Published online Jan 26, 2023. doi: 10.4330/wjc.v15.i1.13
Peer-review started: October 18, 2022
First decision: November 2, 2022
Revised: November 8, 2022
Accepted: December 23, 2022
Article in press: December 23, 2022
Published online: January 26, 2023
Processing time: 85 Days and 11 Hours
Coronavirus disease 2019 (COVID-19) pandemic unmasked the huge deficit in healthcare resources worldwide. It highlighted the need for efficient risk stratification in management of cardiovascular emergencies.
To study the applicability of the old, available and affordable nonconventional biomarkers: albumin and fibrinogen in their ability to predict angiographic severity and clinical outcomes in patients with acute coronary syndrome (ACS).
In this prospective, observational study, 166 consecutive patients with ACS were enrolled. Fibrinogen, albumin and their ratio were determined from serum. Patients with underlying chronic liver disease, active malignancy, autoimmune disease, active COVID-19 infection and undergoing thrombolysis were excluded.
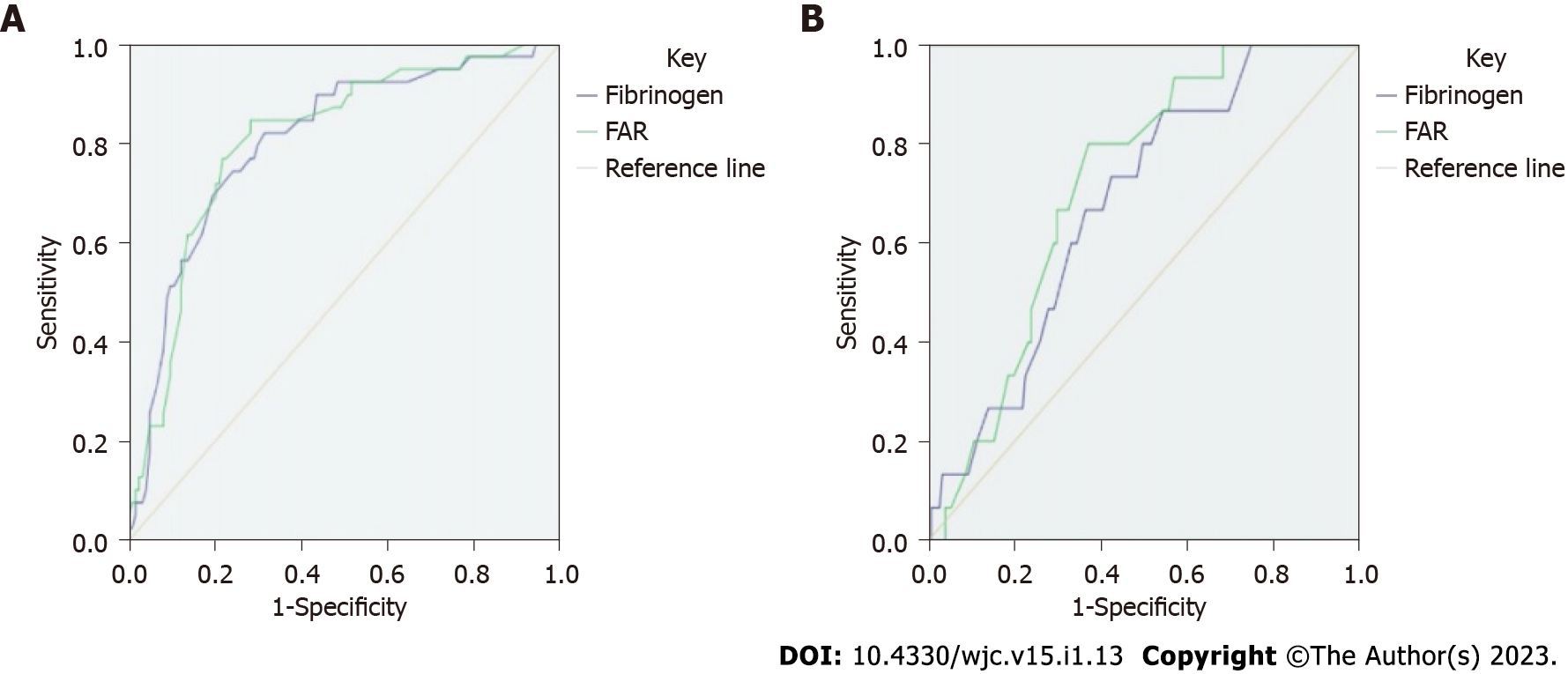
Mean age of the population was 60.5 ± 1.5 years, 74.1% being males. ST elevation myocardial infarction (STEMI) was most common presentation of ACS seen in 57% patients. Fibrinogen albumin ratio (FAR) ≥ 19.2, had a sensitivity of 76.9% and specificity of 78.9 % [area under the receiver operating characteristic curves (AUROC) = 0.8, P = 0.001] to predict ≤ thrombolysis in myocardial infarction (TIMI) 1 flow in culprit artery in STEMI patients. Even in non-STEMI patients, FAR ≥ 18.85 predicted the same with 80% sensitivity and 63% specificity (AUROC = 0.715, P = 0.006).
Novel biomarkers, with their high cost, lack of availability and long turn over time are impractical for real-world use. Identifying ≤ TIMI 1 flow in the culprit artery has significant impact of management and outcome. Our study has shown that readily available biomarkers like fibrinogen and albumin can help identify these high-risk patients with good accuracy. This allows risk-stratification and individualization of treatment in ACS.
Core Tip: The study highlights the role of cost-effective, readily available biomarkers fibrinogen and albumin in predicting angiographic severity and clinical outcomes in patients with acute coronary syndrome. Fibrinogen to albumin ratio independently predicted outcomes with greater accuracy compared to fibrinogen or albumin alone. Fibrinogen albumin ratio (FAR) ≥ 19.2, had a sensitivity of 76.9% and specificity of 78.9 % to predict ≤ thrombolysis in myocardial infarction 1 flow in culprit artery in ST elevation myocardial infarction (STEMI) patients. Even in non-STEMI patients, FAR ≥ 18.85 predicted the same with 80% sensitivity and 63% specificity.
- Citation: Makkar K, Sharma YP, Batta A, Hatwal J, Panda PK. Role of fibrinogen, albumin and fibrinogen to albumin ratio in determining angiographic severity and outcomes in acute coronary syndrome. World J Cardiol 2023; 15(1): 13-22
- URL: https://www.wjgnet.com/1949-8462/full/v15/i1/13.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i1.13
Tremendous progress has been made in the management of acute coronary syndrome (ACS) over last six decades[1]. The success is attributed to be due to improved overall health care facilities, availability of stronger antiplatelet agents and other cardioprotective medications, improved revascularization strategies including both advances in thrombolytic therapy and the ever-improving stent design and technologies which have led to drastic decrease in morbidity and mortality associated with ACS[2-4]. However, despite the obvious progress, gaps exists and ACS continues to be the leading cause of death worldwide with considerable short and long-term mortality and morbidity. The situation is dismal in the developing world where the health care resources are scarce[5]. The coronavirus disease 2019 (COVID-19) pandemic has highlighted the same and the need for efficient triaging and risk-assessment for efficient patient management[6].
Prior to the availability of laboratory resources, the risk stratification was mainly based on the clinical assessment and accordingly clinical risk scores were developed to predict outcomes. Next, with the availability of various laboratory parameters, the risk stratification was further refined by incorporating these biomarkers. Certain novel biomarkers have been recognized ranging from C-reactive protein (CRP) to cysteine rich angiogenic inducer 61 to predict high-risk ACS[7]. Attempt has been made to incorporate these biomarkers to traditional scoring systems to add to their prognostic value, however risk stratification of ACS remains far from perfect[8]. The goal of risk stratification is not only to predict outcomes but also to guide management and more importantly urgency of treatment needed. This is even more relevant in a resource constrained setting. Hence, triaging of patients with ACS and guidance as to which patient needs early intervention and who should be managed medically is a top priority.
Starting from January 27, 2020, when the 1st case of COVID-19 was diagnosed in India, the pandemic had pushed India to the brink, stretching the already thin health care resources. It unmasked the vast deficiencies in our health care system and was a wake-up call to the country to ramp up its preparedness before the next wave. All medical and surgical specialties suffered as result, and acute cardiac care was perhaps the hardest hit[9,10]. Even before the pandemic the condition of cardiac care facilities was suboptimal and registry data of ACS from India showed that only 20% of patients of ACS undergo coronary angiography[11]. In comparison to developed nations, we have half the catheterization labs to cater to our second largest population of world[12]. The morbidity and mortality of ACS is significantly higher compared to the western world.
Novel biomarkers used to prognosticate patients often are experimental and real-world use is often not feasible[13]. Thus, we evaluated role of easily available inflammatory biomarkers like fibrinogen, albumin along with fibrinogen albumin ratio (FAR) role in ACS. They were analyzed to assess if they could predict angiographic severity or clinical outcomes among patients. The aim of the present study was to analyze the role of old, readily available biomarkers, fibrinogen, albumin and FAR in determining angiographic severity and clinical outcomes.
This was a prospective, single center, observational study conducted between August 2019 and December 2020. Consecutive patients with ACS presenting to Cardiology department were included. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki and was reviewed and cleared by the Ethics committee of the Post Graduate Institute of Medical education and Research, Chandigarh (ref no INT/IEC/2019/2750). Informed written consent was obtained from all patients or appropriate legally authorized representatives.
ST elevation myocardial infarction (STEMI) was defined by patients presenting with acute chest pain and electrocardiogram showing ST elevation in ≥ 1 mm in two contiguous leads in all leads other than lead V2-V3. Cutoff point for lead V2-V3 was ≥ 2 mm in males and ≥ 1.5 mm in females[14]. Non-STEMI (NSTEMI) and unstable angina (USA) was defined as per 2014 American Heart Association/American college of cardiology non-ST elevation ACS guidelines[15]. Patients were examined by cardiologists to classify patients from Killip class 1 to 4 depending upon severity of heart failure and cardiogenic shock (CS). Patients with CS were subcategorized as per definition of Society of Cardiovascular angiography and Intervention (SCAI) into stage C to E[16]. Patients were excluded from study if they had undergone fibrinolysis, had underlying chronic liver disease, active malignancy or any autoimmune disease. Patients were followed up telephonically or in person visit at 1, 3 and 6 mo to assess their major adverse cardiovascular and cerebral events (MACCE).
Coronary angiographies were assessed by two interventional cardiologists. Culprit artery was identified by finding of angiography, 12-lead electrocardiogram and regional wall motion abnormality on echocardiography. Coronary flow was classified according to thrombolysis in myocardial infarction (TIMI) risk score[17]. Total occlusion was defined by pre percutaneous coronary artery (PCI) TIMI ≤ 1 and spontaneous recanalization (SR) was defined by TIMI score ≥ 2.
Venous blood samples were taken within 24 h of admission and prior to angiography. Fibrinogen samples were drawn in sodium citrate vacuum tubes and albumin samples in plain serum vials. FAR ratio was calculated by ratio of fibrinogen (gm/dL) and albumin (gm/dL) and multiplying the ratio by 100. Albumin levels were calculated using bromocresol method on a Technicon RA-1000 automated analyzer (Technicon Instruments, Tarrytown, NY, United States). Fibrinogen concentration was measured with turbidimetric assay using ammonium sulphate. Care was taken to ensure all samples collected were processed within 6 h of collection to ensure minimal alteration of the biomarker levels.
Statistical analysis was performed with Statistical Package for the Social Sciences version 26 (SPSS Inc., Chicago, IL, United States). Variables are presented as mean ± SD or median (inter-quartile range). Variable were checked for outliers and normalcy using the Shapiro-Wilk test. Continuous variables with normal distribution were compared with the independent samples Student’s t-test and those with non-normal distribution with the Mann-Whitney U test. Comparison between categorical variables was done using chi-square test or Fisher exact test. A two-sided P value < 0.05 was considered to be significant for all variables.
A total of 166 patients of ACS were included in this study. The mean age of patients was 60.5 ± 10.5 years, with majority of patients being males (74%). Ninety-five (57.2%) patients presented with STEMI while NSTEMI ACS (NSTEACS) patients constituted the remaining 42.8%. Among risk factors of CAD most common was hypertension present in 63% followed by diabetes mellitus in 50% of the cohort. Rest angina was presenting complaint in over 90% patients while new onset shortness of breath was present in 18%. The mean duration of presentation to our hospital after chest pain onset was 12.8 ± 9.9 h. The mechanical complications of ACS were also assessed and patients presenting with severe left ventricular systolic dysfunction (Ejection fraction < 30%) or significant ischemic mitral regurgitation (MR) were more common in patients with STEMI compared to NSTEACS (44.2% vs 21%, P = 0.005 and 31.6% vs 15%, P = 0.014 respectively). Patients with classical CS (SCAI stage-C) or worse was present in 26 (15.6%) patients. Angiography was done in around 88% while 62% underwent PCI. The detailed demographic details and key investigation details are presented in Table 1.
| STEMI (n = 95) | NSTEMI (n = 38) | USA (n = 33) | P value | |
| Risk factors | ||||
| Age, yr (mean ± SD) | 61.2 ± 10.1 | 60.2 ± 11.0 | 60.5 ± 10.5 | 0.5 |
| Males | 73 (76.8) | 25 (65.8) | 25 (75.8) | 0.5 |
| Diabetes | 49 (52) | 20 (52.6) | 14 (42.4) | 0.5 |
| Hypertension | 61 (64) | 22 (58) | 21 (64) | 0.8 |
| Smoking | 31 (32.6) | 12 (31.6) | 10 (30.3) | 0.9 |
| Prior history of CAD | 2 (2.2) | 6 (16.2) | 9 (27.3) | 0.001 |
| Clinical features on presentation | ||||
| Rest angina | 89 (93.6) | 36 (94.7) | 26 (78.8) | 0.013 |
| Ejection fraction < 30% | 42 (44.2) | 10 (26.3) | 5 (15.2) | 0.005 |
| Significant ischemic MR | 30 (31.6) | 9 (23.7) | 2 (6.1) | 0.014 |
| Killip class ≥ 2 | 24 (25.3) | 7 (18.4) | 2 (6) | 0.057 |
| SCAI stage C | 11 (11.6) | 7 (18.4) | 0 | 0.04 |
| SCAI stage D | 3 (3.2) | 0 | 0 | 0.3 |
| SCAI stage E | 5 (5.3) | 0 | 0 | 0.14 |
| Key investigations | ||||
| Creatinine, mg/dL (mean ± SD) | 1.17 ± 0.6 | 1.2 ± 0.6 | 1.05 ± 0.47 | 0.42 |
| CK-MB, (mean ± SD) | 112 ± 98 | 71 ± 57 | 25 ± 24 | 0.001 |
| Fibrinogen, gm/L (mean ± SD) | 6.3 ± 1.2 | 5.3 ± 1.1 | 5.3 ± 1.3 | 0.001 |
| Albumin, gm/dL (mean ± SD) | 3.3 ± 0.33 | 3.4 ± 0.36 | 3.5 ± 30 | 0.075 |
| FAR (mean ± SD) | 19.1 ± 4.8 | 15.4 ± 4.0 | 15.1 ± 4.3 | 0.001 |
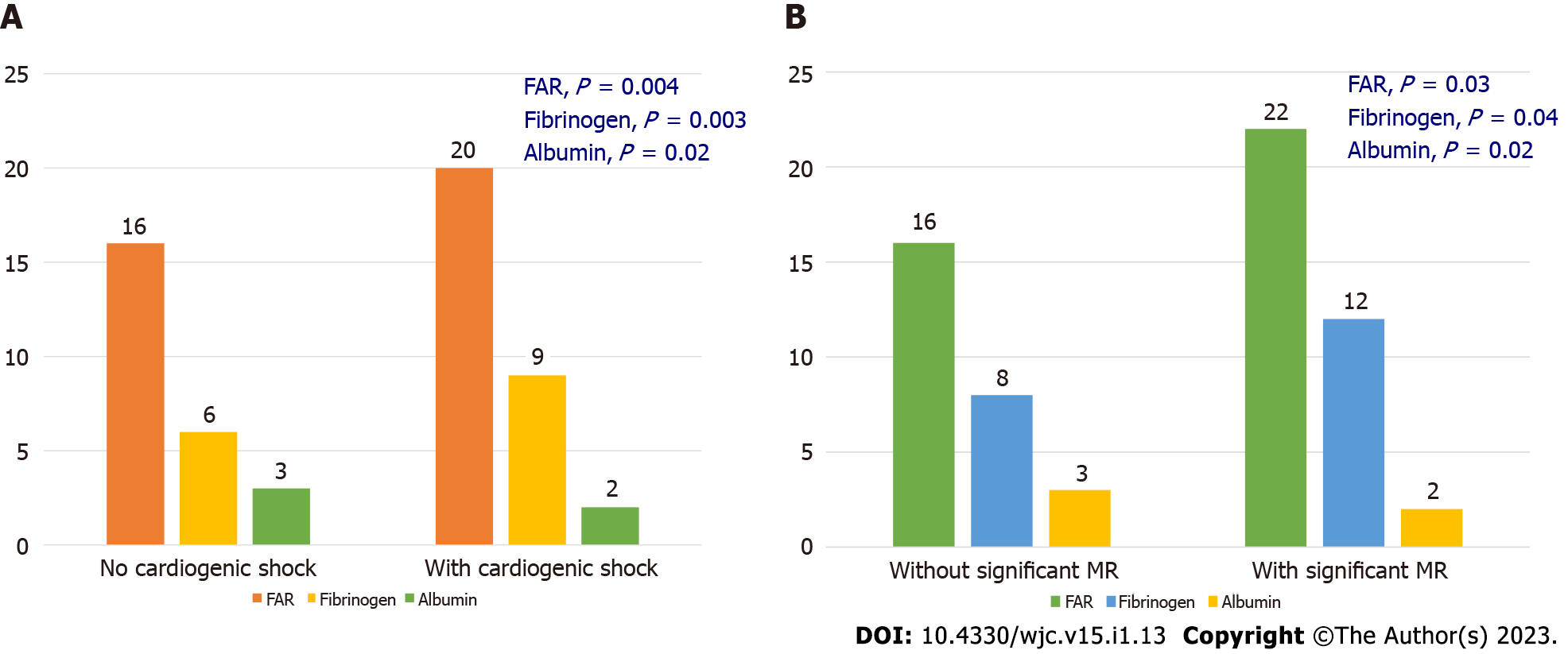
Fibrinogen levels were significantly elevated in patients with STEMI compared to NSTEMI and USA (6.3 ± 1.2 vs 5.3 ± 1.1 and 5.3 ± 1.3 in gm/L, respectively; P = 0.001). FAR was found to be significantly higher in patients with STEMI (19.1 ± 4.8) compared to NSTEMI (15.4 ± 4) and USA (15.1 ± 4.3), P = 0.001. Patients with significant ischemic MR and classical CS or worse at presentation had significantly higher levels of fibrinogen and FAR and lower level of albumin as shown in Table 1.
Angiography showed complete occlusion of culprit artery more commonly in patients with STEMI compared to NSTEACS 41% vs 21%, P = 0.019. Among patients with STEMI, a fibrinogen value of ≥ 6.55 gm/dL predicted TIMI ≤ 1 flow in the culprit artery with a sensitivity of 74.4% and specificity of 74.2% [area under the receiver operating characteristic curves (AUROC) = 0.805, P < 0.001]. FAR also predicted total occlusion of culprit artery with a higher accuracy compared to fibrinogen. A FAR value ≥ 19.2 had a 76.9% sensitivity and 78.2% specificity in predicting TIMI ≤ 1 flow in the culprit artery (AUROC = 0.808, P < 0.001). Similar to STEMI patients in NSTEACS too, both fibrinogen and FAR were able to predict total occlusion of culprit artery as shown in Figure 1. Fibrinogen ≥ 6.10 gm/dL had a 75.3% sensitivity and 55.6% specificity (AUROC of 0.68, P = 0.024) in predicting ≤ TIMI -1 flow in the culprit artery in NSTEMI patients, while fibrinogen alone was not able to predict complete occlusion in patients with USA. Likewise, FAR ≥ 18.85 predicted ≤ TIMI -1 flow in the culprit artery with a greater accuracy than fibrinogen [80% sensitivity and 63% specificity (AUROC of 0.715, P = 0.006)] in patients with NSTEMI. FAR ≥ 17.3 predicted < TIMI -1 flow in culprit artery with 76.4 % sensitivity and 54.3% specificity in patients with USA. Further FAR correlated with angiographic severity as determined by the SYNTAX scores. FAR increased significantly with increasing SYNTAX scores. Accordingly, the FAR values in low SYNTAX (< 22), intermediate SYNTAX (22-33) and high SYNTAX (> 33) groups were 15.8 ± 2.9, 18.4 ± 3.3 and 22.9 ± 4.2 respectively (P < 0.001).
The mean FAR and fibrinogen was significantly higher and mean serum albumin was significantly lower in patients with CS and significant ischemic mitral regurgitation as shown in Table 2 and Figure 2. The overall, 30-d mortality among patients of ACS was higher in patients with was 9.5% in STEMI compared to NSTEACS 2.8%, P = 0.004. Among inflammatory markers albumin was significantly less in patients who succumbed to illness compared to survivors (3.2 ± 0.33 vs 3.4 ± 0.33, P = 0.03). Another inflammatory biomarker assessed in our study was the CRP. CRP levels were significantly higher in non-survivors compared to survivors (56.4 ± 24.3 vs 35.2 ± 18.4, P = 0.04). However, there was no correlation of CRP with angiographic severity or the TIMI flow in our study. Thirty-day mortality of the cohort was 6.6%. MACCE occurred in 10.3% patients at a mean follow up of 6.6 ±1.5 mo.
| Patients with TIMI- ≤ 1 flow (n = 54) | Patients with TIMI- ≥ 2 flow (n = 98) | P value | |
| Age, yr | 60.5 ± 10.2 | 60.5 ± 10.7 | 0.9 |
| Time of presentation to hospital after chest pain onset (h) | 13.4 ± 11.2 | 12.3 ± 8.8 | 0.24 |
| Hypertension | 33 (61) | 71 (65) | 0.3 |
| Active smokers | 16 (29.6) | 36 (32.4) | 0.3 |
| EF < 30% | 23 (42.6) | 33 (29.7) | 0.1 |
| Cardiogenic shock | 10 (18.5) | 15 (13.5) | 0.4 |
| Complete heart block | 8 (14.8) | 7 (6.3) | 0.07 |
| Time to initiation of medical treatment, h | 77.3 ± 63 | 74.5 ± 66 | 0.87 |
| Time to angiography, h | 107 ± 79 | 113 ± 141 | 0.84 |
| CK-MB | 101.2 ± 90 | 75 ± 83.4 | 0.11 |
| Platelet (× 109/L) | 1.89 ± 0.7 | 2.0 ± 0.91 | 0.17 |
| Procalcitonin (ng/mL) | 0.59 ± 0.7 | 1.0 ± 2.6 | 0.27 |
| TLC (× 109/L) | 10.6 ± 3.8 | 10.7 ± 3.9 | 0.8 |
| CRP (mg/dL) | 47.2 ± 34.3 | 39.7 ± 28.4 | 0.16 |
| Fibrinogen (gm/L) | 6.9 ± 1.04 | 5.4 ± 1.2 | 0.001 |
| Albumin (gm/dL) | 3.3 ± 0.35 | 3.4 ± 0.32 | 0.014 |
| FAR | 21.1 ± 3.9 | 15.6 ± 4.1 | 0.001 |
In last sixty years, since first biomarkers of ACS were identified, their role has undergone drastic change and are now integral to management of ACS patients. They not only have a role in early diagnosis but also provide means to gain insights to underlying causes and consequences of ACS. Novel biomarkers are coming up at a rapid rate including myeloperoxidase, pregnancy-associated plasma protein-A, matrix mettaloproteinases, tissue inhibitor of mettaloproteinases, various interleukins and the novel exosomal micro RNAs[18]. However, the long turn-around time and easy accessibility besides the high cost makes them impractical for real-world use.
Pre procedural TIMI flow in culprit artery is strongly related to patient outcomes[19,20]. SR of culprit artery in STEMI patients occurs in 26% those undergoing primary PCI[21]. SR of culprit artery results from endogenous fibrinolytic system leading to dissolution of arterial thrombi. The ST resolution on 12-lead electrocardiogram is not a reliable marker to predict SR, thus necessitating the development of other biomarkers which can help in early identification of the recanalization status of the vessel and guide in patient management and prognostication[22]. Various biomarkers have been tested to predict SR; however, the results are dismal. In our study fibrinogen and FAR were able to predict total occlusion of culprit artery in STEMI with reasonably good accuracy.
The statistics on revascularization by thrombolysis or primary PCI are dismal in the country. Thrombolysis is performed in around 50% patients of STEMI while primary PCI is performed in less than 15% patients in our country[12]. COVID-19 deepened the crises further and these figures are likely to get worse during and post pandemic[6,23,24]. Moreover, the number of patients presenting late to medical facilities after STEMI are likely to increase. It has been seen that patient presenting with STEMI and occluded artery TIMI flow ≤ 1 fear worse as compared to those who have SR and benefit most from early invasive strategy[19,20]. Hence, the importance of early identification of TIMI flow in culprit arteries.
In NSTEACS complete occlusion of culprit artery varies from 19% to 30%. These patients are at increased risk of mortality and adverse events. Risk scoring systems and electrocardiogram are not able to identify these high-risk patients[25]. In our study similar to STEMI, both fibrinogen and FAR were able to identify patients with total occlusion in NSTEACS with reasonable accuracy. Identification of this high-risk group is rather difficult with the currently available tools. Easily accessible, readily available, cost-effective biomarkers can help better manage these patients.
High thrombus burden has remained Achilles-heel of coronary intervention since its advent in 1977[26]. Fibrinogen being precursor of fibrin has been shown to be precursor of thrombosis, inflammatory response during ACS often leads to structural changes in fibrinogen rendering it resistant to fibrinolysis[27]. Albumin also apart from being a reflection of ongoing inflammation has pathophysiological role in thrombosis[28]. In our study only albumin amongst inflammatory biomarkers could predict short term mortality, this was similar to earlier studies showing hypoalbuminemia to be predictor of poor prognosis in patients with ACS and other cardiovascular diseases[29,30]. Thus, these inflammatory biomarkers are not merely bystanders of ongoing inflammation but have potential role in pathophysiology of ACS. The pandemic has made a call for an efficient triage system for better management of cardiac emergencies to avoid putting a strain on already this health care resources in the country. Accordingly, low risk (those who have SR) NSTEACS and STEMI should be managed medically initially while the high-risk group should receive an early invasive strategy. Using fibrinogen, albumin and their composite (FAR) could enable us to better understand and identify these high-risk ACS patients as was shown in the index study.
Our study is a single center study, with a small sample size. Thus, to generalize our results to a large population is not feasible. Serial sampling of these biomarkers was not done to assess their change in level with clinical improvement or deterioration.
To efficiently manage cardiovascular emergencies in a resource constrained setting like ours, there is an ardent need to identify patients at high risk and prioritize resource allocation. Our study shows that by using old, easily available biomarkers we can effectively triage and identify this high-risk subgroup. This should pave way for further large-scale studies to affirm role of fibrinogen and FAR in predicting total occlusion of the culprit artery in patients with ACS.
Despite the obvious progress in our management of acute coronary syndrome (ACS), it continues to be the leading cause of death worldwide with considerable short and long-term mortality and morbidity. The situation is dismal in the developing world where the health care resources are scarce. There is dire need for resource sensitive, readily available, realiable and easlity affordable biomarkers to enable appropriate resource allocation in cardiac emergencies.
The coronavirus disease 2019 (COVID-19) pandemic has highlighted the huge deficit in health care resources worldwide and made a strong case developing efficient triaging and risk-assessment for effective patient management.
The present study aimed to study the applicability of the old, available and affordable nonconventional biomarkers: albumin and fibrinogen in their ability to predict angiographic severity and clinical outcomes in patients with ACS.
In this prospective, observational study, 166 consecutive patients with ACS were enrolled. Fibrinogen, albumin and their ratio were determined from serum. Patients with underlying chronic liver disease, active malignancy, autoimmune disease, active COVID-19 infection and undergoing thrombolysis were excluded.
Mean age of the population was 60.5 ± 1.5 years, 74.1% being males. ST elevation myocardial infarction (STEMI) was most common presentation of ACS seen in 57% patients. Fibrinogen albumin ratio (FAR) ≥ 19.2, had a sensitivity of 76.9% and specificity of 78.9 % [area under the receiver operating characteristic curves (AUROC) = 0.8, P = 0.001] to predict ≤ TIMI 1 flow in culprit artery in STEMI patients. Even in non-STEMI patients, FAR ≥ 18.85 predicted the same with 80% sensitivity and 63% specificity (AUROC=0.715, P = 0.006).
Our study has shown that readily available biomarkers like fibrinogen and albumin and their ratio can help identify these high-risk patients with good accuracy. This allows risk-stratification and individualization of treatment in ACS.
Our study makes a strong case for the readily available and cost-effective biomarkers: Fibrinogen, albumin and their ratio (FAR) to guide appropriate clinical decision making in real world setting. It showed excellent accuracy for predictive angiographic severity and outcomes which are the most valuable piece of Information any clinician needs.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American college of Cardiology, No. 3445007; European society of Cardiology, No. 1036629.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Su G, China; Xia M, China S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Lee E, Choi EK, Han KD, Lee H, Choe WS, Lee SR, Cha MJ, Lim WH, Kim YJ, Oh S. Mortality and causes of death in patients with atrial fibrillation: A nationwide population-based study. PLoS One. 2018;13:e0209687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 135] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 2. | Amini M, Zayeri F, Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. 2021;21:401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 350] [Article Influence: 87.5] [Reference Citation Analysis (0)] |
| 3. | Bhatnagar P, Wickramasinghe K, Wilkins E, Townsend N. Trends in the epidemiology of cardiovascular disease in the UK. Heart. 2016;102:1945-1952. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 215] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 4. | Kumar B, Agstam S, Vijay J, Batta A. Long term safety and efficacy of the Yukon Choice Flex sirolimus-eluting coronary stent-a real-world data from India. Indian Heart J. 2021;73:733-736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (6)] |
| 5. | Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982-3021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6994] [Cited by in RCA: 6383] [Article Influence: 1276.6] [Reference Citation Analysis (0)] |
| 6. | Bhaskar S, Rastogi A, Chattu VK, Adisesh A, Thomas P, Alvarado N, Riahi AD, Varun CN, Pai AR, Barsam S, Walker AH. Key Strategies for Clinical Management and Improvement of Healthcare Services for Cardiovascular Disease and Diabetes Patients in the Coronavirus (COVID-19) Settings: Recommendations From the REPROGRAM Consortium. Front Cardiovasc Med. 2020;7:112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 7. | Klingenberg R, Aghlmandi S, Liebetrau C, Räber L, Gencer B, Nanchen D, Carballo D, Akhmedov A, Montecucco F, Zoller S, Brokopp C, Heg D, Jüni P, Marti Soler H, Marques-Vidal PM, Vollenweider P, Dörr O, Rodondi N, Mach F, Windecker S, Landmesser U, von Eckardstein A, Hamm CW, Matter CM, Lüscher TF. Cysteine-rich angiogenic inducer 61 (Cyr61): a novel soluble biomarker of acute myocardial injury improves risk stratification after acute coronary syndromes. Eur Heart J. 2017;38:3493-3502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Klingenberg R, Aghlmandi S, Räber L, Gencer B, Nanchen D, Heg D, Carballo S, Rodondi N, Mach F, Windecker S, Jüni P, von Eckardstein A, Matter CM, Lüscher TF. Improved risk stratification of patients with acute coronary syndromes using a combination of hsTnT, NT-proBNP and hsCRP with the GRACE score. Eur Heart J Acute Cardiovasc Care. 2018;7:129-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 9. | Kulkarni P, Mahadevappa M, Alluri S. COVID-19 Pandemic and the Impact on the Cardiovascular Disease Patient Care. Curr Cardiol Rev. 2020;16:173-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Cannata A, Watson SA, Daniel A, Giacca M, Shah AM, McDonagh TA, Scott PA, Bromage DI. Impact of the COVID-19 pandemic on in-hospital mortality in cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. 2022;29:1266-1274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 11. | Mohanan PP, Mathew R, Harikrishnan S, Krishnan MN, Zachariah G, Joseph J, Eapen K, Abraham M, Menon J, Thomas M, Jacob S, Huffman MD, Prabhakaran D; Kerala ACS Registry Investigators. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34:121-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 181] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 12. | Arramraju SK, Koganti S, Janapati R, Emmareddy SK, Mandala GR. The report on the Indian coronary intervention data for the year 2017-National Interventional Council. Indian Heart J. 2019;71:146-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Ye XD, He Y, Wang S, Wong GT, Irwin MG, Xia Z. Heart-type fatty acid binding protein (H-FABP) as a biomarker for acute myocardial injury and long-term post-ischemic prognosis. Acta Pharmacol Sin. 2018;39:1155-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 92] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 14. | Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40:237-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1021] [Cited by in RCA: 1047] [Article Influence: 149.6] [Reference Citation Analysis (1)] |
| 15. | Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64:e139-e228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1840] [Cited by in RCA: 2198] [Article Influence: 199.8] [Reference Citation Analysis (0)] |
| 16. | Jentzer JC, van Diepen S, Barsness GW, Henry TD, Menon V, Rihal CS, Naidu SS, Baran DA. Cardiogenic Shock Classification to Predict Mortality in the Cardiac Intensive Care Unit. J Am Coll Cardiol. 2019;74:2117-2128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 377] [Article Influence: 62.8] [Reference Citation Analysis (0)] |
| 17. | TIMI Study Group. The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. N Engl J Med. 1985;312:932-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2767] [Cited by in RCA: 2788] [Article Influence: 69.7] [Reference Citation Analysis (0)] |
| 18. | Wu Y, Pan N, An Y, Xu M, Tan L, Zhang L. Diagnostic and Prognostic Biomarkers for Myocardial Infarction. Front Cardiovasc Med. 2020;7:617277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 19. | Stone GW, Cox D, Garcia E, Brodie BR, Morice MC, Griffin J, Mattos L, Lansky AJ, O'Neill WW, Grines CL. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation. 2001;104:636-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 337] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 20. | Kim YH, Her AY, Jeong MH, Kim BK, Hong SJ, Kim S, Ahn CM, Kim JS, Ko YG, Choi D, Hong MK, Jang Y. Two-Year Clinical Outcomes According to Pre-PCI TIMI Flow Grade and Reperfusion Timing in Non-STEMI After Newer-Generation Drug-Eluting Stents Implantation. Angiology. 2022;73:152-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | . Erratum for the Research Article "Recent global decline of CO(2) fertilization effects on vegetation photosynthesis" by S. Wang, Y. Zhang, W. Ju, J. M. Chen, P. Ciais, A. Cescatti, J. Sardans, I. A. Janssens, M. Wu, J. A. Berry, E. Campbell, M. Fernández-Martínez, R. Alkama, S. Sitch, P. Friedlingstein, W. K. Smith, W. Yuan, W. He, D. Lombardozzi, M. Kautz, D. Zhu, S. Lienert, E. Kato, B. Poulter, T. G. M. Sanders, I. Krüger, R. Wang, N. Zeng, H. Tian, N. Vuichard, A. K. Jain, A. Wiltshire, V. Haverd, D. S. Goll, J. Peñuelas. Science. 2021;371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Verouden NJ, Haeck JD, Koch KT, Henriques JP, Baan J, van der Schaaf RJ, Vis MM, Peters RJ, Wilde AA, Piek JJ, Tijssen JG, de Winter RJ. ST-segment resolution prior to primary percutaneous coronary intervention is a poor indicator of coronary artery patency in patients with acute myocardial infarction. Ann Noninvasive Electrocardiol. 2010;15:107-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Fersia O, Bryant S, Nicholson R, McMeeken K, Brown C, Donaldson B, Jardine A, Grierson V, Whalen V, Mackay A. The impact of the COVID-19 pandemic on cardiology services. Open Heart. 2020;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 24. | Otaal PS, Batta A, Makkar K, Vijayvergiya R. Cardiovascular conundrums of COVID-19 pandemic. J Postgrad Med Educ Res. 2020;1-3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Khan AR, Golwala H, Tripathi A, Bin Abdulhak AA, Bavishi C, Riaz H, Mallipedi V, Pandey A, Bhatt DL. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis. Eur Heart J. 2017;38:3082-3089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 26. | Canfield J, Totary-Jain H. 40 Years of Percutaneous Coronary Intervention: History and Future Directions. J Pers Med. 2018;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 27. | Tadeusiewicz J, Nowak P. [The role of post-translational modification of fibrinogen in the pathogenesis of thrombosis]. Pol Merkur Lekarski. 2015;38:107-112. [PubMed] |
| 28. | Zoellner H, Höfler M, Beckmann R, Hufnagl P, Vanyek E, Bielek E, Wojta J, Fabry A, Lockie S, Binder BR. Serum albumin is a specific inhibitor of apoptosis in human endothelial cells. J Cell Sci. 1996;109 (Pt 10):2571-2580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 180] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 29. | Karki P, Agrawaal KK, Lamsal M, Shrestha NR. Predicting outcomes in acute coronary syndrome using biochemical markers. Indian Heart J. 2015;67:529-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 30. | Sharma YP, Batta A, Makkar K, Hatwal J, A Gawalkar A, Kaur N, Malhi TS, Kasinadhuni G, Gupta H, Panda P, Barwad P. Angiographic profile and outcomes in persistent non-valvular atrial fibrillation: A study from tertiary care center in North India. Indian Heart J. 2022;74:7-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (4)] |