Published online Jul 26, 2023. doi: 10.4330/wjc.v15.i7.342
Peer-review started: March 25, 2023
First decision: June 1, 2023
Revised: June 14, 2023
Accepted: July 3, 2023
Article in press: July 3, 2023
Published online: July 26, 2023
Processing time: 121 Days and 16.6 Hours
Effective management of major cardiovascular risk factors is of great importance to reduce mortality from cardiovascular disease (CVD). The Survey of Risk Factors in Coronary Heart Disease (SURF CHD) II study is a clinical audit of the recording and management of CHD risk factors. It was developed in collaboration with the European Association of Preventive Cardiology and the European Society of Cardiology (ESC). Previous studies have shown that control of major cardiovascular risk factors in patients with established atherosclerotic CVD is generally inadequate. Azerbaijan is a country in the South Caucasus, a region at a very high risk for CVD.
To assess adherence to ESC recommendations for secondary prevention of CVD based on the measurement of both modifiable major risk factors and their therapeutic management in patients with confirmed CHD at different hospitals in Baku (Azerbaijan).
Six tertiary health care centers participated in the SURF CHD II study between 2019 and 2021. Information on demographics, risk factors, physical and laboratory data, and medications was collected using a standard questionnaire in consecutive patients aged ≥ 18 years with established CHD during outpatient visits. Data from 687 patients (mean age 59.6 ± 9.58 years; 24.9% female) were included in the study.
Only 15.1% of participants were involved in cardiac rehabilitation programs. The rate of uncontrolled risk factors was high: Systolic blood pressure (BP) (SBP) (54.6%), low-density lipoprotein cholesterol (LDL-C) (86.8%), diabetes mellitus (DM) (60.6%), as well as overweight (66.6%) and obesity (25%). In addition, significant differences in the prevalence and control of some risk factors [smoking, body mass index (BMI), waist circumference, blood glucose (BG), and SBP] between female and male participants were found. The cardiovascular health index score (CHIS) was calculated from the six risk factors: Non- or ex-smoker, BMI < 25 kg/m2, moderate/vigorous physical activity, controlled BP (< 140/90 mmHg; 140/80 mmHg for patients with DM), controlled LDL-C (< 70 mg/dL), and controlled BG (glycohemoglobin < 7% or BG < 126 mg/dL). Good, intermediate, and poor categories of CHIS were identified in 6%, 58.3%, and 35.7% of patients, respectively (without statistical differences between female and male patients).
Implementation of the current ESC recommendations for CHD secondary prevention and, in particular, the control rate of BP, are insufficient. Given the fact that patients with different comorbid pathologies are at a very high risk, this is of great importance in the management of such patients. This should be taken into account by healthcare organizers when planning secondary prevention activities and public health protection measures, especially in the regions at a high risk for CVD. A wide range of educational products based on the Clinical Practice Guidelines should be used to improve the adherence of healthcare professionals and patients to the management of CVD risk factors.
Core Tip: The article stresses the value of audit studies in clinical practice. It confirms that the control rate of major cardiovascular risk factors is insufficient and stresses the importance of an individual approach to the secondary prevention of atherosclerotic coronary heart disease, considering patients' gender, comorbidities, cultural peculiarities, and the region of their residence.
- Citation: Gabulova R, Marzà-Florensa A, Rahimov U, Isayeva M, Alasgarli S, Musayeva A, Gahramanova S, Ibrahimov F, Aliyev F, Imanov G, Rasulova R, Vaartjes I, Klipstein-Grobusch K, Graham I, Grobbee DE. Risk factors in cardiovascular patients: Challenges and opportunities to improve secondary prevention. World J Cardiol 2023; 15(7): 342-353
- URL: https://www.wjgnet.com/1949-8462/full/v15/i7/342.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i7.342
Atherosclerotic cardiovascular disease (CVD) (ASCVD) remains the leading cause of morbidity and mortality worldwide. According to recent data, the incidence and mortality rates of CVDs have declined in high-income countries, and the majority of global deaths from CVD occur in low- and middle-income countries[1].
The World Health Organization's ‘Global Plan of Action for Noncommunicable Diseases (NCDs) Prevention and Control 2013-2020’ aims to reduce mortality from these causes by a quarter by 2025[2]. Two of the nine global targets focus directly on CVD prevention and control. The recently published European Society of Cardiology (ESC) guidelines on CVD prevention are designed to help health professionals identify the best strategies for managing modifiable risk factors in patients with established ASCVD[3].
Effective control of CVD risk factors plays a critical role in reducing mortality from CVDs. International registry studies provide valuable information on the current status of the problem, identify deficits, and contribute to improving the quality of care and clinical outcomes in different countries.
The Survey of Risk Factors in Coronary Heart Disease (SURF CHD) II study is a clinical audit of the recording and management of CHD risk factors, developed in collaboration with the European Association of Preventive Cardiology and the ESC. It was conducted in countries representing Europe, Asia, and Middle East and more recently North Africa, and South America to assess the recording and monitoring of cardiovascular risk factors in patients with established CHD, and to evaluate the effectiveness of implementation of and adherence to clinical guidelines in daily practice[4,5]. Previous studies have shown that control of major cardiovascular risk factors in patients with established ASCVD varies from country to country, and is generally inadequate[4].
Azerbaijan is located in the South Caucasus region, at the crossroads of Asia and Europe, and is one of the regions at a very high risk for CVDs[6]. Our study aimed to assess adherence to ESC recommendations[7] for secondary prevention of a CVD based on the measurement of both modifiable risk factors and their therapeutic management in patients with confirmed CHD at different hospitals in Baku (Azerbaijan).
Six tertiary public (3) and private (3) health care centres from Baku (Azerbaijan) participated in the cross-sectional SURF CHD II study between November 2019 and July 2021. A one-page standard questionnaire of the study was used to collect information electronically on demographics, diagnostic category, risk factors, physical and laboratory data, and prescribed medications from consecutive patients aged ≥ 18 years with established CHD during routine outpatient visits.
The study protocol was approved by the Ethics Committee of Azerbaijan Society of Cardiology (ASC). CHD was defined as any of the following events in the history: Coronary artery bypass grafting (CABG); elective or urgent percutaneous coronary intervention (PCI); acute coronary syndrome (ACS), defined as cardiac chest pain at rest with objective evidence of acute ischemia or infarction; or stable angina pectoris (SAP), defined as clinical angina with objective confirmation by a positive exercise electrocardiogram or positive myocardial perfusion imaging or presence of stenosis of 70% or more in at least one coronary artery on coronary angiogram.
The questionnaire included demographics, risk factor history, risk factor measurements, and most recent laboratory measurements taken during outpatient visits by cardiologists. Demographic information included age, sex, ethnic group, and educational level. For the risk factor history, information was collected on smoking history, physical activity, family history of CVD, and previous history of hypertension, dyslipidaemia, and diabetes mellitus (DM) type I or II. We also collected information on risk factor and laboratory measurements: Height, weight, calculated body mass index (BMI), waist circumference (WC), systolic blood pressure (BP) (SBP) and diastolic BP (DBP), fasting blood glucose (BG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglyceride (TG), and glycated haemoglobin (HbA1c) for patients with DM.
Participation in cardiac rehabilitation (CR) and use of cardiac medications such as antiplatelet agents, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), Ca antagonists, other antihypertensive drugs, diuretics, statins, PCSK9 inhibitors, other lipid-lowering drugs, insulin, oral hypoglycaemic drugs, and nitrates were also reported in the questionnaire.
Smoking history was categorized into the current smoker (if participants were smokers at the time of the questionnaire or in the previous 6 mo), non-smoker, and ex-smoker (participants that had quit smoking more than 6 mo ago). The level of physical activity was divided into less, more, and equal to the recommended level: 30 min of moderately vigorous physical activity three to five times per week. It was considered that participants had a family history of premature CVD if they had a first-degree relative with a history of ASCVD before the age of 55 years for a male or 65 years for a female. The highest level of education, history of hypertension, dyslipidaemia, DM type 1 or type 2, and participation in CR were documented.
Depending on the BMI value, the following categories were identified[8]: Underweight < 18.5 kg/m2, normal weight 18.5-24.9 kg/m2, and overweight 25-29.9 kg/m2; obesity I degree: 30-34.9 kg/m2, obesity II degree: 35-39.9 kg/m2, and obesity III degree: ≥ 40 kg/m2. WC ≥ 88 cm in women and ≥ 102 cm in men was defined as abdominal obesity[7,8]. Arterial hypertension (AH) was established with the use of antihypertensives or BP > 140/90 mmHg[9]. Dyslipidaemia was defined as the use of statins or TC level of ≥ 200 mg/dL, LDL-C level of ≥ 130 mg/dL, TG level of ≥ 150 mg/dL, and HDL-C level of ≤ 40 mg/dL in men and ≤ 50 mg/dL in women[10]. DM was defined as the use of an antidiabetic drug or HbA1c level of ≥ 6.5%/or fasting BG level of ≥ 126 mg/dL[11].
Therapeutic targets were in accordance with ESC Guidelines and were identified as follows: Uncontrolled AH-SBP ≥ 140 mmHg or DBP ≥ 90 mmHg; uncontrolled DM-HbA1c ≥ 7%; uncontrolled LDL-C ≥ 70 mg/dL. Lifestyle targets were defined as reaching targets for smoking status (non-/ex-smoker), BMI < 25, and moderate/vigorous physical activity[7].
A cardiovascular health index score (CHIS) was calculated to summarize the burden of risk factors. The CHIS was calculated as the number of risk factors that each participant presented, from the following six risk factors: Non-/ex-smoker, BMI < 25 kg/m2, moderate/vigorous physical activity, controlled BP (< 140/90 mmHg; 140/80 mmHg for patients with DM), controlled LDL-C (< 70 mg/dL), and controlled BG (HbA1c < 7% or BG < 126 mg/dL). The following categories were defined: Poor, CHIS ≤ 2; intermediate, CHIS = 3-4; good, CHIS = 5-6[4].
Cases with missing data were excluded from the analysis. Statistical processing of the results was carried out using the Microsoft Excel and IBN SPSS Statistica v.21 software packages. The parameters were tested for normality of distribution using the Kolmogorov-Smirnov test. For normally distributed variables, descriptive statistics were used: mean ± SD, minimum, median, and maximum. To determine the statistical significance of differences between the two groups, Student's t-test (for continuous variables that showed a normal distribution), non-parametric Mann-Whitney U test (for continuous variables that did not show a normal distribution), and χ2 test were used. P < 0.05 was accepted as being statistically significant.
Data from 687 consecutive CHD outpatients (mean age 59.6 ± 9.6 years) were included in the study, and 171 (24.9%) of the participants were women.
Demographic characteristics and CHD category, hospital admission, and participation in CR according to the sex of patients are summarized in Table 1. All patients were Caucasian. The mean age of the female patients was significantly higher than that of the men (P < 0.0001). Of all patients, 39.4% were admitted to the hospital during the last year for a CHD-related reason, and only 15.1% participated in CR programs. Male participants in this study were found to have a higher prevalence in ACS and PCI (P = 0.001 and P = 0.004, respectively). More women than men had systolic AH (SAH) (P = 0.0002). No significant differences in the number of patients who underwent CABG, hospital admission in the last year, and participation in CR were observed between male and female patients.
| Total, n = 687 | Female, n = 171 | Male, n = 516 | P value | |
| Age (years) | 59.6 ± 9.58 | 62.4 ± 8.9 | 58.6 ± 9.6 | < 0.0001 |
| CHD category, n (%) | ||||
| CABG | 153 (22.3) | 41 (24) | 112 (22) | > 0.05 |
| PCI | 351 (51.1) | 71 (42) | 280 (54) | 0.004 |
| ACS | 172 (25.0) | 27 (16) | 145 (28) | 0.001 |
| SAP | 249 (36.2) | 82 (48) | 167 (32) | 0.0002 |
| HA | 271 (39.4) | 68 (40) | 203 (39) | > 0.05 |
| CR | 104 (15.1) | 19 (11.1) | 85 (16.5) | > 0.05 |
Table 2 represents the cardiovascular risk factors stratified by sex. A higher rate of smoking was found among males (32% vs 1.8% in female patients). The number of female patients with no smoking history was significantly higher compared to the male participants (96.5% and 29%, respectively). The sex differences were statistically significant for all categories of smoking history (P < 0.00001).
| Total, n = 687 | Female, n = 171 | Male, n = 516 | P value | |
| Smoking history | ||||
| Current smoker | 169 (24.6) | 3 (1.8) | 166 (32) | < 0.00001 |
| Ex-smoker | 169 (24.6) | 2 (1.2) | 167 (32) | < 0.00001 |
| Never smoked | 314 (45.7) | 165 (96.5) | 149 (29) | < 0.00001 |
| Unknown | 35 (5.1) | 1 (0.6) | 34 (7) | |
| Physical activity | ||||
| Less than below | 223 (32.5) | 66 (38.6) | 157 (30.4) | > 0.05 |
| Moderate | 324 (47.2) | 74 (43.3) | 250 (48.4) | > 0.05 |
| More than above | 82 (11.9) | 19 (11.1) | 63 (12.2) | > 0.05 |
| Unknown | 58 (8.4) | 12 (7.02) | 46 (8.9) | |
| Family history of premature CVD | ||||
| Yes | 265 (38.6) | 58 (33.9) | 207 (40.1) | > 0.05 |
| No | 355 (51.7) | 96 (56.1) | 259 (50.2) | > 0.05 |
| Unknown | 67 (9.8) | 17 (9.9) | 50 (9.7) | |
| Previous history of | ||||
| Hypertension | 537 (78.2) | 142 (83) | 395 (76.6) | > 0.05 |
| Dyslipidaemia | 255 (37.1) | 60 (35.1) | 195 (37.8) | > 0.05 |
| Diabetes | 310 (45.1) | 95 (55.6) | 215 (41.7) | 0.002 |
Of all participants, 48.3% reported a family history of premature CVD. There were no sex differences on this indicator.
A history of hypertension was reported by most patients (78.2%), while dyslipidemia and diabetes were reported by 37.1% and 45.1% of patients, respectively. Statistically significant sex differences between the groups were found in the prevalence of diabetes (55.6% vs 41.7% in females and males, respectively; P = 0.002).
It should be mentioned that body weight and height were not measured in all subjects, and consequently, BMI was calculated only in 31.4% of all participants. The risk factor and laboratory measurement results are displayed in Table 3. The mean BMI value in these patients was found to be 28.4 kg/m2, with the mean value of 29.6 kg/m2 in females and 28 kg/m2 in males (P = 0.002).
| Total | Female | Male | P value | |
| Systolic BP (mmHg) | n = 663 | n = 164 | n = 499 | |
| 138.4 (18.9) | 142.4 (1.4) | 137.1 (17.9) | 0.004 | |
| Diastolic BP (mmHg) | n = 658 | n = 162 | n = 496 | |
| 82.9 (10.7) | 82.7 (11.5) | 82.8 (10.4) | > 0.05 | |
| Heart rate (bmp) | n = 649 | n = 156 | n = 493 | |
| 77.6 (12.7) | 78.5 (12.0) | 77.3 (12.9) | > 0.05 | |
| BMI (kg/m2) | n = 216 | n = 50 | n = 166 | |
| 28.4 (3.02) | 29.6 (3.4) | 28 (2.8) | 0.002 | |
| WC (cm) | n = 30 | n = 13 | n = 17 | |
| 101 (12.9) | 100.8 (15.2) | 101.0 (11.3) | > 0.05 | |
| TC (mg/dL) | n = 347 | n = 86 | n = 261 | |
| 193.9 (52.4) | 200.4 (50.7) | 192.3 (53) | > 0.05 | |
| LDL-C (mg/dL) | n = 371 | n = 101 | n = 270 | |
| 111.2 (49.6) | 118.3 (49.7) | 108.6 (49.3) | > 0.05 | |
| HDL-C (mg/dL) | n = 185 | n = 50 | n = 135 | |
| 53.4 (13.8) | 54.4 (13.1) | 53 (14.1) | > 0.05 | |
| TG (mg/dL) | n = 367 | n = 93 | n = 274 | |
| 161.0 (76.0) | 169.8 (77.8) | 158 (75.4) | > 0.05 | |
| BG (mg/dL) | n = 277 | n = 73 | n = 204 | |
| 146.7 (71.5) | 162.7 (79.9) | 141 (67.5) | 0.04 | |
| HbA1c (%) | n = 137 | n = 44 | n = 93 | |
| 7.71 (1.72) | 8.1 (2.0) | 7.5 (1.5) | > 0.05 |
Waist circumference was measured only in 30 participants (4.4%, 13 females and 17 males), and it was high in 63.3% of those patients. Among them, 83.6% of females and 47.1% of males had abdominal obesity (P = 0.034).
In relation to laboratory data, there were no significant differences between male and female participants in TC, LDL, HDL, TG, or HbA1c values. However, BG levels were found to be higher in female patients (P = 0.04).
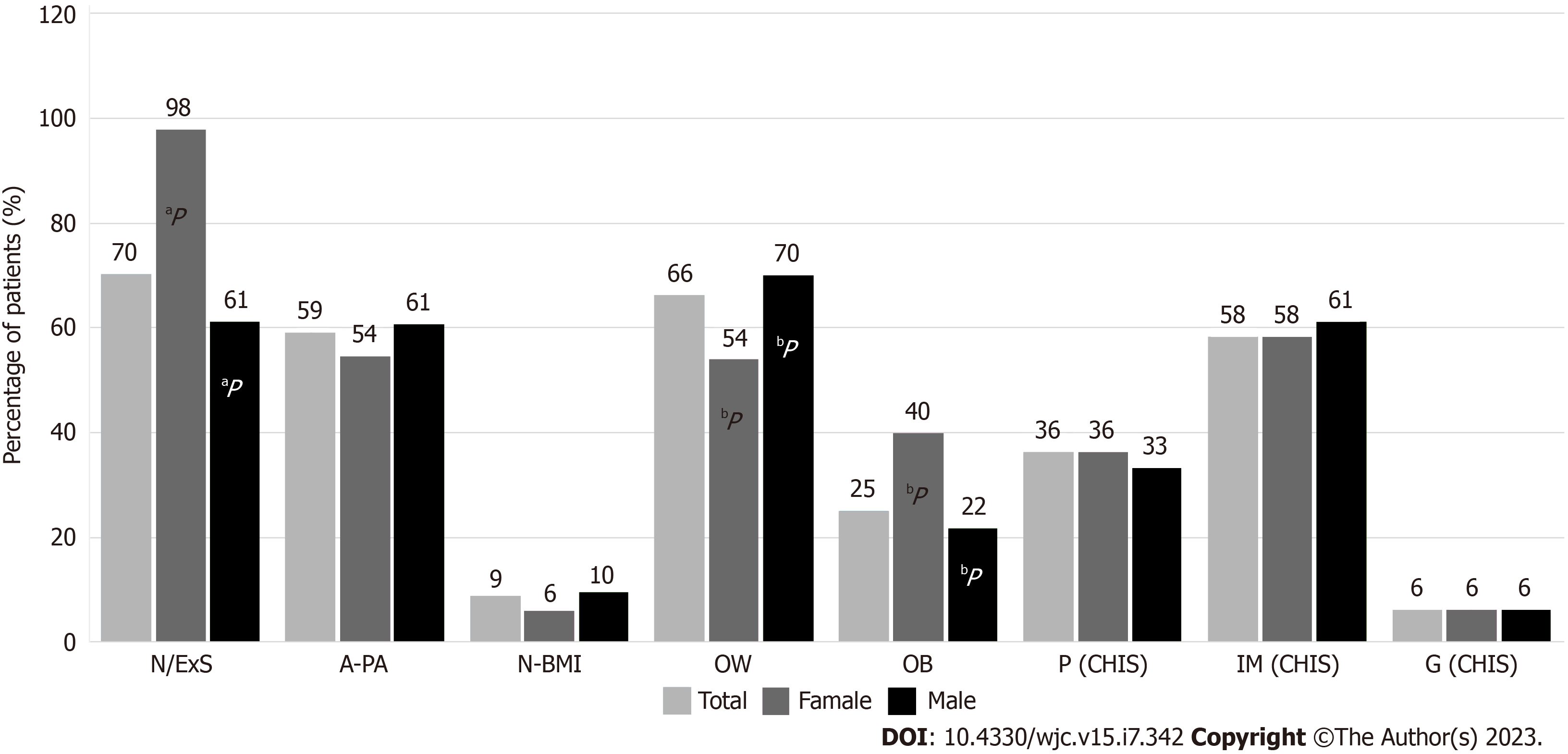
Lifestyle targets and CHIS categories in patients are represented in Figure 1. Non/ex-smokers were predominant among female participants (P < 0.00001). Approximately 60% of patients showed adequate physical activity, without significant differences between groups. However, in terms of BMI values, female patients had significantly higher values than male participants (P = 0.0294).
CHIS categories were calculated in 84 (12.2%) patients who had all the necessary clinical and laboratory measurements done. Good, intermediate, and poor categories were identified in 6%, 58.3%, and 35.7% of patients, respectively (without statistical differences between female and male patients).
When analyzing uncontrolled BP rates across different categories of AH, the prevalence of uncontrolled SBP was higher than that of other BP categories (Table 4). There were no statistical differences between females and males within each category. Differences between the two groups were only observed in the category of isolated systolic hypertension with a higher prevalence in women (P = 0.029).
| BP category, n = 658 | Total (%) | Female (%) | Male (%) | P value |
| SDH | 27.5 | 27.8 | 27.4 | 0.929 |
| ISH | 20.9 | 26.8 | 18.8 | 0.029 |
| IDH | 6.8 | 6.8 | 6.9 | 0.977 |
The rates of uncontrolled risk factors in patients with a previous history of hypertension (n = 537), dyslipidaemia (n = 255), and DM (n = 310) are represented in Figure 2. As shown in the figure, uncontrolled SBP was detected in 292 (54.6%), and uncontrolled DBP was found in 204 (39%) participants. Systolic-diastolic AH (SDH) was found in 169 (31.5%), isolated SAH in 121 (22.5%), and isolated DAH in 34 (6.3%) patients with AH.
The rate of medication use is shown in Table 5. Antiplatelet drugs were used in 84.6%, and beta-blockers in 53.3% of patients, both with an equal rate among female and male participants. Approximately 73.9% of patients were using statins, with a higher usage rate observed among male patients (P = 0.012). As for ACE inhibitors, 51.2% of patients were using them, with a higher usage rate observed among female patients (P = 0.044). Ca antagonists were used in 29.3%, oral hypoglycaemics in 23%, diuretics in 22.3%, and nitrates in 21.3% of patients. Other groups of medications were used in less than 6% of patients. Oral hypoglycemic drugs, insulin, and nitrate use was higher among female patients (P = 0.025,
| Medications | Total | Male | Female | P value |
| n = 687 | n = 516 | n = 171 | ||
| Antiplatelets | 84.6 | 85.3 | 82.5 | 0.377 |
| Beta blockers | 53.3 | 55.2 | 47.4 | 0.074 |
| ACE inhibitors | 51.2 | 49.0 | 57.9 | 0.044 |
| Ca antagonists | 29.3 | 28.7 | 31.0 | 0.565 |
| ARB-s | 6.0 | 5.8 | 6.4 | 0.767 |
| Diuretics | 22.3 | 20.5 | 27.5 | 0.059 |
| Other antihypertensives | 2.3 | 1.9 | 3.5 | 0.238 |
| Nitrates | 21.3 | 7.6 | 62.6 | < 0.00001 |
| Insulin | 7.6 | 6.4 | 11.1 | 0.043 |
| Oral hypoglycaemics | 23 | 20.9 | 29.2 | 0.025 |
| Statins | 73.9 | 76.4 | 66.7 | 0.012 |
| Other lipid lowering | 1.3 | 1.2 | 1.8 | 0.555 |
A clinical audit is a ‘quality improvement process that seeks to improve patient care and outcomes through a systematic review of care and the implementation of change’[12]. The SURF CHD II clinical audit conducted in Azerbaijan has shown that the prevalence of major cardiovascular risk factors in patients with ASCVD is high. The level of recordings of some risk factors was low, as there was a lack of information on BMI, WC, TC, LDL-C, HDL-C, TG, and HbA1c.
The number of patients involved in the CR program was inadequate (15.1%). The rate of uncontrolled RF was high: SBP (54.6%), DBP (39%), LDL-C (86.8%), DM (60.6%), as well as overweight (66.6%) and obesity (25%). In addition, significant differences in prevalence and control of some risk factors (smoking, BMI, WC, BG, and SBP) between female and male participants have been found.
To effectively manage CVDs, it is vital to recognize their multifactorial nature and implement preventive measures that target modifiable risk factors. These measures should include optimizing physical activity, encouraging smoking cessation, reducing BMI, and treating AH, diabetes, and hyperlipidemia. The positive effects of lifestyle modification and optimal pharmacological interventions on cardiovascular morbidity and mortality have been demonstrated in previous studies[13-15].
Smoking cessation is one of the most effective measures for reversing vascular injury and preventing the development of atherosclerosis and fatal cardiovascular outcomes[16,17].
The information collected in several national surveys conducted in Azerbaijan has shown that there is a high prevalence of risk factors such as smoking, overweight, unhealthy diet, and physical inactivity which are responsible for the great majority of NCD cases. One of the studies conducted to gather information on the health of the population is the WHO-recommended STEPS survey. This survey has been conducted nationwide in both 2011 and 2017[18]. Analysis of the study results, conducted among 3000 adult population aged 18 years and above, has shown that smoking is one of the major problems for Azerbaijani society. Overall, the prevalence of smoking was significantly higher among men (48.8%) than among women (0.2%) who were identified as current smokers. This difference in smoking prevalence can be largely attributed to the social stigma surrounding smoking among women, as it is often viewed negatively within the local culture.
The study also found that 24.9% of all respondents had been exposed to secondhand smoke at home, with men showing a higher incidence of exposure than women. The results of the SURF study are consistent with these data: The smoking rate was 24.6%, and it was significantly high among men than in women (32% vs 1.8%, accordingly).
Comorbidities such as hypertension, dyslipidaemia, and diabetes are known risk factors for CHD events and may indicate an increased susceptibility to atherosclerosis development. In the current study, uncontrolled SBP was found in 54.6% of patients with reported AH. According to the STEPS study, the prevalence of AH among the general population was about 30%[18]. Most of the respondents with high BP (65.4%) were not taking any medication. Salt intake was around 10 g per day, with a significant gender difference (11.4% of men vs 26.8% of women). The above-mentioned aspects of behaviour and dietary habits could also contribute to the poor management of BP in the participants of the SURF study.
The SURF study has demonstrated that BMI values were high in 91% of participants, which could indicate that BMI is one of the most common risk factors in the development of coronary artery disease (CAD). But it should also be taken into consideration that parameters such as BMI and WC were measured only in a small group of patients and mainly in persons with apparent high body weight and abdominal obesity. This circumstance may have an impact on the data obtained.
The study results have shown that approximately 50% of the patients did not reach even the first target level of lipids[7], despite the fact that the rate of statin usage among this category of patients was 86.4%. These reasons could include discontinuation of statin therapy due to poor adherence and compliance to treatment recommendations, as well as not achieving the target dosage of the medication[19]. A similar pattern was observed with respect to the patients with DM: Despite insulin and oral hypoglycemic drugs use, HbA1c level did not reach the targets in the majority (60.6%) of them.
The cross-sectional study European Action on Secondary and Primary Prevention by Intervention to Reduce Events (EUROASPIRE) IV was undertaken at 78 centres in 24 European countries with the involvement of 7998 patients < 80 years of age with CAD[20]. While Azerbaijan did not participate in EUROASPIRE, the results acquired from the mentioned study can be compared with the results of the SURF study conducted in our country. It was observed that in Azerbaijani patients with ASCVD, the mean age was younger, the rate of smoking was higher, and the rate of controlled BP level was lower. Uncontrolled LDL-C levels (≥ 70 mg/dL) and BMI greater than 30 kg/m2 were found to be lower in our study.
According to the study results, despite that the smoking rate was significantly high among men than in women, higher values of BMI and WC, as well as BG level and history of DM type 2, were found in female participants. Furthermore, the STEPS study has demonstrated that in the general population, approximately 91% of women are not engaging in vigorous physical activity.
These findings comply with the literature data. A systematic review conducted on the distribution by gender of diabetes, risk factors, complications, and disease control in the Caribbean general population has shown that women were more likely than men to have diabetes and obesity. This review also found that women were less physically active than men, but they were less likely to smoke cigarettes[21]. The authors of this review discovered that there was a statistically significant association between gender and diabetes, with women being at a risk of more than one and a half times greater than men.
It could be concluded from the foregoing that the gender differences in the distribution of CV risk factors such as DM, obesity, lack of physical activity, and smoking should be taken into account in the pharmacological management of patients with and without CVD and when designing rehabilitation programmes.
When comparing the rates of medication usage in our study and the results of the cross-sectional study EUROASPIRE IV[20], the rate of cardioprotective medication use was higher in the latter case (anti-platelets 93.8% vs 84.6%; statins 85.7% vs 73.9%, beta-blockers 82.6% vs 53.3%; ACE inhibitors/ARBs 75.1% vs 51.2%). According to the data of the SURF CHD II[5] study, the use of statins in the European region was 78.94%, which is broadly comparable to our data.
Adherence and compliance play a major role in all pharmacological therapies. The causes of non-compliance can be classified into the following categories: Patient, physician, and health system-related[22]. Similarly, with dyslipidemia, diabetes, and hypertension, the causes of poor control of risk factors should be carefully analyzed for the effective implementation of the guideline recommendations into clinical practice.
Only 15.1% of patients reported participation in CR in our study, despite this is a recommendation class I and the level of evidence A intervention[3]. The literature indicates that the number of patients who participate in CR programs, especially in low-income countries, is extremely low, and patients’ adherence is often scarce[23]. There are several known barriers to the implementation of CR and adherence to such programs. Some of these barriers include limited availability of services, high program costs, long travel distances to access services, low referral rates from healthcare providers, and low levels of patient motivation to participate in rehabilitation programs[23-27], and these reasons may have contributed to the low participation in CR in Azerbaijan.
Another likely reason for the low participation rate in CR could be that these programs are only offered in a limited number of hospitals, and patients are required to cover almost all the costs out-of-pocket. It is expected that reforms in the health system and the financing of medical services, such as the introduction of compulsory health insurance, will help fill this missing gap in the secondary prevention of CVDs.
In 2015, the ‘Strategy for Non-Communicable Diseases’ was adopted in order to achieve a significant reduction in premature deaths associated with NCDs in the country. The objectives of the Strategy are to establish an effective inter-sectoral cooperation mechanism to combat NCDs, to take measures to reduce the main risk factors (tobacco use, alcohol abuse, unhealthy diet, and physical inactivity), and to prevent and control these diseases. Their role does not merely focus on improving the healthcare system and healthcare services, but also on promoting a healthy lifestyle for the population[18].
As a result of the implementation of the project on improving the national legislative framework to combat the tobacco epidemic, the parliament of the country adopted a new law aimed at enhancing limitations on tobacco use in public spaces. This law supports the establishment of tobacco control programs, hotlines, and pharmacotherapy initiatives to assist individuals in smoking cessation[18,28].
Preventive campaigns are the mainstay of activities to combat NCDs in Azerbaijan. The Ministry of Health (MoH) developed a health awareness-raising web portal for the population, which includes articles about non-communicable diseases and their risk factors and prevention strategies. MoH and ASC provide information days and thematic conferences to increase awareness of CVD prevention among the population. Some non-governmental and public organisations also participate in the promotion and popularisation of healthy lifestyles and primary prevention.
Important steps have been taken to improve the rehabilitation services in the country: The new degree programs, which include cardiovascular rehabilitation modules, have been launched[28]. The cardiology curriculum for residents has been updated in line with the ESC standards, and now it contains a chapter on cardiovascular prevention and rehabilitation.
E-training courses for cardiologists from remote areas have been initiated by MoH and ASC. One of the successful programs included the establishment of a portal for specific e-training on cardiovascular risk factors, promotion of physical activity, and tobacco cessation skills for physicians, among others[28].
Despite these measures, the results of the SURF study and previous population-based studies have shown that the rate of risk factors is still high among both the general population and patients with documented CVD. This demonstrates once more the need of consistent training for healthcare professionals, notably primary care physicians, as well as patients, and the need for the healthcare system to pay more attention to this issue. Such measures will undoubtedly help to reduce the frequency of undesirable consequences and rehospitalisations in this category of patients, and hence reduce healthcare costs.
The SURF CHD study uses a one-page, simple questionnaire that allows rapid data collection. It can be completed in a very short period during a routine outpatient visit, requires involving a larger population in the study with minimal effort.
Clinical audits such as SURF also enhance process improvement: In light of the results, changes can be implemented in the procedures to record and manage risk factors, and re-auditing can inform on the effectiveness of these changes to improve risk factor recording and management.
However, it should be mentioned that the current study has several limitations. First, it only included tertiary level hospitals in the capital city (however, it is planned to include primary and secondary health care facilities from the different regions of Azerbaijan at the further stages of the study). Second, for some risk factors such as waist circumference, data were not recorded in all participants. This suggests that some clinicians overlook certain risk factors, and one of the important roles of an audit such as SURF is to stimulate fuller recording of relevant data.
Our study has demonstrated that the control of cardiovascular risk factors and lifestyle changes recommended by clinical CVD prevention guidelines in patients with CHD is unsatisfactory. The number of patients involved in CR program is low, and the high level of uncontrolled risk factors among patients who participated in CR indicates the poor adherence and compliance among patients. Monitoring and control of the modifiable risk factors are not at a desired level, and require more organized work and collaboration of healthcare providers from different healthcare facilities.
The above-mentioned trends and individual and gender characteristics of patients should be considered by healthcare organizers when planning secondary prevention activities and public health protection measures.
The strategic needs for prevention and rehabilitation in Azerbaijan are to increase the number of rehabilitation centres and ensure their adequate geographical distribution, with a particular focus on the regions of the country, and to expand indications of CR services and programs for primary and secondary prevention for the population with high and very high cardiovascular risk. More efforts are needed to improve and strengthen the mechanism for education of primary healthcare providers in the field of cardiac prevention and rehabilitation.
It is also suggested that Standard Operating Procedures should be developed for cardiac clinics in regions to facilitate process improvement.
Low level of monitoring and control of modifiable risk factors necessitates better structured effort and coordination of health care specialists from various healthcare facilities. The strategic needs for prevention and rehabilitation in Azerbaijan are to increase the number of rehabilitation centers and ensure their adequate geographical distribution, with a particular focus on the country's regions, and to expand indications of cardiac rehabilitation (CR) services and programs for primary and secondary prevention for the population with high and very high cardiovascular risk, and to expand indications of CR services and programs for primary and secondary prevention for the population with high and very high cardiovascular risk. It is also proposed that cardiac clinics adopt Standard Operating Procedures. More effort is required to improve and reinforce the process for primary health care provider education in the field of cardiac prevention and rehabilitation.
Previous studies have shown that control of major cardiovascular risk factors is generally inadequate in patients with established atherosclerotic cardiovascular disease (CVD) (ASCVD). Azerbaijan is a country in the South Caucasus, a region at very high risk for CVD. The aim of this study was to evaluate compliance with the recommendations of the European Society of Cardiology (ESC) for secondary prevention of CVD based on the measurement of both modifiable major risk factors and their therapeutic management in patients with confirmed coronary heart disease (CHD) in Azerbaijan. We believe that these results will contribute to the improvement of the situation in secondary prevention of CHD in the country.
This study focused on the national results of the Survey of Risk Factors in CHD (SURF CHD) II study in Azerbaijan.
SURF CHD II study uses a one-page, standard questionnaire that allows rapid data collection. Information on demographics, risk factors, physical and laboratory data, and medications was collected in consecutive outpatients aged ≥ 18 years with established atherosclerotic CHD. Data from 687 patients (mean age 59.6 ± 9.58 years; 24.9% female) were included in the study.
The study results show that the control of cardiovascular risk factors and lifestyle modification measures indicated by clinical CVD prevention recommendations in patients with CHD are inadequate. The number of patients with CHD enrolled in a CR program is small as well.
The findings of the SURF study can be used to improve processes by changing the techniques for documenting and monitoring CVD risk variables, and re-auditing can provide insight into the effectiveness of these modifications in improving the management of patients with ASCVD.
It is critical to efficiently manage the main cardiovascular risk factors in order to prevent CVD mortality. The international SURF CHD II clinical audit measures modifiable risk factors to assess adherence to ESC recommendations for secondary prevention of CVD in patients with established CHD.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Azerbaijan Society of Cardiology, No. 000112; European Association of Cardiology, No. 119457; European Association of Preventive Cardiology.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Azerbaijan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Popovic DS, Serbia; Yang L, China S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Xu ZH
| 1. | Safiri S, Karamzad N, Singh K, Carson-Chahhoud K, Adams C, Nejadghaderi SA, Almasi-Hashiani A, Sullman MJM, Mansournia MA, Bragazzi NL, Kaufman JS, Collins GS, Kolahi AA. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990-2019. Eur J Prev Cardiol. 2022;29:420-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 136] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 2. | Banatvala N, Akselrod S, Bovet P, Mendis S. Global Action Plan for the Prevention and Control of Noncommunicable diseases 2013-2020. Available from: https://www.taylorfrancis.com/chapters/oa-edit/10.4324/9781003306689-36/global-action-plan-prevention-control-ncds-2013%E2%80%932030-nick-banatvala-svetlana-akselrod-pascal-bovet-shanthi-mendis. |
| 3. | Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, Benetos A, Biffi A, Boavida JM, Capodanno D, Cosyns B, Crawford C, Davos CH, Desormais I, Di Angelantonio E, Franco OH, Halvorsen S, Hobbs FDR, Hollander M, Jankowska EA, Michal M, Sacco S, Sattar N, Tokgozoglu L, Tonstad S, Tsioufis KP, van Dis I, van Gelder IC, Wanner C, Williams B; ESC National Cardiac Societies; ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227-3337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3739] [Cited by in RCA: 3310] [Article Influence: 827.5] [Reference Citation Analysis (0)] |
| 4. | Zhao M, Cooney MT, Klipstein-Grobusch K, Vaartjes I, De Bacquer D, De Sutter J, Reiner Ž, Prescott E, Faggiano P, Vanuzzo D, AlFaleh H, Menown IB, Gait D, Posogova N, Sheu WH, Zhao D, Zuo H, Grobbee DE, Graham IM. Simplifying the audit of risk factor recording and control: A report from an international study in 11 countries. Eur J Prev Cardiol. 2016;23:1202-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Marza Florensa A, Vaartjes I, Klipstein-Grobusch K, Zhao M, Cooney MT, Graham I, Grobbee D. Survey of risk factors in coronary heart disease: novel recruitment strategy and preliminary results. Eur J Public Health. 2021;31:ckab164.104. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Campbell NRC, Ordunez P, Giraldo G, Rodriguez Morales YA, Lombardi C, Khan T, Padwal R, Tsuyuki RT, Varghese C. WHO HEARTS: A Global Program to Reduce Cardiovascular Disease Burden: Experience Implementing in the Americas and Opportunities in Canada. Can J Cardiol. 2021;37:744-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 7. | Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Løchen ML, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315-2381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5080] [Cited by in RCA: 4706] [Article Influence: 522.9] [Reference Citation Analysis (1)] |
| 8. | Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1. [PubMed] |
| 9. | Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021-3104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7431] [Cited by in RCA: 6365] [Article Influence: 909.3] [Reference Citation Analysis (0)] |
| 10. | Ahmed HM, Miller M, Nasir K, McEvoy JW, Herrington D, Blumenthal RS, Blaha MJ. Primary Low Level of High-Density Lipoprotein Cholesterol and Risks of Coronary Heart Disease, Cardiovascular Disease, and Death: Results From the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2016;183:875-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Kerner W, Brückel J; German Diabetes Association. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes. 2014;122:384-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 311] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 12. | Rose N, Pang DSJ. A practical guide to implementing clinical audit. Can Vet J. 2021;62:145-152. [PubMed] |
| 13. | de Waure C, Lauret GJ, Ricciardi W, Ferket B, Teijink J, Spronk S, Myriam Hunink MG. Lifestyle interventions in patients with coronary heart disease: a systematic review. Am J Prev Med. 2013;45:207-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Rizzuto D, Fratiglioni L. Lifestyle factors related to mortality and survival: a mini-review. Gerontology. 2014;60:327-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Colom C, Rull A, Sanchez-Quesada JL, Pérez A. Cardiovascular Disease in Type 1 Diabetes Mellitus: Epidemiology and Management of Cardiovascular Risk. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 16. | Yugar-Toledo JC, Vilela-Martin F, Dinamarco N, Rodrigues B, Moreno H. Smoking and Endothelial Dysfunction: An Integrated - Medical and Molecular Review. Med Res Arch. 2022;10. [DOI] [Full Text] |
| 17. | Duncan MS, Freiberg MS, Greevy RA Jr, Kundu S, Vasan RS, Tindle HA. Association of Smoking Cessation With Subsequent Risk of Cardiovascular Disease. JAMA. 2019;322:642-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 243] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 18. | Ng N, Stenlund H, Bonita R, Hakimi M, Wall S, Weinehall L. Preventable risk factors for noncommunicable diseases in rural Indonesia: prevalence study using WHO STEPS approach. Bull World Health Organ. 2006;84:305-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Martin-Ruiz E, Olry-de-Labry-Lima A, Ocaña-Riola R, Epstein D. Systematic Review of the Effect of Adherence to Statin Treatment on Critical Cardiovascular Events and Mortality in Primary Prevention. J Cardiovasc Pharmacol Ther. 2018;23:200-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Kotseva K, Wood D, De Bacquer D, De Backer G, Rydén L, Jennings C, Gyberg V, Amouyel P, Bruthans J, Castro Conde A, Cífková R, Deckers JW, De Sutter J, Dilic M, Dolzhenko M, Erglis A, Fras Z, Gaita D, Gotcheva N, Goudevenos J, Heuschmann P, Laucevicius A, Lehto S, Lovic D, Miličić D, Moore D, Nicolaides E, Oganov R, Pajak A, Pogosova N, Reiner Z, Stagmo M, Störk S, Tokgözoğlu L, Vulic D; EUROASPIRE Investigators. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016;23:636-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 594] [Cited by in RCA: 637] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 21. | Sobers-Grannum N, Murphy MM, Nielsen A, Guell C, Samuels TA, Bishop L, Unwin N. Female gender is a social determinant of diabetes in the Caribbean: a systematic review and meta-analysis. PLoS One. 2015;10:e0126799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86:304-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1064] [Cited by in RCA: 1251] [Article Influence: 89.4] [Reference Citation Analysis (1)] |
| 23. | Pesah E, Turk-Adawi K, Supervia M, Lopez-Jimenez F, Britto R, Ding R, Babu A, Sadeghi M, Sarrafzadegan N, Cuenza L, Anchique Santos C, Heine M, Derman W, Oh P, Grace SL. Cardiac rehabilitation delivery in low/middle-income countries. Heart. 2019;105:1806-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 63] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 24. | Lu M, Xia H, Ma J, Lin Y, Zhang X, Shen Y, Hravnak M. Relationship between adherence to secondary prevention and health literacy, self-efficacy and disease knowledge among patients with coronary artery disease in China. Eur J Cardiovasc Nurs. 2020;19:230-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Winnige P, Vysoky R, Dosbaba F, Batalik L. Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases. World J Clin Cases. 2021;9:1761-1784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 57] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (10)] |
| 26. | Kähkönen O, Saaranen T, Kankkunen P, Lamidi ML, Kyngäs H, Miettinen H. Predictors of adherence to treatment by patients with coronary heart disease after percutaneous coronary intervention. J Clin Nurs. 2018;27:989-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 27. | Turk-Adawi K, Sarrafzadegan N, Grace SL. Global availability of cardiac rehabilitation. Nat Rev Cardiol. 2014;11:586-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 156] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 28. | Gabulova R, Seyidov N. EAPC Country of the month–Azerbaijan. Available from: https://www.escardio.org/Sub-specialty-communities/European-Association-of-Preventive-Cardiology-(EAPC)/Advocacy/Prevention-in-your-country/country-of-the-month-azerbaijan. |