rapid breathing, and decreased sucking can be seen. ECMO was applied in a patient with sustained ventricular tachycardia presented by Tseng et al[15]. The presented cases had a fulminant course and this is not a condition frequently encountered in other forms of viral myocarditis. The reason for this is still unclear. Histological cardiac evaluations are needed for this. Therefore, acute myocarditis due to COVID-19 should be kept in mind in patients who develop malignant arrhythmia in the absence of fever and respiratory symptoms (Figure 1).
Symptomatic treatment is usually applied according to the severity of myocarditis. In all of these cases, severe left ventricular failure developed and they received various inotropic treatments as well as intravenous immunoglobulin (IVIG) and steroid treatments.
In April 2020, reports from the United Kingdom indicated that children may have Kawasaki disease or a clinical condition similar to the described shock syndrome. Since then, similarly affected children have been reported in other parts of the world. This clinical definition is called MIS-C[16]. In both Kawasaki disease (KD) and MIS-C, symptoms and organ dysfunction result from a cytokine storm[17].
It was observed that the inflammatory storm was more prominent in MIS-C[18]. According to Rodriguez-Smith et al[19], the measured levels of S-100 and interleukin (IL)-18 are similar in MIS-C and KD. Therefore, interferon-γ-stimulated chemokine ligand 9 is an indicator that may be important in differentiating MIS-C from KD. The main mediator of coronary artery inflammation in KD is IL-1. However, the main mediators of MIS-C are IL-6 and IL-8 and the inflammatory response seems to be triggered by these factors[17].
A mucosal biopsy from a COVID-19 patient with gastrointestinal system involvement and symptoms showed the presence of SARS-CoV-2 in endothelial cells. Recent studies have reported autoantibodies targeting antigens in mucosal and cardiac tissues in MIS-C patients[20]. At the beginning of the pandemic, pediatric patients were not considered to be at high risk for severe COVID-19 symptoms such as severe acute respiratory syndrome due to the lower presence of ACE 2 receptors in epithelial cells[21]. Later in the pandemic, more serious COVID-19-related complications such as thrombotic events, myocardial dysfunction, and coronary artery disease or aneurysms have been observed in pediatric patients with MIS-C[22]. In a study published in the United States, it was shown that the most common finding in children with MIS-C was cardiac dysfunction with a rate of 40.6%[23]. Serological evidence for SARS-CoV-2 or a history of contact with a COVID-19 patient was found in all patients[24,25]. It has been shown that vaccinated children are less frequently diagnosed with MIS-C[26].
Many hypotheses related to the pathogenesis of MIS-C have been presented, but none of them have been fully proven. Some researchers think that there is a delayed immune response that occurs 2 to 6 wk after infection[27,28]. In childhood, the early and pulmonary stages of COVID-19 are mild or asymptomatic. In the early stage, macrophages are activated and T helper cells begin to release cytokines. Subsequently, plasma and B cells produce antibodies and cause the immune response to intensify. This response results in the hyperinflammatory condition called MIS-C[28]. The fact that most children with MIS-C have positive serology and negative PCR tests supports this view. In addition, it has been reported that autoantibody responses against intestinal and endothelial cells are produced in children with MIS-C[29,30]. The fact that MIS-C is more common, especially in Africans shows the importance of genetic factors[31]. Another hypothesis suggests that neutrophil extracellular traps (NETs) play a role in the pathophysiology of MIS-C. The function of NETs is to trap the virus inside the cell. NETs stimulated by viruses cause hyperimmune and hyperinflammatory responses. These are thought to be increased in patients with respiratory failure and severe disease manifestations[32]. More studies are needed to elucidate the exact mechanism of myocardial damage seen in MIS-C.
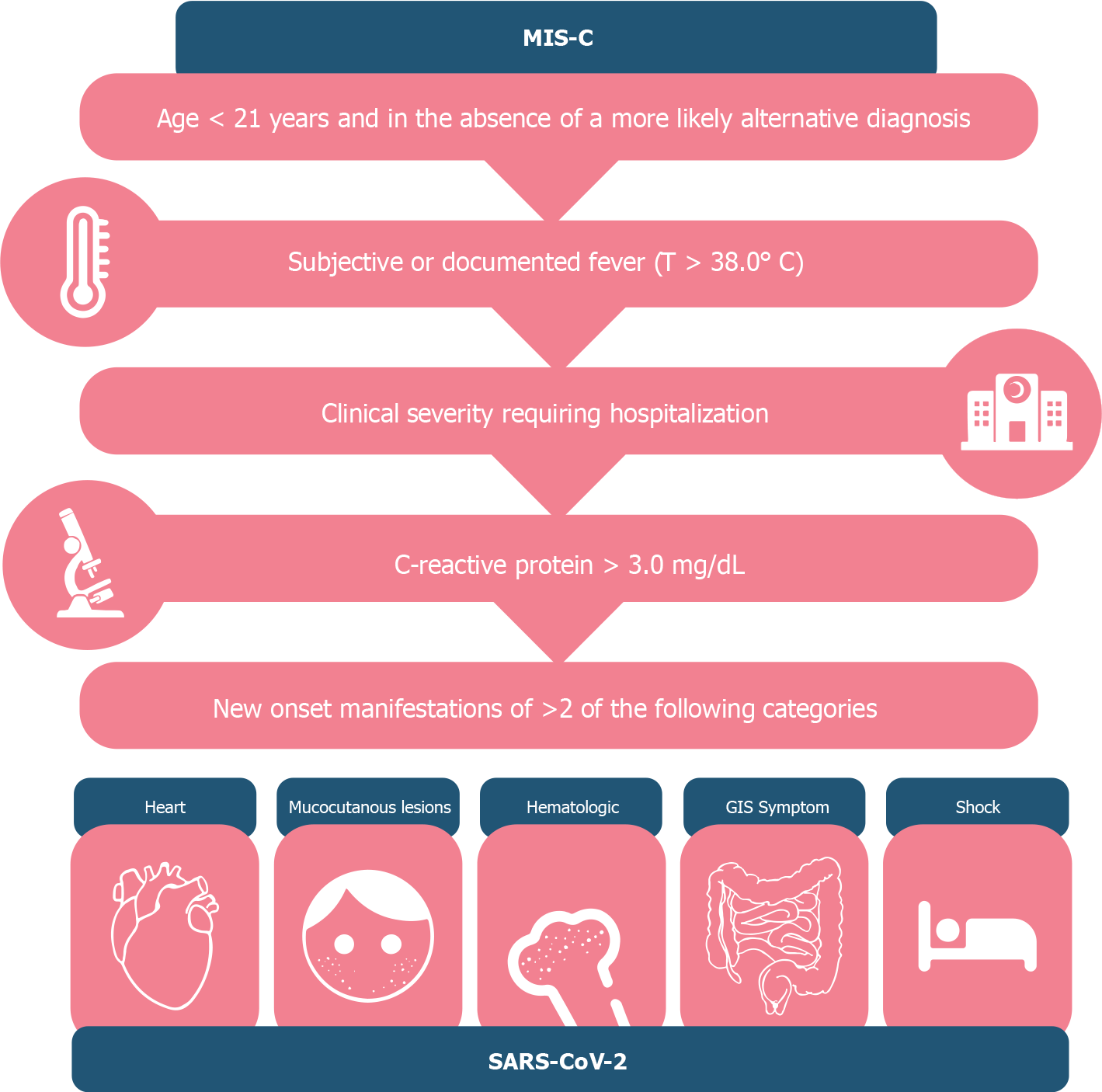
According to the American Centers for Disease Control and Prevention, in a person younger than 21 years of age, MIS-C criteria (Figure 2) without an alternative diagnosis are as follows:
Minimum 24-h history of subjective or objective fever ≥ 38.0°C; severe illness requiring hospitalization; two or more organ systems affected (i.e. cardiac, renal, respiratory, hematological, gastrointestinal, dermatological, neurological).
One or more of the following: elevated C-reactive protein (CRP), erythrocyte sedimentation rate, fibrinogen, procalcitonin, D-dimer, ferritin, lactate dehydrogenase or interleukin 6; elevated neutrophil or decreased lymphocyte counts; low albumin level.
Children with a diagnosis of MIS-C should be hospitalized and followed up by an experienced team. Children who are clinically well enough not to require hospitalization should not be considered to have MIS-C. In these children, close follow-up should be continued as infection markers may increase later. Supportive care is determined according to the severity of the symptoms. Patients presenting with a shock condition should be hospitalized in the intensive care unit as they may need inotropic support and mechanical ventilation[33]. Vasodilatory shock may be seen in some children, and vasopressor drugs should be used in this situation. However, milrinone could be used with caution due to its va
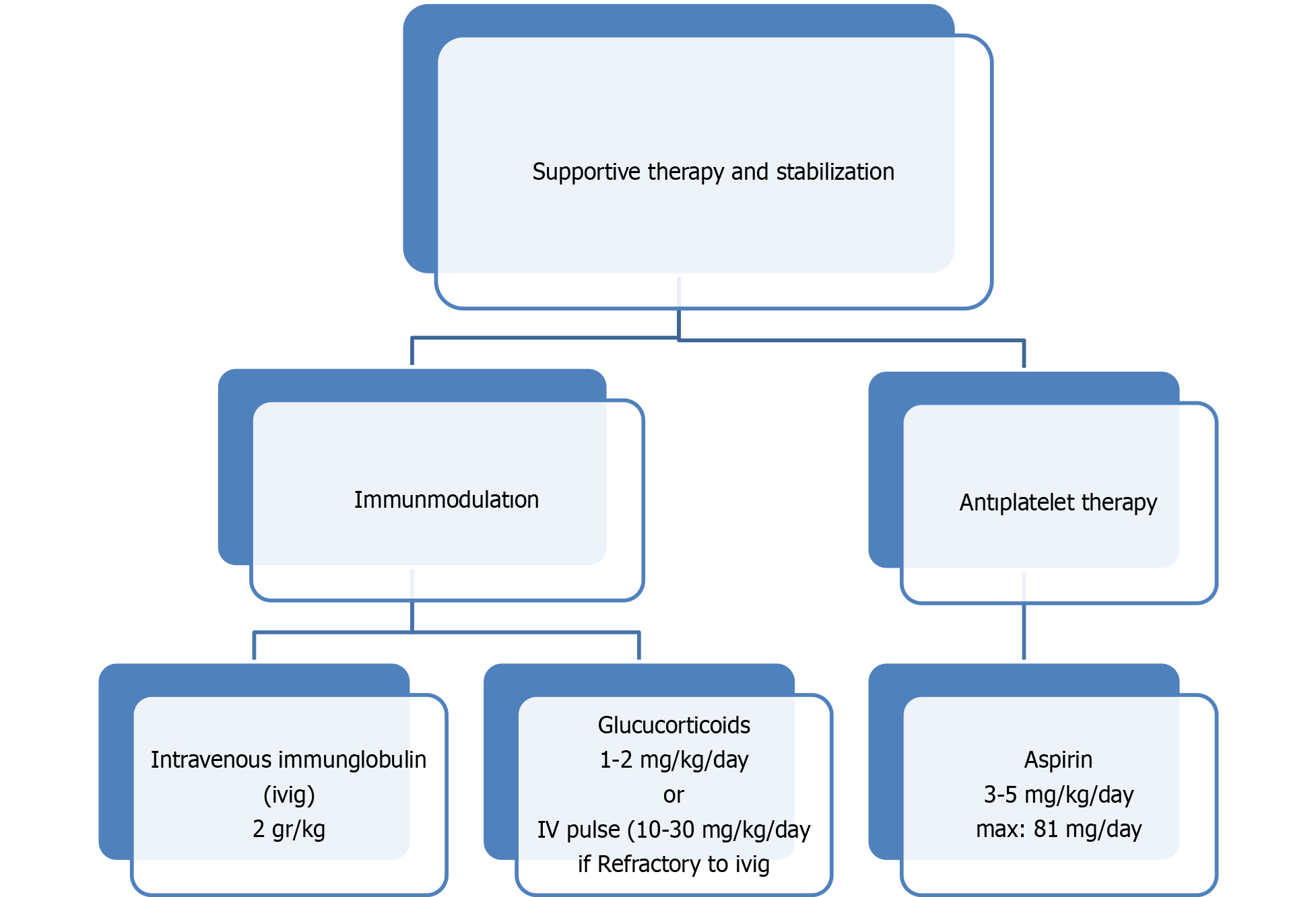
Although the exact pathogenesis of MIS-C is not understood, immune dysregulation is suggested to play an important role[35]. Autoantibody production resulting in activation of Fc-y receptors on neutrophils and macrophages and causing secretion of pro-inflammatory cytokines is one of these mechanisms[20,36-38]. Accordingly, immunomodulation is an important step in treatment. IVIG, glucocorticoids, and biological agents constitute the main treatment approaches (Figure 3)[39,40]. Treatment aims to correct cardiac dysfunction and damage in other organs by suppressing inflammation[27,41].
Steroids are used at low doses in patients with moderate to severe disease or at high doses in patients with refractory disease. Biological agents such as anakinra, tocilizumab, or infliximab are preferred in cases resistant to first-line therapies according to new guidelines[42]. In a series of 52 cases (30 MIS-C and 22 severe diseases) reported from Türkiye, it was emphasized that patients presented with different clinical pictures especially conjunctival hyperemia, high CRP values, and a low leukocyte count could be independent parameters used in diagnosis of the disease[43]. IVIG was administered to 30, a steroid to 27 (high dose steroid in 1 patient), anakinra to 26, plasmapheresis to 14, and various vasoactive agents to 13 patients with severe myocardial involvement. No deaths due to MIS-C were reported in this series. The common opinion of authors in the literature related to MIS-C is that mortality in children is very low with correct treatment in those diagnosed early. In the case of cardiac involvement, the importance of treatment under intensive care conditions has been emphasized.
Patients with MIS-C are at high risk of thrombotic complications for many reasons including hypercoagulopathy, possible endothelial damage, stasis due to immobilization, ventricular dysfunction, and coronary artery aneurysm. Low-dose aspirin (3-5 mg/kg/d, max. 81 mg) should be started and can be discontinued at 4 wk if there is no coronary artery aneurysm. Treatment with aspirin should be avoided in patients with active bleeding, significant bleeding risk, and/or a platelet count of 80000/μL. Therapeutic anticoagulation with enoxaparin or warfarin is recommended in patients with a coronary artery diameter Z-score > 10[44,45].
For hospitalized MIS-C patients with ventricular dysfunction or coronary artery dilatation, echocardiography (ECHO) should be repeated before discharge or on days 5-7. If the first echocardiogram is normal, it should be repeated on days 7-10. Repeat ECHO is recommended on days 7-10, 4-6 wk, 4-6 mo, and 9-12 mo after discharge[46,47].
In MIS-C patients, electrocardiography (ECG) should be performed at 48-h intervals. If grade 1 atrioventricular (AV) block is present, continuous telemetry monitoring is recommended. Holter ECG is recommended on the 7th-10th day after discharge if there is a grade 1 AV block or arrhythmia. Repeat ECG after 4-6 wk and 4-6 months, if there is arrhythmia or 1st-degree AV block, Holter ECG is recommended. After 4-6 months, if arrhythmia persists or ventricular dysfunction and increased troponin, brain-type natriuretic peptide values are present in the initial diagnosis, an exercise stress test is recommended[46,47].
Unlike adult patients, COVID-19 has a milder course in children. However, although MIS-C cases due to COVID-19 are rare, they cause deaths in children when not recognized early. Optimal results are obtained with intensive care unit treatments in cases diagnosed early. Early recognition of the disease and consideration of the latest guidelines are very important for the diagnosis and treatment of MIS-C. To clarify the pathogenesis of MIS-C, rational management strategies, and possible preventive measures are important for planning. MIS-C patients need to be registered to keep track of risk factors, and prognosis, and this is possibly the most appropriate way to identify sequelae. Genetic research will be vital to understanding why some children develop MIS-C after SARS-CoV-2 infection.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Immunology
Country/Territory of origin: Türkiye
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade B
P-Reviewer: Eid N, Malaysia S-Editor: Liu JH L-Editor: Webster JR P-Editor: Zhao S
| 1. | Davies P, Evans C, Kanthimathinathan HK, Lillie J, Brierley J, Waters G, Johnson M, Griffiths B, du Pré P, Mohammad Z, Deep A, Playfor S, Singh D, Inwald D, Jardine M, Ross O, Shetty N, Worrall M, Sinha R, Koul A, Whittaker E, Vyas H, Scholefield BR, Ramnarayan P. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: a multicentre observational study. Lancet Child Adolesc Health. 2020;4:669-677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 346] [Cited by in RCA: 305] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 2. | Dufort EM, Koumans EH, Chow EJ, Rosenthal EM, Muse A, Rowlands J, Barranco MA, Maxted AM, Rosenberg ES, Easton D, Udo T, Kumar J, Pulver W, Smith L, Hutton B, Blog D, Zucker H; New York State and Centers for Disease Control and Prevention Multisystem Inflammatory Syndrome in Children Investigation Team. Multisystem Inflammatory Syndrome in Children in New York State. N Engl J Med. 2020;383:347-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 864] [Cited by in RCA: 983] [Article Influence: 196.6] [Reference Citation Analysis (0)] |
