Published online Sep 26, 2022. doi: 10.4330/wjc.v14.i9.508
Peer-review started: May 26, 2022
First decision: June 16, 2022
Revised: June 30, 2022
Accepted: August 16, 2022
Article in press: August 16, 2022
Published online: September 26, 2022
Processing time: 116 Days and 7.6 Hours
Q fever myocarditis is a rare disease manifestation of Q fever infection caused by Coxiella burnetii. It is associated with significant morbidity and mortality if left untreated. Prior studies have reported myocarditis in patients with acute Q fever. We present the first case of chronic myocarditis in an end-stage heart failure patient with chronic Q fever infection.
A 69-year-old male was admitted with dyspnea on exertion, hypotension and bilateral lower extremity edema for a few months. He has a past medical history of ischemic cardiomyopathy with left ventricular ejection fraction of 25%, implantable cardioverter defibrillator in place, bioprosthetic aortic valve and mitral valve replacement. He continued to have shortness of breath despite diur
Chronic Q fever myocarditis, if left untreated, carries a poor prognosis. It should be kept in differentials, especially in patients with recurrent fevers and contact with farm animals.
Core Tip: Q fever myocarditis is a rare disease (< 1% of cases) caused by infection with Coxiella burnetii (gram-negative proteobacteria). Q fever normally has a pleomorphic and non-specific clinical presentation which leads to delayed diagnosis and treatment, which can lead to worse outcomes. Q fever myocarditis should be kept in differentials not only in patients with acute Q fever but also with chronic Q fever infection, like in our case. Q fever serologies help in making a diagnosis of acute and chronic Q fever. Cardiac positron emission tomography and magnetic resonance imaging can be utilized to diagnose myocarditis in the setting of Q fever. Hydroxychloroquine and doxycycline, in combination, are used for treatment of Q fever myocarditis.
- Citation: Goyal A, Dalia T, Bhyan P, Farhoud H, Shah Z, Vidic A. Rare case of chronic Q fever myocarditis in end stage heart failure patient: A case report. World J Cardiol 2022; 14(9): 508-513
- URL: https://www.wjgnet.com/1949-8462/full/v14/i9/508.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i9.508
Q fever is caused by infection with gram-negative proteobacteria, Coxiella burnetii[1]. Coxiella burnetii is found in many domestic animals like deer, rabbits, rodents, birds, horses and even in arthropods like ticks[2]. Q fever is a zoonosis and is transmitted to humans via inhalation of contaminated aerosols[1]. C. burnetii can survive for extended periods of time and can be carried long distances via wind, hence direct animal contact may not be required for transmission[3]. Disease presentation is variable, ranging from asymptomatic, flu like symptoms to intensive care admission. The variability is mostly due to host factors, bacterial virulence factors and extent of exposure[1]. Myocarditis is a rare disease manifestation of acute Q fever (< 1% of cases)[1]. To the best of our knowledge, less than 30-35 isolated cases of myocarditis with Coxiella have been reported in the literature. However, no case of chronic myocarditis in Chronic Q fever infection has been reported. We present an interesting and rare case of chronic Q fever leading to chronic myocarditis in a patient with a prior history of ischemic cardiomyopathy and valvular heart disease.
A 69-year-old male presented with chief complaints of shortness of breath, fatigue, and intermittent fevers for the last 6 mo which were treated with antibiotics twice.
The patient’s symptoms of dyspnea and fatigue had been ongoing for the last few months with severe hypotension, bilateral lower extremity edema and dyspnea on exertion. He denied any chest pain or pressure.
The patient had several comorbidities including ischemic cardiomyopathy with left ventricular ejection fraction (LVEF) of 25%, prior ST-elevation myocardial infarction status post (s/p) stent to proximal left anterior descending artery, s/p implantable cardioverter defibrillator (ICD) in 2018 for primary prevention, bicuspid aortic valve s/p aortic valve replacement with 25 mm Carpentier-Edwards bioprosthetic prosthesis in October 2012 followed by transcatheter aortic bioprosthetic valve in valve (26 mm Sapien S3) in April 2019, mitral valve repair with 32 mm seguin ring repair in October 2012 and subsequent transcatheter bioprosthetic mitral valve replacement with 29 mm Sapien 3 bioprosthetic valve for mitral regurgitation in June 2019, hyperlipidemia, chronic kidney disease stage III and atrial fibrillation.
The patient denied pertinent family history.
On physical examination, the vital signs were as follows: T max of 100.04 degrees Fahrenheit, blood pressure of 91/61 mmHg, heart rate of 80/minute and oxygen saturation of 96% on room air. The patient’s jugular venous pressure was elevated, and a diastolic murmur was heard at the aortic area, bilateral bibasilar crackles at the lung bases, and minimal bilateral lower extremity edema was present.
Troponin-I level was 0.01 ng/mL (normal) and BNP was 1562 pg/mL. WBC count was normal and multiple blood cultures were negative.
ECG on admission showed atrial paced rhythm with left bundle branch block. Transthoracic echocardiogram (TTE) on admission showed LVEF of 20%-25% with global hypokinesis, mild to moderate aortic regurgitation, mitral valve mean gradient of 10 mmHg (@ HR of 72 bpm) with normal right ventricle size and function and no vegetation. His most recent TTE prior to admission was done at an outside facility on July 2019 and showed LVEF of 30%, no aortic valve or mitral prosthetic valve regurgitation, mean mitral valve gradient of 7 mmHg (@ HR of 67 bpm), and normal RV function. The chest X-ray on admission showed moderate cardiomegaly with central venous congestion and interstitial edema.
To determine his cardiac hemodynamics, shock profile, and whether escalation to temporary mechanical support device is needed, an urgent right heart catheterization was done on admission that showed right atrial pressure 12 mmHg, right ventricular oressure 54/6 mmHg, pulmonary artery pressure 54/25 mmHg, mean pulmonary artery pressure 35 mmHg, pulmonary capillary wedge pressure 24 mmHg and cardiac index by Fick of 2 L/min/m2 with pulmonary artery saturation of 57%. An infectious disease specialist was consulted. He underwent trans-esophageal echocardiogram to look for endocarditis. It showed a moderate paravalvular aortic valve regurgitation, the replaced mitral valve was functioning normally with no stenosis or regurgitation, and no definitive vegetation was noted on defibrillator leads and prosthetic material.
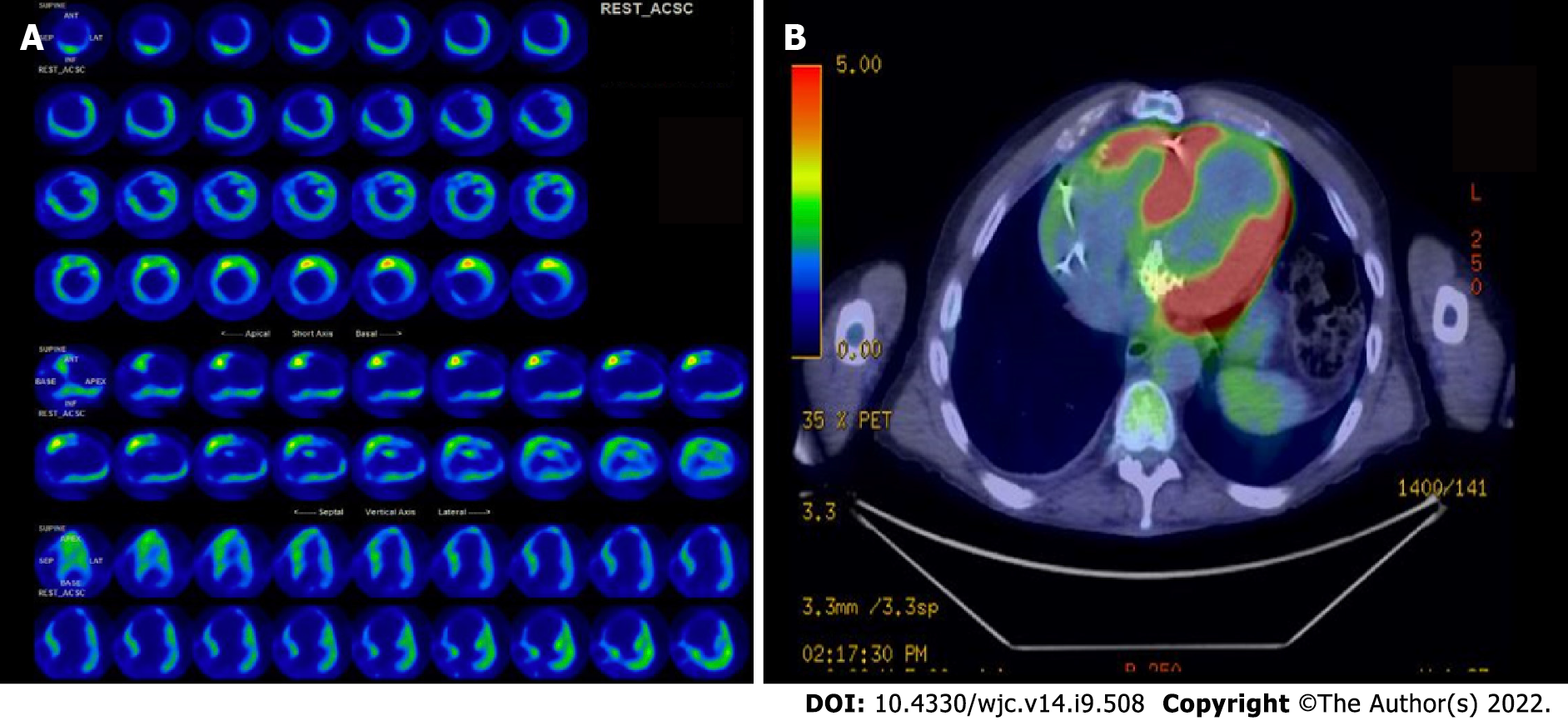
On further discussion with the patient’s wife, his functional status decline was associated with intermittent fevers for the last 6 mo that were treated with antibiotics twice, but no source was identified. On further questioning, the patient reported that he raised horses for the last 30 years and has been in close contact with dogs and cats his whole life. Due to close animal contact, Q fever was suspected. Q fever titers were significantly high: Phase I IgG (1:16384), Phase II IgG (>1:32768), Phase I IgM (1:>2048), and Phase II IgM (>1:2048). 18-Flourine fluorodeoxyglucose (FDG) cardiac positron emission tomography (PET) was preferred over magnetic resonance imaging (MRI) due to the presence of ICD. It revealed heterogenous areas of increased 18-F FDG uptake in the left ventricle raising the concern for myocarditis. The heterogenous uptake was identified in septal, lateral, and anterior walls of the left ventricle (Figure 1A). The basal anterolateral wall demonstrated maximum SUV of 6.9 and basal anteroseptal demonstrated maximum SUV of 5.3. No increased uptake around the valvular structures was noted.
Based on the history above, physical examination, laboratory findings, and discussions with our infectious disease colleagues, the most likely etiology of the patient’s presentation was chronic myocarditis secondary to chronic Q fever infection. Patient met criteria of both chronic Q fever and chronic myocarditis[4,5].
The patient was started on milrinone 0.125 mcg/kg/min and intravenous diuresis for his acute presentation of acute on chronic heart failure; however, it was stopped after a few days due to ventricular ectopies. Moreover, he did not feel any improvement in symptoms with milrinone. For the Q fever myocarditis, treatment with doxycycline 100 mg twice daily and hydroxychloroquine 200 mg three times daily was initiated for an 18-mo course. Prolonged treatment course was utilized due to his history of prosthetic valves. Due to the patient’s significant underlying comorbidities, our advanced heart failure therapy committee meeting deemed him an unsuitable candidate for advanced heart failure therapies at the time of admission. Due to his hypotension, he could not be discharged on guideline directed medical management.
On subsequent follow up clinic visits, the patient was noted to have significant improvement in his heart failure symptoms and his fevers resolved. Repeat Cardiac PET after 1 mo showed complete resolution (Figure 1B). The patient was doing better at 1 wk post discharge follow-up and his blood pressure improved. He was started on dapagliflozin 10 mg daily, losartan 25 mg daily and metoprolol XL 100 mg daily. At the patient’s 6-month routine follow up, he was doing well and repeat phase I and phase II titers were significantly down: Phase I IgG (1:16384), Phase II IgG (1:16384), Phase I IgM (1:256), and Phase II IgM (1:16) (Table 1). Repeat echocardiogram at 6 mo showed no change in the LVEF, no aortic regurgitation and no stenosis or regurgitation of the mitral valve. He will continue doxycycline and hydroxychloroquine for 18 mo.
| Variables | Reference range | Admission | 3 months | 6 months |
| Phase I IgG | <1:16 | 1:16384 | 1:32768 | 1:16384 |
| Phase II IgG | <1:16 | >1:32768 | 1:131072 | 1:16384 |
| Phase I IgM | <1:16 | >1:2048 | 1:1024 | 1:256 |
| Phase II IgM | <1:16 | >1:2048 | 1:2048 | 1:16 |
To the best of our knowledge, this is the first case of chronic myocarditis in a patient with chronic Q fever. Our patient suffered from chronic Q fever infection which ultimately led to chronic myocarditis. Certain conditions like immunosuppression, pregnancy, vascular abnormalities and heart valve conditions predispose individuals to chronic Q fever infection[1]. Our patient had significant valvular heart disease which may have been a predisposing factor for this chronic infection. Myocarditis secondary to Coxiella burnetii is a rare manifestation (< 1%)[6,7]. Chronic Q fever diagnosis can often be delayed for months due to nonspecific symptoms and pleomorphic presentation. Endocarditis is the most commonly reported cardiac pathology in chronic Q fever cases[5]. Myocarditis has been almost always reported in the setting of acute Q fever[8,9].
Myocarditis is most likely underestimated in this population due to non-specific signs and symptoms, and a high index of suspicion is required for diagnosis. The diagnosis of Q fever myocarditis is challenging as C. burnetii does not grow in routine cultures. Thus, serology is used in most cases for diagnosis[3,10]. C. burnetii displays a two-phase antigenic variation due to changes in lipopolysaccharide C antigens: Phase I (often seen in chronic Q fever) and phase II (often seen in acute Q fever). Indirect immunofluorescent assay is used for serological detection. Cut-off for serological titers varies between countries, but the screening test is generally considered positive for acute disease when anti-phase II IgG anti-immunoglobulins return active at a dilution of ≥1:200 or IgM ≥1:50[8]. These positive tests are then diluted and tested for presence of anti-phase I IgG and IgM. Chronic Q fever is found when phase I IgG ≥1:800, usually in the presence of anti-phase II antibodies[3,11]. Cardiac MRI and 18FDG-PET scan have been used before to diagnose Q fever myocarditis[12]. Another point worth mentioning is the negative troponin-I in our patient. Prior studies have shown negative troponin-I with biopsy proven myocarditis. The lack of troponin-I release does not rule out myocarditis[13]. There have been a few cases in the past showing Q fever infection leading to valvulitis[14], and this may explain the aortic regurgitation in our patient which got better with treatment of Q fever.
The prognosis of Q fever myocarditis is uncertain, but it has worse prognosis compared to other forms of Q fever diseases. In some studies, mortality with Q fever myocarditis has been reported to be up to 30%[8,15]. Patients with chronic C. burnetii are usually unable to eradicate the infection without utilizing antibiotics[1]. Center for Disease Control and Prevention recommends doxycycline 100 mg twice daily and hydroxychloroquine 200 mg three times a day for ≥ 18-24 mo as the treatment of choice for Q fever myocarditis, endocarditis or vascular infection[16,17]. Hydroxychloroquine is used mainly to increase the efficacy of doxycycline and prevents the development of chronic Q fever endocarditis. Although this regimen seems long, the addition of hydroxychloroquine has reduced the treatment time from 5 years to 18-24 mo[17]. Our patient was started on the long course of antibiotics to prevent endocarditis due to significant valvular abnormalities. Both doxycycline and hydroxychloroquine can cause photosensitivity, and patients should be warned to avoid excessive sun exposure. Regular heart and eye examinations are needed due to the risk of hydroxychloroquine induced retinopathy[16].
Q fever myocarditis is a rare disease, and a high index of suspicion is required for diagnosis. Given the poor prognosis of Q fever myocarditis and the presence of reliable therapy, it should be kept in differentials for patients with fevers and cardiomyopathy, especially in patients with a history of animal exposure. Multimodality imaging like echocardiogram, cardiac MRI and cardiac PET can be utilized in diagnosing myocarditis in patients with Q fever.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen C, China; Theerasuwipakorn N, Thailand S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Raoult D, Marrie T, Mege J. Natural history and pathophysiology of Q fever. Lancet Infect Dis. 2005;5:219-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 497] [Cited by in RCA: 514] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 2. | Seo MG, Lee SH, VanBik D, Ouh IO, Yun SH, Choi E, Park YS, Lee SE, Kim JW, Cho GJ, Kwon OD, Kwak D. Detection and Genotyping of Coxiella burnetii and Coxiella-Like Bacteria in Horses in South Korea. PLoS One. 2016;11:e0156710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Jacobson A, Sutthiwan P. Myocarditis: A rare manifestation of acute Q fever infection. J Cardiol Cases. 2019;20:45-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, Friedrich MG, Klingel K, Lehtonen J, Moslehi JJ, Pedrotti P, Rimoldi OE, Schultheiss HP, Tschöpe C, Cooper LT Jr, Camici PG. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy: An Expert Consensus Document. Circ Heart Fail. 2020;13:e007405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 344] [Cited by in RCA: 482] [Article Influence: 96.4] [Reference Citation Analysis (0)] |
| 5. | Kampschreur LM, Wegdam-Blans MC, Wever PC, Renders NH, Delsing CE, Sprong T, van Kasteren ME, Bijlmer H, Notermans D, Oosterheert JJ, Stals FS, Nabuurs-Franssen MH, Bleeker-Rovers CP; Dutch Q Fever Consensus Group. Chronic Q fever diagnosis— consensus guideline versus expert opinion. Emerg Infect Dis. 2015;21:1183-1188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Melenotte C, Protopopescu C, Million M, Edouard S, Carrieri MP, Eldin C, Angelakis E, Djossou F, Bardin N, Fournier PE, Mège JL, Raoult D. Clinical Features and Complications of Coxiella burnetii Infections From the French National Reference Center for Q Fever. JAMA Netw Open. 2018;1:e181580. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 91] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 7. | Steffen J, Bogner J, Huber BC. [Q-fever - a rare cause for myocarditis]. Dtsch Med Wochenschr. 2020;145:484-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Fournier PE, Etienne J, Harle JR, Habib G, Raoult D. Myocarditis, a rare but severe manifestation of Q fever: report of 8 cases and review of the literature. Clin Infect Dis. 2001;32:1440-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Hammami R, Bahloul A, Charfeddine S, Feki W, Ayed NB, Abid L, Kammoun S. Q fever presenting as myocarditis. IDCases. 2021;23:e01056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Murcia J, Reus S, Climent V, Manso MI, López I, Tello A. [Acute myocardial failure in a young man: Q-fever myocarditis]. Rev Esp Cardiol. 2002;55:875-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Scott JW, Baddour LM, Tleyjeh IM, Moustafa S, Sun YG, Mookadam F. Q fever endocarditis: the Mayo Clinic experience. Am J Med Sci. 2008;336:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Eldin C, Melenotte C, Million M, Cammilleri S, Sotto A, Elsendoorn A, Thuny F, Lepidi H, Roblot F, Weitten T, Assaad S, Bouaziz A, Chapuzet C, Gras G, Labussiere AS, Landais C, Longuet P, Masseau A, Mundler O, Raoult D. 18F-FDG PET/CT as a central tool in the shift from chronic Q fever to Coxiella burnetii persistent focalized infection: A consecutive case series. Medicine (Baltimore). 2016;95:e4287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Caforio ALP, Malipiero G, Marcolongo R, Iliceto S. Clinically suspected myocarditis with pseudo-infarct presentation: the role of endomyocardial biopsy. J Thorac Dis. 2017;9:423-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Deyell MW, Chiu B, Ross DB, Alvarez N. Q fever endocarditis: a case report and review of the literature. Can J Cardiol. 2006;22:781-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Eldin C, Mélenotte C, Mediannikov O, Ghigo E, Million M, Edouard S, Mege JL, Maurin M, Raoult D. From Q Fever to Coxiella burnetii Infection: a Paradigm Change. Clin Microbiol Rev. 2017;30:115-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 630] [Article Influence: 78.8] [Reference Citation Analysis (0)] |
| 16. | Alicia A HB, Pierre-Edouard F, Stephen G, Joshua H, Gilbert J, Gijs L, William L. N, Christopher P, Daniel S. Diagnosis and management of Q fever-United States. Recommendations and Reports. 2013;62. |
| 17. | Kersh GJ. Antimicrobial therapies for Q fever. Expert Rev Anti Infect Ther. 2013;11:1207-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |