Published online Mar 26, 2023. doi: 10.4330/wjc.v15.i3.106
Peer-review started: December 12, 2022
First decision: January 20, 2023
Revised: January 24, 2023
Accepted: February 22, 2023
Article in press: February 22, 2023
Published online: March 26, 2023
Processing time: 98 Days and 9.4 Hours
Myocardial ischemia and ST-elevation myocardial infarction (STEMI) increase QT dispersion (QTD) and corrected QT dispersion (QTcD), and are also associated with ventricular arrhythmia.
To evaluate the effects of reperfusion strategy [primary percutaneous coronary intervention (PPCI) or fibrinolytic therapy] on QTD and QTcD in STEMI patients and assess the impact of the chosen strategy on the occurrence of in-hospital arrhythmia.
This prospective, observational, multicenter study included 240 patients admitted with STEMI who were treated with either PPCI (group I) or fibrinolytic therapy (group II). QTD and QTcD were measured on admission and 24 hr after reperfusion, and patients were observed to detect in-hospital arrhythmia.
There were significant reductions in QTD and QTcD from admission to 24 hr in both group I and group II patients. QTD and QTcD were found to be shorter in group I patients at 24 hr than those in group II (53 ± 19 msec vs 60 ± 18 msec, P = 0.005 and 60 ± 21 msec vs 69+22 msec, P = 0.003, respectively). The occurrence of in-hospital arrhythmia was significantly more frequent in group II than in group I (25 patients, 20.8% vs 8 patients, 6.7%, P = 0.001). Furthermore, QTD and QTcD were higher in patients with in-hospital arrhythmia than those without (P = 0.001 and P = 0.02, respectively).
In STEMI patients, PPCI and fibrinolytic therapy effectively reduced QTD and QTcD, with a higher observed reduction using PPCI. PPCI was associated with a lower incidence of in-hospital arrhythmia than fibrinolytic therapy. In addition, QTD and QTcD were shorter in patients not experiencing in-hospital arrhythmia than those with arrhythmia.
Core Tip: We evaluated the effect of a reperfusion strategy on QT dispersion (QTD) and corrected QT dispersion (QTcD) in patients with ST-segment elevation myocardial infarction. Primary percutaneous coronary intervention was found to be superior in the reduction of QTD and QTcD and associated with a lower incidence of in-hospital arrhythmias when compared to fibrinolytic therapy. In addition, QTD and QTcD were shorter in patients not experiencing in-hospital arrhythmia than those with arrhythmia.
- Citation: Abdelmegid MAKF, Bakr MM, Shams-Eddin H, Youssef AA, Abdel-Galeel A. Effect of reperfusion strategy on QT dispersion in patients with acute myocardial infarction: Impact on in-hospital arrhythmia. World J Cardiol 2023; 15(3): 106-115
- URL: https://www.wjgnet.com/1949-8462/full/v15/i3/106.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i3.106
Arrhythmia is a major cause of death in ST-elevation myocardial infarction (STEMI) patients, especially in the early in-hospital period[1]. Many studies have shown that dispersion of repolarization is the most common trigger and the main substrate for the occurrence of lethal arrhythmia in patients with STEMI[1-3]. QT dispersion (QTD), the difference between maximal and minimal QT interval calculated on a standard 12-lead electrocardiogram (ECG), measures the heterogeneity of myocardial repolarization[4]. It has previously been discovered that QT interval and QTD are increased in cases of acute ischemia and STEMI[5]. These variations may reflect the changing patterns of underlying recovery of ventricular excitability, which is profoundly disturbed at the earliest phase of acute myocardial infarction (MI)[6]. Moreover, QTD prolongation has been reported as a predictor of arrhythmia in patients with STEMI[7].
Although primary percutaneous coronary intervention (PPCI) is the treatment of choice when managing STEMI patients, fibrinolytic therapy is still an important reperfusion strategy in settings where primary PCI cannot be offered at the appropriate time[8]. Reperfusion of the infarct-related artery, either by fibrinolytic therapy or PPCI, could homogenize the duration of the ventricular action potential, thereby reducing the QTD. However, there are conflicting data about the effects of both perfusion therapy modes with respect to their abilities to reduce QTD in patients with STEMI. Moreover, there are inadequate data relating to the effects of these reperfusion strategies on incidence of in-hospital arrhythmias.
Here, we evaluate the QTD and corrected QT dispersion (QTcD) in patients presenting with STEMI by comparing those treated with PPCI with those receiving fibrinolytic therapy. In addition, the impacts of these treatment modalities on in-hospital incidence of arrhythmia are compared.
This was a prospective, observational, multicenter study that included 240 consecutive patients with first acute STEMI who were treated with either fibrinolytic therapy or PPCI. Patients with STEMI who received either fibrinolytic therapy with successful fibrinolysis or PPCI with final thrombolysis in myocardial infarction (TIMI) flow grade III were included. This study was conducted at 4 centers. PPCI-treated patients were recruited and treated at Assiut University Heart Hospital (a center with resources to perform this procedure at any time), and the fibrinolytic therapy-treated patients were recruited and treated at Sohag Heart & GIT Center, Assiut Police Hospital, and Qena General Hospital.
The STEMI diagnosis in each case was made using the 4th universal definition of MI, which is based on typical electrocardiographic changes alongside clinical symptoms associated with elevation of cardiac biomarkers[9]. Patients were included if they had chest pain for more than 30 min, ST-segment elevation in at least 2 contiguous ECG leads, and hospital admission within 12 hr of onset of chest pain. Successful fibrinolysis was defined as the presence of at least 2 of the following criteria: (1) Disappearance of chest pain within 90 min of starting the fibrinolytic infusion; (2) resolution of ST-segment elevation (in the ECG lead with maximum ST-elevation at baseline) by more than 50% after starting fibrinolytic infusion; or (3) abrupt initial increase in cardiac enzyme levels within the first 24 hr following onset of symptoms[10].
Exclusion criteria were non-ST elevation myocardial infarction, prior history of MI or surgical revascularization, absence of sinus rhythm, presence of bundle branch block or any other inter
Patients were classified into 2 groups based on the reperfusion strategy used. Group I (120 patients) were treated with PPCI and group II (120 patients) received fibrinolytic therapy (1.5 million units of streptokinase given intravenously over 30-60 min).
The 12-lead ECG was recorded at a paper speed of 25 mm/sec. and 10 mm/mV gain standardization. ECG measurements were taken on admission and 24 hr after the reperfusion with either of the two strategies using an ECG machine (EC3T 01 RD/1, MONITOR, Russia). Heart rate, QT interval, and corrected QT (QTc) interval for each ECG lead were calculated automatically using built-in software (ArMaSoft-12-Cardio software, MONITOR, Russia) using Bazett’s formula[11]. QT and QTc dispersions were defined as the differences between the maximum and minimum QT and QTc intervals, respectively, in a given ECG lead. Delta (∆) was defined as the difference in ECG measurement parameters before treatment and 24 hr after reperfusion. For example, ∆ QT interval was defined as the QT interval before treatment minus the QT interval 24 hr after reperfusion. ECG data were included where there were adequate measurements using at least 8 leads total with at least 4 precordial leads. All ECGs were in sinus rhythm.
The study endpoint was designated as the occurrence of arrhythmia during admission. Examples of arrhythmias considered included frequent premature ventricular ectopic beat, non-sustained ventricular tachycardia, sustained ventricular tachycardia, ventricular fibrillation, and atrial fibrillation. The study population was further classified into 2 more groups according to the incidence of in-hospital arrhythmia. These groups comprised an in-hospital arrhythmia group whose arrhythmias were recorded and a group who did not experience arrhythmia during admission (and therefore had no recorded arrhythmia events).
Sample size calculation was carried out using G Power 3 software. The calculated minimum sample of adult patients presenting with STEMI was 238. This calculation was made based on a 2-group 1:1 design [Group I (n = 119): treated with PPCI and Group II (n = 119): treated with fibrinolytic therapy] and would have 85% power to detect an absolute difference of 35% in the mean QTD, at a 1-sided significance level of 0.05.
This study was approved by the Committee of Medical Ethics of the Faculty of Medicine, Assiut University (IRB No. 17101454), and complies with the Declaration of Helsinki. Written informed consent was obtained from all participants. The authors are accountable for all aspects of the work, including full data access, integrity of the data, and the accuracy of the data analysis. They ensure that questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved.
Continuous variables with normal distribution were expressed as mean ± standard deviation (SD) and those without normal distribution as median (interquartile range). Normality of the continuous variables was checked with the Kolmogorov-Smirnov test. Categorical variables were expressed as frequency and percentage (%). Continuous variables were compared using an unpaired student's t-test for normally distributed data and Mann-Whitney test for non-normally distributed data. Comparisons of ECG data before and after reperfusion therapy were conducted using paired t-tests. Chi-Square tests or Fisher exact tests were used when appropriate to compare categorical variables. A P value of < 0.05 was considered statistically significant, with all reported P values being 2-tailed. All statistical analyses were performed using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, United States).
Table 1 shows similar baseline clinical characteristics of both groups of the study population. Moreover, there were no significant differences between the groups with respect to the location of MI and the time from chest pain onset to the start of the reperfusion (Table 1).
| Characteristic | Group I, n = 120 patients | Group II, n = 120 patients | P value |
| Age in yr | 57.9 ± 9.6 | 59.1 ± 10.7 | 0.38 |
| Male sex | 96 (80) | 93 (77.5) | 0.64 |
| Smoking | 49 (40.8) | 58 (48.3) | 0.24 |
| Hypertension | 35 (29.2) | 43 (35.8) | 0.27 |
| Diabetes mellitus | 38 (31.7) | 40 (33.3) | 0.78 |
| CKD | 4 (3.3) | 7 (5.8) | 0.35 |
| Family history of CAD | 15 (12.5) | 21 (17.5) | 0.28 |
| Dyslipidemia | 61 (50.8) | 49 (40.8) | 0.12 |
| Location of MI: Anterior MI non-anterior MI | 72 (60) 48 (40) | 61 (50.8) 59 (49.2) | 0.15 |
| Time from chest pain onset to reperfusion in hr | 4.04 ± 1.96 | 4.39 ± 2.79 | 0.29 |
Regardless of the chosen perfusion strategy, there was a significant reduction in QTD and QTcD from admission to 24 hr after reperfusion. This reduction in both QTD and QTcD was due to a significant increase in the minimum QT interval (∆ = - 15.9 ± 42.4 msec) with a concomitant decrease in maximum QT interval (∆ = 8.5 ± 47.8 msec) for the QTD and an increase in the minimum QTc interval (∆ = - 22.4 ± 44.5 msec) alongside a concomitant decrease in QTc interval (∆ = 5.1 ± 47.8 msec) for the latter measurement (Table 2).
| Parameter | Before reperfusion, n = 240 patients | After reperfusion, n = 240 patients | ∆ | P value |
| Heart rate in beat/min | 78.6 ± 16.2 | 80.5 ± 15.7 | -1.8 ± 16.9 | 0.09 |
| Maximum QT in msec | 407.1 ± 43.0 | 398.7 ± 45.2 | 8.5 ± 47.8 | 0.007 |
| Minimum QT in msec | 325.4 ± 41.7 | 341.3 ± 43.7 | -15.9 ± 42.4 | < 0.001 |
| QTD in msec | 81.8 ± 21.9 | 57.3 ± 18.9 | 24.4 ± 18.7 | < 0.001 |
| Maximum QTc in msec | 461.2 ± 42.5 | 456.1 ± 38.9 | 5.1 ± 47.8 | 0.10 |
| Minimum QTc in msec | 368.5 ± 37.6 | 390.0 ± 36.4 | -22.4 ± 44.5 | < 0.001 |
| QTcD in msec | 92.7 ± 26.1 | 65.2 ± 22.6 | 27.5 ± 19.6 | < 0.001 |
From admission to 24 hr, both QTD and QTcD decreased significantly in both groups I and II (Table 3). Following reperfusion (24 hr later), the QTD and QTcD of patients in group I were significantly shorter than those in group II (P = 0.005 and P = 0.003, respectively). Moreover, ∆ changes in both QTD and QTcD were significantly higher in group I compared with group II (37.6 ± 17.1 msec vs 11.3 ± 7.9 msec, P < 0.001 for the former and 43.6 ± 13.6 msec vs 11.4 ± 8.0 msec, P < 0.001 for the latter) (Table 3).
| Parameter | Group I, n = 120 patients | Group II, n = 120 patients | P value | ||||||||
| Before | After | ∆ | Before | After | ∆ | P1 | P2 | P3 | P4 | P5 | |
| Heart rate in beat/min | 81.0 ± 15.7 | 82.7 ± 16.4 | -1.7 ± 18.9 | 76.2 ± 16.3 | 78.2 ± 14.8 | -2.0 ± 14.9 | 0.34 | 0.14 | 0.02 | 0.02 | 0.87 |
| Maximum QT in msec | 411.7 ± 38.4 | 392.0 ± 44.1 | 19.7 ± 48.8 | 402.6 ± 46.9 | 405.3 ± 45.6 | -2.8 ± 44.3 | < 0.001 | 0.49 | 0.10 | 0.02 | < 0.001 |
| Minimum QT in msec | 320.2 ± 34.6 | 338.1 ± 39.0 | - 17.9 ± 34.4 | 330.6 ± 47.4 | 344.6 ± 48.0 | -14.0 ± 41.3 | < 0.001 | 0.001 | 0.06 | 0.25 | 0.48 |
| QTD in msec | 91.5 ± 20.6 | 53.9 ± 19.1 | 37.6 ± 17.1 | 72.0 ± 18.5 | 60.7 ± 18.1 | 11.3 ± 7.9 | < 0.001 | < 0.001 | < 0.001 | 0.005 | < 0.001 |
| Maximum QTc in msec | 474.3 ± 45.9 | 453.8 ± 38.1 | 20.6 ± 53.1 | 448.1 ± 34.1 | 458.4 ± 39.7 | -10.4 ± 35.8 | < 0.001 | 0.002 | < 0.001 | 0.35 | < 0.001 |
| Minimum QTc in msec | 369.9 ± 43.2 | 393.0 ± 32.1 | - 23.1 ± 51.7 | 367.1 ± 31.1 | 388.9 ± 40.3 | -21.8 ± 36.2 | < 0.001 | < 0.001 | 0.56 | 0.38 | 0.82 |
| QTcD in msec | 104.4 ± 22.1 | 60.8 ± 21.6 | 43.6 ± 13.6 | 80.9 ± 24.4 | 69.6 ± 22.8 | 11.4 ± 8.0 | < 0.001 | < 0.001 | < 0.001 | 0.003 | < 0.001 |
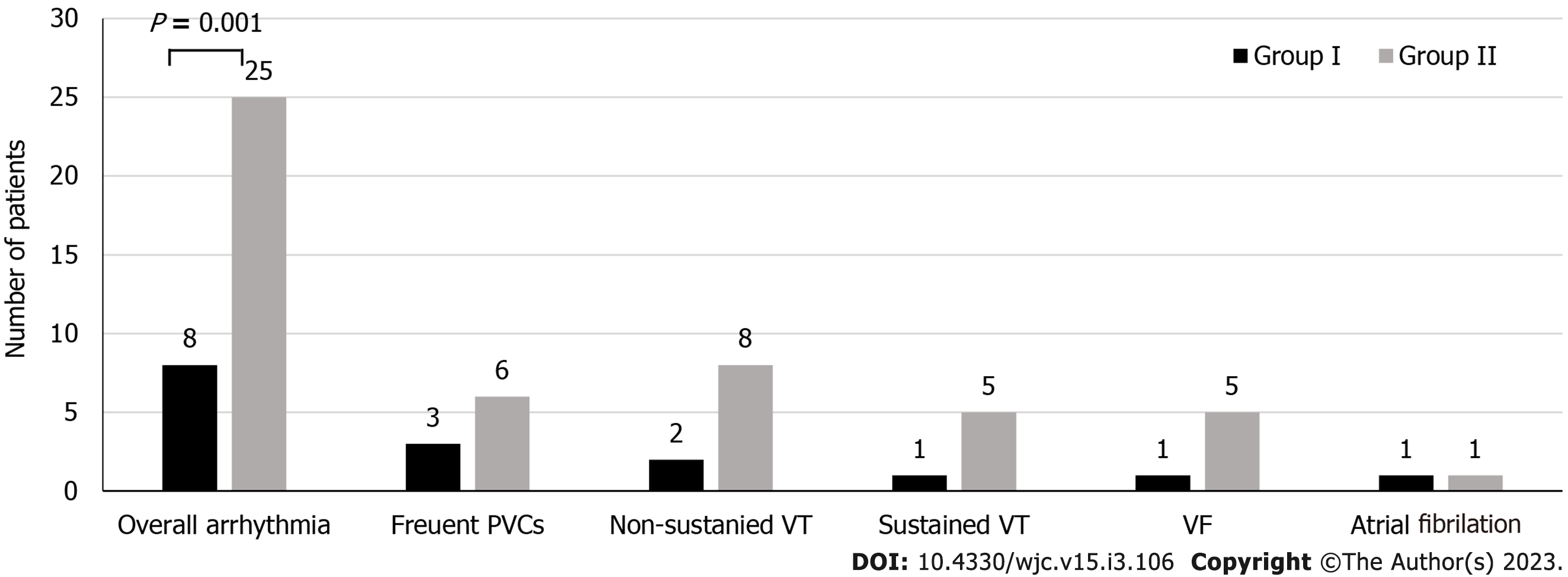
The incidence of in-hospital arrhythmia was significantly lower in group I (8 patients, 6.7%) than in group II (25 patients, 20.8%), P = 0.001. Different types of recorded arrhythmia observed in both groups are illustrated in Figure 1. Patients who did not experience in-hospital arrhythmia had significantly reduced QTD and QTcD values compared to those who did experience in-hospital arrhythmia regardless of the perfusion strategy used (Table 4). Furthermore, the ∆ changes of both QTD and QTcD were significantly higher in patients who did not experience in-hospital arrhythmia (25.9 ± 18.3 msec and 28.7 ± 20.1 msec, respectively; P = 0.003) than patients who experienced in-hospital arrhythmias (14.8 ± 18.9 msec and 19.8 ± 14.5 msec, respectively; P = 0.016) (Table 4).
| Parameter | In-hospital arrhythmia group, n = 33 patients | No in-hospital arrhythmia group, n = 207 patients | P value | ||||||||
| Before | After | ∆ | Before | After | ∆ | P1 | P2 | P3 | P4 | P5 | |
| QTD in msec | 82.1 ± 19.3 | 67.3 ± 22.7 | 14.8 ± 18.9 | 81.7 ± 22.3 | 55.8 ± 17.7 | 25.9 ± 18.3 | < 0.001 | < 0.001 | 0.91 | 0.001 | 0.003 |
| QTcD in msec | 94.0 ± 25.3 | 74.2 ± 24.9 | 19.8 ± 14.5 | 92.5 ± 26.2 | 63.7 ± 21.9 | 28.7 ± 20.1 | < 0.001 | < 0.001 | 0.75 | 0.03 | 0.02 |
It is well known that QTd has a prognostic role for stratifying MI patients who are at higher risk of arrhythmic events. In a recent large meta-analysis of 22 trials, an improved QTd after acute MI was associated with lower risk of associated serious arrhythmia. However, no prognostic role was found with respect to all-cause mortality or sudden cardiac death in such a patient population[12].
The current study provides further evidence supporting the beneficial impact of reperfusion therapy on decreasing both QTD and QTcD in the setting of STEMI. Moreover, to our knowledge, our study is the first to calculate QT and QTc intervals automatically using a software program that eliminates human bias of manual measurement. We showed that reperfusion therapy decreases QTD and QTcD in patients with STEMI regardless of reperfusion strategy. Also, our study demonstrated that PPCI had a more favorable effect on reducing QTD and QTcD (measured 24 hr after treatment) when compared to fibrinolytic therapy. Moreover, we showed that restoration of coronary reperfusion using PPCI had a greater impact in reducing the incidence of in-hospital arrhythmias than fibrinolytic therapy. In addition, QTD and QTcD were shorter in patients without in-hospital arrhythmia than in those with arrhythmia recorded during admission.
In the setting of acute coronary syndrome, evidence suggests that there are electrophysiological alterations in action potentials, causing repolarization dispersion between normal and ischemic fibers and between the epicardium and endocardium. This leads to repolarization delays in regions influenced by acute ischemia, thus causing QT and QTc prolongation[5,13-15]. The present study included STEMI patients with achievement of TIMI flow grade III in group I and successful fibrinolysis in group II. Establishing the patency of the infarct-related artery, either by fibrinolytic therapy or PPCI, could reduce regional myocardial ischemia and homogenize the ventricular action potential, thereby reducing the QTD and QTcD. This theory is supported by studies finding that TIMI flow grades II and III were associated with far lower QTD and QTcD values as compared to TIMI flow grades 0 and I[16,17]. Thus, the degree of QTD and QTcD reduction depends on the reperfusion status of the infarcted artery. The results of PPCI in STEMI patients are superior to fibrinolytic therapy with respect to reestablishing infarct-related artery patency. The present study supports this assumption, as our results revealed that PPCI more significantly reduced QTD and QTcD intervals than fibrinolytic therapy in STEMI patients.
The mechanism of QT prolongation and QTD in the setting of MI is attributed to the elevation in extracellular potassium level, acidosis, and anoxia. These conditions also cause reductions in membrane excitability, shortening of action potential duration, and prolongation of recovery of excitability following an action potential[18]. The prolonged QT and QTD have been linked to the occurrence of arrhythmia in patients with congenital long QT syndrome and with drug-induced torsades des pointes[19,20]. Therefore, MI associated with increased dispersion of cardiac repolarization could lead to the occurrence of arrhythmia[7]. Opening of the infarct-related artery results in perfusion of the infarcted area and consequently washing off of the excess extracellular potassium leading to correction of tissue anoxia and acidosis. This leads to improvement in membrane excitability and recovery of excitability following an action potential, ameliorating repolarization abnormalities and decreasing QTD. Consequently, the occurrence of arrhythmia is less likely. Our results support this mechanism, as the data presented here revealed that patients without in-hospital arrhythmia had shorter QTD and QTcD intervals with higher ∆ than those with arrhythmia.
Lopes et al[21] studied the effect of thrombolytic therapy on QTD in patients with STEMI, and showed that QTD was significantly shorter in patients with STEMI who underwent successful thrombolysis (Table 5). On the other hand, they found that QTD did not correlate with ventricular arrhythmia; however, QTD was higher in patients with ventricular arrhythmia than those without. This conclusion is undermined by the study design (retrospective) and the inclusion of patients with unsuccessful thrombolysis who had high post-procedure QTD. Furthermore, this study measured QT values manually, which introduces the possibility of measurement bias. In line with the present study, Ornek et al[22] and Mulay et al[23] not only found that thrombolytic therapy reduces QTD significantly in STEMI patients in the 1st wk of admission, but also that patients with ventricular arrhythmia had higher QTcD values than patients without arrhythmia (Table 5).
| Ref. | Study type | Study population | Time to evaluation | Reduction of QTD and QTcD | In-hospital arrhythmia | Remarks |
| Lopes et al[21], 2006 | Retrospective | Thrombolytic (n = 154) | 4 d | Sig. after 4 d | QTD not correlated with arrhythmia | CA after 48 h; Reduction in QTD is a predictor of coronary reperfusion |
| Ornek et al[22], 2014 | Prospective | Thrombolytic (n = 20) | 7 d | Sig. after 7 d | QTD correlated with arrhythmia | Use 24-h Holter monitor |
| Mulay et al[23], 2004 | Prospective | STEMI (n = 100) Normal (n = 100) | 24 hr On discharge | NA | Sig. high QTD in patients with ventricular arrhythmias compared to those without | Sig. higher QTD on admission, at 24 h, and at discharge than normal subjects |
| Pan et al[24], 2011 | Prospective | PPCI (n = 81) | 24 h | Sig. after 24 h | NA | QTcD change was an independent predictor of MACE at 1 yr |
| Hamza et al[25], 2014 | Retrospective | PPCI (n = 54) | 90 min 24 hr | Not sig after 90 min Sig. after 24 h | NA | |
| Oni Heris et al[26], 2014 | Prospective | Thrombolytic (n = 160) | 1 hr 4 d | Not sig. after 1 hr Not sig. after 4 d | NA | |
| Babapour et al[27], 2018 | Retrospective | PPCI (n = 77) | 24 h | Not sig. after 24 hr | NA | |
| Cavusoglu et al[28], 2001 | Prospective | PPCI (n = 21) Thrombolytic (n = 21) | 24 h | Sig. in PPCI group Sig. in thrombolytic group Sig. in PPCI compared with thrombolytic | NA | |
| George et al[29], 2015 | Prospective | PPCI (n = 25) Thrombolytic (n = 25) | 24 h | Sig. in PPCI group Not sig. in thrombolytic group Sig. in PPCI compared with thrombolytic | NA | |
| Valizadeh et al[30], 2020 | Prospective | PPCI (n = 70) Thrombolytic (n = 115) | 24 h | Sig. in PPCI group Not sig. in thrombolytic group Not sig. in PPCI compared with thrombolytic | QTD mean in patients with arrhythmia was reduced before and after treatment with a significant reduction after PPCI as compared to thrombolysis |
In concurrence with our study, Pan et al[24] demonstrated that QTcD measured before PPCI was significantly longer than 24 hr after PPCI administration. Furthermore, they showed that the absolute QTcD change after PPCI was an independent predictor of the development of major cardiovascular events at 1 year (Table 5). Hamza et al[25] reported that PPCI was effective in reducing QTc and QTD after 24 h, although the study showed no effect on these arrhythmogenic indices 90 min after successful revascularization with PPCI (Table 5). However, it should be emphasized that they did not monitor patients for the occurrence of arrhythmia.
In contrast to our results, other studies have shown that thrombolytic therapy decreased QTD over time, but without statistical significance. Studies have also shown a decrease in QTD 24 hr after PPCI treatment; however, this decline was also not significant[26,27] (Table 5). Oni Heris et al[26]’s study included patients with successful or unsuccessful thrombolysis who had high QTD following treatment, which would have affected the results of the QTD measured. Additionally, this study compared time points at 1 hr before thrombolytic therapy and 4 d later. Babapour et al[27]’s study was retrospective in design and included all patients with PPCI, irrespective of the final TIMI results. In this study, TIMI 0 and I had a higher value of QTD and QTcD than TIMI II and III, affecting the final results. Our prospective study included patients with successful fibrinolysis or PPCI with final TIMI flow grade III[17]. Moreover, our ECG parameters were computed automatically, thus reducing potential bias and variability.
Few studies have compared the effects of PPCI and fibrinolytic therapy on ventricular repolarization ECG parameters. However, previous attempts to explore the impact of these treatments on the incidence of in-hospital arrhythmia have been deficient. In agreement with our findings, Cavusoglu et al[28] showed that PPCI was associated with more significant decreases in QTD and QTcD as compared to thrombolytic therapy (Table 5). Similarly, George et al[29] found that PPCI was superior in reducing QTD and QTcD in patients with STEMI as compared to thrombolytic therapy. However, these reports included only a small number of patients, were single-center studies, measured ECG parameters manually, and did not observe patients for arrhythmia. On the other hand, Valizadeh et al[30] observed that no significant decreases were seen in QTD and QTcD values in the PPCI group compared to the thrombolytic group, but QTD values in the PPCI group showed a greater reduction after treatment (Table 5). Unlike ours, this was a single-center study and used PPCI or fibrinolytic drugs based on the patient's clinical status. This also raises the possibility of bias in patient assignment to either group, and obviously, PPCI improves survival and decreases complications whatever the patient clinical status. Moreover, this study included all patients who received thrombolysis whether successful or not, and who underwent PPCI regardless of the final TIMI flow. Furthermore, QT values were manually measured, again raising the possibility of bias and error, which the authors themselves stated as a limitation. Nonetheless, they found that mean QTD values in patients with arrhythmia were lower before and after treatment, with a significant reduction after PPCI group as compared to the thrombolytic group, similar to our results.
The present study indeed also has some limitations. Our sample size was relatively small, even though it was powered sufficiently to identify the pre-specified endpoints. Still, the findings need to be endorsed by further studies in larger cohorts. Additionally, various medications can affect the QT interval; however, these could not be standardized at the time of patient enrolment. Finally, long-term observation for arrhythmia development in these patients was not performed, and therefore our findings are only applicable to the acute phase of STEMI.
We demonstrated that reperfusion with PPCI or fibrinolytic therapy was effective in reducing QTD and QTcD in STEMI patients. Reperfusion with PPCI was associated with shorter QTD and QTcD than thrombolytic therapy 24 hr after reperfusion. Moreover, PPCI was associated with a lower incidence of in-hospital arrhythmia than fibrinolytic therapy. Additionally, patients with in-hospital arrhythmia had a higher QTD and QTcD than patients without arrhythmia. Therefore, QTD and QTcD measurements in STEMI patients are important arrhythmogenic parameters that respond to reperfusion therapy.
ST-elevation myocardial infarction (STEMI) increases QT dispersion (QTD) and corrected QT dispersion (QTcD), and is also associated with ventricular arrhythmia. Fibrinolytic therapy or primary percutaneous coronary intervention (PPCI) was used as the reperfusion strategy in acute STEMI patients.
Cardiac arrhythmia in the setting of acute myocardial infarction (MI) has serious impact on patient morbidity and mortality. Every effort should be made to prevent post-MI arrhythmia and to predict its occurrence as early as possible.
To compare the impact of revascularization with fibrinolysis or PPCI in STEMI patients on cardiac electrical stability, as indicated by QTD and QTcD measurements.
Two groups of patients were treated for acute STEMI; 1 group of patients were treated with fibrinolysis, and the other group of patients were treated with PPCI. QTD and QTcD were measured at baseline and at 24 hr following successful reperfusion. We compared these measures between the two groups and observed all patients for incidence of arrhythmia during hospital admission.
There were significant reductions in QTD and QTcD at 24 hr in both study groups. QTD and QTcD were found to be shorter in group I at 24 hr than in group II. Moreover, the incidence of in-hospital arrhythmia was significantly higher in group II as compared to group I.
In STEMI patients, both PPCI and fibrinolytic therapy effectively reduced QTD and QTcD, with a more significant reduction observed after PPCI. Furthermore, PPCI was associated with a lower incidence of in-hospital arrhythmia.
PPCI was superior to fibrinolytic therapy with respect to the electrical stability of the heart.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: European Society of Cardiology, ESC 291324.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Diez E, Argentina; Routray S, India S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Gheeraert PJ, De Buyzere ML, Taeymans YM, Gillebert TC, Henriques JP, De Backer G, De Bacquer D. Risk factors for primary ventricular fibrillation during acute myocardial infarction: a systematic review and meta-analysis. Eur Heart J. 2006;27:2499-2510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 81] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Shenthar J, Deora S, Rai M, Nanjappa Manjunath C. Prolonged Tpeak-end and Tpeak-end/QT ratio as predictors of malignant ventricular arrhythmias in the acute phase of ST-segment elevation myocardial infarction: a prospective case-control study. Heart Rhythm. 2015;12:484-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Yu Z, Chen Z, Wu Y, Chen R, Li M, Chen X, Qin S, Liang Y, Su Y, Ge J. Electrocardiographic parameters effectively predict ventricular tachycardia/fibrillation in acute phase and abnormal cardiac function in chronic phase of ST-segment elevation myocardial infarction. J Cardiovasc Electrophysiol. 2018;29:756-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Malik M, Batchvarov VN. Measurement, interpretation and clinical potential of QT dispersion. J Am Coll Cardiol. 2000;36:1749-1766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 408] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 5. | Parale GP, Adnaik AR, Kulkarni PM. Dynamics of QT dispersion in acute myocardial infarction. Indian Heart J. 2003;55:628-631. [PubMed] |
| 6. | Higham PD, Furniss SS, Campbell RW. QT dispersion and components of the QT interval in ischaemia and infarction. Br Heart J. 1995;73:32-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 205] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Aziz F, Doddi S, Alok A, Penupolu S, Singh V, Benz M, Abed M. QT dispersion as a predictor for arrhythmias in patients with acute ST elevation myocardial infarction. J Thorac Dis. 2010;2:86-88. [PubMed] |
| 8. | Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7073] [Cited by in RCA: 6650] [Article Influence: 950.0] [Reference Citation Analysis (0)] |
| 9. | Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018;72:2231-2264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1366] [Cited by in RCA: 2493] [Article Influence: 356.1] [Reference Citation Analysis (1)] |
| 10. | Pomés Iparraguirre H, Conti C, Grancelli H, Ohman EM, Calandrelli M, Volman S, Garber V. Prognostic value of clinical markers of reperfusion in patients with acute myocardial infarction treated by thrombolytic therapy. Am Heart J. 1997;134:631-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Ahnve S. Correction of the QT interval for heart rate: review of different formulas and the use of Bazett's formula in myocardial infarction. Am Heart J. 1985;109:568-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 237] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | Bazoukis G, Yeung C, Wui Hang Ho R, Varrias D, Papadatos S, Lee S, Ho Christien Li K, Sakellaropoulou A, Saplaouras A, Kitsoulis P, Vlachos K, Lampropoulos K, Thomopoulos C, Letsas KP, Liu T, Tse G. Association of QT dispersion with mortality and arrhythmic events-A meta-analysis of observational studies. J Arrhythm. 2020;36:105-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Perkiömäki JS, Koistinen MJ, Yli-Mäyry S, Huikuri HV. Dispersion of QT interval in patients with and without susceptibility to ventricular tachyarrhythmias after previous myocardial infarction. J Am Coll Cardiol. 1995;26:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 283] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 14. | Nash MP, Bradley CP, Paterson DJ. Imaging electrocardiographic dispersion of depolarization and repolarization during ischemia: simultaneous body surface and epicardial mapping. Circulation. 2003;107:2257-2263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Rautaharju PM, Gregg RE, Zhou SH, Startt-Selvester RH. Electrocardiographic estimates of regional action potential durations and repolarization time subintervals reveal ischemia-induced abnormalities in acute coronary syndrome not evident from global QT. J Electrocardiol. 2011;44:718-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Moreno FL, Villanueva T, Karagounis LA, Anderson JL. Reduction in QT interval dispersion by successful thrombolytic therapy in acute myocardial infarction. TEAM-2 Study Investigators. Circulation. 1994;90:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 162] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Nikiforos S, Hatzisavvas J, Pavlides G, Voudris V, Vassilikos VP, Manginas A, Hatzeioakim G, Foussas S, Iliodromitis EK, Hatseras D, Kremastinos DT, Cokkinos DV. QT-interval dispersion in acute myocardial infarction is only shortened by thrombolysis in myocardial infarction grade 2/3 reperfusion. Clin Cardiol. 2003;26:291-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Shaw RM, Rudy Y. Electrophysiologic effects of acute myocardial ischemia: a theoretical study of altered cell excitability and action potential duration. Cardiovasc Res. 1997;35:256-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 213] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Day CP, McComb JM, Campbell RW. QT dispersion: an indication of arrhythmia risk in patients with long QT intervals. Br Heart J. 1990;63:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 793] [Cited by in RCA: 788] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 20. | Shah RR. Drug-induced QT dispersion: does it predict the risk of torsade de pointes? J Electrocardiol. 2005;38:10-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 51] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Lopes NH, Grupi C, Dina CH, de Gois AF, Hajjar LA, Ayub B, Rochitte CE, Ramires JA, Hueb WA, Kalil R. [QT interval dispersion analysis in acute myocardial infarction patients: coronary reperfusion effect]. Arq Bras Cardiol. 2006;87:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 22. | Ornek E, Duran M, Ornek D, Demirçelik BM, Murat S, Kurtul A, Çiçekçioğlu H, Çetin M, Kahveci K, Doger C, Çetin Z. The effect of thrombolytic therapy on QT dispersion in acute myocardial infarction and its role in the prediction of reperfusion arrhythmias. Niger J Clin Pract. 2014;17:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Mulay DV, Quadri SM. QT dispersion and early arrhythmic risk in acute myocardial infarction. Indian Heart J. 2004;56:636-641. [PubMed] |
| 24. | Pan KL, Hsu JT, Chang ST, Chung CM, Chen MC. Prognostic value of QT dispersion change following primary percutaneous coronary intervention in acute ST elevation myocardial infarction. Int Heart J. 2011;52:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Hamza O, Bouzid A, Mouffok M, Azzouz A, Mokhtar OA, Bendaoud N, Saidane M, Latrèche S, Benkhedda S, Merad K. Evaluation of corrected QT and QT dispersion changes in acute ST elevation myocardial infarction after primary percutaneous coronary intervention. Arch Cardiovasc Dis. 2014;Suppl 6: 26-27. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Oni Heris S, Rahimi B, Faridaalaee G, Hajahmadi M, Sayyadi H, Naghipour B. QT Dispersion after Thrombolytic Therapy. Int Cardiovasc Res J. 2014;8:161-165. [PubMed] |
| 27. | Babapour B, Shahbazzadegan B, Khademi B. Effect of primary percutaneous coronary intervention on ventricular repolarization through evaluation of QT dispersion in patient with acute myocardial infarction. Int J of Community Med Public Health. 2018;5:506-510. [DOI] [Full Text] |
| 28. | Cavusoglu Y, Gorenek B, Timuralp B, Unalir A, Ata N, Melek M. Comparison of QT dispersion between primary coronary angioplasty and thrombolytic therapy for acute myocardial infarction. Isr Med Assoc J. 2001;3:333-337. [PubMed] |
| 29. | George KS, Waly HMF, Abdul Moteleb MT. Assessment of QT Dispersion in Patients with Acute STEMI Receiving Thrombolytic Versus those Performing Primary Percutaneous Coronary Intervention (PCI) Therapy. Med J of Cairo Univ. 2015;83:1023-1030. |
| 30. | Valizadeh A, Soltanabadi S, Koushafar S, Rezaee M, Jahankhah R. Comparison of QT dispersion in patients with ST elevation acute myocardial infarction (STEMI) before and after treatment by streptokinase versus primary percutaneous coronary intervention (PCI). BMC Cardiovasc Disord. 2020;20:493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |