Published online Dec 26, 2023. doi: 10.4330/wjc.v15.i12.649
Peer-review started: August 17, 2023
First decision: September 29, 2023
Revised: October 13, 2023
Accepted: November 13, 2023
Article in press: November 13, 2023
Published online: December 26, 2023
Processing time: 129 Days and 20.7 Hours
Isolated single coronary artery is a rare congenital anomaly. R-I subtype single coronary artery is even rarer. In this subtype, a very large right coronary artery extends in the coronary sulcus to the anterior base of the heart where it produces the left anterior descending coronary artery. Currently, only a few case reports are available in the literature for this anomaly.
Here, we report the case of a 62-year-old woman who presented to the cardiology clinic with decreased exercise tolerance and poor blood pressure control. The patient underwent coronary angiography (CAG) and emission computed tomography (ECT). CAG images revealed a single gigantic right coronary artery (R-I type) arising from the right coronary sinus with branches supplying the left coronary territory. The ECT results confirmed myocardial ischemia at the location of the absent left coronary artery. The ECT findings confirmed that ischemia was consistent with the vascular loss location in CAG images. In such anomalies, there is a compensatory widening of the coronary artery lumen. Medical treatment was administered, and the patient was discharged.
Isolated single coronary arteries are associated with ischemia and potentially fatal acute coronary events. Hence, controlling risk factors is critical.
Core Tip: We present the rare case of an elderly woman with an isolated single right coronary artery (R-I subtype) detected by coronary angiography and myocardial ischemia confirmed by emission computed tomography. Since such an anomaly may be fatal in these patients, providing appropriate medical treatment promptly has a positive effect on their prognosis.
- Citation: Zhou YP, Wang LL, Qiu YG, Huang SW. R-I subtype single right coronary artery with congenital absence of left coronary system: A case report. World J Cardiol 2023; 15(12): 649-654
- URL: https://www.wjgnet.com/1949-8462/full/v15/i12/649.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i12.649
An isolated single coronary artery is a rare congenital anomaly in which only one coronary artery arises from the aortic trunk and supplies the entire heart via a single coronary ostium[1]. Such an anomaly occurs in approximately 0.024%-0.044% of the population[2]. The R-I subtype single coronary artery is even rarer, with a reported incidence of 0.0008%[3]. In the R-I variant, a single large right coronary artery (RCA) extends to the anterior base of the heart and produces the left anterior descending coronary artery, which supplies blood flow to the left side of the heart.
According to our literature review, a single RCA is exceedingly rare, and only a few cases have been reported. Saglam et al[4] described a 72- year- old woman with a single coronary artery anomaly who was admitted with atypical chest pain and may be a new subtype of the Lipton R-I subtype. Siddiqui et al[5] presented a single RCA arising from the right sinus of Valsalva in the absence of an equivalent left coronary artery system branches and associated mitral valve prolapse. Yoldaş et al[6] reported an extremely rare case of a 14-mo-old girl who was diagnosed with a single RCA, a coronary artery fistula communicating with the right ventricle, and congenital absence of a left coronary artery. In these reports, coronary angiography (CAG) and multidetector computed tomography CAG findings were shared. However, we did not find any case reports that further verified the presence of myocardial ischemia. Herein, we presented the case of a 62-year-old woman with an R-I subtype single coronary artery and verified that myocardial ischemia was consistent with the area of vascular loss observed in emission computed tomography (ECT) images.
A 62-year-old female with many cardiovascular risk factors such as diabetes, hyperlipidemia, and hypertension presented to our cardiology clinic with decreased exercise tolerance and poor blood pressure (BP) control.
The patient reported that the symptoms began 2 wk before presentation.
In addition to the cardiovascular risk factors mentioned above, the patient’s history of past illnesses was not significantly different.
The patient denied having a history of decreased tolerance to exercise. However, within her family, her father has a history of hypertension.
On physical examination, the vital signs were as follows: body temperature of 37.3 °C; heart rate of 92 beats per min; BP of 151/86 mmHg; and body mass index of 23.4 kg/m2. Dyspnea, heart murmurs, and other signs of heart failure were not observed.
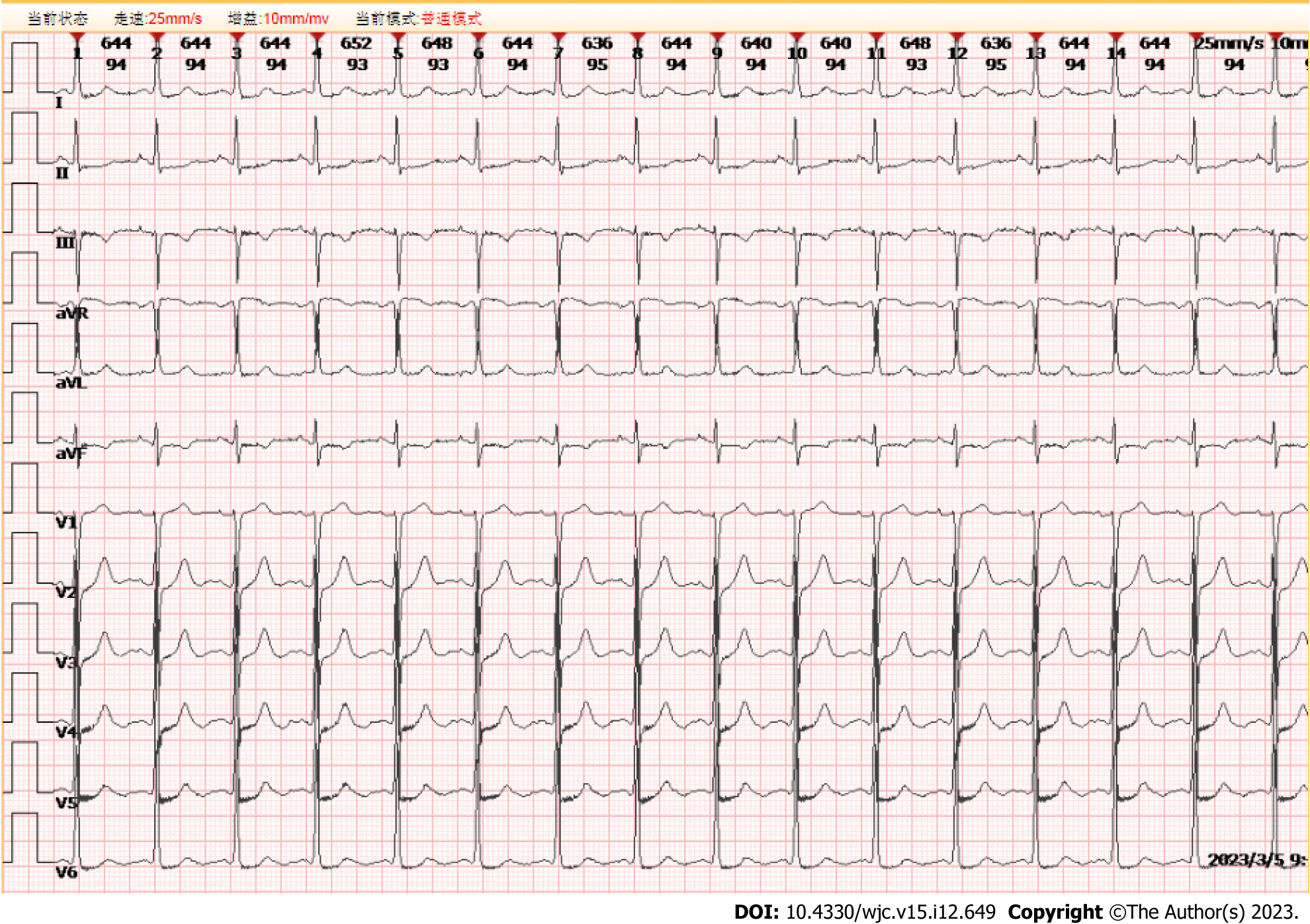
Cardiac troponin I levels were negative. The lipid profile revealed low-density lipoprotein, high-density lipoprotein, and total cholesterol levels of 3.16, 1.19, and 4.96 mmol/L, respectively. Fasting blood glucose was 9.49 mmol/L, and 2 h after a meal the blood glucose level rose to 22.54 mmol/L. Glycosylated hemoglobin A1c was 7.51%. Electrocardiography showed a normal sinus rhythm with ST-T wave slight depressions in leads I, II, III, aVF, and V4-V6 (Figure 1). The echocardiography of the heart revealed no regional wall motion abnormalities and good left ventricular systolic function.
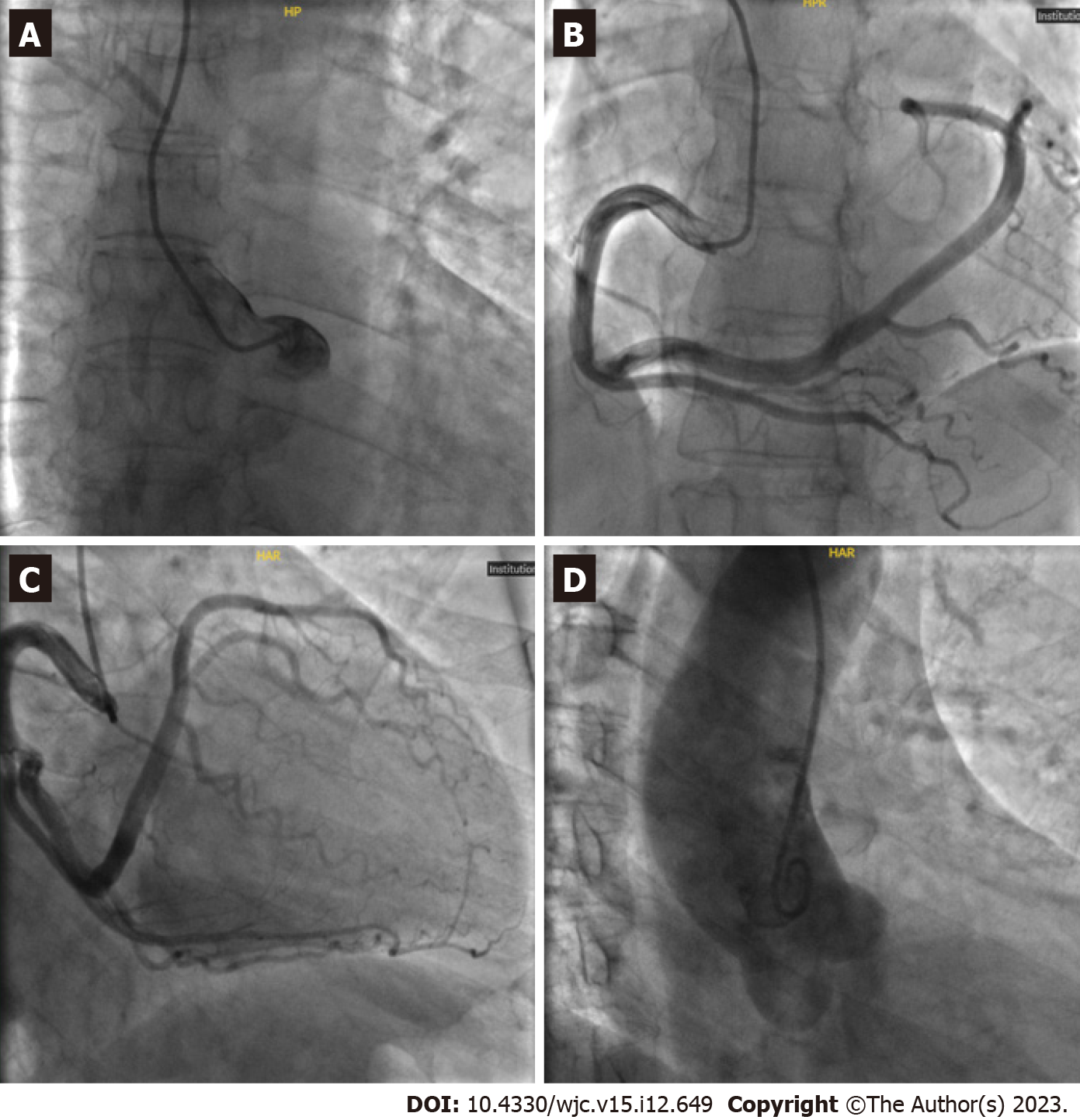
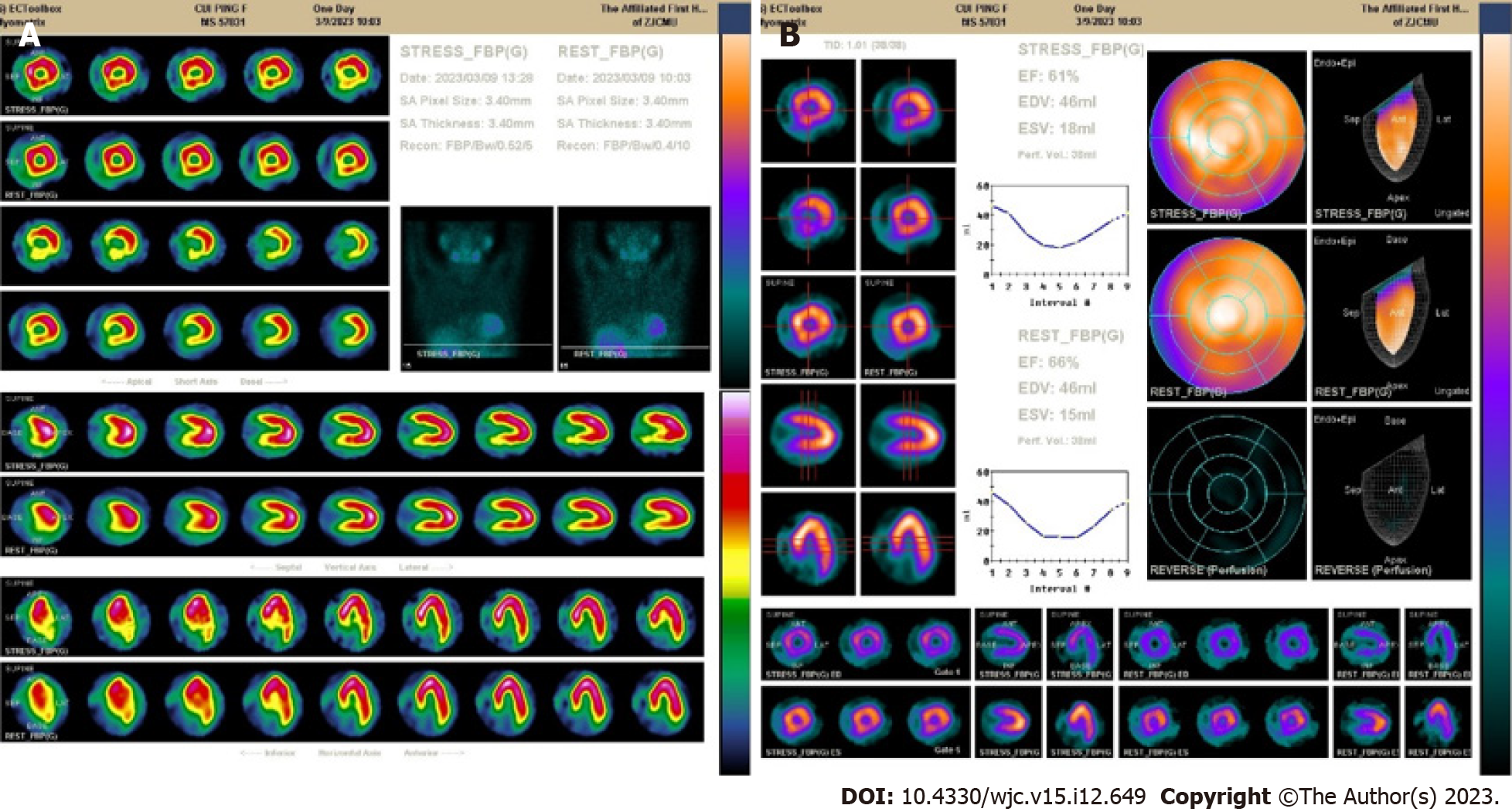
During CAG, selective cannulation of the left coronary artery (LCA) was not possible, and nonselective injection revealed the absence of a coronary artery arising from the left coronary sinus. Aortography showed the absence of the LCA, with no other vessels arising from the left or non-coronary cusps. We could not locate the left anterior descending artery or left circumflex artery (Figure 2, Videos 1, 2, 3 and 4). After selective injection into the right coronary sinus, a single ostium was visualized (Figure 2B). The RCA is a large vessel without significant atheromatous occlusive stenosis. The RCA passed within the right coronary sulcus before continuing through the crux of the heart to the left part of the coronary sulcus and terminating anteriorly in a small vessel supplying the territory of the left anterior descending coronary artery (Figure 2C). The ECT results showed that the inferior wall basal segment, inferior lateral wall basal segment, inferior septal wall middle segment, and basal segment of the left ventricle had a small-to-medium range of moderate myocardial blood flow perfusion reduction, considering the presence of myocardial ischemia (Figure 3A). Overall, left ventricular systolic function was normal without abnormal wall motion. However, the resting left ventricular ejection fraction value of the left ventricle was normal, and the load left ventricular ejection fraction value did not increase, indicating a decrease in the left ventricular systolic reserve function (Figure 3B).
Combined with the patient’s previous medical history and the CAG and ECT imaging findings, the final diagnosis was a single RCA of the R-I type without significant coronary atherosclerosis. Myocardial ischemia was consistent with the area of vascular loss.
The patient was managed with a β blocker, angiotensin receptor enkephalin enzyme inhibitor, nitrate for hypertension, statin for hyperlipidemia, biguanides, α-glucosidase inhibitor, and sulfonylurea for diabetes. Since the patient had high risk factors such as hypertension, diabetes, and hyperlipidemia with a single RCA, we administered aspirin (100 mg once daily) for the primary prevention of coronary heart disease and trimetazidine (35 mg twice daily) to improve myocardial hypoxia. The patient was discharged on postoperative day 3, with blood glucose and blood pressure controlled smoothly, and the symptoms disappeared.
At the last follow-up (6 mo postoperatively), the patient felt better with no recurrence of symptoms.
The presence of a right single coronary artery with congenital absence of the LCA (type R-I, the anomaly in the present case) is the least common type of single coronary artery, with a reported incidence of 0.0008%[3]. R-I subtype single RCA with congenital absence of left coronary system has been reported only a few times. The first reported case of a single RCA was described in 1867[7]. In a 31-year angiographic study by Villa et al[8], which examined the incidence of congenital coronary artery abnormalities in adults, only one R-I subtype single coronary artery was found in 13500 coronary angiography cases. Even though Desmet et al[9] examined 50000 coronary angiographies and Lipton et al[10] examined 4382 coronary angiographies, neither of them reported any cases of R-I type single coronary artery.
R-I subtype single coronary artery typically presents with a benign clinical course of disease, and the diagnosis is usually an incidental finding on noninvasive imaging. Invasive CAG can be used to diagnose symptomatic patients. Upadhyaya et al[11] presented the case of a young male patient with non-ST-elevated myocardial infarction. The patient was found to have a single coronary artery by employing invasive CAG. The few cases of R-I subtype detected by arteriography and autopsy have a co-compensatory mechanism of an enlarged aortic opening of regional citrate anticoagulation and an enormous dilation of the blood vessel itself with a sharp increase in lumen diameter, which can allow for perfusion of the entire heart through a single blood vessel[12,13].
In our case, because the patient had decreased exercise tolerance and many risk factors, she underwent CAG directly, which confirmed a single, gigantic, and hyperdominant RCA arising from the right coronary sinus with branches supplying the left coronary territory. However, this discovery was accidental. With the development of minimally invasive cardiac surgery, the number of clinically significant incidental findings detected using computed tomography has increased to 18.7%[14]. The patient was discharged on postoperative day 3 without having to undergo diagnostic computed tomography angiography. This is a limitation of the present study.
The main purpose of ECT is to observe myocardial blood perfusion and metabolism, and it is usually employed to diagnose patients with myocardial ischemia and coronary heart disease. To further confirm the presence of myocardial ischemia and the relationship between ischemia and the coronary artery-deficient area of the heart, the patient underwent ECT. The results of ECT showed that the RCA was insufficient for perfusion of the entire heart, whether at rest or after an increased cardiac load. We observed ischemia in the myocardium, where blood vessels were absent. In patients with a single coronary artery, the effect of coronary artery stenosis or occlusion may be catastrophic. Therefore, active preventive treatment is important for improving patient prognosis.
CAG revealed a congenital vascular anomaly. The presence of myocardial ischemia was confirmed by ECT. Through a literature search, we found that this is the first case report of a patient with a single RCA R-I subtype who underwent ECT to verify myocardial ischemia. Although we discovered this abnormality serendipitously in our clinical practice, acute coronary events can be fatal in these patients. Therefore, once this variant is identified, active treatment and control of risk factors are necessary to improve patient prognosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: El-Serafy AS, Egypt; Sef D, United Kingdom; Batta A, India S-Editor: Liu JH L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Smith JC. Review of single coronary artery with report of 2 cases. Circulation. 1950;1:1168-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 134] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 2. | Passman RS, Ferrari VA, Holland GA, Herling IM, Kolansky DM. Single coronary artery: an angiographic and MRI case report. Cathet Cardiovasc Diagn. 1997;40:177-178. [PubMed] [DOI] [Full Text] |
| 3. | Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21:28-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1278] [Cited by in RCA: 1361] [Article Influence: 38.9] [Reference Citation Analysis (1)] |
| 4. | Saglam M, Dogan D, Sahin S, Turkkan C, Kula O. Single right coronary artery with absence of the left main coronary artery, left anterior descending artery, and circumflex artery. Echocardiography. 2017;34:1401-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Siddiqui SM, Kesava Rao RC, Kaza S, Padma Kumar EA. Computed tomography coronary angiography diagnosis of single right coronary artery with congenital absence of left coronary artery system equivalents. Indian J Radiol Imaging. 2016;26:198-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Yoldaş T, Beyazal M, Örün UA. Single right coronary artery with right ventricular fistula and congenital absence of left coronary artery: an extremely rare combination. Cardiol Young. 2019;29:1402-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Kettner M, Mall G, Bratzke H. Single coronary artery: a fatal R-I type. Forensic Sci Med Pathol. 2013;9:214-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Barriales Villa R, Morís C, López Muñiz A, Hernández LC, San Román L, Barriales Alvarez V, Testa A, de la Hera J, Sanmartín JC, Cortina A. Adult congenital anomalies of the coronary arteries described over 31 years of angiographic studies in the Asturias Principality: main angiographic and clinical characteristics. Rev Esp Cardiol. 2001;54:269-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Desmet W, Vanhaecke J, Vrolix M, Van de Werf F, Piessens J, Willems J, de Geest H. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J. 1992;13:1637-1640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 197] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Lipton MJ, Barry WH, Obrez I, Silverman JF, Wexler L. Isolated single coronary artery: diagnosis, angiographic classification, and clinical significance. Radiology. 1979;130:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 340] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Upadhyaya SGN, Mughal LH, Connolly D, Lip G. Single right coronary artery with congenital absence of left coronary system. BMJ Case Rep. 2018;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Hartmann M, Verhorst PM, von Birgelen C. Isolated "superdominant" single coronary artery: a particularly rare coronary anomaly. Heart. 2007;93:687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Koksal A, Canyigit M, Akgoz A, Kaya D, Dincer H, Akhan O. Extremely rare R-I subtype coronary artery anomaly and accompanying incomplete myocardial bridging on the left anterior descending artery in a symptomatic patient: multidetector computed tomography and coronary angiography findings. Acta Radiol. 2009;50:760-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Sef D, Birdi I. Clinically significant incidental findings during preoperative computed tomography of patients undergoing cardiac surgery. Interact Cardiovasc Thorac Surg. 2020;31:629-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |