Published online Apr 26, 2024. doi: 10.4330/wjc.v16.i4.191
Peer-review started: December 27, 2023
First decision: January 17, 2024
Revised: January 26, 2024
Accepted: February 29, 2024
Article in press: February 29, 2024
Published online: April 26, 2024
Processing time: 118 Days and 1.9 Hours
Aspirin is widely used for primary or secondary prevention of ischemic events. At the same time, chronic aspirin consumption can affect blood clot formation during surgical intervention and increase intraoperative blood loss. This is especially important for high-risk surgery, including neurosurgery. Current European Society of Cardiology guidelines recommend aspirin interruption for at least 7 d before neurosurgical intervention, but this suggestion is not supported by clinical evidence. This narrative review presents evidence that challenges the necessity for aspirin interruption in neurosurgical patients, describes options for aspirin effect monitoring and the clinical implication of these methods, and summarizes current clinical data on bleeding risk associated with chronic aspirin therapy in neu
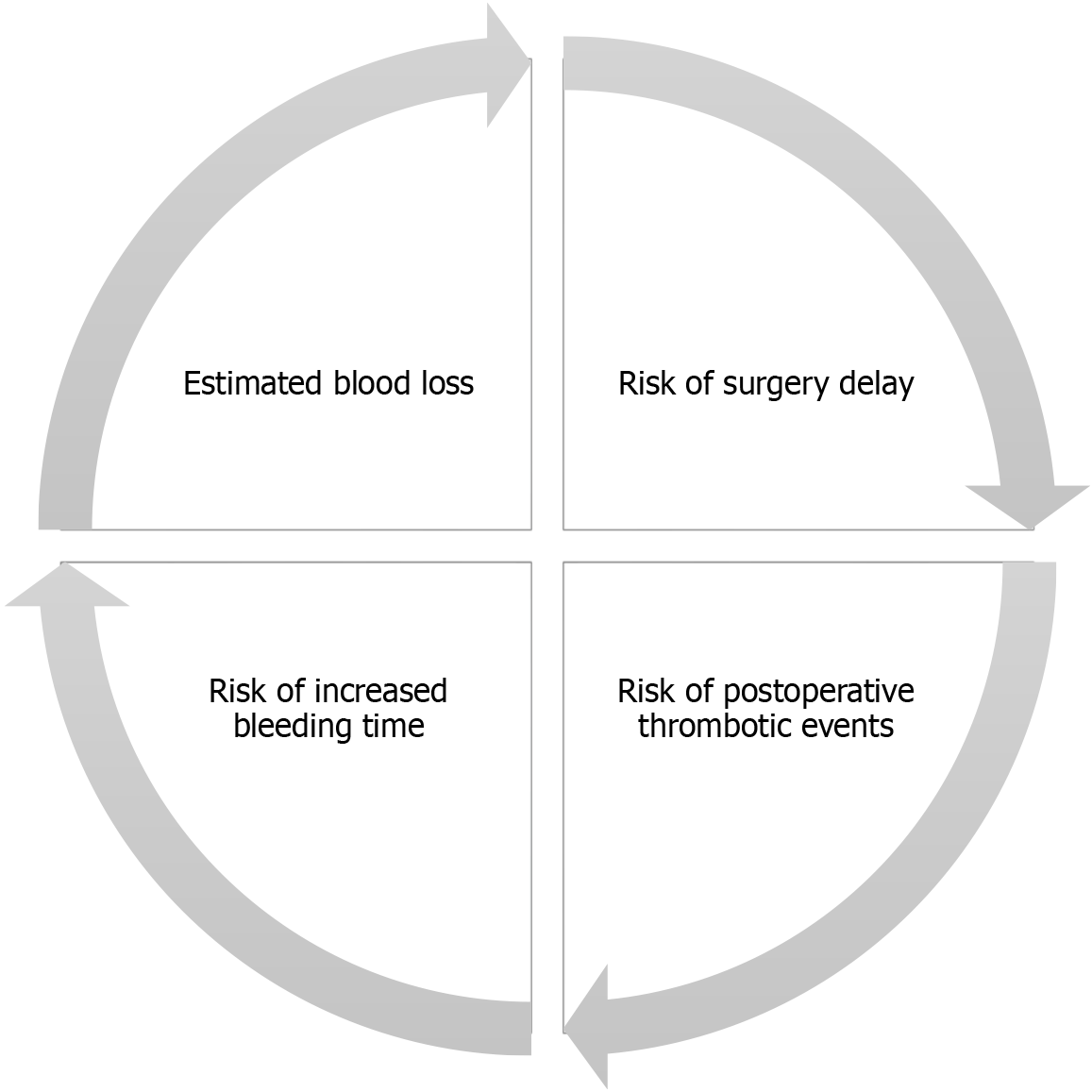
Core Tip: A decision on continuing or interrupting aspirin use before neurosurgical intervention should be made based on a discussion of specialists involved in perioperative management (neurosurgeon, anesthesiologist, cardiologist, etc), taking into account estimated blood loss; risk of complications associated with increased bleeding time; risk of postoperative ischemic complication associated with aspirin interruption; and risk of surgery postponement.
- Citation: Kulikov A, Konovalov A, Pugnaloni PP, Bilotta F. Aspirin interruption before neurosurgical interventions: A controversial problem. World J Cardiol 2024; 16(4): 191-198
- URL: https://www.wjgnet.com/1949-8462/full/v16/i4/191.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i4.191
Aspirin (acetylsalicylic acid, ASA) is a well-known inhibitor of platelet aggregation and due to this effect it is widely used for primary or secondary prevention of ischemic events[1]. At the same time, chronic aspirin consumption can affect blood clot formation during surgical intervention and increase intraoperative blood loss[2]. This is especially important for high-risk surgery, including neurosurgery, where even mild hemostatic disorders can provoke severe postoperative complications, such as acute intracranial hemorrhage[3].
Historically, the indication to interrupt aspirin therapy before neurosurgical procedures is based not on the clinical evidence, but on an expert’s consensus[4]. Over the years, this suggestion has consistently repeated in various guidelines, including 2022 European Society of Cardiology (ESC) guidelines, which state that “in patients with high peri-operative bleeding risk (e.g., undergoing spinal surgery or certain neurosurgical operations) aspirin should be discontinued for at least 7 d”[5]. However, clinical data, accumulated from observational studies in patients undergone spinal and intracranial surgery, do not prove a possible additional risk of postoperative hemorrhage associated with preoperative chronic aspirin therapy. Instead, there is a trend towards a beneficial effect of aspirin continuation concerning postope
This narrative review summarizes evidence that challenges the necessity for aspirin interruption in neurosurgical patients, describes options for aspirin effect monitoring and the clinical implication of these methods, and summarizes current clinical data on bleeding risk associated with chronic aspirin therapy in neurosurgical patients, including brain tumor surgery, cerebrovascular procedures, and spinal surgery.
The antiplatelet effect of aspirin is mediated by inhibiting cyclooxygenase (COX) activity inside platelets followed by suppression of thromboxane A2 (TXA2) synthesis[8]. TXA2 plays an important role in the amplification of platelet aggregation, and aspirin effectively depresses this mechanism of platelet activation[9].
Among the clinically important aspects of the antiplatelet effect of aspirin are the increased effectiveness of low doses (75-325 mg/d), due to the absence of concomitant inhibition of prostacyclin in endothelial cells, and irreversible COX inhibition, in contrast to other nonsteroidal anti-inflammatory drugs (NSAIDs). Ibuprofen, ketorolac, etc compete re
However, aspirin is recognized as a rather weak antiplatelet agent because it produces only partial platelet inhibition, and other non-TXA2–dependent activators of platelet aggregation [e.g., thrombin, ADP (adenosine diphosphate), and collagen] can bypass the aspirin-dependent mechanism and result in effective coagulation[8]. Moreover, up to 25% of patients can be resistant to conventional aspirin therapy[11].
The immediate clinical effect of aspirin uptake on primary hemostasis results in increased bleeding time[12]. Due to significant difficulties in standardizing this type of test, significant efforts in recent decades have been put into developing alternative and reliable measures of the antiplatelet effect of aspirin. Among the tested methods were light transmission aggregometry, serum thromboxane B2 concentration, impedance aggregometry, thromboelastography platelet mapping system, VerifyNow® assay (Werfen, Barcelona, Spain), platelet function analyzer–100 (Siemens Healthineers, Erlangen, Germany), etc. Each of these proposed methods demonstrated significant variability in the assessment of aspirin effect and poor correlation to each other[13,14]. Even more importantly, there is still no reliable clinical evidence of predictive value of any of these tests and correlation with clinically significant outcomes[15].
From a practical point of view, it seems important that non-specific viscoelastic tests (thromboelastography, rotational thromboelastometry), which were designed for integral assessment of blood clot formation, cannot demonstrate aspirin-associated hypocoagulation. At the same time, this phenomenon can be interpreted as the principal possibility of dense clot formation in the presence of aspirin[16].
Clinical evidence on aspirin continuation or discontinuation in general surgery is minimal. The largest seminal RCT (POISE-2), which included more than 10000 patients, revealed a higher frequency of major bleeding in the aspirin cohort with a hazard ratio 1.23 (95%CI: 1.01 to 1.49; P = 0.04)[2]. However, the design and conclusions of this trial were criticized due to the potential interaction of aspirin with perioperative anticoagulants and NSAIDs[17]. As a result, current guidelines on perioperative bleeding suggest that “aspirin should not be withdrawn peri-operatively unless the risk of bleeding exceeds the thrombotic risk from withholding the drug”[18]. But, as mentioned above, neurosurgical patients should be treated in a special way. Data on bleeding risk in different sub-cohorts of neurosurgical patients is presented below and summarized in Table 1.
| Ref. | No. of patients | Reported schemes | Key message |
| Brain tumor surgery | |||
| Merriman et al[19], 1979 | 2 | 4-20 tablets of aspirin 325 mg/d | Complications could be associated with preoperative aspirin consumption |
| Case report | |||
| Hanalioglu et al[20], 2019 | 1291 | 3 groups: | ASA was not associated with increased bleeding risk |
| Retrospective single-center, cohort study | No ASA (1068 patients) | ||
| Stopped ASA (at least 7 d before surgery – 104 patients) | |||
| Continued ASA (119 patients) | |||
| Rychen et al[21], 2023 | 312 | ASA was continued perioperatively for extraaxial surgery, and discontinued 2 d before intraaxial surgery (83 patients). No ASA in prospective control (106 patients) and long-term ASA discontinuation in retrospective control group (123 patients) | Presented protocol of perioperative antithrombotics management was not associated with an increased hemorrhagic risk |
| Prospective cohort study with retrospective control | |||
| Enciu et al[22], 2023 | 304 | 2 groups: | Short-term (even < 2 d) discontinuation of low-dose aspirin was not associated with increased bleeding risk |
| Retrospective single-center, cohort study | Short-term ASA discontinuation (lower than 7 d) (45 patients) | ||
| Standard-term ASA discontinuation (259 patients) | |||
| Rychen et al[7], 2023 | 646 (7 studies) | ASA was continued perioperatively in 61.8% and discontinued in 38.2% of the cases | Perioperative ASA continuation in elective craniotomies was not associated with an increased hemorrhagic risk |
| Systematic review | |||
| Cerebrovascular surgery | |||
| Schubert et al[23], 2014 | 158 | ASA was prescribed in 138 patients pre- or intraoperatively | Antiplatelet therapy did not increase the risk of hemorrhage, but improved outcomes after revascularization procedures |
| Retrospective single-center, cohort study | |||
| Nakamizo et al[24], 2017 | 401 | 2 groups: | Intracranial hemorrhage after aneurism clipping was more frequent in the antithrombotics group |
| Retrospective single-center, cohort study | Continued antithrombotics, including ASA (45 patients) | ||
| No antithrombotics (259 patients) | |||
| Rashidi et al[25], 2021 | 200 | 2 groups: | Continued ASA use was not associated with an increased risk of a postoperative hemorrhage |
| Retrospective single-center, cohort study | Continued ASA or short-term ASA discontinuation (lower than 7 d) (32 patients) | ||
| No ASA (168 patients) | |||
| Ebel et al[26], 2021 | 215 | 2 groups: | Short (≤ 5 d) aspirin discontinuation time did not appear to have increased rates of postoperative bleeding |
| Retrospective single-center, cohort study | Patients were treated with antithrombotics (50 patients) | ||
| No antithrombotics (165 patients) | |||
| Spinal surgery | |||
| Goes et al[6], 2017 | 370 (3 studies) | 2 groups: | There is no difference in perioperative complications between aspirin continuation and discontinuation |
| Meta-analysis | ASA-continuing group (170 patients) | ||
| ASA-discontinuing group (200 patients) | |||
| Zhang et al[29], 2017 | 414 (4 studies) | 2 groups: | Continued aspirin administration do not have an increased risk for bleeding |
| Meta-analysis | ASA-continuing group | ||
| ASA-discontinuing group | |||
| Cheng et al[30], 2018 | 1173 (7 studies) | 3 groups: | No difference in intraoperative blood loss, operation time, and postoperative complications |
| Systematic review | No ASA therapy (587 patients) | ||
| Stopped ASA (3-10 d before surgery – 416 patients) | |||
| Continued ASA (170 patients | |||
| Claydon et al[28], 2022 | 364 | 2 groups: | There was no association of low-dose ASA continuation with increased blood loss |
| Prospective, multi-center observational cohort study | ASA-continuing group (21 patients) | ||
| No ASA group | |||
| Tarukado et al[27], 2023 | 88 | 3 groups: | Continuing ASA did not affect perioperative complications or clinical outcomes |
| Retrospective single-center, cohort study | No antithrombotics (65 patients) | ||
| Stopped ASA (9 patients) | |||
| Continued ASA (14 patients) | |||
One of the initial concerns on the safety of perioperative aspirin consumption in brain tumor surgery was presented in a small case series[19]. This study was based on two cases where postoperative hematomas were seemingly caused by a platelet defect due to aspirin use. This defect, not detectable by standard bleeding and clotting tests, could arise from both massive and small doses of aspirin. Highlighting the serious implications for neurosurgery, the study pointed out that such a defect can be effectively treated with platelet transfusions.
Data from a more recent retrospective study examining 1291 patients who underwent elective intracranial tumor surgery is much more reasonable[20]. The patients were divided based on their aspirin usage into three groups: no aspirin, stopped aspirin, and continued aspirin. The stopped-aspirin group included 104 patients (108 operations), and the continued-aspirin group had 119 patients (126 operations). The study highlighted that operative blood loss and complication rates were not significantly different between the groups, suggesting that perioperative aspirin use does not elevate hemorrhagic risk.
A similar conclusion was reached in a prospective cohort study, focused on the perioperative management of antithrombotics (AT) in elective intracranial procedures[21]. This analysis involved 312 patients divided into three groups: 83 patients (27%) continued AT, 106 (34%) did not use AT, and 123 (39%) were historical AT users. The study's approach was to continue aspirin for extraaxial or shunt surgeries and stop aspirin 2 d before intervention for intraaxial patho
The risk of postoperative bleeding in patients undergoing endoscopic endonasal surgery for pituitary adenomas with short-term discontinuation of low-dose aspirin was the focus of another retrospective study[22]. It included 304 patients, and 45 of them (14.8%) had short-term perioperative aspirin discontinuation. This study found no increased rate of postoperative bleeding in patients who discontinued aspirin for a short period.
The risk of postoperative hematoma formation in patients undergoing stereotactic brain biopsies is a critical concern in clinical practice because in these clinical settings, there is no direct visual control of potential vascular injury. Unfortunately, we did not succeed in finding any clinical evidence of additional risk of such complications in patients on chronic aspirin therapy.
Risk of hemorrhagic complication in 158 patients who underwent revascularization surgery for moyamoya disease or cerebrovascular atherosclerotic disease was assessed in a retrospective observational study[23]. The study had a low complication rate with a high patency rate of 97%, and no mortality. Early morbidity was 10.7%, and ischemia was seen in 6.9% of patients. It was found that neither the type of treated pathology nor the surgical technique significantly influenced outcomes. Notably, antiplatelet therapy did not increase the risk of hemorrhage, but improved outcomes.
Patients who underwent craniotomy for unruptured intracranial aneurysm were included in another retrospective study[24]. Data on 401 cases were analyzed. Patients were divided into two groups: those who received perioperative antithrombotic treatment (45 patients) and those who did not (356 patients). The study found no significant difference in mortality, morbidity, or symptomatic brain infarction between the groups. However, intracranial hemorrhage was more frequent in the antithrombotic group. Posterior aneurysm location and surgical procedure were associated with severe morbidity, and intracranial hemorrhage was associated with antithrombotic treatment.
A more recent retrospective study did not find additional bleeding risk in patients on continued aspirin treatment undergoing cerebral aneurysm surgery[25]. 200 consecutive clipping procedures were analyzed and found that postoperative hemorrhage occurred in 3.1% of patients with aspirin and 3.0% of patients without aspirin. The difference was not statistically significant. However, cardiopulmonary complications were more frequent in the aspirin group. The study suggests that aspirin use may be relatively safe in patients with increased cardiovascular risk and emergency cerebrovascular surgery. Patients undergoing craniotomy for the treatment of neurovascular lesions with short (≤ 5 d) aspirin discontinuation time did not appear to have increased rates of postoperative bleeding in another retrospective study, which included 215 cases[26].
A relatively large amount of clinical evidence has accumulated to date regarding the safety of continued aspirin use in spinal neurosurgery. For instance, in a retrospective cohort study, which included 88 patients, the safety of continuing low-dose aspirin during microendoscopic laminectomy was investigated[27]. The patients were categorized into three groups based on their anticoagulation therapy status. There was no statistically significant difference between the three groups in operation time. The study concluded that continuing aspirin in these clinical settings did not affect perioperative complications or clinical outcomes. Another prospective multi-center observational cohort study focused on risk factors affecting blood loss during elective anterior lumbar surgery. Based on an analysis of 364 patients, the continuation of low-dose aspirin was not associated with increased blood loss[28].
Previous studies were systematized in a couple of reviews[29,30]. They assessed the impact of aspirin on bleeding and cardiovascular events in the perioperative period and concluded that continuation of aspirin does not increase the risk of blood loss, operative time, or postoperative blood transfusion during spinal surgery. However, both reviews acknowledged the need for more research to understand the relationship between aspirin use and cardiovascular risks, emphasizing the importance of considering individual patient risks when managing aspirin therapy in spinal surgeries.
Presented clinical data reflects the paucity of reliable evidence on clinical decision-making for continuing or interrupting aspirin uptake in the perioperative period in patients scheduled for elective neurosurgical procedures. Potential disturbance in intraoperative blood clot formation stimulates a defensive approach, but the impact on the outcome of aspirin uptake in these specific clinical settings remains uncertain. Inconsistency in clinical data provokes variability in clinical practice[31,32].
Moreover, even guidelines on this issue do not coincide with each other. For instance, European Society of Anaes
Of course, the decision on continuing or interrupting aspirin in particular cases should be made based on the dis
It should be taken into account that high estimated blood loss can be aggravated by the antiplatelet effect of aspirin. This is particularly important in cases where surgical manipulation would be performed inside the tissues with the abnormal structure of the vascular wall, i.e. neoplasms. This risk is presumably lower for cerebrovascular and spinal surgery. On the other hand, the risk of thrombotic complication can outweigh the bleeding risk in patients with high cardiac risk (history of myocardial infarction, coronary stenting, unstable angina etc, which are among the most common indications for chronic aspirin consumption). In such cases, aspirin continuation can provide a better outcome.
Furthermore, in neurosurgical practice, it is frequently necessary to treat patients who can have serious consequences due to the delay in surgical intervention (e.g., intracranial bleeding of a brain lesion, progressive neurologic deficit due to mass effect, occurrence of seizures in patients with intracranial mass, etc). Risk-benefit balance of aspirin interruption in such cases remains uncertain, but ESC recommendation for aspirin discontinuation might cause the underestimation of risks and harm of surgery delay.
Aspirin interruption before neurosurgical interventions remains a controversial clinical issue. Neurosurgical patients are very heterogeneous and might present different risks of perioperative bleeding. But the current form of recommendation of aspirin discontinuation makes all clinical situations equal and motivates physicians to make the same clinical decisions in any case. Future studies should be designed for rational and evidence-based clinical decision-making.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Health care sciences and services
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Teragawa H, Japan S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Zhao S
| 1. | Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, Benetos A, Biffi A, Boavida JM, Capodanno D, Cosyns B, Crawford C, Davos CH, Desormais I, Di Angelantonio E, Franco OH, Halvorsen S, Hobbs FDR, Hollander M, Jankowska EA, Michal M, Sacco S, Sattar N, Tokgozoglu L, Tonstad S, Tsioufis KP, van Dis I, van Gelder IC, Wanner C, Williams B; ESC National Cardiac Societies; ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227-3337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3739] [Cited by in RCA: 3312] [Article Influence: 828.0] [Reference Citation Analysis (0)] |
| 2. | Devereaux PJ, Mrkobrada M, Sessler DI, Leslie K, Alonso-Coello P, Kurz A, Villar JC, Sigamani A, Biccard BM, Meyhoff CS, Parlow JL, Guyatt G, Robinson A, Garg AX, Rodseth RN, Botto F, Lurati Buse G, Xavier D, Chan MT, Tiboni M, Cook D, Kumar PA, Forget P, Malaga G, Fleischmann E, Amir M, Eikelboom J, Mizera R, Torres D, Wang CY, VanHelder T, Paniagua P, Berwanger O, Srinathan S, Graham M, Pasin L, Le Manach Y, Gao P, Pogue J, Whitlock R, Lamy A, Kearon C, Baigent C, Chow C, Pettit S, Chrolavicius S, Yusuf S; POISE-2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370:1494-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 586] [Cited by in RCA: 590] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 3. | Lassen B, Helseth E, Rønning P, Scheie D, Johannesen TB, Mæhlen J, Langmoen IA, Meling TR. Surgical mortality at 30 days and complications leading to recraniotomy in 2630 consecutive craniotomies for intracranial tumors. Neurosurgery. 2011;68:1259-68; discussion 1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 4. | James DN, Fernandes JR, Calder I, Smith M. Low-dose aspirin and intracranial surgery. A survey of the opinions of consultant neuroanaesthetists in the UK. Anaesthesia. 1997;52:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Mehilli J, Halvorsen S. The '10 commandments' for the 2022 European Society of Cardiology guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur Heart J. 2023;44:336-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Goes R, Muskens IS, Smith TR, Mekary RA, Broekman MLD, Moojen WA. Risk of aspirin continuation in spinal surgery: a systematic review and meta-analysis. Spine J. 2017;17:1939-1946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Rychen J, Saemann A, Fingerlin T, Guzman R, Mariani L, Greuter L, Soleman J. Risks and benefits of continuation and discontinuation of aspirin in elective craniotomies: a systematic review and pooled-analysis. Acta Neurochir (Wien). 2023;165:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 8. | Awtry EH, Loscalzo J. Aspirin. Circulation. 2000;101:1206-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 526] [Cited by in RCA: 536] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 9. | FitzGerald GA. Mechanisms of platelet activation: thromboxane A2 as an amplifying signal for other agonists. Am J Cardiol. 1991;68:11B-15B. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 240] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 10. | Schafer AI. Effects of nonsteroidal antiinflammatory drugs on platelet function and systemic hemostasis. J Clin Pharmacol. 1995;35:209-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 239] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 11. | Helgason CM, Bolin KM, Hoff JA, Winkler SR, Mangat A, Tortorice KL, Brace LD. Development of aspirin resistance in persons with previous ischemic stroke. Stroke. 1994;25:2331-2336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 266] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 12. | Amrein PC, Ellman L, Harris WH. Aspirin-induced prolongation of bleeding time and perioperative blood loss. JAMA. 1981;245:1825-1828. [PubMed] [DOI] [Full Text] |
| 13. | Cattaneo M. Laboratory detection of 'aspirin resistance': what test should we use (if any)? Eur Heart J. 2007;28:1673-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 75] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Aradi D, Storey RF, Komócsi A, Trenk D, Gulba D, Kiss RG, Husted S, Bonello L, Sibbing D, Collet JP, Huber K; Working Group on Thrombosis of the European Society of Cardiology. Expert position paper on the role of platelet function testing in patients undergoing percutaneous coronary intervention. Eur Heart J. 2014;35:209-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 195] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 15. | Karger R, Reuter K, Rohlfs J, Nimsky C, Sure U, Kretschmer V. The Platelet Function Analyzer (PFA-100) as a Screening Tool in Neurosurgery. ISRN Hematol. 2012;2012:839242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Orlikowski CE, Payne AJ, Moodley J, Rocke DA. Thrombelastography after aspirin ingestion in pregnant and non-pregnant subjects. Br J Anaesth. 1992;69:159-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 44] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Filipescu DC, Stefan MG, Valeanu L, Popescu WM. Perioperative management of antiplatelet therapy in noncardiac surgery. Curr Opin Anaesthesiol. 2020;33:454-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Kietaibl S, Ahmed A, Afshari A, Albaladejo P, Aldecoa C, Barauskas G, De Robertis E, Faraoni D, Filipescu DC, Fries D, Godier A, Haas T, Jacob M, Lancé MD, Llau JV, Meier J, Molnar Z, Mora L, Rahe-Meyer N, Samama CM, Scarlatescu E, Schlimp C, Wikkelsø AJ, Zacharowski K. Management of severe peri-operative bleeding: Guidelines from the European Society of Anaesthesiology and Intensive Care: Second update 2022. Eur J Anaesthesiol. 2023;40:226-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 146] [Article Influence: 73.0] [Reference Citation Analysis (1)] |
| 19. | Merriman E, Bell W, Long DM. Surgical postoperative bleeding associated with aspirin ingestion. Report of two cases. J Neurosurg. 1979;50:682-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Hanalioglu S, Sahin B, Sahin OS, Kozan A, Ucer M, Cikla U, Goodman SL, Baskaya MK. Effect of perioperative aspirin use on hemorrhagic complications in elective craniotomy for brain tumors: results of a single-center, retrospective cohort study. J Neurosurg. 2019;132:1529-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 21. | Rychen J, Weiger VF, Halbeisen FS, Ebel F, Ullmann M, Mariani L, Guzman R, Soleman J. Perioperative continuation or ultra-early resumption of antithrombotics in elective neurosurgical cranial procedures. Neurosurg Focus. 2023;55:E6. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Enciu A, Loeschner D, Alhallak M, Kellner G, Meyer A, Lauten A, Steinbrecher A, Gerlach R. Management and risk of postoperative bleeding in patients with low-dose antiplatelet aspirin medication during endoscopic endonasal surgery for pituitary adenomas. Acta Neurochir (Wien). 2023;165:2995-3001. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Schubert GA, Biermann P, Weiss C, Seiz M, Vajkoczy P, Schmiedek P, Thomé C. Risk profile in extracranial/intracranial bypass surgery--the role of antiplatelet agents, disease pathology, and surgical technique in 168 direct revascularization procedures. World Neurosurg. 2014;82:672-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Nakamizo A, Michiwaki Y, Kawano Y, Amano T, Matsuo S, Fujioka Y, Tsumoto T, Yasaka M, Okada Y. Impact of antithrombotic treatment on clinical outcomes after craniotomy for unruptured intracranial aneurysm. Clin Neurol Neurosurg. 2017;161:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Rashidi A, Lilla N, Skalej M, Sandalcioglu IE, Luchtmann M. Impact of acetylsalicylic acid in patients undergoing cerebral aneurysm surgery - should the neurosurgeon really worry about it? Neurosurg Rev. 2021;44:2889-2898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 26. | Ebel F, Ullmann M, Guzman R, Soleman J. Does the discontinuation time of antiplatelet or anticoagulation treatment affect hemorrhagic complications in patients undergoing craniotomy for neurovascular lesions? Br J Neurosurg. 2021;35:619-624. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Tarukado K, Ono T, Doi T, Harimaya K, Nakashima Y. Safety and Clinical Results of Continuous Low-Dose Aspirin in Microendoscopic Laminectomy. Spine Surg Relat Res. 2023;7:350-355. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Claydon MH, Biddau DT, Laggoune JP, Malham GM. Who bleeds during elective anterior lumbar surgery? N Am Spine Soc J. 2022;12:100180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 29. | Zhang C, Wang G, Liu X, Li Y, Sun J. Safety of continuing aspirin therapy during spinal surgery: A systematic review and meta-analysis. Medicine (Baltimore). 2017;96:e8603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Cheng A, Poon MTC, Demetriades AK. Aspirin therapy discontinuation and intraoperative blood loss in spinal surgery: a systematic review. Neurosurg Rev. 2018;41:1029-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Korinth MC. Low-dose aspirin before intracranial surgery--results of a survey among neurosurgeons in Germany. Acta Neurochir (Wien). 2006;148:1189-96; discussion 1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Fiaschi P, Iaccarino C, Stefini R, Prior E, Prior A, Zona G. Clinical practice for antiplatelet and anticoagulant therapy in neurosurgery: data from an Italian survey and summary of current recommendations - part I, antiplatelet therapy. Neurosurg Rev. 2021;44:485-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |