Published online Sep 26, 2023. doi: 10.4330/wjc.v15.i9.462
Peer-review started: March 15, 2023
First decision: June 14, 2023
Revised: June 29, 2023
Accepted: August 17, 2023
Article in press: August 17, 2023
Published online: September 26, 2023
Processing time: 189 Days and 16.2 Hours
Wellen’s syndrome is a form of acute coronary syndrome associated with proximal left anterior descending artery (LAD) stenosis and characteristic electrocardiograph (ECG) patterns in pain free state. The abnormal ECG pattern is classified into type A (biphasic T waves) and type B (deeply inverted T waves), based on the T wave pattern seen in the pericodial chest leads.
We present the case of a 37-year-old male with history of type 1 diabetes mellitus (T1DM), gastroparesis, mild peripheral artery disease and right toe cellulitis on IV antibiotics who presented to the emergency department with nausea, vomiting and abdominal pain for 3 d and as a result couldn’t take his insulin. Noted to have fasting blood sugar 392 mg/dL. Admitted for diabetic gastroparesis. During the hospital course, the patient was asymptomatic and denied any chest pain. On admission, No ECG and troponin draws were performed. On day 2, the patient became hypoxic with oxygen saturation 80% on room air, intermittent mild right-sided chest pain which he attributed to vomiting from his gastroparesis. Initial ECG done was significant for Biphasic T wave changes in leads V2 and V3 and elevated high sensitivity troponin. Patient was transitioned to cardiac intensive care unit and cardiac catheterization performed with result significant for extensive coronary artery disease.
This case highlights an exceptional manifestation of Wellen's syndrome, wherein the right coronary artery and circumflex artery display a remarkable 100% constriction, alongside a proximal LAD stenosis of 90%-95%. Notably, this occurrence transpired in a patient grappling with extensive complications arising from T1DM. Moreover, it underscores the utmost significance of promptly recognizing the presence of Wellen's syndrome and swiftly initiating appropriate medical intervention.
Core Tip: When a patient exhibits atypical symptoms preceding chest pain and displays distinct T wave abnormalities on the electrocardiogram, it is crucial to seek immediate cardiology intervention. This entails conducting emergent cardiac catheterization to evaluate the presence of proximal stenosis in the left anterior descending artery, or in rare instances, the right coronary artery and left circumflex artery. Such stenosis can lead to the development of ischemic cardiomyopathy if left untreated. Acting promptly and carefully monitoring the characteristic T wave patterns, alongside normal or minimally elevated cardiac biomarkers, contributes to improved mortality prognosis.
- Citation: Obi MF, Sharma M, Namireddy V, Gargiulo P, Noel C, Hyun C, Gale BD. Variant of Wellen’s syndrome in type 1 diabetic patient: A case report. World J Cardiol 2023; 15(9): 462-468
- URL: https://www.wjgnet.com/1949-8462/full/v15/i9/462.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i9.462
Wellen's syndrome is a distinctive condition characterized by distinct alterations in the ST-T waves in the precordial leads, indicating an obstruction in the proximal left anterior descending coronary artery[1]. This syndrome has been observed in individuals experiencing unstable angina, as well as those with atypical presentations devoid of acute chest pain. If left untreated, Wellen's syndrome can cause myocardial infarction and necrosis in the anterior wall of the heart. The hallmark features of Wellen's syndrome are biphasic T waves (type A in 25% of cases) or deeply inverted T waves (type B in 75% of cases) in V2-V3, which can extend to V1-V6 and often involve the proximal anterior left anterior descending artery (LAD). Nevertheless, research has demonstrated that this syndrome is not confined solely to the proximal anterior LAD, as similar changes have been reported in the right coronary artery (RCA) and circumflex artery[2]. The correlation between T wave changes in precordial leads and the heightened risk of developing anterior wall myocardial infarction, despite medical intervention, was first elucidated by de Zwaan et al[3] in 1982. The diagnostic criteria for Wellen's syndrome encompass a history of angina, deeply inverted or biphasic T waves in the precordial leads, normal or slightly elevated serum cardiac enzymes, absence of precordial Q waves, minimal or isoelectric ST segment elevation (less than 1 mm), and the presence of the specific electrocardiograph (ECG) pattern during pain-free states[4]. Risk factors associated with Wellen's syndrome include diabetes mellitus, arterial hypertension, metabolic syndrome, hypercholesterolemia, smoking, and a family history of premature heart disease, all of which are present in our patient. This case report, accompanied by a review of the existing literature, emphasizes the critical importance of early recognition of Wellen's syndrome, not only in relation to the proximal LAD, but also its involvement in both the RCA and circumflex artery.
A 37-year-old man with chief complaint of nausea, vomiting, abdominal pain for 3-day duration associated with diarrhea.
The patient arrived at the emergency department with complaints of abdominal pain, characterized as burning, non-radiating and constant, 7/10 in severity, which he attributed to his gastroparesis as he has had multiple admissions with gastroparesis flares. Patient has a past medical history of type 1 diabetes, diabetic gastroparesis, major depression, anxiety, smoking (1 pack per week), 1 g of marijuana consumption and right 4th toe cellulitis recently treated with IV antibiotics. Admits to intermittent depressive episode; during which he stops taking his medication including insulin but denied suicidal ideation and intent.
Diabetic gastroparesis, type 1 diabetes mellitus, peripheral artery disease, and right toe cellulitis on antibiotics.
A noteworthy familial background of cardiovascular disease is documented, encompassing the father, parental uncle, and grandfather, each of whom underwent double bypass surgeries. The father's bypass operation was performed at the relatively young age of 40.
In the physical exam the abdomen was non-distended, tenderness on palpation of the 4 quadrants, positive bowel sounds, no organomegaly appreciated. The blood pressure on admission was 129/99 with heart rate of 124 bpm. Chest symmetry with respiration, no crackles or wheezing noted and normal vesicular breath sounds. Normal S1, S2 and no pathological murmur heard. The patient was euvolemic, and no bilateral lower extremity edema was noted.
Urine toxicology is positive for marijuana. Given the atypical presentation, high sensitivity troponin was not ordered. Uncontrolled diabetes, Hyperlipidemia and hypoxia noted (Table 1).
| Hematology | Values | Chemistry | Values |
| WBC | 17.00 | High sensitivity troponin | 12072.1 |
| Hemoglobin | 13.7 | LDH | 472 |
| Hematocrit | 40.3 | TSH | 0.810 |
| MCV | 95.1 | T4 | 1.27 |
| MCH | 32.3 | Hemoglobin A1C | 10.9 |
| RDW | 12.1 | Sodium | 138 |
| Platelet count | 256 | Potassium | 4.1 |
| Neutrophil | 79.4 | Chloride | 105 |
| Lymphocytes | 13.3 | CO2 level | 23 |
| Monocytes | 7.0 | Blood urea nitrogen | 21 |
| EOS count | 0.1 | Creatinine | 1.05 |
| Basophils | 0.2 | GRF estimation | > 60 |
| Nucleated RBC | 0 | LDL | 127 |
| RBC | 4.2 | HDL | 44 |
| Procalcitonin | 0.07 | Total cholesterol | 184 |
| Calcium | |||
| Arterial blood gas | |||
| pH | 7.40 | ||
| pCO2 | 46 | ||
| O2 | 64 | ||
| HCO3 | 28.5 |
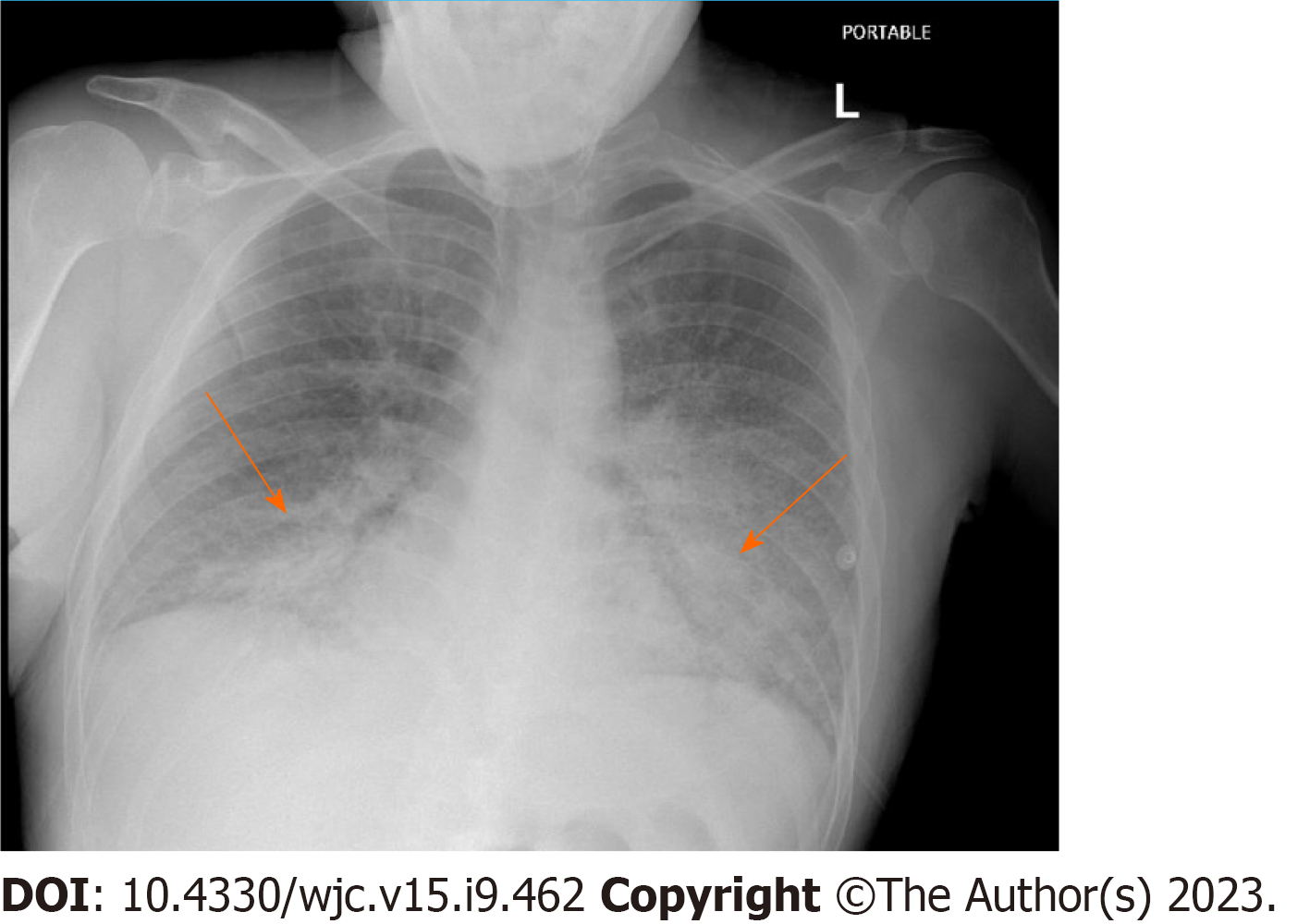
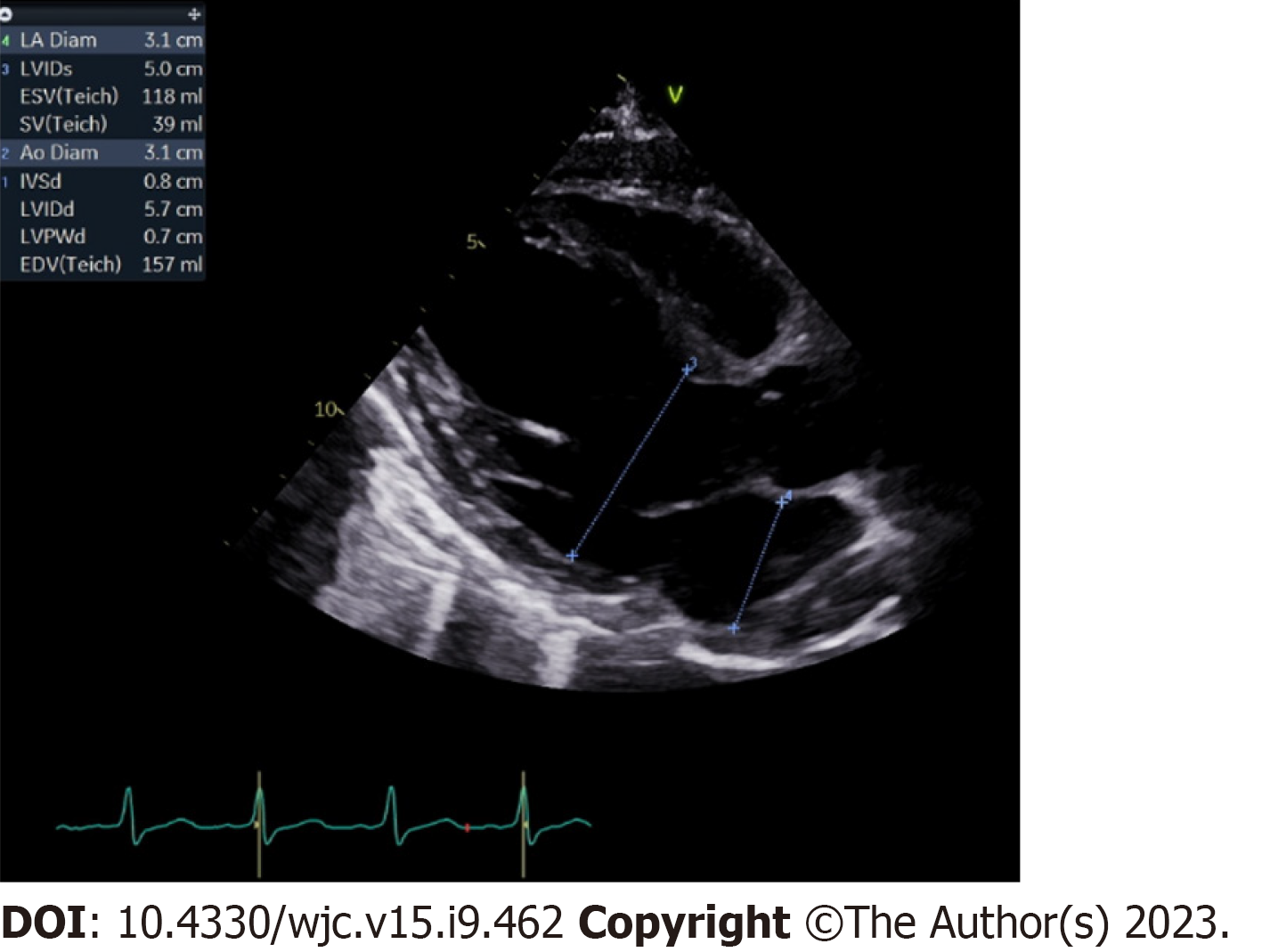
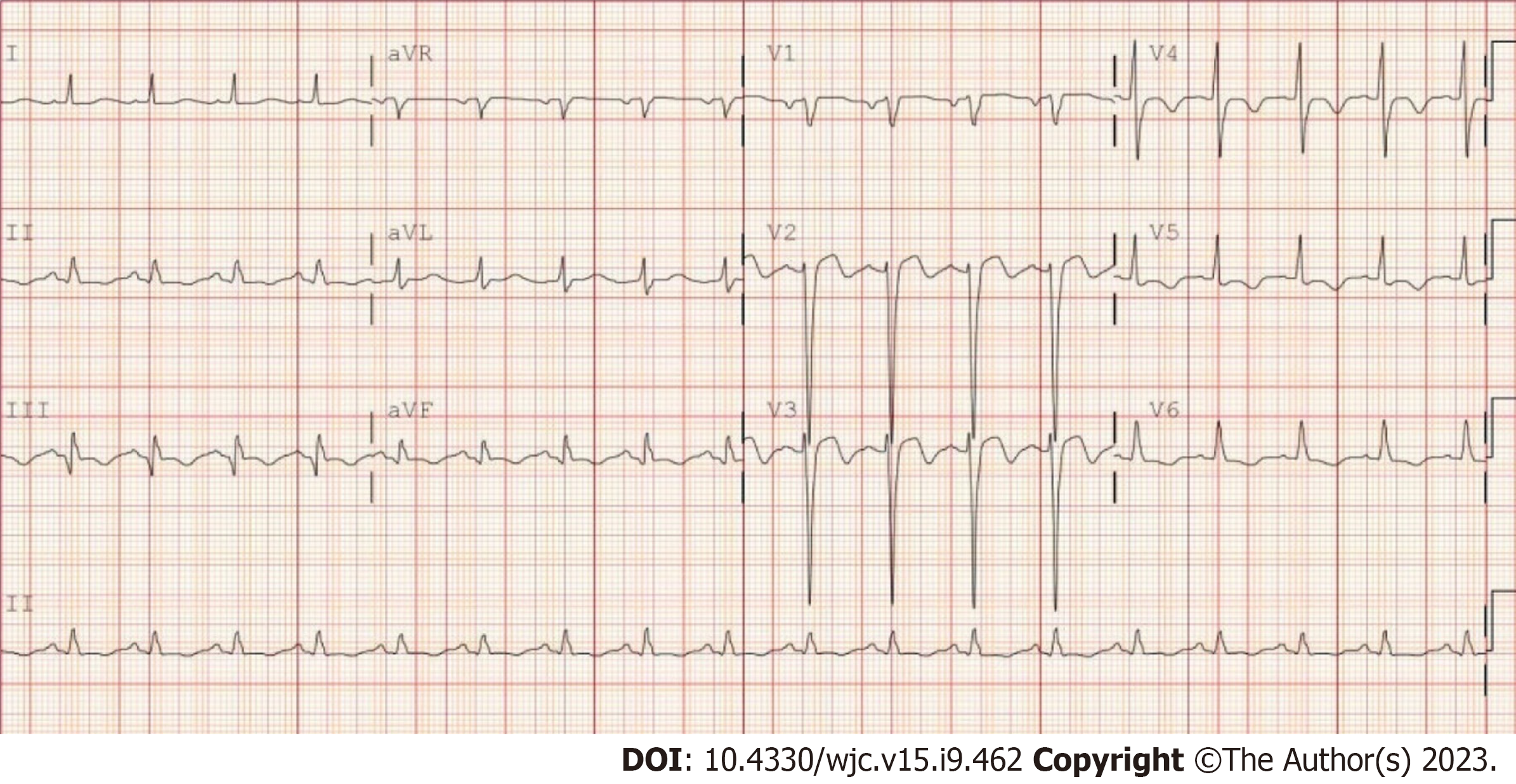
Patient was admitted for diabetic gastroparesis, bedside point of care ultrasound; was significant for inferior vena cava (IVC) dilation and Kerley B lines. A chest X ray was ordered, which shows acute pulmonary edema (Figure 1). Given acute and sudden onset of hypoxia, echocardiogram (ECHO) was ordered (Figure 2), after notable elevation in cardiac enzyme (elevated high sensitivity troponin). The first electrocardiogram (EKG) was then ordered (Figure 3).
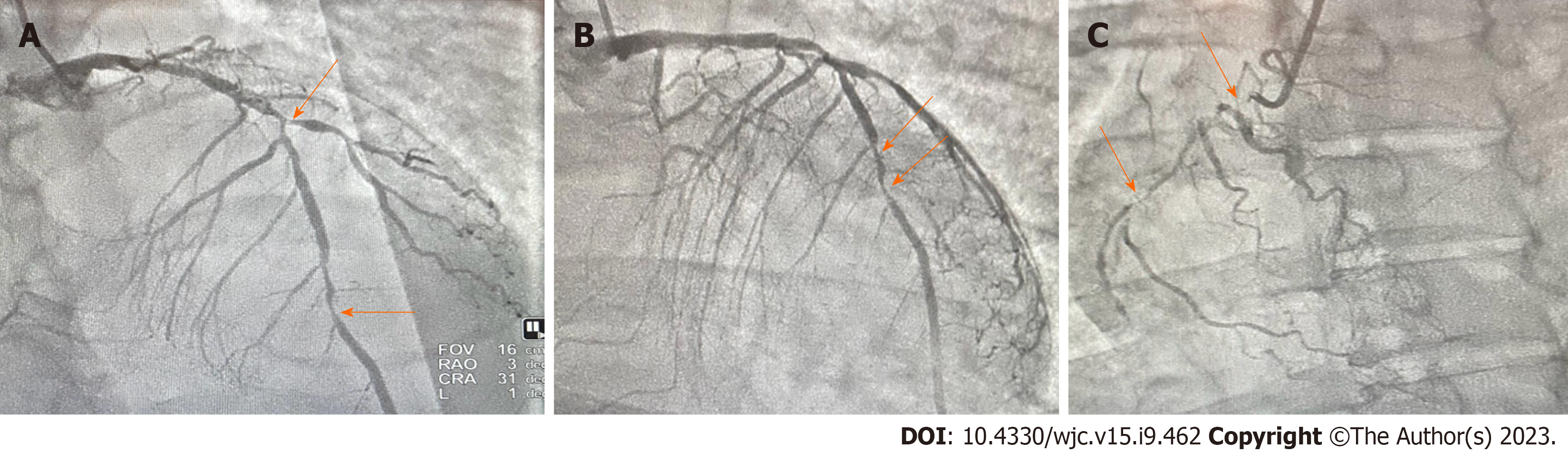
The patient underwent a treatment regimen that involved the administration of 3 L of normal saline, along with medications such as Benadryl, famotidine, Zofran, and IV fluids at a rate of 125 mL/h. Additionally, the patient received Reglan 10 mg every 8 h and pantoprazole. On the second day at 6:00 pm, the patient experienced a drop in oxygen saturation, reaching the mid-80s while breathing room air. To address this, the patient was placed on a venti-mask at 50% oxygen concentration. During the examination, the patient acknowledged experiencing mild and intermittent right-sided chest pain, attributing it to vomiting and noting a history of similar pain during gastroparesis flares over the past 5 years. The patient denied any previous history of heart disease. A point-of-care ultrasound at the bedside revealed notable dilation of the IVC and the presence of Kerley B lines. Chest X-ray was ordered, which confirmed the diagnosis of acute pulmonary edema (Figure 1). Given the sudden onset of hypoxia, further investigations were initiated, including laboratory tests and an EKG (Figure 2). The patient received a 40 mg dose of furosemide and was subsequently continued on furosemide 40 mg every 12 h. To alleviate anxiety, the patient was given a STAT dose of alprazolam 0.25 mg orally. Following these measures, an initial EKG was ordered, along with a high sensitivity troponin test (Figure 3). Later that day, a cardiology consultation was sought, and an ECHO was performed. The ECHO revealed a moderately dilated left ventricle with a severely reduced ejection fraction of less than 20%. The left atrium was also found to be moderately dilated (Figure 2). The cardiologist was informed about the clinical findings and the elevated troponin levels. As a result, the acute coronary syndrome (ACS) protocol was initiated. The patient received a heparin drip following a loading dose of aspirin 81mg and a statin 80 mg, both given immediately. The patient was transferred to the cardiac center for coronary angiographic catheterization and right heart catheterization. The results of these procedures indicated the presence of extensive disease in the LAD, with stenosis extending to both the RCA and circumflex artery (Figure 4).
Conclusion of the cardiac coronary angiogram report indicated the following: Dominance: Right dominant; left main: Mild luminal irregularities less than 30%; left another decending artery: Min lad: 90% stenosis; distal lad: 95% stenosis; diagonal 1: 90% stenosis; circumflex artery: Ostial circ: 100 % stenosis; and RCA: Prox rca: 100% stenosis.
Following the placement of an intra-aortic balloon pump in the cardiac laboratory center, the patient was promptly transferred to the intensive care unit. In this setting, the patient's treatment regimen included the immediate initiation of aspirin 81 mg, ticagrelor 180 mg given STAT, followed by 90 mg every 12 h. Additionally, a nitroglycerin drip and 80 mg of atorvastatin were administered. The cardiologist recommended transferring the patient to a tertiary center for urgent coronary artery bypass graft (CABG) surgery given significant coronary artery lesions. On January 23, 2023, the patient underwent quadruple CABG, and a subsequent bedside ECHO revealed no evidence of pericardial effusion. Upon improvement, the patient was discharged with a medication regimen consisting of spironolactone 25 mg, metoprolol succinate 25 mg, aspirin 81 mg, atorvastatin 80 mg, valsartan 40 mg, and dapagliflozin 5 mg once a day.
Follow up in Cardiology clinic 1 wk post discharge from the tertiary center after contrary bypass graft. Notable significant improvement of symptoms with improved functional capacity and activities of daily living.
Wellen’s syndrome was first described in 1982 by de Zwaan et al[3] as proximal LAD T- wave syndrome in the process of evaluating subgroup of patients with unstable angina during a stable and pain-free period[5]. Our patient presents with no chest pain, but abdominal pain, which he attributed to his recurrent gastroparesis. Wellen’s syndrome was then discovered to be associated with significant critical occlusion of the LAD with a characteristic presentation distinctive to abnormal T wave changes in precordial leads in patients with suspected ACS. The electrocardiographic manifestation of Wellen’s syndrome is characterized by 2 patterns; pattern A has biphasic T waves in V2-V3 (25%), and pattern B has symmetric and deeply inverted T waves in precordial chest leads (75%)[5,6]. In this case report, the patient presented on EKG with biphasic T wave in V2-V3 (Figure 2). These T wave changes signifies severe myocardial dysfunction or ischemia, although patients have been known to exhibit this syndrome during a pain free period at the time EKG is taken and have normal or minimally elevated cardiac enzymes, the prognosis of its event represents high risk of extensive anterior wall myocardial infarction within time of presentation[7]. Wellen’s syndrome can also be a pre-coronary infarction stage that can lead to detrimental ACS. The concept of occlusion and reperfusion in the EKG sequence of Wellen’s syndrome likely involves sudden complete occlusion of the LAD causing transient anterior ST segment elevation myocardia injury, leading to chest pain and diaphoresis stage not captured on EKG. Second stage then involves re-perfusion of the LAD likely secondary to spontaneous clot lysis leading to resolution of the chest pain with improvement in ST elevation and the appearance of biphasic or inverted T wave morphology[8]. Although Wellen’s syndrome is known to involve mostly the LAD the syndrome is not limited to the anterior leads. The precordial T wave changes can be seen in the inferior or lateral leads with RCA or circumflex artery occlusion as noted in many studies and events in our case presentation. Diagnostic criteria of Wellen’s syndrome includes[9]: Isoelectric or minimally elevated (< 1 mm) ST segment elevation; no precordial Q waves; deeply inverted or biphasic T waves in V2-V3 but may extend to V1-6; ECG pattern present in pain free state; preserved precordial R wave progression; recent history of angina; and normal or elevated serum cardiac markers.
Wellen’s syndrome is often not an acute process as it can develop over days or weeks especially seen in people with risk factors (smoking, hypertension, diabetes and metabolic syndrome etc.). Although the syndrome is a temporary obstruction of the culprit coronary artery (pre-infarction state), LAD or artery involved can re-occlude at any time and the first EKG seen is normalization of the T wave called pseudo-normalization after which the T wave becomes upright and prominent; thus sign of hyper acute ST-elevation myocardial infarction during which the patient complains of chest pain that is associated with other symptoms of ACS[10]. Sometimes Wellen’s syndrome can manifest in normal coronaries following an episode of vasospasm seen in cases of cocaine abuse, however, it is still appropriate to rule out thrombus formation or coronary thrombosis with angiogram during presentation given the syndromes risk of leading to sever and extensive anterior wall myocardial infarction and possible death. The phenomenon of re-occulsion and re-perfusion was likely experienced by our patient, however given the history of uncontrolled diabetes with complications, his pre
It is well known fact that uncontrolled diabetes can lead to cardiovascular disease. Its pathophysiology is linked to hyperglycemic state leading to an increase in oxidative stress, which results in micro and macrovascular complications. Persistent elevation in blood sugar can cause an overproduction of superoxide by the mitochondrial electron transport chain leading to complications seen in diabetic patients. The activation of superoxide overproduction pathway leads to increase generation of nitric oxide due to uncoupled state of endothelial nitric oxide synthase (NOS) and inducible NOS. All which leads to deoxyribonucleic acid (DNA) damage due to the formation of the strong oxidant peroxynitrite[11]. DNA damage causes rapid activation of poly (adenosine diphosphate-ribose) polymerase, depleting the intracellular concentration of its substrate nicotinamide adenine dinucleotide, and slowing the rate of glycolysis, electron transport, and adenosine-triphosphate formation and thus causing acute endothelial dysfunction[12]. Hyperglycemic state is an inflammatory state as it induces surge of inflammatory cytokines (such as C reactive protein, interleukin interleukin (IL)-6, IL-8 tumor necrosis factor-α, and endothelin-1and as result contribute to plaque instability. Accumulation of these inflammatory cytokines leads to endothelial injury and hypercoagulability increasing the risk for cardiovascular event. In clotting cascade, the quantity of clotting factors, including glycation and oxidation is affected during hyperglycemic state increasing the risk of thrombosis[13]. Patients with type 1 diabetes are on insulin regimen for glycemic control. Hyperinsulinemia can lead to an increase in hepatic synthesis on prothrombic factors leading to thrombotic state.
Cardiac autonomic neuropathy (CAN) is the most common complication seen in type I diabetic patients. Poor glycemic control is the risk factor of CAN with prevalence approximately 20%, increases with age and a known predictor of cardiovascular morbidity and mortality in type 1 diabetes[14]. Type 1 diabetes is thought to be caused by an autoimmune reaction that destroys the beta cells of the pancreas. The same immunological factors are seen affecting the sympathetic ganglia leading to cardiac sympathetic dysfunction[15]. All these pathologies can also be seen in patients with type 2 diabetes. In correlation to our patient, who presented with uncontrolled and complicated diabetes as such has increased risk of CAN and arthrosclerosis. Our patient presented with Wellen’s syndrome, but the diagnosis was late given that patient delayed medical evaluation for cardiac disease, as he believed that all his symptoms of intermittent chest discomfort were due to prolonged vomiting and gastroparesis flares.
Wellen's syndrome emphasizes the need for serial EKGs in patients with cardiovascular risk factors, as critical stenosis may be detected and require invasive interventions. This case report highlights the extensive nature of Wellen's syndrome, involving occlusion in the LAD, RCA, and circumflex arteries. It demonstrates that Wellen's syndrome extends beyond proximal LAD disease and presents distinct EKG changes. Clinicians face diagnostic challenges due to atypical presentations, delaying ACS identification. Thus, it is vital for clinicians to identify Wellen's syndrome on EKGs and evaluate high-risk patients regardless of atypical symptoms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yu F, China S-Editor: Lin C L-Editor: A P-Editor: Xu ZH
| 1. | Ajibawo T, Andreev A, Sahni S. Wellens' Syndrome Presenting as Epigastric Pain and Syncope: An Unusual Presentation. Cureus. 2020;12:e6877. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Schnell O, Cappuccio F, Genovese S, Standl E, Valensi P, Ceriello A. Type 1 diabetes and cardiovascular disease. Cardiovasc Diabetol. 2013;12:156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103:730-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 319] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Miner B, Grigg WS, Hart EH. Wellens Syndrome. 2023 Jul 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 5. | Kyaw K, Latt H, Aung SSM, Tun NM, Phoo WY, Yin HH. Atypical Presentation of Acute Coronary Syndrome and Importance of Wellens' Syndrome. Am J Case Rep. 2018;19:199-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Al-Assaf O, Abdulghani M, Musa A, AlJallaf M. Wellen's Syndrome: The Life-Threatening Diagnosis. Circulation. 2019;140:1851-1852. [PubMed] [DOI] [Full Text] |
| 7. | Smith SW. Announcing Smith's ECG Blog. 2023 Mar 19 [cited 30 July 2023]. In: Smith's ECG Blog [Internet]. Available from https://hqmeded-ecg.blogspot.com/2023/05/a-30-something-woman-with-heart-score.html. |
| 8. | Alexander J, Rizzolo D. Wellens syndrome: An important consideration in patients with chest pain. JAAPA. 2023;36:25-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 9. | Ceriello A. Postprandial hyperglycemia and diabetes complications: is it time to treat? Diabetes. 2005;54:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 674] [Cited by in RCA: 671] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 10. | Desouza CV, Bolli GB, Fonseca V. Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care. 2010;33:1389-1394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 335] [Cited by in RCA: 299] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 11. | Suryawan IGR, Bakhriansyah J, Puspitasari M, Gandi P, Intan RE, Alkaff FF. To reperfuse or not to reperfuse: a case report of Wellens' syndrome with suspected COVID-19 infection. Egypt Heart J. 2020;72:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Avram A, Chioncel V, Guberna S, Cuciureanu I, Brezeanu RC, Andrei CL, Sinescu C. Myocardial bridging-an unusual cause of Wellens syndrome: A case report. Medicine (Baltimore). 2020;99:e22491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Torelli E, Sardeo F, Nuzzo E, Cicchinelli S, Petrucci M, Pignataro G, Covino M, Franceschi F, Candelli M. Wellens Syndrome without chest pain, is it possible? Eur Rev Med Pharmacol Sci. 2020;24:7718-7721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Mufti M, Joea R, Sobnosky S, Longtine J. Wellens’ Syndrome: An Atypical Presentation of an Already Silent Killer. J Med Cases. 2018;9:173-176. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Mathew R, Zhang Y, Izzo C, Reddy P. Wellens' Syndrome: A Sign of Impending Myocardial Infarction. Cureus. 2022;14:e26084. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |