Published online Feb 26, 2023. doi: 10.4330/wjc.v15.i2.45
Peer-review started: December 3, 2022
First decision: January 20, 2023
Revised: January 25, 2023
Accepted: February 15, 2023
Article in press: February 15, 2023
Published online: February 26, 2023
Processing time: 79 Days and 20.7 Hours
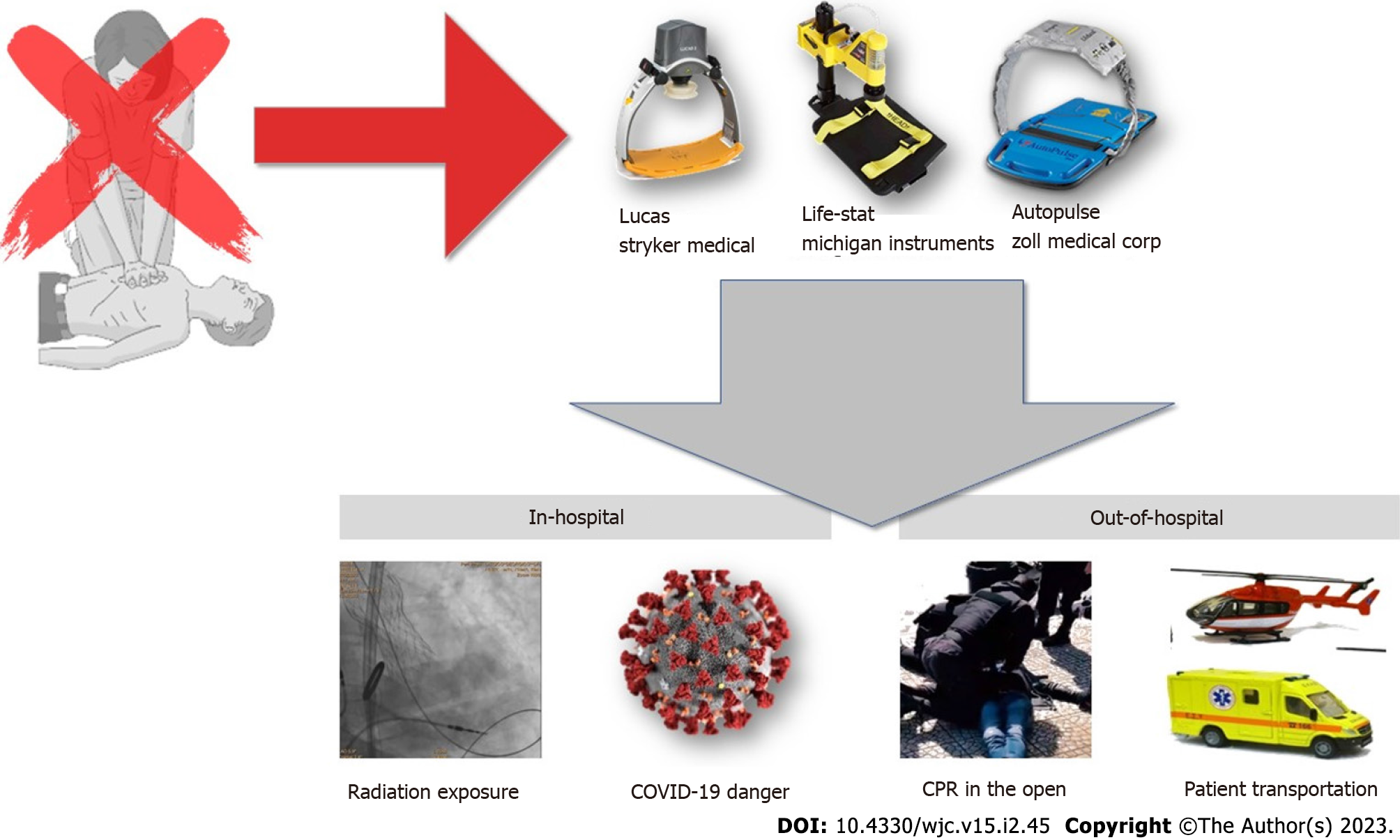
Mechanical automated compression devices are being used in cardiopulmonary resuscitation instead of manual, “hands-on”, rescuer-delivered chest compressions. The -theoretical- advantages include high-quality non-stop compressions, thus freeing the rescuer performing the compressions and additionally the ability of the rescuer to stand reasonably away from a potentially “hazardous” victim, or from hazardous and/or difficult resuscitation conditions. Such circumstances involve cardiopulmonary resuscitation (CPR) in the Cardiac Catheterization Laboratory, especially directly under the fluoroscopy panel, where radiation is well known to cause detrimental effects to the rescuer, and CPR during/after land or air transportation of cardiac arrest victims. Lastly, CPR in a coronavirus disease 2019 patient/ward, where the danger of contamination and further serious illness of the health provider is very existent. The scope of this review is to review and present literature and current guidelines regarding the use of mechanical compressions in these “hostile” and dangerous settings, while comparing them to manual compressions.
Core Tip: The use of automated compression devices in ‘hostile’ environments, both in in- and out-of- hospital cases of cardiac arrest, seems to be beneficial both regarding compressions’ quality but especially the rescuers’ safety. So far, while experimental data is extensive, real-life studies examining their use in non-friendly situations are still limited. Since high-quality cardiopulmonary resuscitation remains the key to a successful resuscitation, their use such difficult and “hostile” situations should be seriously taken into consideration. Noteworthy, such a use is indeed implied by guidelines.
- Citation: Latsios G, Leopoulou M, Synetos A, Karanasos A, Papanikolaou A, Bounas P, Stamatopoulou E, Toutouzas K, Tsioufis K. Cardiac arrest and cardiopulmonary resuscitation in “hostile” environments: Using automated compression devices to minimize the rescuers’ danger. World J Cardiol 2023; 15(2): 45-55
- URL: https://www.wjgnet.com/1949-8462/full/v15/i2/45.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i2.45
Cardiopulmonary resuscitation (CPR) is the pillar of cardiac arrest treatment. High numbers of people sustain cardiac arrest both inside and outside of the hospital every year[1] thus, making the need for high-quality CPR crucial, in order to save human lives.
The cornerstone of high-quality CPR is effective chest compressions (CC). The characteristics of great-quality CCs are proper rate, adequate depth, full chest recoil, and minimal interruptions[2]. However, during the highly demanding resuscitation setting optimal quality of CCs is not always achieved. Rescuer exhaustion is the main reason for suboptimal CCs, as compressions are extremely demanding and tiring for the providing rescuer. In a study of manual compressions, the vast majority of rescuers reported serious back discomfort, mostly related to the duration of CPR, while approximately 20% of the rescuers suffered back injury or reported a prolapsed-disk diagnosis[3].
Besides operator exhaustion, hostile settings related to cardiac arrest are often the reason for CCs of suboptimal quality. Those settings include but are not limited to, resuscitation in a moving ambulance during patient transportation, inside the computed tomography (CT) scanner, or in the cardiac Catheterization Laboratory (CathLab). Especially for the CathLab, it is not only difficult for the operator to perform high-quality CCs due to the existence of the equipment, but it is also very dangerous, due to the hazardous ionizing radiation.
Mechanical automated chest compression devices (ACDs) implement all the necessary qualifications to solve all the aforementioned problems and have been implemented in clinical practice. Many studies, reviews, and meta-analyses have contemplated the use of ACDs in the clinical setting of a cardiac arrest, presenting both the upsides of their use and the potential obstacles. ACDs can deliver high-quality compressions, of consistent rate and depth, lasting up to one hour when disconnected from their energy source[4,5].
There are mainly two device types of ACDs, based on the compressions’ delivery style (Figure 1). The first type is piston-driven (PD) (Lucas© Stryker Medical, United States, Life-Stat© Michigan Instruments, United States) –thus applying anteroposterior thrust on the sternum. A recent study showed that the use of a piston-driven ACD (which uses a suction cup) is associated with higher coronary perfusion pressure[6]. The second type of ACD uses a load-distribution band (LDB) (Autopulse© Zoll Medical Corp, United States) and distributes the force applied to the patients’ torso more evenly[7]. Both types have been studied in the settings of both the in-hospital cardiac arrest (IHCA) and the out-of-hospital-cardiac arrest (OHCA) and they seem to be more beneficial in the setting of IHCA[7]. A novel idea, however, is that they can be of great value in a 'non-friendly' setting of a cardiac arrest, either IHCA or OHCA. In this review, we present current data and literature regarding the implementation of ACDs in cardiac arrest in a ‘hostile’ environment.
The use of ACDs in the hospital environment (Figure 1) combines various advantages. The devices can be deployed fast, and they solve the problem of energy loss, as the in-hospital hospital-bed mattresses tend to absorb up to 40% of the force produced during chest compressions[8]. They are easier to use and considerably less invasive than the Extracorporeal Membrane Oxygenation that is used in cardiac arrest settings, and they additionally require easier training[9]. Furthermore, the infrastructure of the hospital environment is highly advanced, offering high-quality post-resuscitation care, a well-trained resuscitation team, very efficient airway management, and minimized response times; thus, in-hospital setting CPR, assisted by ACDs, can offer a superior, more organized peri-arrest care to patients. So far, data indicated that the use of ACDs in the IHCA setting can be beneficial when compared to manual cardiac compressions, although further data could elucidate more on the standing debate[7].
However, although the ACDs can offer a sustainable solution to the very important constant-high-quality-compressions problem, they can pose limitations. Patient safety has been studied, and patient injuries (such as rib fractures, liver lacerations, or vertebral body fractures) have sporadically been reported[9]. Furthermore, device failure has also been reported[10,11]. A learning curve required for the correct use and placement of the devices, with minimum interruptions of the ongoing manual compressions, has also been brought to attention[10]. The randomized COMPRESS-RCT study[12], although prematurely terminated due to unfavorable outcomes in the use of a certain ACD type (Lucas) in the hospital environment, did accentuate important aspects and limitations regarding the implementation of efficient ACD-study protocols. Hospital survival was low, while the identified problems where delays in the intra-arrest randomization, non-superior compressions quality in the Lucas arm, and low overall recruitment[12].
Radiation exposure: Despite the limitations arising from using ACDs in the hospital environment, data suggest that their use in special settings and non-friendly situations is beneficial and even suggested. More specifically, although improved techniques, equipment, and training led to a fall in cardiac arrest cases in the cardiac cath lab[13], prolonged CPR may still be required[13]. The presence of the equipment as well as the ionizing radiation constitute a ‘hostile’ environment. Radiation exposure during manual CCs is a major concern, as accumulated doses over time have been associated with multiple health hazards[14]. As a result, the protection of the rescuers from radiation should be a priority. The use of ACDs in the CathLab can substitute manual compressions, thus eliminating the need for extra personnel during the resuscitation process. Furthermore, ACDs can offer good-quality compressions during the ongoing catheterization process (i.e. primary PCI), as they are greatly translucent[15]. The Lucas device has been reported to allow free movement of the radiation detector and allow all views during catheterization, except for the straight anteroposterior[16]. The device compressions do not affect the interventions during catheterization, although minor interruptions for coronary stenting may be warranted[16]. Although the initial device deployment delay has been reported as a drawback, the time needed can be reduced to a median of seven seconds with proper staff training[17]. So far, the Lucas device has been mainly studied in the CathLab in the form of case reports. During PCI arrest, it has been shown that the device, when compared to manual CCs, has better outcomes in terms of both return of spontaneous circulation (ROSC) and survival rates at hospital discharge[18]. The blood pressure levels that the device can maintain during resuscitation are also of vital importance[19]. The device can also assist the resuscitation process as it can be used during the transportation of the patient to the cath lab. A study contemplated that better ROSC rates are achieved for patients transferred to the CathLab with ongoing mechanical compressions[20]. In the event of PCI, a Lucas case series argued that the device was beneficial for patients[16]; Autopulse case reports also argue that uninterrupted visualization during catheterization is achieved thus allowing all interventions[21,22]. On the other hand, a study stated that ongoing CPR upon arrival at the CathLab and continuous mechanical compressions for over 10-20 min in the CathLab were both predictive of poor outcomes[23]. Of interest, a recent study revealed that for patients undergoing PCI under mechanical compressions, mild hyperkalemia might be beneficial, identifying the potassium (KCl) concentration of 5.1 mmol/L to be the optimal cut-off, for the prediction of survival to hospital discharge[24].
The topic of ACD compressions inside the CT scanner has not been studied as extensively. So far, a case report of a pulmonary embolism that sustained cardiac arrest suggested that contrast-enhanced CT imaging with ongoing chest compressions is feasible after cardiac arrest[25]. Experimental data suggest that an ECG-triggered protocol allows almost artifact-free chest evaluation during mechanical compressions[26].
Coronavirus disease 2019 danger: CPR is a complex intervention, requiring extensive skills from quite a few knowledgeable healthcare providers. The risks of viral transmission through aerosol and droplet generation during CPR have not yet been fully identified, but a transmission can be detrimental to these valuable and scarce CPR team members[33]. On the other hand, patients with coronavirus disease 2019 (COVID-19) who require intubation and ventilation have extremely poor survival rates[27-29]. The best way to express this concept has already been written, and we also stand for[30]: This pandemic has changed the risk-benefit balance for CPR: from "there is no harm in trying" to "there is little benefit to the patient and potentially significant harm to staff".
During the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus pandemic, the advanced life support algorithm must be followed with extreme caution to personal protection, especially regarding personal protective equipment, airway management, and compressions, and an ACD should be used, as soon as the device is available[31-32]. The high contagiousness of the SARS-CoV-2 virus changed significantly every day clinical practice and the CPR process. Occupational exposure of healthcare and other personnel to all airborne transmitted pathogens is not by any means negligible but can be minimized through a high index of suspicion, preparedness, and appropriate protection[33].
Regarding changes and additions to the already existing OHCA protocol, it is suggested that cardic arrest recognition should be performed by searching for the absence of pulse and normal breathing while completely avoiding listening to or feeling breath sounds, by placing one's ear and cheek near the victim's mouth[31]. A cloth should also be placed on the unconscious victim's mouth during the resuscitation process. CPR should be performed only through chest compressions and quick and effective use of an AED is of vital importance without any additive risk to the resuscitation process. Hand sanitizing is an efficient alternative to soap-based hand washing, which is advised immediately after the process[31,34].
Regarding the IHCA CPR process, advanced airway management is mainly endotracheal intubation should be performed by the most trained and experienced physician, as the risk of cross-infection is high. The use of PPE is highly advised in the hospital setting, while participants in the CPR process should be trained on how to correctly handle, put on and safely remove all PPE equipment[31,34]. As the need for protection through PPE use may delay CPR initiation for patients with COVID-19, "donning/doffing" training can help minimize those delays. Regarding the algorithm, adjustments have been made to accommodate those newly surfaced needs; no CPR should commence without the use of PPE, and for shockable rhythms, up to three back-to-back shocks are allowed to restore the patient's rhythm. CPR should start only with chest compressions, while defibrillation for all shockable rhythms should be given with only minimal delays[31,32].
A mechanical compression device should be used as soon as it becomes available in any setting that allows their safe and efficient use, especially in the need for prolonged CPR[7,34]. The obvious advantage, besides the ones already discussed earlier, is the need for one less –COVID-19 exposed- person in the CPR team. Furthermore, this at-risk person would be the one the closest for the longest duration, to the SARS-CoV-2 infected victim. Therefore, automated chest compression devices have been proposed to be used during COVID-19 CPR[35,36]. When they are not available it was discussed to reduce the duration of the CPR cycles from two to one minute as the quality of chest compressions can deteriorate fast if the rescuer wears PPE[33,35,36].
The ACDs have been studied quite extensively in the setting of an OHCA (Figure). So far the results are mixed, as a study suggested that a load distribution band presents worse neurological outcomes and worse survival when compared to manual CCs; however, a meta-analysis concluded that ACDs are associated with better ROSC outcomes, provided that the staff applying them is sufficiently trained[37,38]. In the same meta-analysis, load-distribution devices outperformed piston-driven devices, a finding that may be associated with the necessary pause for application[38,39]. Interestingly, in another meta-analysis of survival to thirty days, it was found that survival to hospital admission or survival to discharge was comparable between the two arms (manual CCs and the Lucas device), although manual CPR proved superior to the Autopulse device; regarding patient safety, manual CCs were superior to the devices[7,40].
The OHCA setting is at its core the most challenging one. Compressions, of undetermined quality, are most often initiated by bystanders after significant delays. ADCs, brought by the rapid response EMS (emergency medical system e.g. ambulances or motorcycles) can offer continuous high-quality compressions, on the scene of a cardiac arrest, while defibrillation can take place simultaneously; in this way, quality is maintained at a high standard and the need for pauses is minimized[38]. However, in the randomized ASPIRE trial the deployment of the load-distribution device created a delay of 2.1 min to the first shock in ventricular fibrillation. As a result, the trial was prematurely terminated due to neurological and survival adverse outcomes[37]. In another randomized trial no difference regarding early survival between the manual and the mechanical arm was noted[41]. Prolongation of time to first shock was also prominent in CIRC and LINC trials[42,43]. Applicability factors, such as body weight, have also been highlighted and they may also cause delays[42,43]. In a recent study, the mechanical (Lucas) arm did not show added benefit regarding the ROSC rate, but its use did not lead to a higher risk of traumatic injury. The same study suggested that ACDs may be more useful in cases of delayed ambulance response times, or events happening in remote locations[44]. However, liver lacerations, occasionally associated with massive post-resuscitation hemorrhage, have been twice reported in the Lucas arm along with one Autopulse-associated tension pneumothorax that caused an air embolus[45]. The pre-hospital use of ACDs has been associated with worse neurological outcomes to hospital discharge when compared to manual compressions[46,47]. The LINC trial randomized SCA victims into manual compression vs Lucas-mediated compressions on the scene and showed no differences in either four-hour survival, six-month survival, or neurological outcomes between the two arms[43]. Similarly, in the PARAMEDIC trial (2:1 randomized trial of manual CCs: Lucas) no superiority of the device was proven in the primary outcome of thirty-day survival[48]. Furthermore, in the randomized CIRC trial (LDB device vs manual CPR) the two arms of the study displayed similar survival rates and neurological outcomes to discharge[42]. However, ACDs have been proposed to improve both pre-hospital and admission-to-hospital survival, especially when operated by a two-member paramedic team, the victim is young and the arrest takes place in a city center[5,7].
Cardiac arrests that are treated within Emergency Departments are considered cases of OHCA[49]. Patients that are treated for cardiac arrest in the Emergency Department are in the vast majority, patients that sustained a cardiac arrest outside of the hospital and were transferred with continuous compressions to the ED; thus, the resuscitation process can be quite challenging and may pose difficulties. Research has not definitively concluded regarding the effect of ACDs in ED departments. While a large randomized trial from Japan concluded that the mechanical arm of patients treated in the ED for an OHCA presented worse survival outcomes possibly due to deployment pauses[50], another randomized trial examined the effect of trained personnel operating LDB devices and concluded that better CPR quality is delivered to the patient, with shorter interruption times during deployment of the device[51].
However, the most challenging setting is during patient transportation. Cardiac arrest patients are sometimes transferred to the hospital with ongoing CPR, of doubtful quality[52] or they may arrest en route to the hospital. Rather conclusive data showed manual compressions during transfer to be ineffective for the patient and unsafe for the providing staff[53]. Various difficulties -including but not limited to uneven pavements and tight spaces and doorways during the victim transfer to the ambulance, sudden stops, accelerations, turns, and confined ambulance space, adversely affect delivered CPR quality[7]. Those are the exact settings in that an ACD may effectively assist the resuscitation process and favorably alter its course. An observational study found that ACDs use, contrary to manual CPR, minimizes compression interruptions during the extrication of a patient, except for the deployment pause[54]. Research has presented beneficial outcomes so far for the use of ACDs of both types during transportation, in terms of higher ROSC, survival to hospital admission, and quantitative CPR quality irrespective of transportation conditions or vehicle type[55,56]. However, regarding survival and outcomes, the heterogeneity of the included trials still poses a significant challenge to the generalization of the results. In every case, the vast majority of studies highlight the need for proper personnel training. The Danish cardiac arrest registry reported a marked reduction in mortality, when resuscitated OHCA victims were transferred to CathLab-capable tertiary centers rather than when being transferred to the nearest district hospital, irrespective of the overall distance the resuscitated victim had to travel by ambulance[57]. During the resuscitation process, an OHCA victim may need to undergo a large distance transportation by ambulance. ACDs may facilitate the process, thus having a place in the resuscitation process during transportation. Experimental data, using manikins, has concluded that the Lucas-2 device, in use by experienced hands, is a good alternative to manual compressions during a rescue-helicopter transfer and it complies -as a system- with all European Resuscitation Council (ERC) recommendations[58]. A randomized study, also using manikins, concluded that the Lucas system increased CPR quality and reduced pauses during helicopter rescue, but prolonged the time interval to first defibrillation[59]. Similarly, regarding transportation down stairwells and through tight spaces, experimental data proposing a new Lucas-2 system with shoulder strap fixation during non-supine stretcher transportation, allowed uninterrupted compressions, while yielding better chest compression fractions for the overall resuscitation period[60]. A randomized triple cross-over experimental study in an alpine setting revealed that Corpuls and Lucas-3 maintained the adequate quality of CPR during transportation and the piston was placed correctly even during challenging terrestrial transport[61]. Furthermore, a manikin-based study contemplated that while ambulance speed can affect manual compressions quality during transportation, devices of both types can resolve quality issues[62]. A similar experimental study showed good device performance during transport on a soft stretcher or gurney involving a stairwell, trips with a turntable ladder, a rescue basket, and an ambulance including loading/unloading of the patient, but underlined the need to check patient-device connection and stability[63]. All experimental studies highlight the need for real-world data. A retrospective observational study in Switzerland concluded that the implementation of mechanical compression devices in helicopter transportation can be beneficial, especially for non-trauma patients[64]. However, a recent German registry reported that mechanical devices are not associated with better survival rates when used during transport, but are associated with better survival in prolonged resuscitation. They are, however, associated with worse survival when a fibrinolytic was used; rescuer safety could be a sufficient reason for their use[65].
The use of mechanical compression devices has been used as a bridge to uncontrolled organ donation[66]. Although both ethical and clinical challenges are raised, the use of ACDs can reduce the time of warm ischemia[67]. During the insertion of extracorporeal CPR (cardiopulmonary bypass), the use of an ACD may be useful and it is applied with positive results, although data are still scarce[7]. In the case of refractory cardiac arrest, ethical dilemmas require very careful consideration[68].
Regarding current guidelines for in-hospital practice, the American Heart Association in 2010 stated that piston-driven or load-distributing band chest compression devices may be considered in patients undergoing PCI or CT scanning, for prolonged resuscitation (class IIa) or when manual resuscitation is challenging (class IIb)[69].
The ERC in its 2015 guidelines strongly recommended the use of ACDs in the cath lab during coronary interventions[70]. It is mandatory for trained personnel to implement the use of such devices, but there is insufficient evidence to support or refute their routine use in cardiac arrest[7].
In the latest (post COVID-19 pandemic) 2021 ERC guidelines the use of ACDs is considered if high-quality manual CPR is not practical or is dangerous for the provider[71].
The use of ACDs in 'hostile' environments, both in in- and out-of-hospital cases of cardiac arrest, seems to be beneficial both regarding compressions' quality and especially the rescuers' safety (Figure 1) So far, while experimental data is extensive, real-life studies examining their use in non-friendly situations are still limited. Since high-quality CPR remains the key to successful resuscitation, their use in such difficult and "hostile" situations should be seriously taken into consideration. Noteworthy, such use is indeed implied by guidelines.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Emergency medicine
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mohey NM, Egypt; Sharma D, India S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Gräsner JT, Herlitz J, Tjelmeland IBM, Wnent J, Masterson S, Lilja G, Bein B, Böttiger BW, Rosell-Ortiz F, Nolan JP, Bossaert L, Perkins GD. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation. 2021;161:61-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 395] [Article Influence: 98.8] [Reference Citation Analysis (0)] |
| 2. | Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, Gazmuri RJ, Travers AH, Rea T. Part 5: Adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S414-35. [RCA] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 625] [Article Influence: 69.4] [Reference Citation Analysis (0)] |
| 3. | Jones AY. Can cardiopulmonary resuscitation injure the back? Resuscitation. 2004;61:63-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Yuksen C, Prachanukool T, Aramvanitch K, Thongwichit N, Sawanyawisuth K, Sittichanbuncha Y. Is a mechanical-assist device better than manual chest compression? Open Access Emerg Med. 2017;9:63-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Kłosiewicz T, Puślecki M, Zalewski R, Sip M, Perek B. Impact of automatic chest compression devices in out-of-hospital cardiac arrest. J Thorac Dis. 2020;12:2220-2227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Mälberg J, Smekal D, Marchesi S, Lipcsey M, Rubertsson S. Suction cup on a piston-based chest compression device improves coronary perfusion pressure and cerebral oxygenation during experimental cardiopulmonary resuscitation. Resusc Plus. 2022;12:100311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Latsios G, Leopoulou M, Synetos A, Karanasos A, Melidi E, Toutouzas K, Tsioufis K. The role of automated compression devices in out-of- and in- hospital cardiac arrest. Can we spare rescuers’ hands? Emergency Care Journal, 2021; 17: 2. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Perkins GD, Kocierz L, Smith SC, McCulloch RA, Davies RP. Compression feedback devices over estimate chest compression depth when performed on a bed. Resuscitation. 2009;80:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 123] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 9. | Couper K, Yeung J, Nicholson T, Quinn T, Lall R, Perkins GD. Mechanical chest compression devices at in-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2016;103:24-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Spiro JR, White S, Quinn N, Gubran CJ, Ludman PF, Townend JN, Doshi SN. Automated cardiopulmonary resuscitation using a load-distributing band external cardiac support device for in-hospital cardiac arrest: a single centre experience of AutoPulse-CPR. Int J Cardiol. 2015;180:7-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Capone E, Durfey N. Severe Vertebral Body Fracture-Dislocation as a Result of Chest Compressions: A Case Report. J Emerg Med. 2022;63:e17-e21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Couper K, Quinn T, Booth K, Lall R, Devrell A, Orriss B, Regan S, Yeung J, Perkins GD. Mechanical versus manual chest compressions in the treatment of in-hospital cardiac arrest patients in a non-shockable rhythm: A multi-centre feasibility randomised controlled trial (COMPRESS-RCT). Resuscitation. 2021;158:228-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Latsios G, Mpompotis G, Tsioufis K, Toutouzas K, Skalidis E, Synetos A, Avramidis D, Tousoulis D. Advanced cardiopulmonary resuscitation (CPR) in the Catheterization Laboratory: Consensus document of the Working Groups of 1) Cardiopulmonary Resuscitation/Acute Cardiac Care and 2) Hemodynamic and Interventional Cardiology, Hellenic Cardiological Society. Hellenic J Cardiol. 2017;58:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Hirshfeld JW Jr, Ferrari VA, Bengel FM, Bergersen L, Chambers CE, Einstein AJ, Eisenberg MJ, Fogel MA, Gerber TC, Haines DE, Laskey WK, Limacher MC, Nichols KJ, Pryma DA, Raff GL, Rubin GD, Smith D, Stillman AE, Thomas SA, Tsai TT, Wagner LK, Wann LS. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in Cardiovascular Imaging: Best Practices for Safety and Effectiveness: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;71:e283-e351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 15. | Yadav K, Truong HT. Cardiac Arrest in the Catheterization Laboratory. Curr Cardiol Rev. 2018;14:115-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Wagner H, Terkelsen CJ, Friberg H, Harnek J, Kern K, Lassen JF, Olivecrona GK. Cardiac arrest in the catheterisation laboratory: a 5-year experience of using mechanical chest compressions to facilitate PCI during prolonged resuscitation efforts. Resuscitation. 2010;81:383-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 17. | Levy M, Yost D, Walker RG, Scheunemann E, Mendive SR. A quality improvement initiative to optimize use of a mechanical chest compression device within a high-performance CPR approach to out-of-hospital cardiac arrest resuscitation. Resuscitation. 2015;92:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Wagner H, Hardig BM, Rundgren M, Zughaft D, Harnek J, Götberg M, Olivecrona GK. Mechanical chest compressions in the coronary catheterization laboratory to facilitate coronary intervention and survival in patients requiring prolonged resuscitation efforts. Scand J Trauma Resusc Emerg Med. 2016;24:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Larsen AI, Hjørnevik AS, Ellingsen CL, Nilsen DW. Cardiac arrest with continuous mechanical chest compression during percutaneous coronary intervention. A report on the use of the LUCAS device. Resuscitation. 2007;75:454-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Venturini JM, Retzer E, Estrada JR, Friant J, Beiser D, Edelson D, Paul J, Blair J, Nathan S, Shah AP. Mechanical chest compressions improve rate of return of spontaneous circulation and allow for initiation of percutaneous circulatory support during cardiac arrest in the cardiac catheterization laboratory. Resuscitation. 2017;115:56-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Latsios G, Antonopoulos A, Vogiatzakis N, Melidi E, Koufakis N, Toutouzas K, Papaioannou S, Tsiamis E, Tousoulis D. Successful primary PCI during prolonged continuous cardiopulmonary resuscitation with an automated chest compression device (AutoPulse). Int J Cardiol. 2016;225:258-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Dallan LA, Vargas TT, Janella BL, Cade JR, Almeida B, Spadaro AG, Perin MA. Chest compressions using mechanical devices are more effective than manual compressions in cardiac arrest concomitant with emergency percutaneous coronary intervention. J Am Coll Cardiol. 2014;63:A1868. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 23. | Madsen Hardig B, Kern KB, Wagner H. Mechanical chest compressions for cardiac arrest in the cath-lab: when is it enough and who should go to extracorporeal cardio pulmonary resuscitation? BMC Cardiovasc Disord. 2019;19:134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Chyrchel M, Hałubiec P, Duchnevič O, Łazarczyk A, Okarski M, Januszek R, Rzeszutko Ł, Bartuś S, Surdacki A. Prognostic Factors in Patients with Sudden Cardiac Arrest and Acute Myocardial Infarction Undergoing Percutaneous Interventions with the LUCAS-2 System for Mechanical Cardiopulmonary Resuscitation. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 25. | Schubert EC, Kanz KG, Linsenmaier U, Bogner V, Wirth S, Angstwurm M. Use of computed tomography and mechanical CPR in cardiac arrest to confirm pulmonary embolism: a case study. CJEM. 2016;18:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Graef J, Leidel BA, Bressem KK, Vahldiek JL, Hamm B, Niehues SM. Computed Tomography Imaging in Simulated Ongoing Cardiopulmonary Resuscitation: No Need to Switch Off the Chest Compression Device during Image Acquisition. Diagnostics (Basel). 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 27. | Hayek SS, Brenner SK, Azam TU, Shadid HR, Anderson E, Berlin H, Pan M, Meloche C, Feroz R, O'Hayer P, Kaakati R, Bitar A, Padalia K, Perry D, Blakely P, Gupta S, Shaefi S, Srivastava A, Charytan DM, Bansal A, Mallappallil M, Melamed ML, Shehata AM, Sunderram J, Mathews KS, Sutherland AK, Nallamothu BK, Leaf DE; STOP-COVID Investigators. In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ. 2020;371:m3513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 28. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6231] [Cited by in RCA: 6657] [Article Influence: 1331.4] [Reference Citation Analysis (0)] |
| 29. | Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, Greninger AL, Pipavath S, Wurfel MM, Evans L, Kritek PA, West TE, Luks A, Gerbino A, Dale CR, Goldman JD, O'Mahony S, Mikacenic C. Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N Engl J Med. 2020;382:2012-2022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1819] [Cited by in RCA: 1862] [Article Influence: 372.4] [Reference Citation Analysis (0)] |
| 30. | Fritz Z, Perkins GD. Cardiopulmonary resuscitation after hospital admission with covid-19. BMJ. 2020;369:m1387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 31. | Latsios G, Synetos A, Mastrokostopoulos A, Vogiatzi G, Bounas P, Nikitas G, Papanikolaou A, Parisis C, Kanakakis I, Goudevenos J. CardioPulmonary Resuscitation in patients with suspected or confirmed Covid-19. A consensus of the Working group on CardioPulmonary Resuscitation of the Hellenic Society of Cardiology. Hellenic J Cardiol. 2021;62:24-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Chahar P, Marciniak D. Cardiopulmonary resuscitation in COVID-19 patients. Cleve Clin J Med. 2020;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Fragkou PC, Dimopoulou D, Latsios G, Koudounis P, Synetos A, Dimopoulou A, Tsioufis K, Papaevangelou V, Tsiodras S. Transmission of Infections during Cardiopulmonary Resuscitation. Clin Microbiol Rev. 2021;34:e0001821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 34. | Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, Koster RW, Wyllie J, Böttiger B; ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81:1219-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 933] [Cited by in RCA: 864] [Article Influence: 61.7] [Reference Citation Analysis (0)] |
| 35. | Malysz M, Dabrowski M, Böttiger BW, Smereka J, Kulak K, Szarpak A, Jaguszewski M, Filipiak KJ, Ladny JR, Ruetzler K, Szarpak L. Resuscitation of the patient with suspected/confirmed COVID-19 when wearing personal protective equipment: A randomized multicenter crossover simulation trial. Cardiol J. 2020;27:497-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 36. | Małysz M, Smereka J, Jaguszewski M, Dąbrowski M, Nadolny K, Ruetzler K, Ładny JR, Sterliński M, Filipiak KJ, Szarpak Ł. An optimal chest compression technique using personal protective equipment during resuscitation in the COVID-19 pandemic: a randomized crossover simulation study. Kardiol Pol. 2020;78:1254-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Hallstrom A, Rea TD, Sayre MR, Christenson J, Anton AR, Mosesso VN Jr, Van Ottingham L, Olsufka M, Pennington S, White LJ, Yahn S, Husar J, Morris MF, Cobb LA. Manual chest compression vs use of an automated chest compression device during resuscitation following out-of-hospital cardiac arrest: a randomized trial. JAMA. 2006;295:2620-2628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 268] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 38. | Westfall M, Krantz S, Mullin C, Kaufman C. Mechanical versus manual chest compressions in out-of-hospital cardiac arrest: a meta-analysis. Crit Care Med. 2013;41:1782-1789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 39. | Yost D, Phillips RH, Gonzales L, Lick CJ, Satterlee P, Levy M, Barger J, Dodson P, Poggi S, Wojcik K, Niskanen RA, Chapman FW. Assessment of CPR interruptions from transthoracic impedance during use of the LUCAS™ mechanical chest compression system. Resuscitation. 2012;83:961-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 40. | Khan SU, Lone AN, Talluri S, Khan MZ, Khan MU, Kaluski E. Efficacy and safety of mechanical versus manual compression in cardiac arrest - A Bayesian network meta-analysis. Resuscitation. 2018;130:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 41. | Jay R, Brennan P, Brenner, Overvad K, Olsen A, Tjønneland A, Boutron-Ruault MC, Clavel-Chapelon F, Fagherazzi, Katzke V, Kühn T, Boeing H, Bergmann MM, Steffen A, Naska A, Trichopoulou A, Trichopoulos D, Saieva C, Grioni S, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita HB, Peeters PH, Hjartåker A, Weiderpass E, Arriola L, Molina-Montes E, Duell EJ, Santiuste C, Alonso de la Torre R, Barricarte Gurrea A, Stocks T, Johansson M, Ljungberg B, Wareham N, Khaw KT, Travis RC, Cross AJ, Murphy N, Riboli E, Scelo G. Alcohol consumption and the risk of renal cancers in the European Prospective Investigation into Cancer and Nutrition (EPIC). Wozniak MB, Brennan P, Brenner DR, Overvad K, Olsen A, Tjønneland A, Boutron-Ruault MC, Clavel-Chapelon F, Fagherazzi G, Katzke V, Kühn T, Boeing H, Bergmann MM, Steffen A, Naska A, Trichopoulou A, Trichopoulos D, Saieva C, Grioni S, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita HB, Peeters PH, Hjartåker A, Weiderpass E, Arriola L, Molina-Montes E, Duell EJ, Santiuste C, Alonso de la Torre R, Barricarte Gurrea A, Stocks T, Johansson M, Ljungberg B, Wareham N, Khaw KT, Travis RC, Cross AJ, Murphy N, Riboli E, Scelo G.Int J Cancer. 2015 Oct 15;137(8):1953-66. [Epub 2015 Apr 28]. doi: 10.1002/ijc.29559. Urol Oncol. 2017;35:117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 42. | Wik L, Olsen JA, Persse D, Sterz F, Lozano M Jr, Brouwer MA, Westfall M, Souders CM, Malzer R, van Grunsven PM, Travis DT, Whitehead A, Herken UR, Lerner EB. Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial. Resuscitation. 2014;85:741-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 226] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 43. | Rubertsson S, Lindgren E, Smekal D, Östlund O, Silfverstolpe J, Lichtveld RA, Boomars R, Ahlstedt B, Skoog G, Kastberg R, Halliwell D, Box M, Herlitz J, Karlsten R. Mechanical chest compressions and simultaneous defibrillation vs conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest: the LINC randomized trial. JAMA. 2014;311:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 303] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 44. | Saleem S, Sonkin R, Sagy I, Strugo R, Jaffe E, Drescher M, Shiber S. Traumatic Injuries Following Mechanical versus Manual Chest Compression. Open Access Emerg Med. 2022;14:557-562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 45. | Koster RW, Beenen LF, van der Boom EB, Spijkerboer AM, Tepaske R, van der Wal AC, Beesems SG, Tijssen JG. Safety of mechanical chest compression devices AutoPulse and LUCAS in cardiac arrest: a randomized clinical trial for non-inferiority. Eur Heart J. 2017;38:3006-3013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 46. | Buckler DG, Burke RV, Naim MY, MacPherson A, Bradley RN, Abella BS, Rossano JW; CARES Surveillance Group. Association of Mechanical Cardiopulmonary Resuscitation Device Use With Cardiac Arrest Outcomes: A Population-Based Study Using the CARES Registry (Cardiac Arrest Registry to Enhance Survival). Circulation. 2016;134:2131-2133. [PubMed] [DOI] [Full Text] |
| 47. | Youngquist ST, Ockerse P, Hartsell S, Stratford C, Taillac P. Mechanical chest compression devices are associated with poor neurological survival in a statewide registry: A propensity score analysis. Resuscitation. 2016;106:102-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 48. | Perkins GD, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, Lamb SE, Slowther AM, Woollard M, Carson A, Smyth M, Whitfield R, Williams A, Pocock H, Black JJ, Wright J, Han K, Gates S; PARAMEDIC trial collaborators. Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet. 2015;385:947-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 334] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 49. | Poole K, Couper K, Smyth MA, Yeung J, Perkins GD. Mechanical CPR: Who? Crit Care. 2018;22:140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 50. | Hayashida K, Tagami T, Fukuda T, Suzuki M, Yonemoto N, Kondo Y, Ogasawara T, Sakurai A, Tahara Y, Nagao K, Yaguchi A, Morimura N; SOS‐KANTO 2012 Study Group. Mechanical Cardiopulmonary Resuscitation and Hospital Survival Among Adult Patients With Nontraumatic Out-of-Hospital Cardiac Arrest Attending the Emergency Department: A Prospective, Multicenter, Observational Study in Japan (SOS-KANTO [Survey of Survivors after Out-of-Hospital Cardiac Arrest in Kanto Area] 2012 Study). J Am Heart Assoc. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 51. | Ong ME, Quah JL, Annathurai A, Noor NM, Koh ZX, Tan KB, Pothiawala S, Poh AH, Loy CK, Fook-Chong S. Improving the quality of cardiopulmonary resuscitation by training dedicated cardiac arrest teams incorporating a mechanical load-distributing device at the emergency department. Resuscitation. 2013;84:508-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 52. | Russi CS, Myers LA, Kolb LJ, Lohse CM, Hess EP, White RD. A Comparison of Chest Compression Quality Delivered During On-Scene and Ground Transport Cardiopulmonary Resuscitation. West J Emerg Med. 2016;17:634-639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 53. | Wik L, Kramer-Johansen J, Myklebust H, Sørebø H, Svensson L, Fellows B, Steen PA. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1002] [Cited by in RCA: 938] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 54. | Lyon RM, Crawford A, Crookston C, Short S, Clegg GR. The combined use of mechanical CPR and a carry sheet to maintain quality resuscitation in out-of-hospital cardiac arrest patients during extrication and transport. Resuscitation. 2015;93:102-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 55. | Ong ME, Mackey KE, Zhang ZC, Tanaka H, Ma MH, Swor R, Shin SD. Mechanical CPR devices compared to manual CPR during out-of-hospital cardiac arrest and ambulance transport: a systematic review. Scand J Trauma Resusc Emerg Med. 2012;20:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 56. | Hock Ong ME, Ornato JP, Edwards DP, Dhindsa HS, Best AM, Ines CS, Hickey S, Clark B, Williams DC, Powell RG, Overton JL, Peberdy MA. Use of an automated, load-distributing band chest compression device for out-of-hospital cardiac arrest resuscitation. J Am Med Assoc. 2006;295:2629-2637. [RCA] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 143] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 57. | Tranberg T, Lippert FK, Christensen EF, Stengaard C, Hjort J, Lassen JF, Petersen F, Jensen JS, Bäck C, Jensen LO, Ravkilde J, Bøtker HE, Terkelsen CJ. Distance to invasive heart centre, performance of acute coronary angiography, and angioplasty and associated outcome in out-of-hospital cardiac arrest: a nationwide study. Eur Heart J. 2017;38:1645-1652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 79] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 58. | Gässler H, Kümmerle S, Ventzke MM, Lampl L, Helm M. Mechanical chest compression: an alternative in helicopter emergency medical services? Intern Emerg Med. 2015;10:715-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 59. | Putzer G, Brugger H, Strapazzon G, Paal P. Does a higher ROSC-rate with mechanical CPR lead to better survival in helicopter rescue? Resuscitation. 2014;85:e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 60. | Chen CB, Chen KF, Chien CY, Kuo CW, Goh ZNL, Seak CK, Seak JC, Seak CJ; SPOT Consortium. Shoulder strap fixation of LUCAS-2 to facilitate continuous CPR during non-supine (stair) stretcher transport of OHCAs patients. Sci Rep. 2021;11:9858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 61. | Alexander E, Katharina T, Verena F, Jürgen G, Maximilian N, Calvin K, Andreas S, Wolfgang S, Harald H, Dominik R. Comparison of different mechanical chest compression devices in the alpine rescue setting: a randomized triple crossover experiment. Scand J Trauma Resusc Emerg Med. 2021;29:84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 62. | Kamauzaman THT, Ngu JTH, Arithra A, Noh AYM, Siti-Azrin AH, Nor J. Simulation study on quality of CPR between manual chest compression and mechanical chest compression devices performed in ambulance. Med J Malaysia. 2021;76:171-176. [DOI] [Full Text] |
| 63. | Jörgens M, Königer J, Kanz KG, Birkholz T, Hübner H, Prückner S, Zwissler B, Trentzsch H. Testing mechanical chest compression devices of different design for their suitability for prehospital patient transport - a simulator-based study. BMC Emerg Med. 2021;21:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 64. | Pietsch U, Reiser D, Wenzel V, Knapp J, Tissi M, Theiler L, Rauch S, Meuli L, Albrecht R. Mechanical chest compression devices in the helicopter emergency medical service in Switzerland. Scand J Trauma Resusc Emerg Med. 2020;28:71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 65. | Gässler H, Kurka L, Rauch S, Seewald S, Kulla M, Fischer M. Mechanical chest compression devices under special circumstances. Resuscitation. 2022;179:183-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 66. | Ortega-Deballon I, Hornby L, Shemie SD. Protocols for uncontrolled donation after circulatory death: a systematic review of international guidelines, practices and transplant outcomes. Crit Care. 2015;19:268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 67. | Manara AR, Murphy PG, O'Callaghan G. Donation after circulatory death. Br J Anaesth. 2012;108 Suppl 1:i108-i121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 200] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 68. | Dalle Ave AL, Shaw DM, Gardiner D. Extracorporeal membrane oxygenation (ECMO) assisted cardiopulmonary resuscitation or uncontrolled donation after the circulatory determination of death following out-of-hospital refractory cardiac arrest-An ethical analysis of an unresolved clinical dilemma. Resuscitation. 2016;108:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 69. | Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, Samson RA, Kattwinkel J, Berg RA, Bhanji F, Cave DM, Jauch EC, Kudenchuk PJ, Neumar RW, Peberdy MA, Perlman JM, Sinz E, Travers AH, Berg MD, Billi JE, Eigel B, Hickey RW, Kleinman ME, Link MS, Morrison LJ, O'Connor RE, Shuster M, Callaway CW, Cucchiara B, Ferguson JD, Rea TD, Vanden Hoek TL. Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S640-S656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 570] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 70. | Lott C, Truhlář A, Alfonzo A, Barelli A, González-Salvado V, Hinkelbein J, Nolan JP, Paal P, Perkins GD, Thies KC, Yeung J, Zideman DA, Soar J; ERC Special Circumstances Writing Group Collaborators. Corrigendum to "European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances" [Resuscitation 161 (2021) 152-219]. Resuscitation. 2021;167:91-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 71. | Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, Lott C, Olasveengen T, Paal P, Pellis T, Perkins GD, Sandroni C, Nolan JP. Corrigendum to "European Resuscitation Council Guidelines 2021: Adult Advanced Life Support" [Resuscitation 161 (2021) 115-151]. Resuscitation. 2021;167:105-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |