Published online Oct 26, 2024. doi: 10.4330/wjc.v16.i10.595
Revised: August 21, 2024
Accepted: September 11, 2024
Published online: October 26, 2024
Processing time: 246 Days and 1.8 Hours
Unroofed coronary sinus (UCS) is a rare subtype of atrial septal defect. It is fre
This report describes a rare case of an adolescent patient with UCS featuring atrial situs solitus, absence of the right superior vena cava and a persistent left superior vena cava draining into the left atrium consistent with total unroofing of the co
UCS is a complex condition requiring careful consideration of associated ano
Core Tip: In this report, we present an exceedingly rare case of a teenager with an unroofed coronary sinus and a single persistent left superior vena cava in conjugation with severe mitral regurgitation secondary to redundant and prolapsing leaflets, in the absence of other associated cardiac anomalies. This peculiar condition was detected by echocardiography and corrected by appropriate surgical intervention.
- Citation: Bitar F, Bulbul Z, Jassar Y, Zareef R, Abboud J, Arabi M, Bitar FF. Unroofed coronary sinus, left-sided superior vena cava and mitral insufficiency: A case report and review of the literature. World J Cardiol 2024; 16(10): 595-603
- URL: https://www.wjgnet.com/1949-8462/full/v16/i10/595.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i10.595
Unroofed coronary sinus (UCS), also known as coronary sinus (CS) septal defect, denotes a particularly rare and uncommon subtype of atrial septal defects, accounting for less than 1% of all cases within this category[1]. It arises from the incomplete development of the left atrial venous folds during embryogenesis and was first elucidated by Raghib and colleagues in 1965[2]. This anomaly manifests as a communication between the left atrium and the CS, secondary to partial or complete absence of the CS roof, resulting in a left to right shunt.
UCS is an atypical atrial septal defect as it is characterized by interatrial shunting across a normal structure, the CS ostium[3,4]. It often co-exists with a persistent left superior vena cava (LSVC) and other concomitant cardiac abnorma
In this report, we present a unique case of absent RSVC in a visceroatrial situs solitus, persistent LSVC draining into UCS, associated with severe mitral insufficiency in the absence of atrioventricular septal defect. Furthermore, we present a comprehensive examination of the existing literature, tackling the diagnostic hurdles and exploring surgical inter
A 19-year-old female was referred to our Children's Heart Center with the diagnosis of an atrial septal defect for further evaluation and treatment.
The patient had minimal exercise intolerance and assumed a sedentary lifestyle. She had normal growth and deve
Besides her congenital heart disease, she did not have a significant medical history.
She has no family history of congenital heart disease.
On physical examination, her vital signs were normal except for an oxygen saturation of 95%. She had a grade 2/6 systolic murmur at the apex and another grade 2/6 systolic ejection murmur at the left upper sternal border with fixed splitting of the second heart sound.
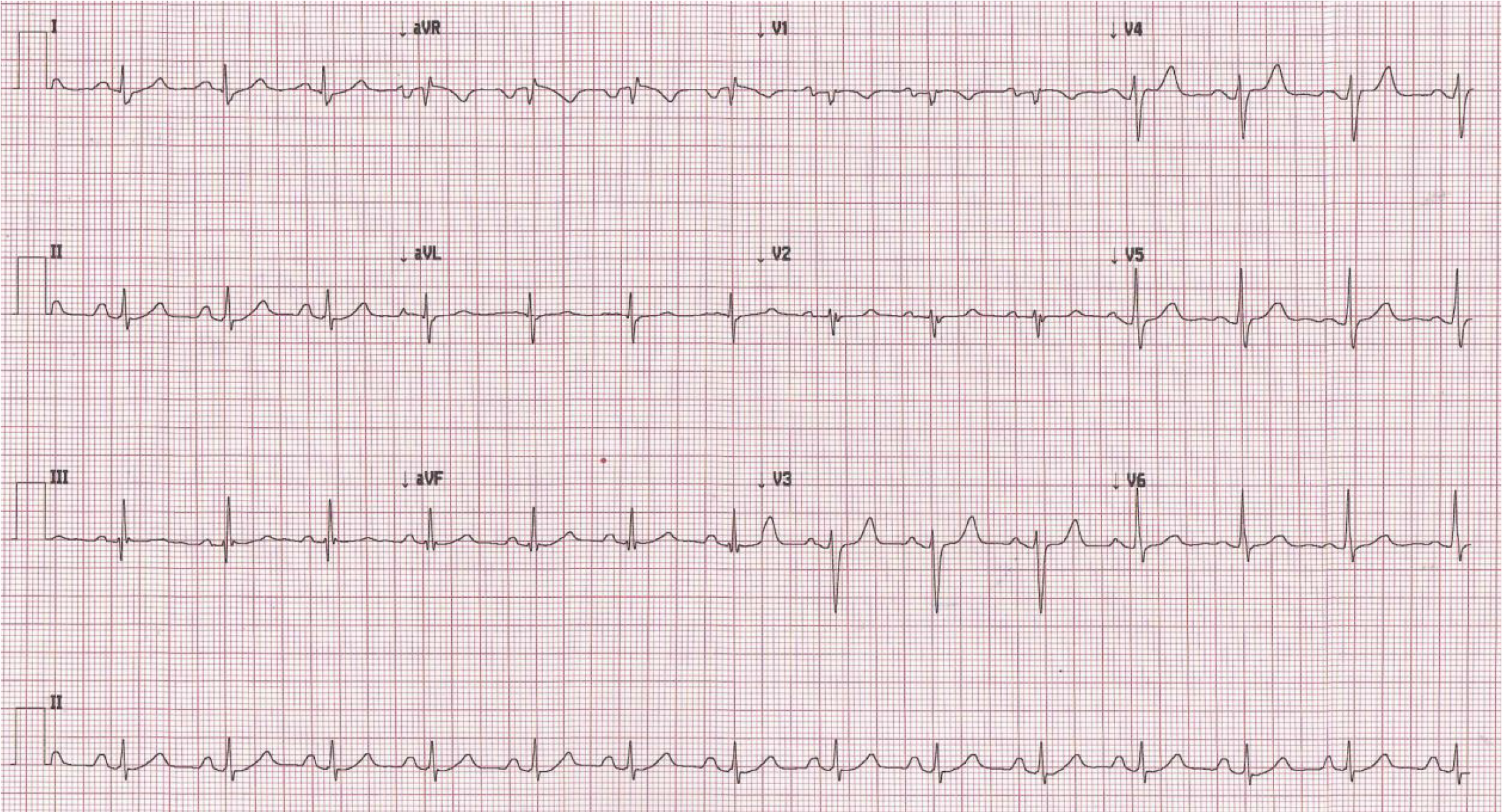
An electrocardiogram (ECG) revealed a normal sinus rhythm and QRS frontal axis, with a wide P wave suggestive of left atrial enlargement (Figure 1).
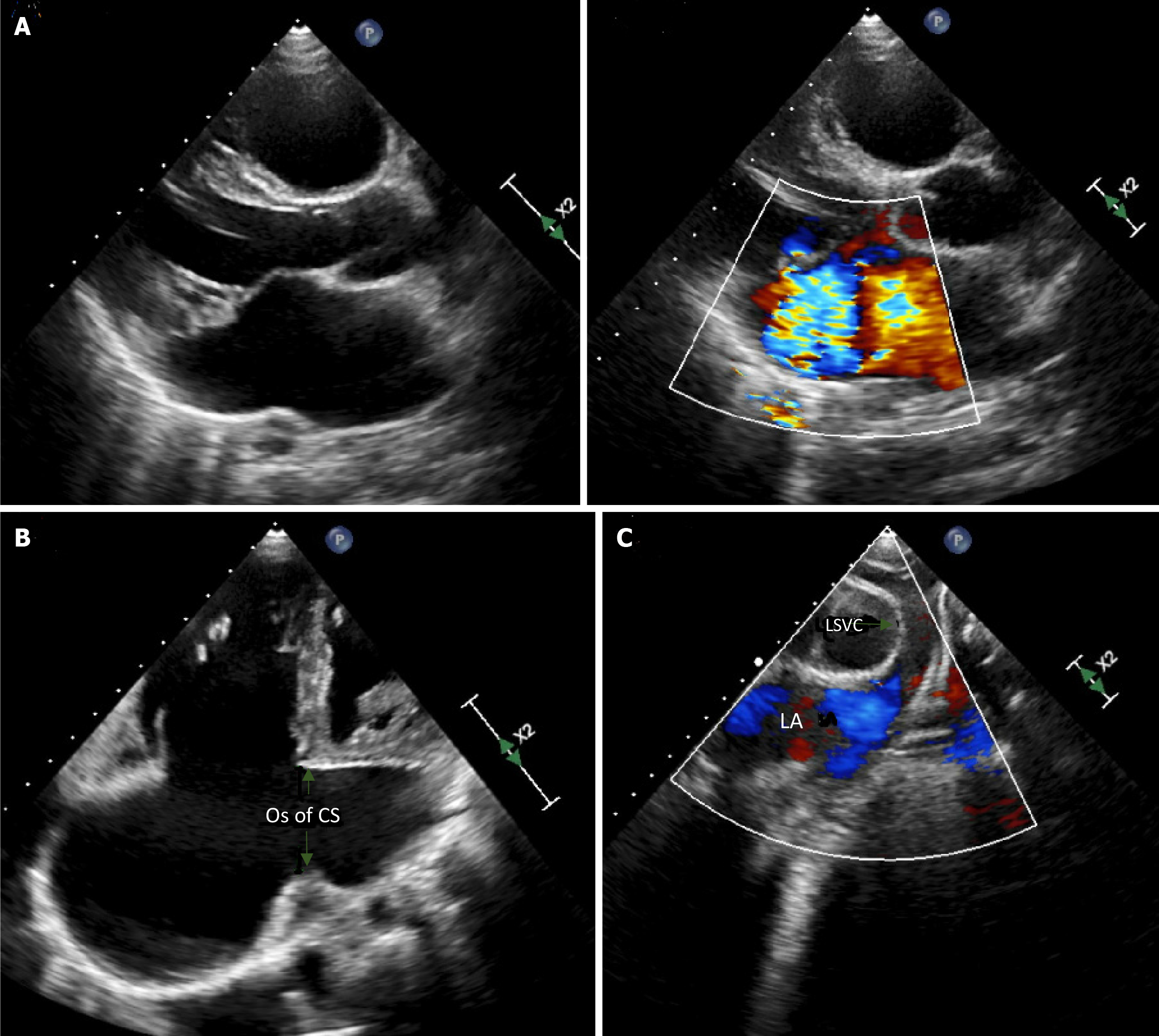
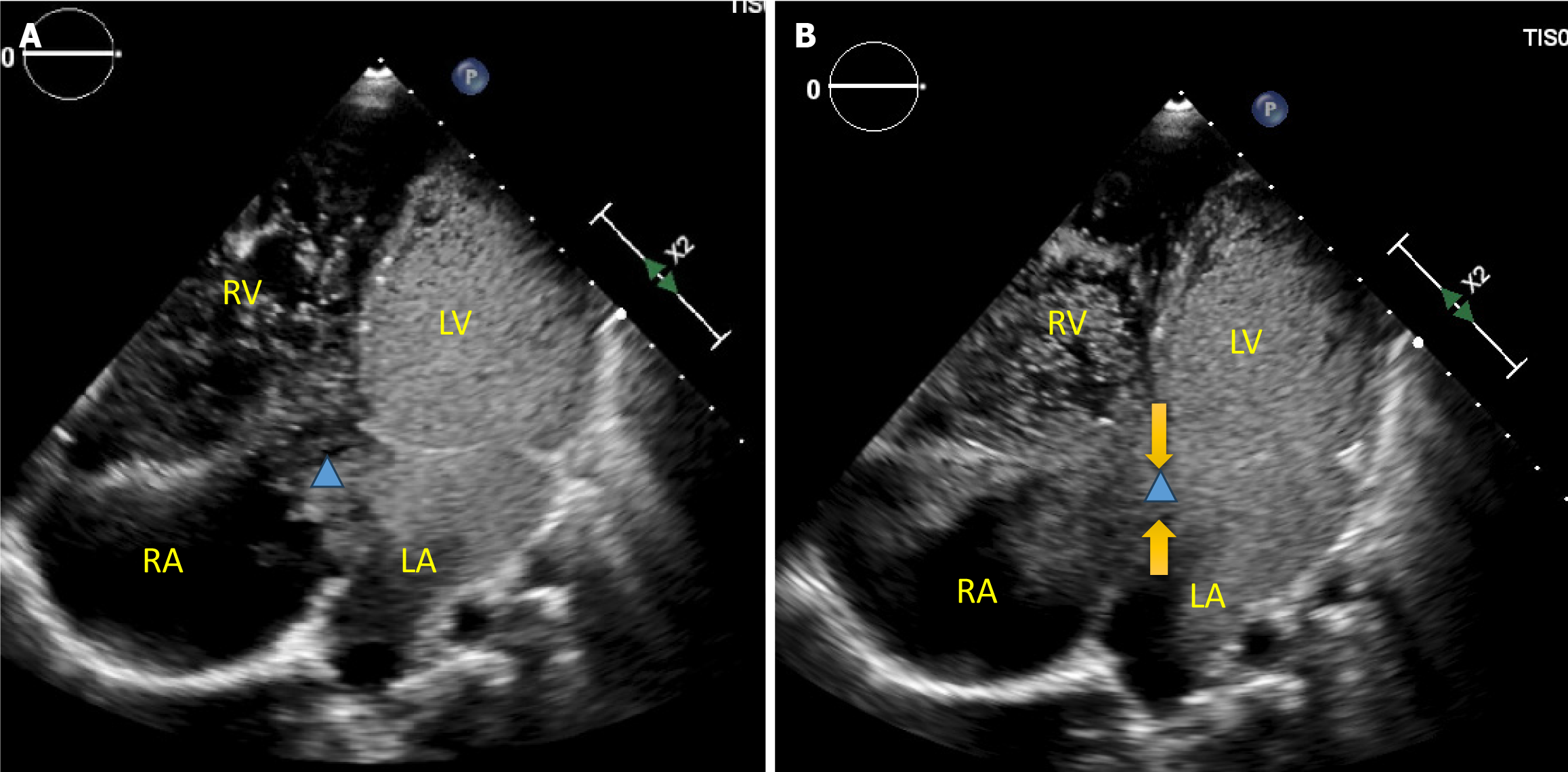
A chest x-ray was significant for an enlarged cardiac silhouette with prominent right atrium and increased vasculature suggestive of congestion. An echocardiogram (Figure 2) showed right atrium and ventricle dilation, with preserved right ventricular systolic function and absent RSVC. There was a right-sided brachiocephalic vein draining into a LSVC. Additionally, the ostium of the CS appeared significantly dilated with exuberant flow by color Doppler. The superior vena cava-CS continuity was interrupted consistent with UCS, while the LSVC was visualized to drain directly in the roof of the left atrium between the base of the left atrial appendage and the left upper pulmonary vein. Notably, the mitral valve leaflets were thickened, myxomatous and prolapsing resulting in multiple jets of severe mitral regurgitation. The mitral valve was bifoliate without a cleft, and the atrioventricular septum was intact without a primum atrial septal defect. Moderate tricuspid regurgitation was present and Doppler interrogation estimated the right ventricular systolic pressure to be around 30 mmHg. Contrast echocardiography, performed by injecting agitated saline through the antecubital vein of the left arm, showed sequential opacification of the LSVC, the left atrium, and the left ventricle. Concomitant with the opacification of the left ventricle, the right atrium and right ventricle opacified through the orifice of the CS (Figure 3). The inferior vena cava had a normal connection to the right atrium, and there was no evidence of a hemizygous connection. Pulmonary veins drained into the left atrium.
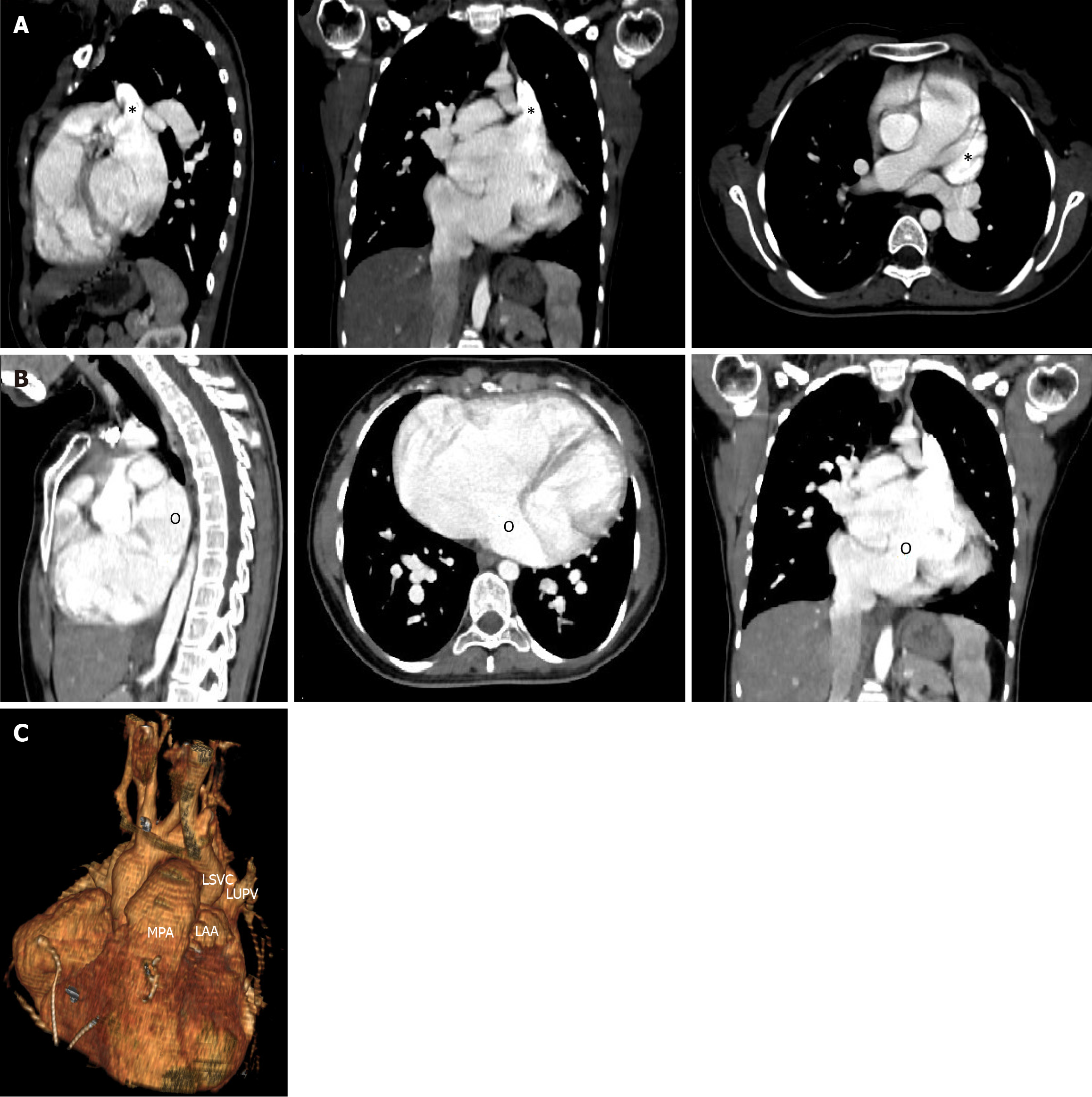
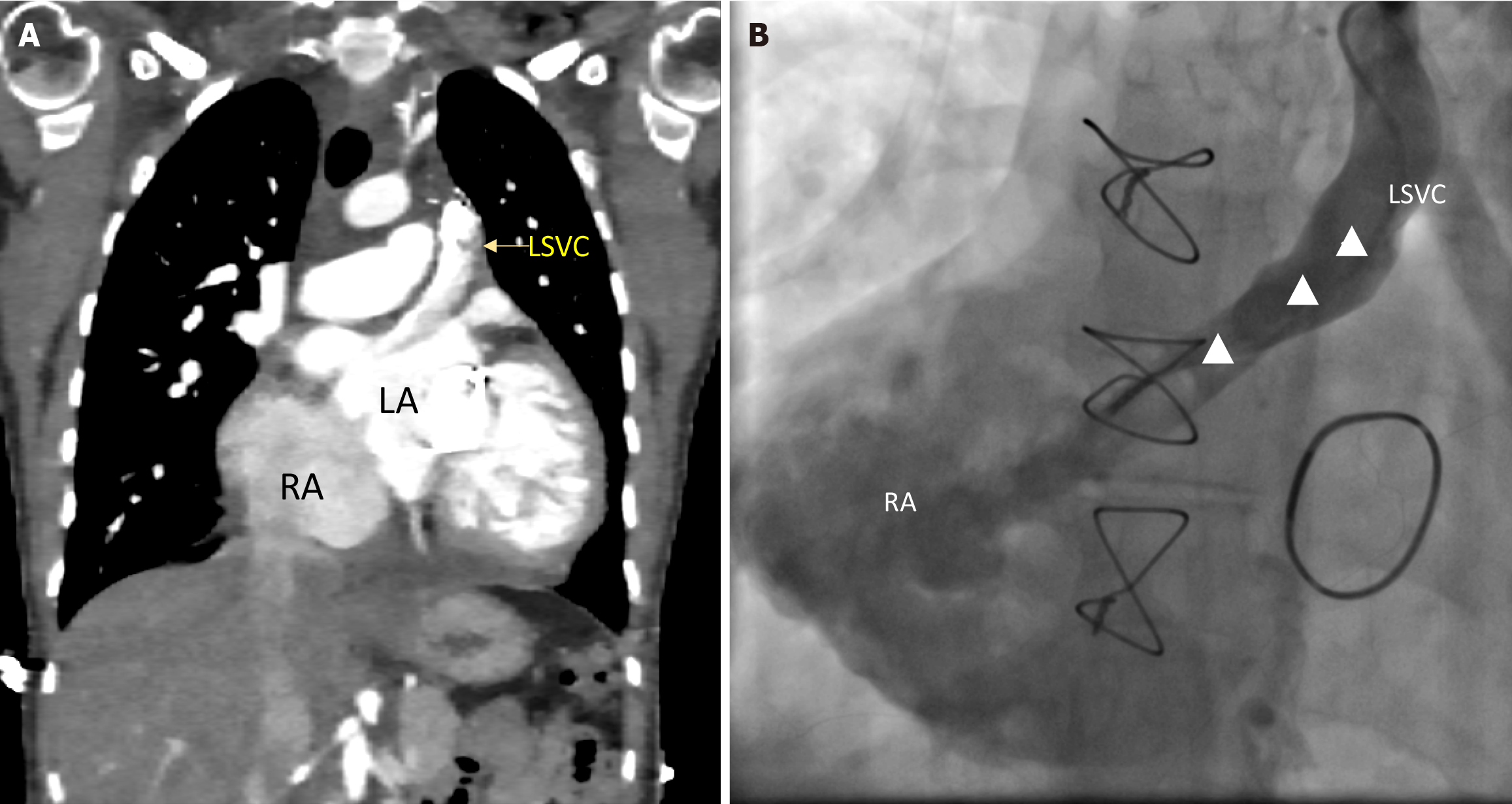
Subsequent computed tomography (CT) scan findings corroborated the echocardiographic diagnosis, confirming the presence of a single LSVC draining into the roof of the left atrium and complete unroofing of the CS. The ostium of the CS was dilated and served as the connection between the right atrium and the left atrium (Figure 4).
Workup confirmed the diagnosis of absent RSVC, persistent LSVC draining into the left atrium, and a completely UCS, in association with severe mitral insufficiency.
The patient underwent surgical intervention as follows:
After median sternotomy, cardiopulmonary bypass was established via bi-caval venous and aortic cannulation. Upon inspection, the RSVC was absent and a persistent LSCV was noted. Antegrade cardioplegia was used. The right and left atrium were opened. Inspection of the right atrial cavity revealed a dilated and significantly enlarged CS ostium. In
The repair of the LSVC to the left atrium was carried out using the repositioning of the atrial septum technique; a pericardial patch was sutured to the posterior rim of the LSVC using a continuous 5-0 polypropylene suture. The suture line was continued along the rim of the atrial septum and rim of the CS ostium where the caval orifice was positioned on the right side of this septum.
Examination of the mitral valve confirmed the absence of a cleft and the severe prolapse of the anterior and posterior leaflets. The mitral valve repair was performed using the 4-chord technique with annuloplasty as described by Chemtob et al[7].
Post-operatively, a repeat CT scan and a LSVC angiogram revealed a patent intra-atrial baffle without any significant residual shunt (Figure 5).
This report describes a unique case of absent RSVC in a visceroatrial situs solitus, persistent LSVC draining into the left atrium, and a completely UCS, in association with severe mitral insufficiency in the absence of atrioventricular septal defect (AVSD). UCS is a rare condition often associated with other congenital anomalies. It exhibits various types and classifications, such as the Kirklin and Barratt-Boyes classification which utilizes the extent of the unroofing and the presence or absence of the LSVC[8].
The combination of an UCS, absent RSVC and a persistent LSVC is extremely rare in patients without heterotaxia syndrome. The rare obliteration of the right anterior cardinal vein and persistence of the left one during embryological development results in the absent RSVC with persistent LSVC[9]; if occurred concomitantly with failure of the formation of the left atrio-venous fold results in UCS[2]. Specific genes implicated in the association between UCS and persistence of LSVC have not been yet identified. However, both defects are linked to abnormal development of the venous system during fetal life. These anomalies are also frequently associated with genetic syndromes such as Noonan syndrome and Holt-Oram syndrome suggesting a potential genetic contribution.
Our patient had visceral and atrial situs solitus as confirmed by the P wave morphology and axis on the ECG, the drainage of the supra-hepatic portion of the inferior vena cava by imaging and ultimately the usual disposition of the atrial appendages upon direct inspection by the surgeon.
Bertram et al[3] reported on 121 cases, with absent RSVC, and normal cardiac lateralization, UCS was found in only seven patients: One with a ventricular septal defect, another with tetralogy of Fallot, a third with double outlet right ventricle and the remaining four did not exhibit associated congenital heart disease[10]. Martinez and his group reported an additional 12 cases, none had an UCS[7]. Doksöz et al[11] reported a child with absent RSVC, persistent LSVC which drained to the UCS, in association with AVSD and cor-triatriatum sinister. Kumar and his group reported a patient with absent RSVC, persistent LSVC draining into the UCS, a common atrium and an AVSD[12]. Partial UCS syndrome with persistent LSVC, absent RSVC and right-sided pericardial defect was also described in a pediatric patient[13].
UCS is rarely associated with mitral valve diseases, with only sporadic reports of mitral insufficiency in adult patients or in association with AVSD, where the regurgitation is usually through a cleft[14-17]. Mitral stenosis was reported once in the literature[18]. Detailed information on those cases is reported in Table 1.
| Case number | Ref. | Associated cardiac disease |
| 1 | Brown et al[27] | None |
| 2 | Wood[28] | None |
| 3 | Sherafat et al[29] | None |
| 4 | Kabbani et al[30] | VSD |
| 5 | Choi et al[31] | DORV |
| 6 | Choi et al[31] | None |
| 7 | Pugliese et al[32] | TOF |
| 8 | Doksöz et al[11] | Cor triatriatum, AVSD |
| 9 | Kumar et al[12] | Common atrium, AVSD |
| 10 | Yilmaz et al[13] | Right sided pericardial defect |
| 11 | Bitar et al (current case) | Myxomatous MV |
In our patient, the presence of severe mitral insufficiency was associated with neither congenital heart disease, nor a cleft. Upon direct inspection, the mitral valve was free of a cleft, and the cause of the regurgitation was due to severe prolapse of both leaflets with elongated chords. Of interest, those changes could not have been attributed to age as is the case in adults with Barlow’s disease.
UCS is occasionally misdiagnosed as a primum atrial septal defect[3,19]. To differentiate atrial septal defect from a large and dilated CS, it is crucial to note that the former shows a defect in the atrial septum near the atrioventricular valve (AVV), with a cleft in the left AVV. However, a dilated CS, secondary to either a persistent LSVC or anomalous con
While transthoracic and contrast echocardiography are typically effective in the accurate diagnosis of UCS in most instances[19-24], the condition remains undetected preoperatively in approximately one-third of cases[19]. In our case the absence of the RSVC, the presence of LSVC and its draining site, the roof of the left atrium, the mitral valve pathology and degree of regurgitation as well as the unroofing of the CS were correctly identified by transthoracic and contrast echocardiography. We elected to perform a CT scan to further delineate the exact drainage of the LSVC in relationship to the left upper pulmonary vein and the base of the atrial appendage.
Although surgical repair has traditionally been the standard treatment, innovative percutaneous therapies are progressively emerging as alternatives[25,26]. In our case, the rarity of the condition, the lack of large series, and the absence of a RSVC limited the surgical options; as extra cardiac repair, be it ligation of the LSVC, in the case where a bridging vein is present, or rerouting using a conduit to the RSVC would not be feasible. Mitral valve prolapse and redundant leaflets resulting in severe mitral regurgitation associated with LSVC to UCS may present an additional challenging surgical scenario, as roofing the CS is a concern due to its proximity to the posterior mitral valve leaflet. This proximity could compromise the surgical repair or result in replacement of the mitral valve. In cases of concurrent mitral valve repair, safely diverting the LSVC to the right atrium without obstructing the mitral valve or the pulmonary veins and closure of the CS orifice becomes a crucial aspect of the surgical approach.
Preserving the CS drainage on the left side in the context of mitral valve surgery can offer certain advantages. This simplification potential can reduce overall complexity and operative time while also minimizing the risk of potential complications or obstructions that may arise during redirection. In cases involving mitral valve repair or replacement, opting to avoid roofing of the CS may prove to be a better choice; hence, intra-cardiac baffling without roofing the CS was deemed the procedure of choice in our patient. Post-operative imaging revealed a patent intra-atrial baffle without any significant residual shunt. However, long-term follow-up via echocardiography is definitely needed.
In conclusion, UCS is a complex condition which often requires careful consideration of associated anomalies and tailored surgical approaches, especially in cases involving severe mitral insufficiency, and single LSVC.
| 1. | Chen JL, Yu CG, Wang DJ, Chen HB. Misdiagnosis of unroofed coronary sinus syndrome as an ostium primum atrial septal defect by echocardiography: A case report. World J Clin Cases. 2022;10:1592-1597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 2. | Raghib G, Ruttenberg HD, Anderson RC, Amplatz K, Adams P JR, Edwards JE. Termination of left superior vena cava in left atrium, atrial septal defect, and absence of coronary sinus; a developmental complex. Circulation. 1965;31:906-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 192] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Bertram H, Paul T, Kaulitz R, Luhmer I, Kallfelz HC. [Coronary sinus defects: rare form of interatrial communication]. Z Kardiol. 1996;85:899-905. [PubMed] |
| 4. | Chaturvedi A, Dubinsky TJ, Maki JH. MR findings of a rare defect, coronary sinus ASD. Int J Cardiovasc Imaging. 2012;28:429-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Gajjar TP, Rao JN, Desai NB. Echocardiographic diagnosis and surgical closure of coronary sinus type of atrial septal defect. J Card Surg. 2011;26:653-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Martínez-Villar M, Gran F, Ferrer Q, Giralt G, Sabaté-Rotés A, Albert DC. Persistent Left Superior Vena Cava With Absent Right Superior Vena Cava. Rev Esp Cardiol (Engl Ed). 2016;69:220-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Chemtob RA, Mick S, Gillinov M, Hodges K, Wierup P. Repair of bileaflet prolapse in Barlow syndrome: The 4-chord technique. J Card Surg. 2019;34:605-609. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Kirklin J, Barratt-Boyes B. Cardiac Surgery. Morphology, Diagnostic Criteria, Natural History, Techniques. 1st ed. New Jersey: Willy, 1986. |
| 9. | Sheikh AS, Mazhar S. Persistent left superior vena cava with absent right superior vena cava: review of the literature and clinical implications. Echocardiography. 2014;31:674-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Bartram U, Van Praagh S, Levine JC, Hines M, Bensky AS, Van Praagh R. Absent right superior vena cava in visceroatrial situs solitus. Am J Cardiol. 1997;80:175-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 89] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Doksöz Ö, Güven B, Yozgat Y, Özdemir R, Meşe T, Tavlı V, Alayunt EA. Absent right superior vena cava with persistent left superior vena cava which drains to unroofed coronary sinus in a child with atrioventricular septal defect and cor triatriatum sinister: preop correct diagnosis and successful surgery in a single session. Congenit Heart Dis. 2014;9:E37-E40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Kumar V, Thingnam SKS, Soni R, Walia S, Kumar B. Absent right superior vena cava with left superior vena cava draining into unroofed coronary sinus with common atrium in a child with an atrioventricular septal defect. J Card Surg. 2020;35:1743-1745. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Yilmaz AT, Arslan M, Demirkiliç U, Kuralay E, Ozal E, Tatar H, Oztürk OY. Partially unroofed coronary sinus syndrome with persistent left superior vena cava, absent right superior vena cava and right-sided pericardial defect. Eur J Cardiothorac Surg. 1996;10:1027-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Sarwar G, Ahmed B, Suleman N, Khan G. Complicated unroofed coronary sinus syndrome. J Coll Physicians Surg Pak. 2005;15:171-173. [PubMed] |
| 15. | Konstantinides S, van Tournout FA, Bennett JM. Unroofed coronary sinus associated with atrial septal defect and significant mitral regurgitation. J Thorac Cardiovasc Surg. 1990;99:377-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Egoh Y, Isomatsu Y, Kurosawa H, Kawana M, Iwasaki T, Takahashi S. [A case of unroofed coronary sinus with mitral and tricuspid valve regurgitation]. Nihon Kyobu Geka Gakkai Zasshi. 1989;37:755-759. [PubMed] |
| 17. | Yamada K, Miyazaki S, Oboshi M, Suezawa C, Sakakibara Y, Nishimura K. Surgical repair of unroofed coronary sinus with severe mitral regurgitation in an elderly patient. J Cardiol Cases. 2019;19:29-32. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Awasthy N, Ambatkar P, Radhakrishnan S, Iyer KS. Lutembacher syndrome with unroofed left superior vena cava: a diagnostic dilemma. Pediatr Cardiol. 2013;34:1985-1988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Shi H, Yan J, Wang Q, Hua Z, Li S, Zhang J. Surgical management of unroofed coronary sinus syndrome: A 20-year-single-center experience. J Card Surg. 2021;36:589-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Xie MX, Yang YL, Cheng TO, Wang XF, Li K, Ren PP, Lü Q, Lin H, Li L. Coronary sinus septal defect (unroofed coronary sinus): echocardiographic diagnosis and surgical treatment. Int J Cardiol. 2013;168:1258-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Ozturk S, Durmus G, Kalyoncuoglu M, Sari M, Ozbek O, Can M. Unroofed Coronary Sinus Atrial Septal Defect Misdiagnosed as Ostium Primum Defect. Korean Circ J. 2018;48:89-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 22. | Al-Dairy A, Ahmad R, Hasan R. Misdiagnosis of persistent left superior vena cava with unroofed coronary sinus as a coronary sinus-type atrial septal defect. Clin Case Rep. 2023;11:e7826. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Ma J, Zheng Y, Xu S, Teng H, Lv L, Li Y, Liang Y, Zhang Y. The value of cardiac CT in the diagnosis of unroofed coronary sinus syndrome. BMC Cardiovasc Disord. 2022;22:516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Sun T, Fei HW, Huang HL, Chen OD, Zheng ZC, Zhang CJ, Hou YS. Transesophageal echocardiography for coronary sinus imaging in partially unroofed coronary sinus. Echocardiography. 2014;31:74-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Mohammad Nijres B, Kenny D, Kazmouz S, Hijazi ZM. Transcatheter closure of unroofed coronary sinus using covered stents in an adult with drainage of the coronary sinus to the right ventricle after supra-annular tricuspid valve replacement. Catheter Cardiovasc Interv. 2017;90:1154-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Wang C, Ma L, Li YJ, Pan X. Percutaneous repair of unroofed coronary sinus with an atrial septal occluder. Eur Heart J Case Rep. 2023;7:ytad032. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 27. | Brown JF, Crumpton CW, Huston JH, Rowe GG, Tuchman H, Weinstein AB. Superior vena cava draining into left atrium; another cause for left ventricular hypertrophy with cyanotic congenital heart disease. Am J Med. 1956;21:481-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Wood P. Anomalous drainage of the SVC or IVC into the left atrium. In: Wood P. Diseases of the Heart and Circulation. 2nd ed, London: Eyre & Spottiswoode, 1957; 457. |
| 29. | Sherafat M, Friedman S, Waldhausen JA. Persistent left superior vena cava draining into the left atrium with absent right superior vena cava. Ann Thorac Surg. 1971;11:160-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Kabbani SS, Feldman M, Angelini P, Leachman RD, Cooley DA. Single (left) superior vena cava draining into the left atrium. Surgical repair. Ann Thorac Surg. 1973;16:518-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Choi JY, Anderson RH, Macartney FJ. Absent right superior caval vein (vena cava) with normal atrial arrangement. Br Heart J. 1987;57:474-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Pugliese P, Murzi B, Aliboni M, Eufrate S. Absent right superior vena cava and persistent left superior vena cava. Clinical and surgical considerations. J Cardiovasc Surg (Torino). 1984;25:134-137. [PubMed] |