| 3. | Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, Newburger JW, Kleinman LC, Heidemann SM, Martin AA, Singh AR, Li S, Tarquinio KM, Jaggi P, Oster ME, Zackai SP, Gillen J, Ratner AJ, Walsh RF, Fitzgerald JC, Keenaghan MA, Alharash H, Doymaz S, Clouser KN, Giuliano JS Jr, Gupta A, Parker RM, Maddux AB, Havalad V, Ramsingh S, Bukulmez H, Bradford TT, Smith LS, Tenforde MW, Carroll CL, Riggs BJ, Gertz SJ, Daube A, Lansell A, Coronado Munoz A, Hobbs CV, Marohn KL, Halasa NB, Patel MM, Randolph AG; Overcoming COVID-19 Investigators; CDC COVID-19 Response Team. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med. 2020;383:334-346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1587] [Cited by in RCA: 1856] [Article Influence: 371.2] [Reference Citation Analysis (0)] |
| 4. | Moraleda C, Serna-Pascual M, Soriano-Arandes A, Simó S, Epalza C, Santos M, Grasa C, Rodríguez M, Soto B, Gallego N, Ruiz Y, Urretavizcaya-Martínez M, Pareja M, Sanz-Santaeufemia FJ, Fumadó V, Lanaspa M, Jordan I, Prieto L, Belda S, Toral-Vázquez B, Rincón E, Gil-Villanueva N, Méndez-Echevarría A, Castillo-Serrano A, Rivière JG, Soler-Palacín P, Rojo P, Tagarro A; EPICO-AEP Working Group. Multi-inflammatory Syndrome in Children Related to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Spain. Clin Infect Dis. 2021;72:e397-e401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 81] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 5. | Chiotos K, Bassiri H, Behrens EM, Blatz AM, Chang J, Diorio C, Fitzgerald JC, Topjian A, John ARO. Multisystem Inflammatory Syndrome in Children During the Coronavirus 2019 Pandemic: A Case Series. J Pediatric Infect Dis Soc. 2020;9:393-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 255] [Cited by in RCA: 272] [Article Influence: 54.4] [Reference Citation Analysis (0)] |
| 6. | Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088-1095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1701] [Cited by in RCA: 1489] [Article Influence: 297.8] [Reference Citation Analysis (1)] |
| 7. | Belozerov KE, Kupreeva AD, Avrusin IS, Masalova VV, Kornishina TL, Isupova EA, Snegireva L, Kalashnikova O, Malekov D, Pozdnyakov A. Heart involvement in patients with multisystem inflammatory syndrome associated with SARS-CoV-2: A description of a series of clinical observations. Pediatr G N Speransky. 2021;100:35-45. |
| 8. | Adeghate EA, Eid N, Singh J. Mechanisms of COVID-19-induced heart failure: a short review. Heart Fail Rev. 2021;26:363-369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 9. | Kohli U, Meinert E, Chong G, Tesher M, Jani P. Fulminant myocarditis and atrial fibrillation in child with acute COVID-19. J Electrocardiol. 2022;73:150-152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Sabatino J, Ferrero P, Chessa M, Bianco F, Ciliberti P, Secinaro A, Oreto L, Avesani M, Bucciarelli V, Calcaterra G, Calabrò MP, Russo MG, Bassareo PP, Guccione P, Indolfi C, Di Salvo G. COVID-19 and Congenital Heart Disease: Results from a Nationwide Survey. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 11. | Mitrofanova LB, Makarov IA, Runov AL, Vonsky MS, Danilova IA, Sidorin VS, Moiseva OM, Konradi AO. Kliniko -morphological and molecular biological study of the myocardium in patients with COVID-19. Russ J Cardiol. 2022;27:4810. |
| 12. | Oberweis ML, Codreanu A, Boehm W, Olivier D, Pierron C, Tsobo C, Kohnen M, Abdelrahman TT, Nguyen NT, Wagner K, de la Fuente Garcia I. Pediatric Life-Threatening Coronavirus Disease 2019 With Myocarditis. Pediatr Infect Dis J. 2020;39:e147-e149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Fischer Q, Brillat-Savarin N, Ducrocq G, Ou P. Case report of an isolated myocarditis due to COVID-19 infection in a paediatric patient. Eur Heart J Case Rep. 2020;4:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Kesici S, Aykan HH, Orhan D, Bayrakci B. Fulminant COVID-19-related myocarditis in an infant. Eur Heart J. 2020;41:3021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 15. | Tseng YS, Herron C, Garcia R, Cashen K. Sustained ventricular tachycardia in a paediatric patient with acute COVID-19 myocarditis. Cardiol Young. 2021;31:1510-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607-1608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1565] [Cited by in RCA: 1766] [Article Influence: 353.2] [Reference Citation Analysis (0)] |
| 17. | Riollano-Cruz M, Akkoyun E, Briceno-Brito E, Kowalsky S, Reed J, Posada R, Sordillo EM, Tosi M, Trachtman R, Paniz-Mondolfi A. Multisystem inflammatory syndrome in children related to COVID-19: A New York City experience. J Med Virol. 2021;93:424-433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 18. | Ahmed M, Advani S, Moreira A, Zoretic S, Martinez J, Chorath K, Acosta S, Naqvi R, Burmeister-Morton F, Burmeister F, Tarriela A, Petershack M, Evans M, Hoang A, Rajasekaran K, Ahuja S. Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine. 2020;26:100527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 316] [Cited by in RCA: 358] [Article Influence: 71.6] [Reference Citation Analysis (0)] |
| 19. | Rodriguez-Smith JJ, Verweyen EL, Clay GM, Esteban YM, de Loizaga SR, Baker EJ, Do T, Dhakal S, Lang SM, Grom AA, Grier D, Schulert GS. Inflammatory biomarkers in COVID-19-associated multisystem inflammatory syndrome in children, Kawasaki disease, and macrophage activation syndrome: a cohort study. Lancet Rheumatol. 2021;3:e574-e584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 20. | Kabeerdoss J, Pilania RK, Karkhele R, Kumar TS, Danda D, Singh S. Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: immunological mechanisms, clinical manifestations and management. Rheumatol Int. 2021;41:19-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 232] [Cited by in RCA: 201] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 21. | Sanna G, Serrau G, Bassareo PP, Neroni P, Fanos V, Marcialis MA. Children's heart and COVID-19: Up-to-date evidence in the form of a systematic review. Eur J Pediatr. 2020;179:1079-1087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 89] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 22. | Royal College of Paediatrics and Child Health. Paediatric multisystem inflammatory syndrome temporally associated with COVID- 19 (PIMS) - guidance for clinicians. 2020; 178: 379-385. |
| 23. | CDC. Multisystem Inflammatory Syndrome in Children (MIS-C) in the United States. 2021. |
| 24. | Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, Roguski K, Wallace B, Prezzato E, Koumans EH, Lee EH, Geevarughese A, Lash MK, Reilly KH, Pulver WP, Thomas D, Feder KA, Hsu KK, Plipat N, Richardson G, Reid H, Lim S, Schmitz A, Pierce T, Hrapcak S, Datta D, Morris SB, Clarke K, Belay E; California MIS-C Response Team. COVID-19-Associated Multisystem Inflammatory Syndrome in Children - United States, March-July 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1074-1080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 416] [Cited by in RCA: 557] [Article Influence: 111.4] [Reference Citation Analysis (0)] |
| 25. | Belay ED, Abrams J, Oster ME, Giovanni J, Pierce T, Meng L, Prezzato E, Balachandran N, Openshaw JJ, Rosen HE, Kim M, Richardson G, Hand J, Tobin-D'Angelo M, Wilson S, Hartley A, Jones C, Kolsin J, Mohamed H, Colles Z, Hammett T, Patel P, Stierman B, Campbell AP, Godfred-Cato S. Trends in Geographic and Temporal Distribution of US Children With Multisystem Inflammatory Syndrome During the COVID-19 Pandemic. JAMA Pediatr. 2021;175:837-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 204] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 26. | Zambrano LD, Newhams MM, Olson SM, Halasa NB, Price AM, Boom JA, Sahni LC, Kamidani S, Tarquinio KM, Maddux AB, Heidemann SM, Bhumbra SS, Bline KE, Nofziger RA, Hobbs CV, Bradford TT, Cvijanovich NZ, Irby K, Mack EH, Cullimore ML, Pannaraj PS, Kong M, Walker TC, Gertz SJ, Michelson KN, Cameron MA, Chiotos K, Maamari M, Schuster JE, Orzel AO, Patel MM, Campbell AP, Randolph AG; Overcoming COVID-19 Investigators. Effectiveness of BNT162b2 (Pfizer-BioNTech) mRNA Vaccination Against Multisystem Inflammatory Syndrome in Children Among Persons Aged 12-18 Years - United States, July-December 2021. MMWR Morb Mortal Wkly Rep. 2022;71:52-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 204] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 27. | Nakra NA, Blumberg DA, Herrera-Guerra A, Lakshminrusimha S. Multi-System Inflammatory Syndrome in Children (MIS-C) Following SARS-CoV-2 Infection: Review of Clinical Presentation, Hypothetical Pathogenesis, and Proposed Management. Children (Basel). 2020;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 247] [Cited by in RCA: 270] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 28. | Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, Bonanomi E, D'Antiga L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395:1771-1778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1578] [Cited by in RCA: 1669] [Article Influence: 333.8] [Reference Citation Analysis (0)] |
| 29. | Jiang L, Tang K, Levin M, Irfan O, Morris SK, Wilson K, Klein JD, Bhutta ZA. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis. 2020;20:e276-e288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 526] [Cited by in RCA: 520] [Article Influence: 104.0] [Reference Citation Analysis (1)] |
| 30. | Gruber CN, Patel RS, Trachtman R, Lepow L, Amanat F, Krammer F, Wilson KM, Onel K, Geanon D, Tuballes K, Patel M, Mouskas K, O'Donnell T, Merritt E, Simons NW, Barcessat V, Del Valle DM, Udondem S, Kang G, Gangadharan S, Ofori-Amanfo G, Laserson U, Rahman A, Kim-Schulze S, Charney AW, Gnjatic S, Gelb BD, Merad M, Bogunovic D. Mapping Systemic Inflammation and Antibody Responses in Multisystem Inflammatory Syndrome in Children (MIS-C). Cell. 2020;183:982-995.e14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 422] [Cited by in RCA: 432] [Article Influence: 86.4] [Reference Citation Analysis (0)] |
| 31. | Pouletty M, Borocco C, Ouldali N, Caseris M, Basmaci R, Lachaume N, Bensaid P, Pichard S, Kouider H, Morelle G, Craiu I, Pondarre C, Deho A, Maroni A, Oualha M, Amoura Z, Haroche J, Chommeloux J, Bajolle F, Beyler C, Bonacorsi S, Carcelain G, Koné-Paut I, Bader-Meunier B, Faye A, Meinzer U, Galeotti C, Melki I. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. 2020;79:999-1006. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 397] [Cited by in RCA: 372] [Article Influence: 74.4] [Reference Citation Analysis (0)] |
| 32. | Zuo Y, Yalavarthi S, Shi H, Gockman K, Zuo M, Madison JA, Blair C, Weber A, Barnes BJ, Egeblad M, Woods RJ, Kanthi Y, Knight JS. Neutrophil extracellular traps in COVID-19. JCI Insight. 2020;5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 788] [Article Influence: 157.6] [Reference Citation Analysis (0)] |
| 33. | Matic KM. SARS-CoV-2 and Multisystem Inflammatory Syndrome In Children (MIS-C). Curr Probl Pediatr Adolesc Health Care. 2021;51:101000. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 34. | Ramcharan T, Nolan O, Lai CY, Prabhu N, Krishnamurthy R, Richter AG, Jyothish D, Kanthimathinathan HK, Welch SB, Hackett S, Al-Abadi E, Scholefield BR, Chikermane A. Paediatric Inflammatory Multisystem Syndrome: Temporally Associated with SARS-CoV-2 (PIMS-TS): Cardiac Features, Management and Short-Term Outcomes at a UK Tertiary Paediatric Hospital. Pediatr Cardiol. 2020;41:1391-1401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 236] [Cited by in RCA: 233] [Article Influence: 46.6] [Reference Citation Analysis (0)] |
| 35. | Ouldali N, Pouletty M, Mariani P, Beyler C, Blachier A, Bonacorsi S, Danis K, Chomton M, Maurice L, Le Bourgeois F, Caseris M, Gaschignard J, Poline J, Cohen R, Titomanlio L, Faye A, Melki I, Meinzer U. Emergence of Kawasaki disease related to SARS-CoV-2 infection in an epicentre of the French COVID-19 epidemic: a time-series analysis. Lancet Child Adolesc Health. 2020;4:662-668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 36. | Cheng MH, Zhang S, Porritt RA, Noval Rivas M, Paschold L, Willscher E, Binder M, Arditi M, Bahar I. Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation. Proc Natl Acad Sci U S A. 2020;117:25254-25262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 236] [Article Influence: 47.2] [Reference Citation Analysis (0)] |
| 37. | Noval Rivas M, Porritt RA, Cheng MH, Bahar I, Arditi M. COVID-19-associated multisystem inflammatory syndrome in children (MIS-C): A novel disease that mimics toxic shock syndrome-the superantigen hypothesis. J Allergy Clin Immunol. 2021;147:57-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 38. | Taghadosi M, Safarzadeh E, Asgarzadeh A, Roghani SA, Shamsi A, Jalili C, Assar S, Soufivand P, Pournazari M, Feizollahi P, Nicknam MH, Asghariazar V, Vaziri S, Shahriari H, Mohammadi A. Partners in crime: Autoantibodies complicit in COVID-19 pathogenesis. Rev Med Virol. 2023;33:e2412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 39. | Dove ML, Jaggi P, Kelleman M, Abuali M, Ang JY, Ballan W, Basu SK, Campbell MJ, Chikkabyrappa SM, Choueiter NF, Clouser KN, Corwin D, Edwards A, Gertz SJ, Ghassemzadeh R, Jarrah RJ, Katz SE, Knutson SM, Kuebler JD, Lighter J, Mikesell C, Mongkolrattanothai K, Morton T, Nakra NA, Olivero R, Osborne CM, Panesar LE, Parsons S, Patel RM, Schuette J, Thacker D, Tremoulet AH, Vidwan NK, Oster ME. Multisystem Inflammatory Syndrome in Children: Survey of Protocols for Early Hospital Evaluation and Management. J Pediatr. 2021;229:33-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 40. | Ouldali N, Toubiana J, Antona D, Javouhey E, Madhi F, Lorrot M, Léger PL, Galeotti C, Claude C, Wiedemann A, Lachaume N, Ovaert C, Dumortier M, Kahn JE, Mandelcwajg A, Percheron L, Biot B, Bordet J, Girardin ML, Yang DD, Grimaud M, Oualha M, Allali S, Bajolle F, Beyler C, Meinzer U, Levy M, Paulet AM, Levy C, Cohen R, Belot A, Angoulvant F; French Covid-19 Paediatric Inflammation Consortium. Association of Intravenous Immunoglobulins Plus Methylprednisolone vs Immunoglobulins Alone With Course of Fever in Multisystem Inflammatory Syndrome in Children. JAMA. 2021;325:855-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 246] [Article Influence: 61.5] [Reference Citation Analysis (0)] |
| 41. | DeBiasi RL. Immunotherapy for MIS-C - IVIG, Glucocorticoids, and Biologics. N Engl J Med. 2021;385:74-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 42. | Harwood R, Allin B, Jones CE, Whittaker E, Ramnarayan P, Ramanan AV, Kaleem M, Tulloh R, Peters MJ, Almond S, Davis PJ, Levin M, Tometzki A, Faust SN, Knight M, Kenny S; PIMS-TS National Consensus Management Study Group. A national consensus management pathway for paediatric inflammatory multisystem syndrome temporally associated with COVID-19 (PIMS-TS): results of a national Delphi process. Lancet Child Adolesc Health. 2021;5:133-141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 211] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 43. | Ozsurekci Y, Gürlevik S, Kesici S, Akca UK, Oygar PD, Aykac K, Karacanoglu D, Sarıtas Nakip O, Ilbay S, Katlan B, Ertugrul İ, Cengiz AB, Basaran O, Cura Yayla BC, Karakaya J, Bilginer Y, Bayrakci B, Ceyhan M, Ozen S. Multisystem inflammatory syndrome in children during the COVID-19 pandemic in Turkey: first report from the Eastern Mediterranean. Clin Rheumatol. 2021;40:3227-3237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 44. | Sharathkumar AA, Faustino EVS, Takemoto CM. How we approach thrombosis risk in children with COVID-19 infection and MIS-C. Pediatr Blood Cancer. 2021;68:e29049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 45. | McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, Baker AL, Jackson MA, Takahashi M, Shah PB, Kobayashi T, Wu MH, Saji TT, Pahl E; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; and Council on Epidemiology and Prevention. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation. 2017;135:e927-e999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1586] [Cited by in RCA: 2440] [Article Influence: 305.0] [Reference Citation Analysis (1)] |
| 46. | Sperotto F, Friedman KG, Son MBF, VanderPluym CJ, Newburger JW, Dionne A. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: a comprehensive review and proposed clinical approach. Eur J Pediatr. 2021;180:307-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 214] [Cited by in RCA: 249] [Article Influence: 62.3] [Reference Citation Analysis (0)] |
| 47. | Canter CE, Simpson KE. Diagnosis and treatment of myocarditis in children in the current era. Circulation. 2014;129:115-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 157] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 48. | Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R, Klingel K, Linhart A, Maisch B, McKenna W, Mogensen J, Pinto YM, Ristic A, Schultheiss HP, Seggewiss H, Tavazzi L, Thiene G, Yilmaz A, Charron P, Elliott PM; European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636-2648, 2648a. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 2273] [Article Influence: 189.4] [Reference Citation Analysis (0)] |