Published online Oct 26, 2023. doi: 10.4330/wjc.v15.i10.531
Peer-review started: June 7, 2023
First decision: July 4, 2023
Revised: July 23, 2023
Accepted: August 3, 2023
Article in press: August 3, 2023
Published online: October 26, 2023
Processing time: 139 Days and 4.3 Hours
Cardiac arrest is a leading cause of mortality in America and has increased in the incidence of cases over the last several years. Cardiopulmonary resuscitation (CPR) increases survival outcomes in cases of cardiac arrest; however, healthcare workers often do not perform CPR within recommended guidelines. Real-time audiovisual feedback (RTAVF) devices improve the quality of CPR performed. This systematic review and meta-analysis aims to compare the effect of RTAVF-assisted CPR with conventional CPR and to evaluate whether the use of these devices improved outcomes in both in-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA) patients.
To identify the effect of RTAVF-assisted CPR on patient outcomes and CPR quality with in- and OHCA.
We searched PubMed, SCOPUS, the Cochrane Library, and EMBASE from inception to July 27, 2020, for studies comparing patient outcomes and/or CPR quality metrics between RTAVF-assisted CPR and conventional CPR in cases of IHCA or OHCA. The primary outcomes of interest were return of spontaneous circulation (ROSC) and survival to hospital discharge (SHD), with secondary outcomes of chest compression rate and chest compression depth. The methodological quality of the included studies was assessed using the Newcastle-Ottawa scale and Cochrane Collaboration’s “risk of bias” tool. Data was analyzed using R statistical software 4.2.0. results were statistically significant if P < 0.05.
Thirteen studies (n = 17600) were included. Patients were on average 69 ± 17.5 years old, with 7022 (39.8%) female patients. Overall pooled ROSC in patients in this study was 37% (95% confidence interval = 23%-54%). RTAVF-assisted CPR significantly improved ROSC, both overall [risk ratio (RR) 1.17 (1.001-1.362); P = 0.048] and in cases of IHCA [RR 1.36 (1.06-1.80); P = 0.002]. There was no significant improvement in ROSC for OHCA (RR 1.04; 0.91-1.19; P = 0.47). No significant effect was seen in SHD [RR 1.04 (0.91-1.19); P = 0.47] or chest compression rate [standardized mean difference (SMD) -2.1; (-4.6-0.5)]; P = 0.09]. A significant improvement was seen in chest compression depth [SMD 1.6; (0.02-3.1); P = 0.047].
RTAVF-assisted CPR increases ROSC in cases of IHCA and chest compression depth but has no significant effect on ROSC in cases of OHCA, SHD, or chest compression rate.
Core Tip: Real-time audiovisual feedback (RTAVF) devices have been shown to significantly improve cardiopulmonary resuscitation (CPR) quality in manikin/simulation studies. Despite this improvement, previous reviews have not seen a translation into improvement in patient outcomes. This systematic review and meta-analysis is the largest one to-date conducted on this topic, including 13 studies and 17600 patients. We found that the use of RTAVF devices significantly improves CPR quality metrics of chest compression rate and depth. Contrary to prior literature, we found that usage significantly increases return of spontaneous circulation in cases of in-hospital cardiac arrest but does not improve survival to hospital discharge.
- Citation: Sood N, Sangari A, Goyal A, Sun C, Horinek M, Hauger JA, Perry L. Do cardiopulmonary resuscitation real-time audiovisual feedback devices improve patient outcomes? A systematic review and meta-analysis. World J Cardiol 2023; 15(10): 531-541
- URL: https://www.wjgnet.com/1949-8462/full/v15/i10/531.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i10.531
Nearly 356000 out-of-hospital cardiac arrest (OHCA) cases and 292200 in-hospital cardiac arrest (IHCA) cases occur annually in the United States, making cardiac arrest one of the leading causes of natural death in America[1-3]. In addition, the incidence of cardiac arrest cases has increased over the last twenty years, but little progress has been made in improving survival to hospital discharge (SHD) and functional status including neurological and cardiovascular outcomes[2,4]. Consequently, cardiac arrest places a significant burden on public health and society and remains important to research and manage effectively[5,6].
High quality cardiopulmonary resuscitation (CPR) increases survival outcomes in cases of cardiac arrest[7-14]. The International Liaison Committee on Resuscitation guidelines specifically emphasize the quality of manual chest compression, including proper hand position, hands off time, compression rate, and compression depth[15]. However, the quality of CPR performed by healthcare workers (HCWs) often does not meet recommended guidelines, with the average rate of chest compressions and compression depth being lower than recommended[16-25].
Real-time audiovisual feedback (RTAVF) devices have enabled improvement in consistency and quality of CPR both inside and outside the hospital[26,27]. The American Heart Association (AHA) and the International Liaison Committee on Resuscitation have recommended the use of RTAVF devices for CPR training[28-30]. Previous systematic reviews and meta-analyses examining the effect of RTAVF devices during cardiac arrest cases concluded that RTAVF-assisted CPR resulted in closer adherence to CPR guidelines but not improved patient outcomes[31,32]. However, these studies focused on simulation manikin studies, including only three human trials. This systematic review and meta-analysis aims to compare the effect of RTAVF-assisted CPR with conventional CPR and to evaluate whether the use of these devices improved outcomes in both in-hospital and OHCA patients.
Database searches were performed by two independent authors in PubMed, SCOPUS, the Cochrane Library, and EMBASE with individualized search strategies developed for each database (Supplementary Table 1). The search included all studies from the establishment of the database to July 27, 2020 without language, methodology, or document filters. References cited in relevant reviews and included studies were also examined. The current systematic review and meta-analysis was constructed in accordance with the PRISMA 2009 guidelines.
Studies were included if HCWs were performing CPR using RTAVF devices, where HCWs were defined as anyone with medical training including physicians, nurses, paramedics, emergency medical services, physician assistants, and medical residents. Studies must compare RTAVF-assisted CPR with CPR performed without any device or disabled audiovisual feedback features on cardiac arrest patients, and complete data must be available with a minimum of two metrics reported with measures of central tendency and variability. Language was restricted to English. Simulation studies, animal studies, case reports, conference abstracts, reviews, trial protocols, and studies with incomplete or missing data were excluded.
Abstracts of studies were reviewed for relevance by two independent authors. Abstracts with common agreement between reviewers were identified for further review of the full manuscript. Disagreements regarding the inclusion or exclusion of any studies were independently resolved by a third author. Data was extracted from articles selected for inclusion in the present study. Primary outcomes of interest were patient outcomes: return of spontaneous circulation (ROSC) and SHD. Secondary outcomes of interest were CPR quality metrics: chest compression rate and chest compression depth. Mean values and standard deviations were extracted from studies. Methodological quality was reviewed utilizing the Newcastle-Ottawa Quality Assessment scale for cohort studies and using the Cochrane Collaboration’s “risk of bias” tool for randomized controlled trials (RCT)[33,34]. Methodological quality was assessed by two independent authors with disagreements resolved by a third author.
Data was analyzed using R statistical software 4.2.0. Random-effects models were used[35,36]. When values were presented as interquartile range or range or median, they were converted into mean and standard deviation for analysis using the methodology presented in Wan et al[37] 2014. Pooled risk ratio (RR) or standardized mean difference (SMD) was calculated for binary and continuous metrics respectively[38-40]. Heterogeneity was assessed using I2[41,42]. Publication bias was assessed using funnel plots and Egger’s tests. Results were statistically significant if P < 0.05.
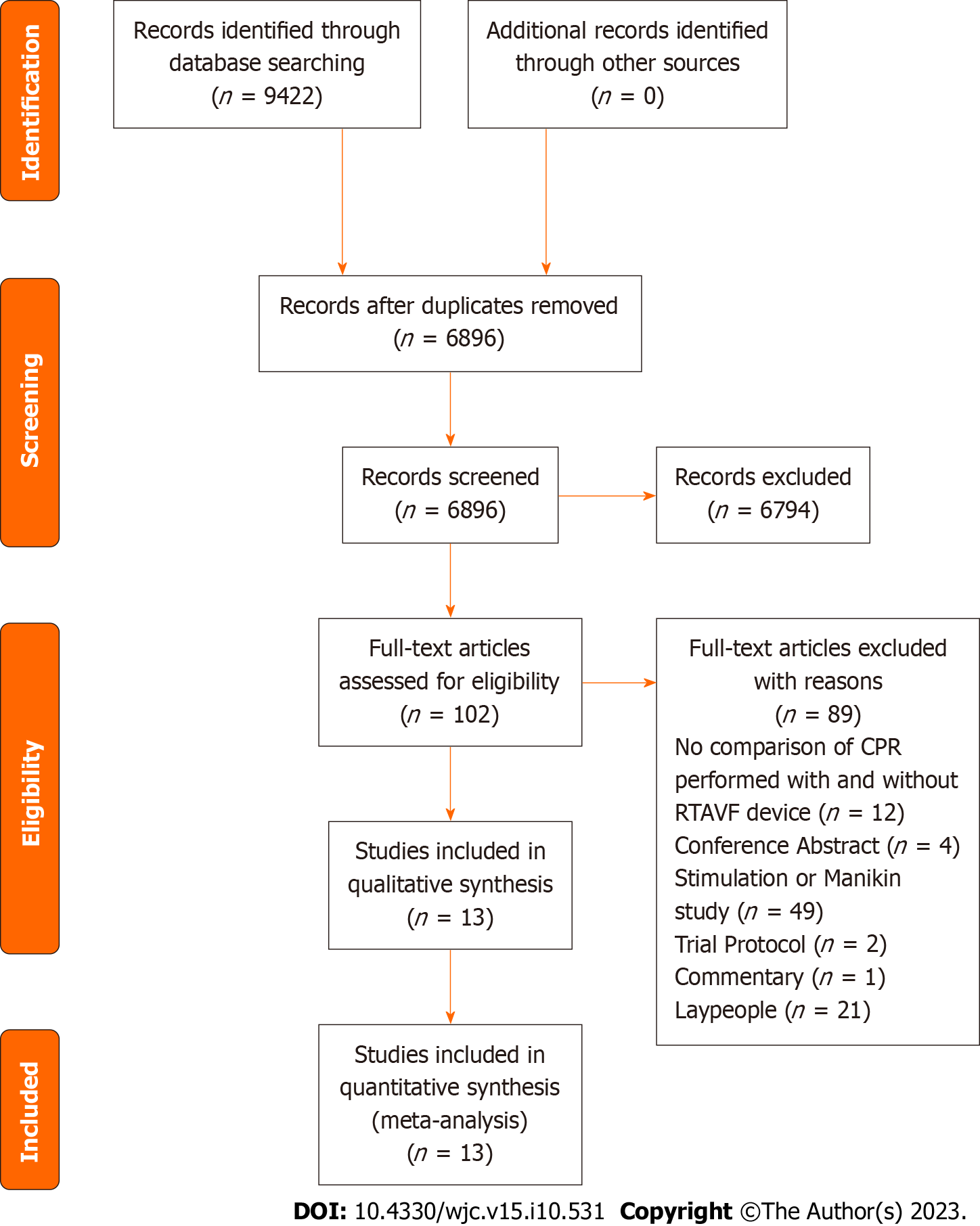
A PRISMA flow diagram is shown in Figure 1. The systematic search of articles identified 9422 results. 102 full-text articles were identified as potentially relevant after title and abstract screening. Thirteen studies were included after full-text review (Figure 1)[8,26,27,43-52]. Thirteen studies reported data on ROSC and ten reported data on SHD. Important characteristics for each study are summarized in Table 1.
| Ref. | Region | Enrollment year | n | Female | ROSC | Setting | Study type |
| Abella et al[26], 2007 | United States | 2002-2005 | 156 | 71 | 43% | IHCA, adult patients | Prospective cohort |
| Goharani et al[45], 2019 | Iran | 2015 | 900 | 546 | 55% | IHCA, adult patients | RCT |
| Hostler et al[46], 2011 | United States, Canada | 2007-2009 | 1587 | 1000 | 45% | OHCA, adult (> 20 yr) | RCT |
| Kramer-Johansen J et al[27], 2006 | London, Norway, Sweden | 2002-2003 | 284 | 106 | 19% | OHCA, adult | Non-randomized controlled trial |
| Lakomek et al[47], 2020 | Germany | 2016 | 196 | 112 | 54% | OHCA, adult | Non-randomized controlled trial |
| Vahedian-Azimi et al[52], 2020 | Iran | 2013-2014 | 22 | 10 | 27% | IHCA, adult | RCT |
| Vahedian-Azimi et al[51], 2016 | Iran | 2014 | 80 | 49 | 54% | IHCA, adult (≥ 18 yr) | RCT |
| Couper et al[43], 2015 | England | 2009-2013 | 400 | 182 | 40% | IHCA, adult (≥ 18 yr) | Prospective cohort |
| BoBrow et al[8], 2013 | Arizona | 2008-2011 | 484 | 162 | 23% | OHCA, adult (≥ 18 years) | Prospective cohort |
| Crowe et al[44], 2015 | Arizona | 2010-2013 | 101 | 27 | 42% | OHCA/IHCA, adult | Prospective before-after |
| Sutton et al[50], 2014 | Pennsylvania | 2011-2013 | 8 | 2 | 50% | IHCA, children (1-8 yr) | Prospective cohort |
| Lukas et al[48], 2012 | Germany | 2007-2011 | 638 | 184 | 50% | OHCA, adults (> 18 yr) | Retrospective Matched-pair analysis |
| Park et al[49], 2018 | South Korea | 2013-2016 | 12670 | 4571 | 9% | OHCA, > 15 yr | Before-after |
A total number of 17600 participants from 13 studies were included for analysis. Patients were on average 69 ± 17.5 years old, with 7022 (39.8%) female patients. All studies were published between the years 2006 and 2020. Six studied the influence of RTAVF devices in OHCA, while six studied their influence in IHCA. One examined both OHCA and IHCA (Table 1)[44]. All studies examined adult populations, with Park et al[49] 2018 examining patients greater than 15 years old.
Risk of bias was assessed in all 13 studies. Of the studies included, four were RCTs[45,46,51,52]. Using Cochrane’s Risk of Bias tool, the risk of bias was assessed to be low risk in three RCTs and medium risk in one RCT (Supplementary Table 2). Using the Newcastle-Ottawa Scale, the risk of bias was assessed to be low in eight studies and medium in one study (Supplementary Table 3). Egger’s test found no evidence of publication bias in any outcomes of interest (Supplementary Figure 1).
Pooled ROSC was 37% (95% confidence interval (CI) = 23%-54%) (Supplementary Figure 2A). Park et al[49] 2018 was identified as a potential outlier using leave-one-out sensitivity analysis with the lowest survival rate of 9%. Visual inspection of the associated funnel plot found no clear asymmetry (Supplementary Figure 2B).
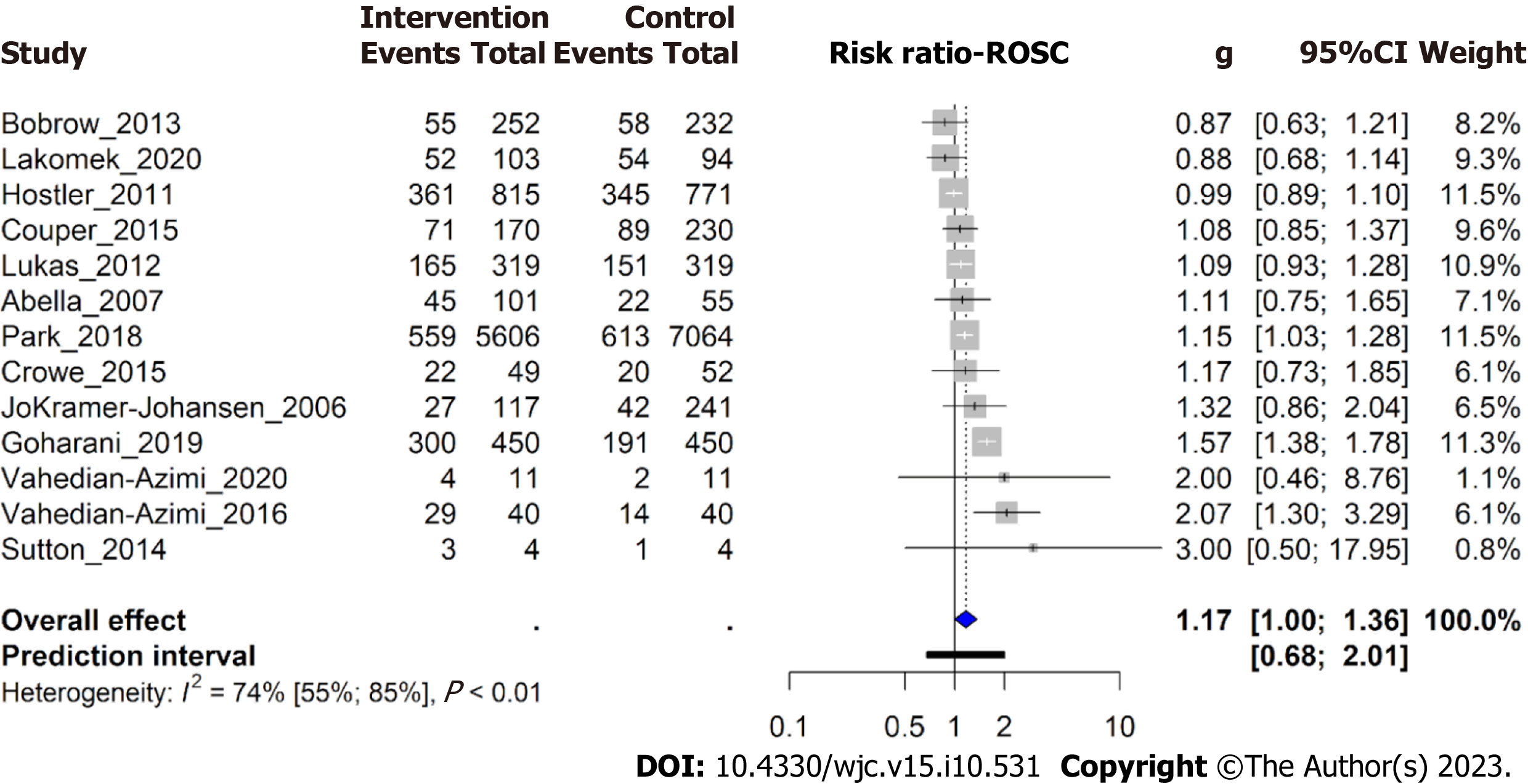
Thirteen trials reported ROSC as an outcome of interest (n = 17600). ROSC occurred in 1693 patients (21.0%) in the RTAVF-assisted CPR group and 1602 patients (16.8%) in the conventional CPR group. All studies included data on ROSC in both the RTAVF-assisted CPR group and the conventional CPR group. Using a random-effects model, patients in the RTAVF group were significantly more likely to achieve ROSC than the conventional CPR group (RR 1.17; 95%CI = 1.001-1.362; P = 0.048) (Figure 2).
Subgroup analysis revealed that the location of cardiac arrest was significantly correlated with patient outcomes (P value for interaction = 0.02) (Supplementary Figure 3). ROSC in the setting of IHCA was significantly improved in the RTAVF group (RR 1.36; 1.06-1.80; P = 0.002). However, ROSC in the setting of OHCA was not significantly different between the two groups (RR 1.04; 0.91-1.19; P = 0.47).
Potential causes of heterogeneity in ROSC were explored, with subgroup analysis on study type comparing RCTs with non-RCTs, and region comparing studies within Europe, Middle East/Asia, and North America (Supplementary Figure
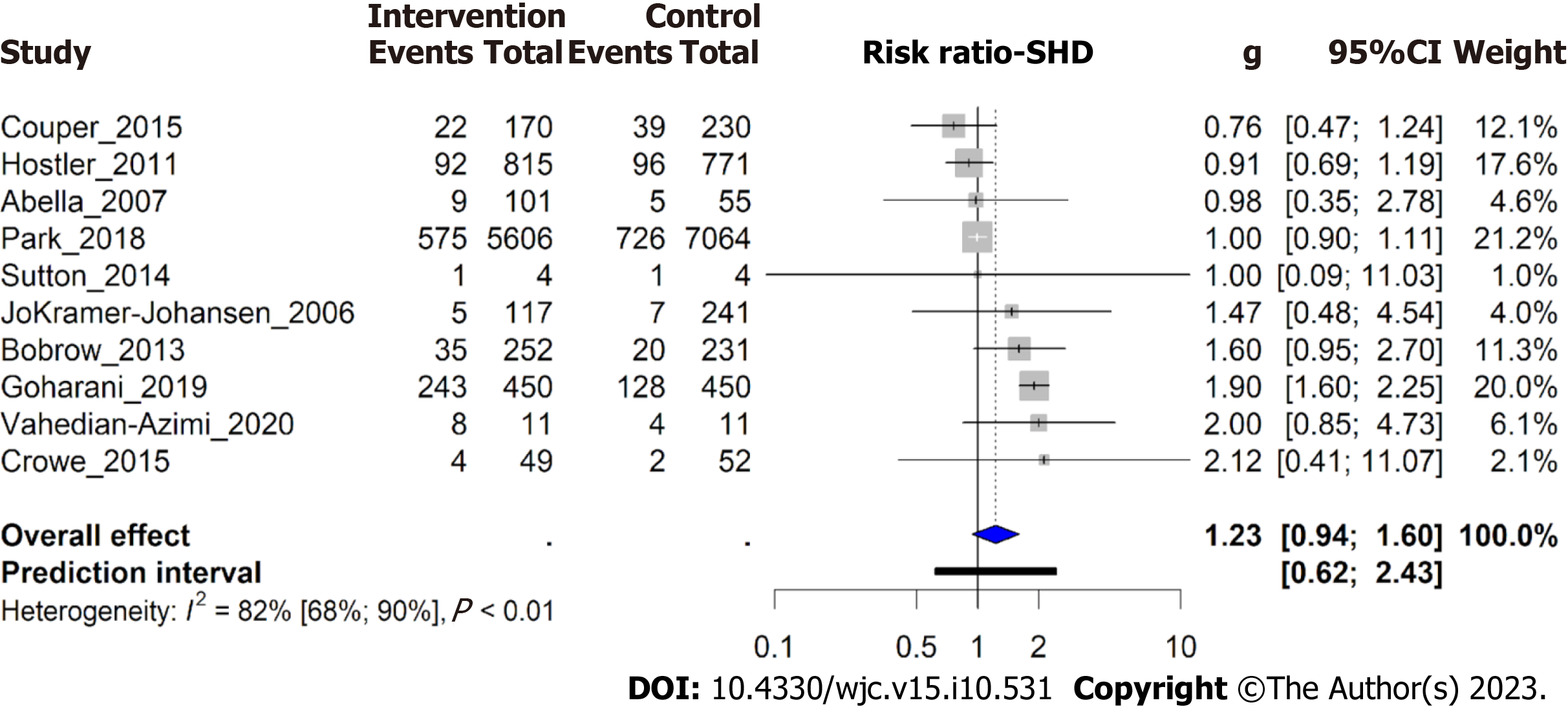
Ten trials reported SHD as an outcome of interest (n = 16684). SHD was reported in 994 patients (13.1%) in the RTAVF-assisted CPR group and in 1028 patients (11.2%) in the conventional CPR group. No significant difference was found in SHD between the two groups (RR 1.23; 0.94-1.60; P = 0.12) (Figure 3). Subgroup analysis found no significant correlation between SHD and the location of cardiac arrest (P value for interaction = 0.26) (Supplementary Figure 5).
Eight studies reported compression rate as an outcome of interest (n = 2804). The average compression rate was 107.3 ± 9.4 in the RTAVF-assisted CPR group and 117.5 ± 13.8 in the conventional CPR group, with a nationally recommended rate of 100-120 compressions per minute[53]. A non-significant difference was seen between the two, with patients in the intervention group receiving a lower compression rate [SMD -2.1; (-4.6-0.5); P = 0.09] (Supplementary Figure 6). While both groups had an average compression rate within the nationally recommended guidelines, the proportion of compressions that fell between 100-120 compressions per minute was likely higher in the intervention group than in the control group (Supplementary Figure 6). Eight studies reported compression depth as an outcome of interest (n = 2625). The average compression depth was 4.59 cm ± 0.91 cm in the intervention group and 4.24 cm ± 1.29 cm in the control group, with a nationally recommended compression depth of 5-6 cm in the average adult[53]. Neither group had an average compression depth that met AHA guidelines. However, a significant difference was seen between the two groups, with patients in the intervention group receiving a higher compression depth, closer to AHA guidelines [SMD 1.6 (0.02-3.1); P = 0.047] (Supplementary Figure 7).
This manuscript analyzed the most recent evidence with regards to the efficacy of real-time audiovisual feedback devices in improving CPR quality and patient outcomes. A total of 13 studies (n = 17600) were included, making it the largest study of this topic to date.
Currently, patient outcomes after cardiac arrest remain poor. This meta-analysis found an average ROSC of 37%, which is consistent with previous literature findings ranging between 13% and 72%[54-59].
The AHA mandated that beginning January 2019, all AHA courses that teach adult CPR will be required to use a real-time audiovisual feedback device. These devices typically measure one or more of the following CPR metrics: Chest compression rate, depth, hand position, recoil, ventilation volume, ventilation rate, and hands-off time. Multiple types of feedback devices exist, including manikins with integrated sensors, devices that can be added to existing manikins, and hand-held devices that can be easily transferred from patient to patient[60]. As this meta-analysis examined the effect of using RTAVF devices during CPR on patient outcomes, the only type of RTAVF devices that were analyzed were hand-held devices that can be used during CPR on patients, rather than manikin-based RTAVF devices.
Thirteen studies with a total of 17600 patients were analyzed. These studies were a mixture of 4 RCT, 2 non-RCT, 4 cohort studies, 2 before-after studies, and 1 matched pair registry study. Studies took place across the globe with only 5 in the United States. These studies were both clinically and statistically heterogenous, with varying protocols and outcomes. Despite this heterogeneity, all studies did examine the primary outcome of ROSC with ten of thirteen also examining SHD.
Contrary to prior literature reviews, this analysis found that the use of real-time audiovisual feedback devices did significantly improve ROSC in cases of IHCA. This may be because prior meta-analyses included only three human intervention studies, while this meta-analysis had a larger number of studies and patients[31,32]. In addition, Kirkbright et al[32] 2013, Gugelmin-Almeida et al[31] 2021, and Lv et al[61] 2022 included only 1, 2, and 5 studies focusing on IHCA, respectively. This meta-analysis found that the location of cardiac arrest played a significant role in whether RTAVF devices influenced ROSC, with a significant increase in ROSC seen in cases of IHCA and no such increase seen in cases of OHCA. This could be another reason why prior reviews found no significant impact of RTAVF devices on ROSC. In particular, Lv et al[61] 2022 found that RTAVF-assisted CPR did not improve ROSC across all studies, but did not differentiate between ROSC outcomes in IHCA and OHCA settings. These findings suggest that hospitals should prioritize the rollout and adoption of RTAVF devices in areas most likely to see IHCA, such as intensive care units, telemetry units, and EDs, rather than with paramedics or ambulances[62,63]. This difference in survival may be due to the inherent rushed nature of CPR for patients suffering OHCA. Unlike cases of IHCA where a dedicated HCW can focus exclusively on performing high quality CPR, in cases of OHCA, paramedics may be obligated to multi-task, performing CPR while also keeping track of the other required tasks to bring the patient into the hospital safely. As such, the quality of CPR may be reduced in cases of OHCA vs IHCA. Another explanation could be tied to the fact that the time-to-CPR from arrest is lower in cases of IHCA vs OHCA, and as such CPR quality may play a more important role in IHCA than in OHCA[64,65].
Despite the increase in ROSC when using RTAVF devices, no similar increase was seen in SHD. This insignificance may relate to how CPR quality plays little role in the improvement of survival after ROSC. It could also be due to the presence of comorbidities including heart failure, sepsis, and myocardial infarction and that effective CPR is one factor among many steps required for improved survival. Without additional improvements in other steps required in the care of post-cardiac arrest patients, the increase in CPR quality may be insufficient to translate into improved SHD.
Repeated studies in the literature have shown that CPR quality when performed on manikins improves when using a RTAVF device[31,32]. Consistent with existing literature, this meta-analysis also found that CPR quality was increased in RTAVF-assisted CPR. The average compression rate in both groups fell within AHA guidelines, while the average compression depth in both groups fell outside of AHA guidelines[53]. However, for both compression rate and depth, the RTAVF group was more likely to have a higher proportion of compressions falling within guidelines compared to the conventional CPR group, showing that RTAVF-assisted CPR was superior to conventional CPR. Prior studies have shown the importance of proper compression depth in patient outcomes[10,16,66]. In CPR training courses being taught with RTAVF devices, a larger focus should be put on achieving adequate compression depth.
Overall, the evidence suggests that RTAVF-assisted CPR is of superior quality than conventional CPR. In addition, RTAVF-assisted CPR has a small benefit in patient outcomes, specifically improving ROSC in cases of IHCA. However, this meta-analysis has multiple limitations. First, the studies examined were both statistically and clinically heterogeneous, with varying study parameters, outcomes, and designs, limiting the internal validity of the meta-analysis. This was partially accounted for using a random-effects model and by subgroup analysis, but not all heterogeneity could be accounted for. This may partially be due to the limitations of I2 as a metric for heterogeneity. This study contained relatively larger studies than most examining this topic, and prior literature has documented that as sampling error decreases, I2 tends to increase, which can erroneously lead to assumptions that clinical heterogeneity has also increased. In addition, as this meta-analysis examined the class of all RTAVF devices used in CPR, some degree of clinical heterogeneity is expected, as the expected effects of individual devices can vary. Second, nine of these thirteen studies were not RCT, which can introduce sources of both confounding and selection bias. However, ROSC outcomes of cardiac arrest patients are dependent upon many non-controllable factors that cannot undergo randomization including time from arrest to CPR initiation and presence of shockable rhythm which may limit the advantage an RCT would have over other nonrandomized studies designs. Third, this meta-analysis only examined RTAVF devices that could be used during CPR on patients rather than RTAVF devices that are built into manikins. As such, these results cannot be extrapolated to that class of RTAVF devices. Fourth, this meta-analysis only reviewed publications in the literature until 2020, precluding studies published thereafter from inclusion in this analysis. Fifth, this meta-analysis was limited by the evidence that could be extracted from prior reports in the literature, and evidence on long-term patient outcomes and neurological function from RTAVF-assisted CPR is lacking. Future research should examine such cohorts and associated long-term outcomes. In addition, further research into why the improvements seen in ROSC with RTAVF-assisted CPR were not translated into improvements in SHD is warranted, along with research examining which RTAVF device provides the highest improvement in patient outcomes and CPR quality.
This meta-analysis examined 13 studies (n = 17600) and found that RTAVF-assisted CPR resulted in a significantly increased rate of ROSC, specifically in cases of IHCA but did not improve SHD. This is a novel finding, with prior meta-analyses finding that the use of RTAVF devices did not significantly improve patient outcomes. Consistent with what has been found previously, the use of RTAVF devices resulted in improved CPR quality, as measured by compression rate and depth.
Cardiac arrest is a leading cause of mortality in America and continues to grow in prevalence. Cardiopulmonary resuscitation (CPR) increases survival outcomes in cases of cardiac arrest; however, healthcare workers often do not perform CPR within recommended guidelines. Real-time audiovisual feedback (RTAVF) devices provide live feedback on CPR performance and subsequently improves the quality of CPR performed.
Effective CPR in cardiac arrest is critical to emergent management and stabilization. RTAVF-assisted CPR devices may improve performance, compliance with recommended guidelines, and survival, therefore, this systematic review and meta-analysis seeks to compare the effect of RTAVF-assisted CPR devices with conventional CPR on patient outcomes in the setting of in-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA).
To investigate the impact of RTAVF-assisted CPR on patient outcomes and CPR quality with respect to in- and OHCA.
The literature search was conducted on PubMed, SCOPUS, the Cochrane Library, and EMBASE from inception to July 27, 2020, for studies reporting patient outcomes and/or CPR quality metrics between an RTAVF-assisted CPR and conventional CPR in the setting of IHCA or OHCA. The primary outcomes of interest extracted and analyzed were return of spontaneous circulation (ROSC) and survival to hospital discharge (SHD). Data was analyzed using R statistical software 4.2.0. Results were statistically significant if P < 0.05.
Thirteen studies (n = 17600) were included after deduplication, screening, and full-text analysis. Patients were on average 69 ± 17.5 years old, with 7022 (39.8%) female patients. Overall pooled ROSC was 37% among all studies. RTAVF-assisted CPR significantly improved ROSC in the case of IHCAs and improved chest compression depth. No significant improvements were seen in ROSC in cases of OHCA, SHD, or compression rate.
This meta-analysis found that RTAVF-assisted CPR increases ROSC in the setting of IHCA but has no significant effect on ROSC in the setting of OHCA or SHD. Consistent with previous manikin simulation studies, the meta-analysis found that RTAVF-assisted CPR results in improvements in both chest compression rate and depth.
Cardiac arrest remains a leading cause of mortality with increasing prevalence. The findings of this study suggest that RTAVF-assisted CPR may improve ROSC in the setting of IHCAs but not in the setting of OHCA. Hospitals should prioritize implementing RTAVF devices in areas with the highest rates of IHCA rather than to paramedics or ambulances.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Peng D, China; Xiang T, China S-Editor: Qu XL L-Editor: A P-Editor: Xu ZH
| 1. | Holmberg MJ, Ross CE, Fitzmaurice GM, Chan PS, Duval-Arnould J, Grossestreuer AV, Yankama T, Donnino MW, Andersen LW; American Heart Association’s Get With The Guidelines–Resuscitation Investigators. Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12:e005580. [PubMed] |
| 2. | Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141:e139-e596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3254] [Cited by in RCA: 5484] [Article Influence: 1096.8] [Reference Citation Analysis (1)] |
| 3. | Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Ferguson JF, Generoso G, Ho JE, Kalani R, Khan SS, Kissela BM, Knutson KL, Levine DA, Lewis TT, Liu J, Loop MS, Ma J, Mussolino ME, Navaneethan SD, Perak AM, Poudel R, Rezk-Hanna M, Roth GA, Schroeder EB, Shah SH, Thacker EL, VanWagner LB, Virani SS, Voecks JH, Wang NY, Yaffe K, Martin SS. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153-e639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2995] [Cited by in RCA: 3264] [Article Influence: 1088.0] [Reference Citation Analysis (0)] |
| 4. | Wu L, Narasimhan B, Bhatia K, Ho KS, Krittanawong C, Aronow WS, Lam P, Virani SS, Pamboukian SV. Temporal Trends in Characteristics and Outcomes Associated With In-Hospital Cardiac Arrest: A 20-Year Analysis (1999-2018). J Am Heart Assoc. 2021;10:e021572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Stecker EC, Reinier K, Marijon E, Narayanan K, Teodorescu C, Uy-Evanado A, Gunson K, Jui J, Chugh SS. Public health burden of sudden cardiac death in the United States. Circ Arrhythm Electrophysiol. 2014;7:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 226] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 6. | Murphy TW, Cohen SA, Avery KL, Balakrishnan MP, Balu R, Chowdhury MAB, Crabb DB, Huesgen KW, Hwang CW, Maciel CB, Gul SS, Han F, Becker TK; Interdisciplinary Cardiac Arrest Research Review (ICARE) group. Cardiac arrest: An interdisciplinary scoping review of the literature from 2019. Resusc Plus. 2020;4:100037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Azeli Y, Barbería E, Fernández A, García-Vilana S, Bardají A, Hardig BM. Chest wall mechanics during mechanical chest compression and its relationship to CPR-related injuries and survival. Resusc Plus. 2022;10:100242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Bobrow BJ, Vadeboncoeur TF, Stolz U, Silver AE, Tobin JM, Crawford SA, Mason TK, Schirmer J, Smith GA, Spaite DW. The influence of scenario-based training and real-time audiovisual feedback on out-of-hospital cardiopulmonary resuscitation quality and survival from out-of-hospital cardiac arrest. Ann Emerg Med. 2013;62:47-56.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 9. | Cheskes S, Schmicker RH, Christenson J, Salcido DD, Rea T, Powell J, Edelson DP, Sell R, May S, Menegazzi JJ, Van Ottingham L, Olsufka M, Pennington S, Simonini J, Berg RA, Stiell I, Idris A, Bigham B, Morrison L; Resuscitation Outcomes Consortium (ROC) Investigators. Perishock pause: an independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation. 2011;124:58-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 320] [Cited by in RCA: 305] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 10. | Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, Callaway CW, Bishop D, Vaillancourt C, Davis D, Aufderheide TP, Idris A, Stouffer JA, Stiell I, Berg R; Resuscitation Outcomes Consortium Investigators. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120:1241-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 609] [Cited by in RCA: 590] [Article Influence: 36.9] [Reference Citation Analysis (0)] |
| 11. | Gallagher EJ, Lombardi G, Gennis P. Effectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest. JAMA. 1995;274:1922-1925. [PubMed] |
| 12. | Vadeboncoeur T, Stolz U, Panchal A, Silver A, Venuti M, Tobin J, Smith G, Nunez M, Karamooz M, Spaite D, Bobrow B. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation. 2014;85:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 214] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 13. | Van Hoeyweghen RJ, Bossaert LL, Mullie A, Calle P, Martens P, Buylaert WA, Delooz H. Quality and efficiency of bystander CPR. Belgian Cerebral Resuscitation Study Group. Resuscitation. 1993;26:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 326] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 14. | Wik L, Steen PA, Bircher NG. Quality of bystander cardiopulmonary resuscitation influences outcome after prehospital cardiac arrest. Resuscitation. 1994;28:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 286] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 15. | Kwon OY. The changes in cardiopulmonary resuscitation guidelines: from 2000 to the present. J Exerc Rehabil. 2019;15:738-746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, Vanden Hoek TL, Becker LB. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 974] [Cited by in RCA: 898] [Article Influence: 44.9] [Reference Citation Analysis (0)] |
| 17. | Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O'Hearn N, Wigder HN, Hoffman P, Tynus K, Vanden Hoek TL, Becker LB. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 500] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 18. | Ashton A, McCluskey A, Gwinnutt CL, Keenan AM. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation. 2002;55:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 187] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 19. | Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D, McKnite S, von Briesen C, Sparks CW, Conrad CJ, Provo TA, Lurie KG. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960-1965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 563] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 20. | Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, Bigham B, Morrison LJ, Larsen J, Hess E, Vaillancourt C, Davis DP, Callaway CW; Resuscitation Outcomes Consortium (ROC) Investigators. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40:1192-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 329] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 21. | Sunde K, Eftestøl T, Askenberg C, Steen PA. Quality assessment of defribrillation and advanced life support using data from the medical control module of the defibrillator. Resuscitation. 1999;41:237-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 69] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, Berg MD, Chameides L, O'Connor RE, Swor RA. Part 4: CPR overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S676-S684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 295] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 23. | Valenzuela TD, Kern KB, Clark LL, Berg RA, Berg MD, Berg DD, Hilwig RW, Otto CW, Newburn D, Ewy GA. Interruptions of chest compressions during emergency medical systems resuscitation. Circulation. 2005;112:1259-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 232] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 24. | van Alem AP, Sanou BT, Koster RW. Interruption of cardiopulmonary resuscitation with the use of the automated external defibrillator in out-of-hospital cardiac arrest. Ann Emerg Med. 2003;42:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 118] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 25. | Wik L, Kramer-Johansen J, Myklebust H, Sørebø H, Svensson L, Fellows B, Steen PA. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1002] [Cited by in RCA: 938] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 26. | Abella BS, Edelson DP, Kim S, Retzer E, Myklebust H, Barry AM, O'Hearn N, Hoek TL, Becker LB. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 282] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 27. | Kramer-Johansen J, Myklebust H, Wik L, Fellows B, Svensson L, Sørebø H, Steen PA. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 404] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 28. | Bhanji F, Finn JC, Lockey A, Monsieurs K, Frengley R, Iwami T, Lang E, Ma MH, Mancini ME, McNeil MA, Greif R, Billi JE, Nadkarni VM, Bigham B; Education, Implementation, and Teams Chapter Collaborators. Part 8: Education, Implementation, and Teams: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2015;132:S242-S268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 29. | Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW Jr, Hoek TV, Halverson CC, Doering L, Peberdy MA, Edelson DP; American Heart Association Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on P. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. 2013;127:1538-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 226] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 30. | Soar J, Mancini ME, Bhanji F, Billi JE, Dennett J, Finn J, Ma MH, Perkins GD, Rodgers DL, Hazinski MF, Jacobs I, Morley PT; Education, Implementation, and Teams Chapter Collaborators. Part 12: Education, implementation, and teams: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2010;81 Suppl 1:e288-e330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 129] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 31. | Gugelmin-Almeida D, Tobase L, Polastri TF, Peres HHC, Timerman S. Do automated real-time feedback devices improve CPR quality? A systematic review of literature. Resusc Plus. 2021;6:100108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 32. | Kirkbright S, Finn J, Tohira H, Bremner A, Jacobs I, Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85:460-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 127] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 33. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24818] [Article Influence: 1772.7] [Reference Citation Analysis (3)] |
| 34. | Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomised Studies in Meta-Analyses. Beyond the Basics 2014. |
| 35. | Tufanaru C, Munn Z, Stephenson M, Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Based Healthc. 2015;13:196-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 718] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 36. | Sood N, Sangari A, Goyal A, Conway JAS. Predictors of survival for pediatric extracorporeal cardiopulmonary resuscitation: A systematic review and meta-analysis. Medicine (Baltimore). 2022;101:e30860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 37. | Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3433] [Cited by in RCA: 7017] [Article Influence: 637.9] [Reference Citation Analysis (0)] |
| 38. | Deeks JJ, Higgins JPT, Altman DG. 9.2.3.2 The standardized mean difference: The Cochrane Collaboration; 2011. Available from: https://handbook-5-1.cochrane.org/chapter_9/9_2_3_2_the_standardized_mean_difference.htm. |
| 39. | Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing Meta-Analysis with R: A Hands-On Guide. 2021. |
| 40. | Sangari A, Sood N, Sood A, Maini K, Hauger J. 42 Improving Patient Selection in International Pediatric ECPR Cohorts. Annals of Emergency Medicine. 2021;78:S18. |
| 41. | Deeks JJ, Higgins JP, Altman DG. 9.5.2 Identifying and measuring heterogeneity: The Cochrane Collaboration; 2011. Available from: https://handbook-5-1.cochrane.org/chapter_9/9_5_2_identifying_and_measuring_heterogeneity.htm. |
| 42. | Sood N, Goyal A, Grogan D, Reddy V. Abstract 9115: Determining Optimal Hemoglobin Transfusion Threshold for Patients With Severe Traumatic Brain Injury: A Systematic Review and Meta-Analysis. Circulation. 2021;144:A9115-A. [DOI] [Full Text] |
| 43. | Couper K, Kimani PK, Abella BS, Chilwan M, Cooke MW, Davies RP, Field RA, Gao F, Quinton S, Stallard N, Woolley S, Perkins GD; Cardiopulmonary Resuscitation Quality Improvement Initiative Collaborators. The System-Wide Effect of Real-Time Audiovisual Feedback and Postevent Debriefing for In-Hospital Cardiac Arrest: The Cardiopulmonary Resuscitation Quality Improvement Initiative. Crit Care Med. 2015;43:2321-2331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 44. | Crowe C, Bobrow BJ, Vadeboncoeur TF, Dameff C, Stolz U, Silver A, Roosa J, Page R, LoVecchio F, Spaite DW. Measuring and improving cardiopulmonary resuscitation quality inside the emergency department. Resuscitation. 2015;93:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 45. | Goharani R, Vahedian-Azimi A, Farzanegan B, Bashar FR, Hajiesmaeili M, Shojaei S, Madani SJ, Gohari-Moghaddam K, Hatamian S, Mosavinasab SMM, Khoshfetrat M, Khabiri Khatir MA, Miller AC; MORZAK Collaborative. Real-time compression feedback for patients with in-hospital cardiac arrest: a multi-center randomized controlled clinical trial. J Intensive Care. 2019;7:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 46. | Hostler D, Everson-Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, Sears GK, Emerson SS, Nichol G; Resuscitation Outcomes Consortium Investigators. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2011;342:d512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 180] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 47. | Lakomek F, Lukas RP, Brinkrolf P, Mennewisch A, Steinsiek N, Gutendorf P, Sudowe H, Heller M, Kwiecien R, Zarbock A, Bohn A. Real-time feedback improves chest compression quality in out-of-hospital cardiac arrest: A prospective cohort study. PLoS One. 2020;15:e0229431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 48. | Lukas RP, Gräsner JT, Seewald S, Lefering R, Weber TP, Van Aken H, Fischer M, Bohn A. Chest compression quality management and return of spontaneous circulation: a matched-pair registry study. Resuscitation. 2012;83:1212-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 49. | Park JH, Shin SD, Ro YS, Song KJ, Hong KJ, Kim TH, Lee EJ, Kong SY. Implementation of a bundle of Utstein cardiopulmonary resuscitation programs to improve survival outcomes after out-of-hospital cardiac arrest in a metropolis: A before and after study. Resuscitation. 2018;130:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 50. | Sutton RM, Niles D, French B, Maltese MR, Leffelman J, Eilevstjønn J, Wolfe H, Nishisaki A, Meaney PA, Berg RA, Nadkarni VM. First quantitative analysis of cardiopulmonary resuscitation quality during in-hospital cardiac arrests of young children. Resuscitation. 2014;85:70-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 51. | Vahedian-Azimi A, Hajiesmaeili M, Amirsavadkouhi A, Jamaati H, Izadi M, Madani SJ, Hashemian SM, Miller AC. Effect of the Cardio First Angel™ device on CPR indices: a randomized controlled clinical trial. Crit Care. 2016;20:147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 52. | Vahedian-Azimi A, Rahimibashar F, Miller AC. A comparison of cardiopulmonary resuscitation with standard manual compressions versus compressions with real-time audiovisual feedback: A randomized controlled pilot study. Int J Crit Illn Inj Sci. 2020;10:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 53. | Merchant RM, Topjian AA, Panchal AR, Cheng A, Aziz K, Berg KM, Lavonas EJ, Magid DJ; Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S337-S357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 428] [Article Influence: 85.6] [Reference Citation Analysis (0)] |
| 54. | Banerjee P, Ganti L, Stead TG, Vera AE, Vittone R, Pepe PE. Every one-minute delay in EMS on-scene resuscitation after out-of-hospital pediatric cardiac arrest lowers ROSC by 5. Resusc Plus. 2021;5:100062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 55. | Chan PS, McNally B, Tang F, Kellermann A; CARES Surveillance Group. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation. 2014;130:1876-1882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 383] [Cited by in RCA: 454] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 56. | Chan PS, Tang Y; American Heart Association's Get With the Guidelines®‐Resuscitation Investigators. Risk-Standardizing Rates of Return of Spontaneous Circulation for In-Hospital Cardiac Arrest to Facilitate Hospital Comparisons. J Am Heart Assoc. 2020;9:e014837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 57. | Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS; American Heart Association Get with the Guidelines–Resuscitation Investigators. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 671] [Article Influence: 51.6] [Reference Citation Analysis (0)] |
| 58. | Schmidbauer S, Yates EJ, Andréll C, Bergström D, Olson H, Perkins GD, Friberg H. Outcomes and interventions in patients transported to hospital with ongoing CPR after out-of-hospital cardiac arrest - An observational study. Resusc Plus. 2021;8:100170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 59. | Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, Zong Q, Chen S, Lv C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 529] [Article Influence: 105.8] [Reference Citation Analysis (0)] |
| 60. | Sood N, Sangari A, Hauger JA. Abstract 344: Comparing the Efficacy of Real-Time Audiovisual Feedback Devices and Active Compression-Decompression Devices in Out-of-Hospital Cardiac Arrest: A Network Meta-Analysis. Circulation. 2020;142:A344-A. [DOI] [Full Text] |
| 61. | Lv GW, Hu QC, Zhang M, Feng SY, Li Y, Zhang Y, Zhang YY, Wang WJ. Effect of real-time feedback on patient's outcomes and survival after cardiac arrest: A systematic review and meta-analysis. Medicine (Baltimore). 2022;101:e30438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 62. | Leung KHB, Sun CLF, Yang M, Allan KS, Wong N, Chan TCY. Optimal in-hospital defibrillator placement. Resuscitation. 2020;151:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 63. | Perman SM, Stanton E, Soar J, Berg RA, Donnino MW, Mikkelsen ME, Edelson DP, Churpek MM, Yang L, Merchant RM; American Heart Association's Get With the Guidelines®—Resuscitation (formerly the National Registry of Cardiopulmonary Resuscitation) Investigators. Location of In-Hospital Cardiac Arrest in the United States-Variability in Event Rate and Outcomes. J Am Heart Assoc. 2016;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 64. | Bobrow BJ, Panczyk M. Time to Compress the Time to First Compression. J Am Heart Assoc. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 65. | Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, Karlsson T, Svensson L. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307-2315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 650] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 66. | Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, Vadeboncoeur TF, Clark LL, Gallagher JV, Stapczynski JS, LoVecchio F, Mullins TJ, Humble WO, Ewy GA. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 337] [Article Influence: 22.5] [Reference Citation Analysis (1)] |