Published online Jul 26, 2022. doi: 10.4330/wjc.v14.i7.392
Peer-review started: February 25, 2022
First decision: April 8, 2022
Revised: April 19, 2022
Accepted: June 24, 2022
Article in press: June 24, 2022
Published online: July 26, 2022
Processing time: 144 Days and 23.5 Hours
Coronavirus disease 2019 (COVID-19) is primarily an infection of the respiratory tract, but it can have multisystem manifestations. Cardiac complications of COVID-19 can range from acute myocardial injury, cardiac arrhythmias, or heart failure, amongst others. Heart failure (HF) in COVID-19 can be a de novo process or due to worsening of pre-existing cardiovascular ailment. HF in a patient with COVID-19 not only poses challenges in clinical presentation and management of COVID-19 but also affect prognosis of the patient. This article aims to succinctly revisit the implications of this pandemic regarding pre-existing HF or new-onset HF based on prevailing data. It also focuses on the management and special recommendations from prior studies and guidelines.
Core Tip: The mini-review is composed of assimilation of guidelines and current literature recommendations for managing heart failure in coronavirus disease 2019 (COVID-19) patients. We discuss many important aspects of heart-failure in COVID-19 from epidemiology to post recovery rehabilitation.
- Citation: Sharma M, Jagirdhar GSK, Guntupalli KK, Kashyap R, Surani S. Heart failure in general and cardiac transplant patients with COVID-19. World J Cardiol 2022; 14(7): 392-402
- URL: https://www.wjgnet.com/1949-8462/full/v14/i7/392.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i7.392
Since its emergence in December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has affected all continents. The case count of coronavirus disease 2019 (COVID-19) continues to soar to-date, as evident by more than 300 million global caseloads[1]. COVID-19 typically presents as a respiratory tract infection, but we have witnessed it herald a multisystem disorder in a lot of patients, including but not limited to the cardiovascular system. Cardiac manifestations of COVID-19 can be broad, and symptoms generally stem from myocardial injury, cardiac arrhythmias, cardiogenic shock, heart failure (HF), or sudden cardiac death[2-5]. This article attempts to provide a brief review of all the major topics related to heart failure and covid-19 from epidemiology, diagnostic tools to the important management options, and post-recovery rehabilitation. It gives insights on breakthrough vaccination and cardiac complications post COVID-19. It attempts to touch on treatment options in various situations encountered while treating heart failure patients.
An accurate incidence of HF in COVID-19 is difficult to determine as there are not abundant definitive data on it. HF in COVID-19 can be due to worsening of preexisting known or undiagnosed heart disease. Besides, it could also be a new onset HF due to hemodynamic stress, ischemic cardiomyopathy, or nonischemic cardiomyopathy. Available studies have not always clearly discerned a new-onset HF from worsening of chronic HF. As evident in Table 1, HF was present at baseline in up to 23% of cases while up to 7% of patients with COVID-19 had a new-onset HF as a complication of the infection[6-9]. However, we must bear in mind that there seems to be a wider range in these data reported. The other caveat is that not all studies have clearly demarcated the incidence and acuity of pure right heart failure from left heart failure to biventricular loss. Creel-Bulos C et al[10], described five patients with acute right HF in their case series from March 23 to April 4, 2020, in an intensive care unit in Georgia, United States. With the progression of the pandemic, Corica et al[11] conducted a combined pooled analysis of 3813 patients and found to have right HF in as high as 20.4% of patients with COVID-19.
| Ref. | Study type | Country of origin | Incidences |
| Zhou et al[6], 2020 | Retrospective cohort study | China | Total patients 191. deceased 54 patients (28 had chronic hf exacerbation, i.e., 52%) survived 137 patients (16 had chronic hf exacerbation, i.e., 12%) P < 0.0001 |
| Arentz et al[7], 2020 | Case series | United states | Total patients 21. nine patients (42.9%) acute on chronic hf |
| Ruan et al[8], 2020 | Multicenter retrospective analysis | China | Total patients 150. death 68 acute on chronic hf 5 (7%) |
| Shis et al[9], 2020 | Single-center cohort jan 2020 - feb 2020 | China | Total patients 416. new-onset heart failure 4.1% |
| Chen et al[12], 2020 | Retrospective study | China | Total patients 274. acute on chronic hf 1 (< 1%) new-onset hf 21 (7.7%). 1 recovered and 20 died |
| Inciardi et al[13], 2020 | Retrospective study | Italy | Total patients 99. acute on chronic hf 21 (21%) |
Two types of mechanisms for myocardial injury are described in prior literature. ie direct or specific and indirect effects[24].
SARS-CoV-2 directly attaches to the ACE2 on the myocardium and causes cell damage and death. It also decreases the protective and anti-inflammatory properties of ACE2 on the myocardium through its downregulation.
Sympathetic activity causing Tachycardia from underlying infection, prolonged immobility causing coagulopathy, hypoxemia, hemodynamic changes are indirect effects worsening the cardiac status[24]. Severe inflammatory response causing surge of cytokines like Interleukins, Tumor necrosis factor, interferons' play a major role in the pathogenesis of pulmonary and myocardial damage leading to acute respiratory distress syndrome (ARDS) and various cardiac complications[25]. It can precipitate new cardiac failure and worsen the course in underlying failure patients[25].
Pre-existing HF can exacerbate during COVID-19, as evident in other viral illnesses such as Influenza [15]. Stress cardiomyopathy, vasculitis, thrombosis of coronary arteries, fissuring, and rupture of atheromatous plaque leading to acute myocardial ischemia can be some of the ischemic and nonischemic causes of acute cardiomyopathy and subsequent HF[16,17]. One study evaluated that cardiogenic shock resulting from myocardial injury occurred in up to 10% of patients in shock and can result in worse prognosis compared to hypovolemic or distributive shock in COVID-19 patients[26]. 48% of patients had normal Ejection fraction and low cardiac index shock from low end diastolic volumes which was due to use of Peak end expiratory pressures and mechanical ventilation causing decreased venous return. Cytokine storm detailed above can result in distributive shock[26]. Pulmonary embolism from coagulopathy and pericardial tamponade can cause obstructive shock which are reported in COVID-19. Worsening of chronic kidney disease or onset of acute kidney injury leading to volume overload has been reported in up to 29% of patients with COVID-19 and chronic HF[6,18].
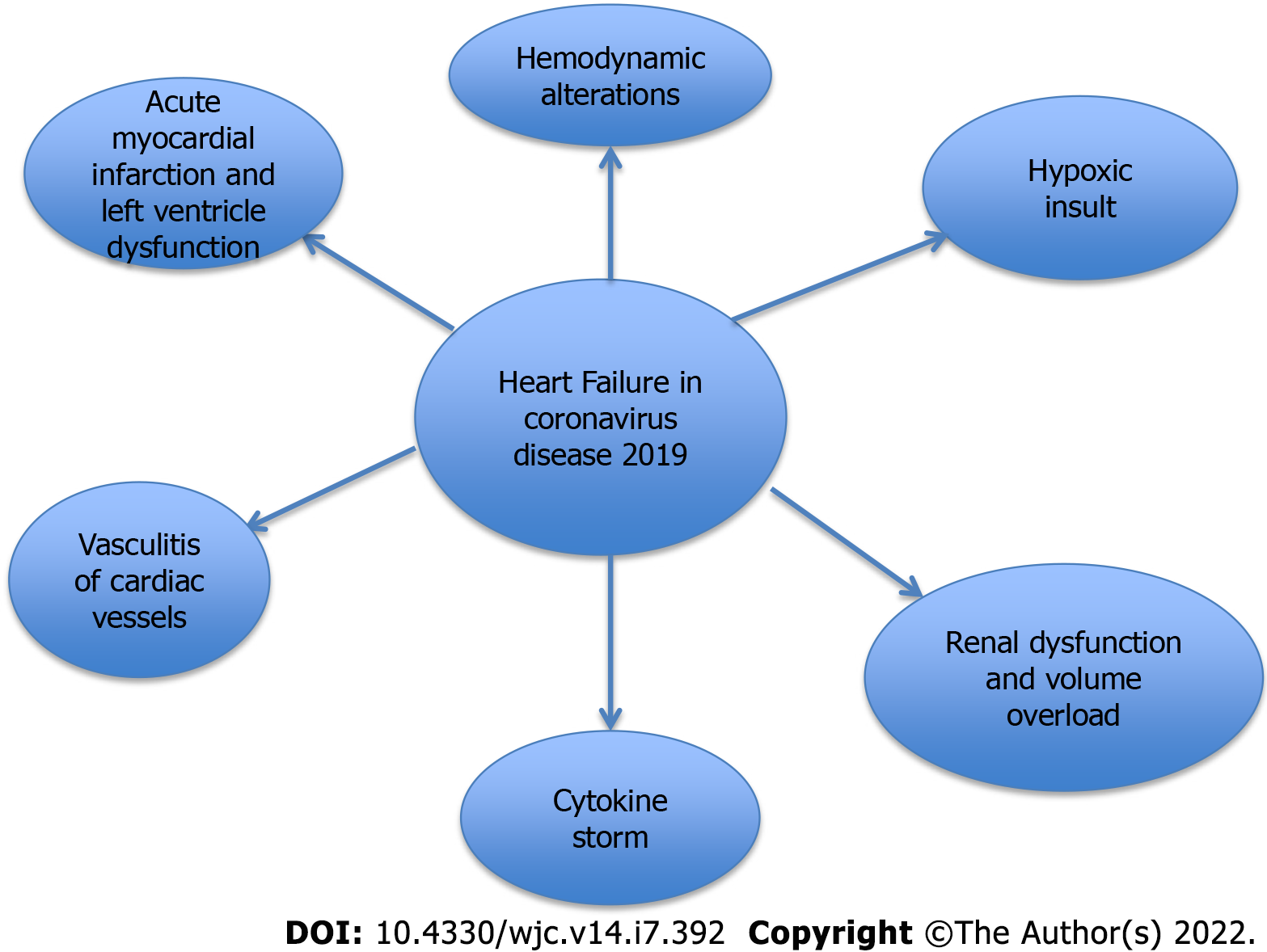
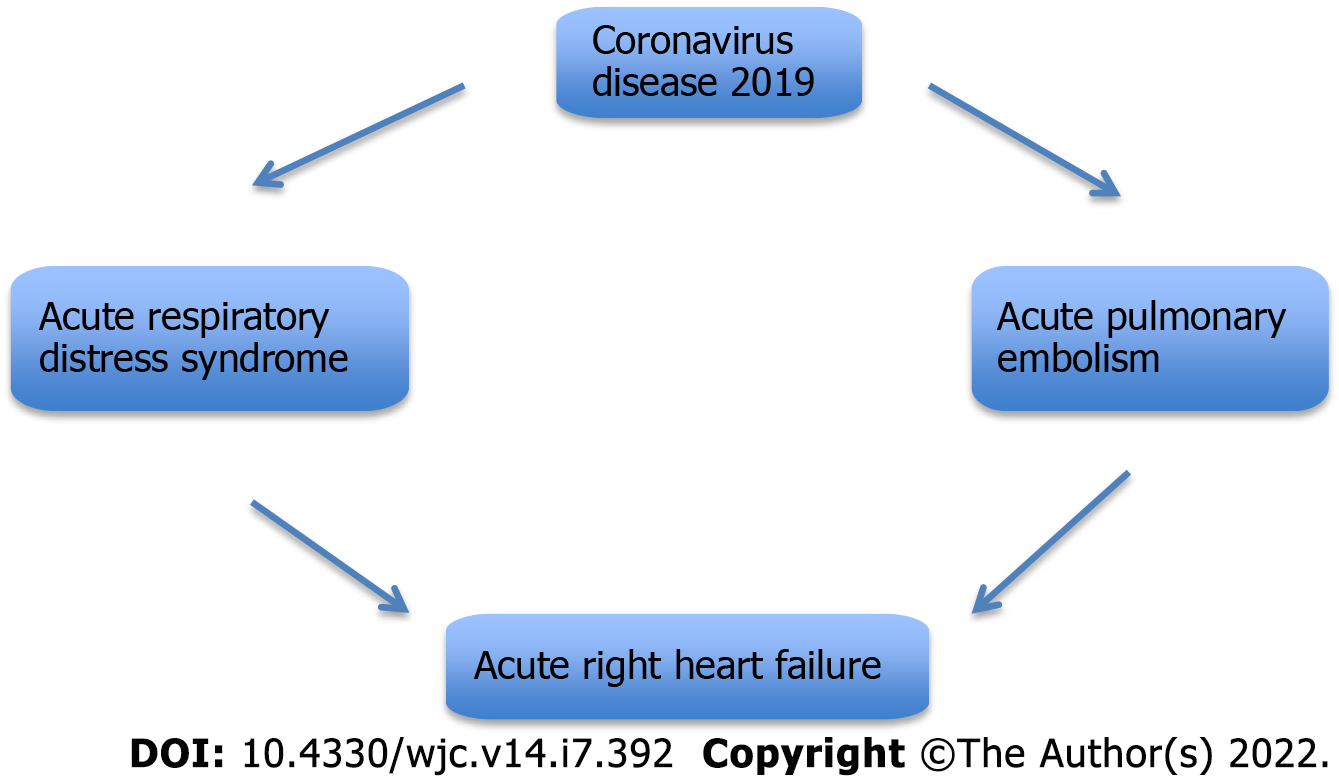
Acute right heart failure (RHF) in COVID-19 has been primarily thought to be due to ARDS and severe hypoxemia. RHF due to acute pulmonary embolism has also been reported in 5%-22% of cases by different authors[19,20]. High clot burden was also found in patients with right heart strain from pulmonary embolism[21]. Patients with COVID-19 are several times at higher risk of pulmonary embolism compared to non-COVID-19 patients and is also associated with higher mortality[20]. Severe Acute Respiratory distress syndrome may lead to pulmonary hypertension and cause right-sided heart failure. Myocardial injury and myocarditis can also weaken the right heart ventricle in COVID-19. Right heart failure in COVID-19 is associated with increased mortality[22,23] Etiopathology of HF in COVID-19 has been summarized in inline diagrams in Figures 1 and 2.
Symptoms of HF, in general, can be due to reduced cardiac output causing fatigue and weakness. It could also be due to excessive fluid accumulation resulting in dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, and edema. Patients in cardiogenic shock could have a low cardiac output state. Overall, it can be difficult to accurately distinguish most of the symptoms of HF from COVID-19 itself, so careful examination and use of diagnostic tools are imperative. Signs of fluid overload like weight gain, Jugular venous distension, fine crackles at lung bases, wheezing, third heart sound, abdominal distension, ascites, and pitting pedal edema can be used as important clues at the bedside to determine new-onset or exacerbation of HF in COVID-19 patients.
Plasma B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-pro BNP) are useful laboratory markers in suspected HF. High sensitivity troponins (hs-cTn) are often elevated as a marker of myocardial inflammation[16]. BNP less than 100 pg/mL and NT-proBNP less than 450 pg/mL have high negative predictive for HF[27]. Elevated plasma BNP and NT-proBNP also indicate poor prognosis in general, and this relationship holds true for HF in COVID-19 as well[28]. Elevated NT-proBNP level was detected in 12.9% of 3219 patients in a study from Wuhan, China. The adjusted hazard ratio for NT-proBNP was 5.71 (95%CI 3.50-7.47)[29]. In another study conducted on 397 patients with COVID-19 in Milan, Italy, 14.9% had elevated BNP levels, and the mortality rate was higher by 33.9% in these patients[30]. Elevation of BNP, NT-Pro BNP or troponin, hs-cTn should be interpreted with caution. It should not trigger evaluation for heart failure or Myocardial infarction unless patients have accompanying signs and symptoms or EKG changes to suggest diagnosis.
Electrocardiogram (EKG) may not receive ample attention in the diagnosis of HF beyond the milieu of a cardiologist. Perhaps, it is highly unlikely that a patient with a normal EKG will have a dysfunctional left ventricle (LV). Atrial fibrillation, old myocardial infarction, left ventricular hypertrophy, axis deviation, bundle branch block, and ST-T wave abnormalities may hint towards underlying acute or chronic HF in patients with COVID-19[16]. EKG changes commonly observed in COVID-19 patients were atrial fibrillation or flutter, Premature atrial (APCs) and ventricular contractions, Bundle branch block, interventricular conduction delay, and repolarization abnormalities[31]. Abnormal EKGs changes like APCs, Right BBB/Intraventricular block, Ischemic T wave inversions, and non-specific repolarization abnormalities were associated with an increased risk of adverse cardiac events or death in patients with underlying comorbidities like cardiovascular or renal diseases[31,32].
An echocardiogram is one of the most important diagnostic tools for HF. There have been some studies utilizing echocardiograms in patients with COVID-19. Szekely et al[33], performed an echocardiogram in 100 patients within 24 h of hospitalization with COVID-19. 32% of patients had a normal echocardiogram, 39% had right ventricle (RV) dilatation and dysfunction, 16% had LV diastolic dysfunction, and 10% had LV systolic abnormality. Reassessment with echocardiogram due to deterioration during hospital course showed worsening of RV failure in 12 patients and LV systolic failure in 5 patients[33]. In a prospective international study of 1216 patients from 69 countries, 667 patients (55%) were found to have an abnormal echocardiogram. 479 (39%) had LV dysfunction while 397 (33%) had RV dysfunction. Echocardiography findings changed management in 33% of these patients[34]. In an International multicenter study of 305 patients admitted with COVID-19, RV dysfunction was found in 26.3%, LV diastolic dysfunction in 13.2%, and LV global systolic dysfunction in 18.4% of patients. Moreover, multivariate adjustments showed that myocardial injury with abnormal echocardiograms represented higher mortality in comparison to normal echocardiograms[35]. Hence, an echocardiogram is a vital diagnostic tool that should be used by clinicians taking care of COVID-19 patients in a timely and appropriate manner. The Trans-thoracic echocardiogram has also been performed successfully among COVID-19 patients with ARDS who were in prone position by temporarily deflating the lower thoracic portion of the air mattress. This helps in placing the probe between the thorax and the mattress surface[36].
The role of cardiac magnetic resonance imaging (MRI) has been so far more relevant in patients that are on the road to recovery from acute COVID-19 illness. Because of inflammatory cardiomyopathy, some of these patients can develop HF as a sequela. In a German study of 100 patients that were in the recovery phase from acute COVID-19 illness, cardiac MRI was abnormal in 78% of patients at an average of 71 days from initial diagnosis. Compared to the control group, these patients had lower LV and RV ejection fractions. Furthermore, endomyocardial biopsy in three patients with elevated T1/T2 signal, late gadolinium enhancement, and LV ejection fraction less than 50% revealed lymphocytic infiltration with no detection of the viral genome[37]. In another study of 148 patients with severe COVID-19 infection, cardiac MRI was done at a median of 68 days post-discharge from the hospital. The myocarditis-like scar was seen in 26%, and infarction was found in 54%, but 89% of these patients had normal LV function[38]. Thus, cardiac MRI and endomyocardial biopsy in selected COVID-19 patients may be of value in timely diagnosis and initiation of goal-directed medical therapy where HF arises as a late complication in subacute and chronic recovery phases (Table 2).
| Diagnostic tools | Likely heart failure | Likely COVID/ARDS |
| BNP/NT-Pro BNP and clinical findings | BNP > 100 pg/mL or NT-Pro BNP > 450 pg/mL Signs and symptoms of right and left heart failure | < 450 pg/mL Absence of signs and symptoms of volume overload |
| EKG | Abnormal ekg findings of LVH, LAE, Sinus tachycardia, LAD, RAD, AF, PVCs, BBB | Nonspecific findings or symptoms of pulmonary embolism, Right heart strain or myocardial ischemia |
| ECHO | Ejection Fraction%, RV dilatation and dysfunction, LV Diastolic dysfunction, LV global systolic dysfunction | Findings of pulmonary arterial hypertension; RV dysfunction, enlargement and abnormal contraction, septal dyskinesia. Acute Cor pulmonale |
| CMRI | Establishes ischemic vs nonischemic heart failure, quantification of ventricular function and scar burden | Distinguishes pulmonary vs extrapulmonary causes for acute respiratory distress syndrome |
Management of HF exacerbation during COVID-19 should be based on the volume status, the previous history of heart failure, and vital signs. Patients with heart failure and COVID-19 have worse hospitalization and in-hospital mortality outcomes in a systematic review and meta-analysis of 18 studies[39].
Shared decision-making among consultants is necessary to guide clinical management regarding immunosuppression, multiple treatments, multiorgan involvement, and associated complications in COVID-19.
Chronic heart failure patients have a higher risk of in-hospital complications like acute heart failure, acute renal failure, sepsis and length of stay, and in-hospital mortality[40,41].
Medications should be initiated per Guideline-directed medical therapy and continued. Special considerations exist for each class of drugs which are discussed below.
Diuretics in heart failure and COVID-19 help to decongest the lungs. Prior to starting diuretics, they require careful monitoring of the volume status by physical examination, BNP, and bedside ultrasound assessment for the IVC (inferior vena cava) collapsibility[42]. Pulmonary artery catheter, Echocardiography, and cardiac output monitoring are other methods for advanced hemodynamic monitoring in patients with complex hemodynamics. Conservative fluid strategy with judicious initiation or up-titration of diuretics with daily weights is recommended[43]. Aiming for a negative fluid balance is necessary for these patients. Watching for signs of hypotension and over diuresis which can result in kidney injury is necessary. Nephrotoxic medications should be used carefully along with diuretics, i.e., NSAIDs, Remdesivir, or nephrotoxic antibiotics like vancomycin[42,44]. If there is diuretic resistance, then ultrafiltration can be considered to treat heart failure and AKI[42].
It was hypothesized that medications associated with upregulation of ACE2 receptors could worsen the COVID-19 infection, which was not proven in further studies. Outcomes among heart failure patients were similar regardless of ACE inhibitor or ARB use[40].
Heart failure society of America/American College of Cardiology/American Heart Association guidelines recommends against adding or discontinuing these medications beyond the standard of practice in patients with preexisting heart failure, hypertension, or ischemic heart disease. However, careful decision-making and medication discontinuation should be done in acute kidney injury, hypotension, hyperkalemia, and shock on a patient-to-patient basis[45].
Carvedilol is the recommended beta-blocker in patients with heart failure and COVID-19 due to its anti-cytokine action[46,47]. However, these medications should not be started for COVID-19 and HF beyond the standard of practice. Assessment of hemodynamic stability is necessary before the initiation of beta-blockers[42]. Patients previously on beta-blockers can have inappropriate bradycardia with COVID-19. Dose changes should be made if patients develop a low output state[45]. Betablockers also help patients with sinus tachycardia and tachyarrhythmias[45]. Antiviral medications like Remdesivir and Tocilizumab can influence the pharmacokinetics of cardiovascular medications, increasing the risk of toxicities and arrhythmias.
Most of the indications for digoxin in HF with reduced ejection fraction are as a rate control agent in those with low blood pressure and atrial fibrillation[48]. Digoxin has antiviral and anti-inflammatory properties per prior literature[46]. Again, there is no recommendation to start patients with new-onset HF and COVID-19 on these medications beyond clinical practice. Digoxin levels should be closely monitored when given anti-viral medications and immunomodulators that may interact with it[42].
Consideration should be given for interaction between anticoagulants' current and emerging COVID-19 therapies. Monitoring the liver and kidney function is also necessary. Unfractionated Heparin or Low molecular weight heparin (LMWH) is the preferred anticoagulant in hospitalized patients with prior anticoagulation for other causes. It is particularly preferred in sick patients due to drug interactions with oral anticoagulants[45]. If oral anticoagulants are needed in less sick patients, switching to direct oral anticoagulants is preferred over Vitamin K antagonists. Prophylactic Anticoagulation with LMWH can be considered in all inpatients if there is no hemorrhagic risk[49].
Careful use in heart failure patients based on volume status and kidney function. Electrolytes should also be monitored.
Stopping GDMT, i.e., Beta-blockers, ACE/ARB, and mineralocorticoid receptor antagonists in patients with chronic heart failure with COVID, are associated with increased in-hospital mortality per prior studies[50]. If GDMT therapy has been discontinued inpatient for AKI or hemodynamic instability, during discharge of patients post heart failure exacerbation, they should be restarted as they have favorable outcomes in heart failure patients[50].They should follow up with the cardiologist or physician for heart failure to review and adjust the dose of GDMT.
Patients with heart failure have pulmonary edema superimposed on COVID-19 pneumonia. High BNP levels elevation in patients with ARDS indicates cardiogenic shock and pulmonary edema. Use of non-invasive ventilation and prone ventilation help to decrease pulmonary edema. Heart Failure patients are susceptible to hypoxia and ARDS and therefore may require intubation and lung-protective ventilation. These methods also help to manage right heart failure from ARDS[51].
The shock from sepsis and heart failure can develop. Dehydration and hypoperfusion can worsen symptoms. Clinical assessment, bedside echo, and monitoring of hemodynamics help in assessing the pathophysiology of shock. Volume status assessment, careful use of diuretics, and intravenous fluid repletion are needed. The greatest benefit of fluid resuscitation was seen in patients with signs of hypoperfusion who are in hypovolemic shock[26]. In patients with Mixed shock (cardiogenic and septic), vasopressors or inotropes should be started.
Norepinephrine is the preferred vasopressor agent for septic and cardiogenic shock, especially in hypotensive patients[51].If there are signs of low organ perfusion or severe decreased cardiac output, inotropes such as dobutamine and epinephrine can be added[51].Cardiac output monitoring helps in the selection and titration of inotropes and vasopressors.
Bedside, Intra-aortic balloon pump should be considered in severe cardiogenic shock refractory to vasopressors or inotropes[52]. ECMO as mechanical circulatory support is used in the setting of ARDS/hypoxemia with refractory cardiogenic shock in available centers[45,51].
Myocarditis in COVID-19: Patients can present with Heart failure symptoms. Inotropes and vasopressors, mechanical circulatory support, and mechanical ventilation can be used in severe cases.
Heart Transplant and Heart and lung transplant recipients are on immunosuppression with medications like calcineurin inhibitors, prednisone, and antimetabolites. They are prone to COVID-19 infection from immunosuppression and can have severe symptoms and outcomes[53,54]. For patients with mild symptoms, supportive treatment with the continuation of immunosuppression is recommended.
In patients with moderate to severe illness, anti-metabolites such as azathioprine and mycophenolate mofetil can be held inpatient per the international society of heart and lung transplantation recommendations[55].
These patients should be treated at a heart transplant center. After the infection resolves, careful monitoring is required when restarting immunosuppression in these patients due to effects from the allograft[53].
Breakthrough infections after the COVID-19 vaccination have been frequently observed in older patients and those with comorbidities. One study described close to 12% of breakthrough infections after vaccination[56]. In another study of 700 breakthrough cases close to 49% of the patients were symptomatic[57]. Despite increased breakthrough infection in this patient population, they did not develop disease severe enough to require supplemental oxygen or ICU admission[56,58].
Vaccinated people have a shorter duration of virus transmission, short symptom duration, and restricted tissue dissemination[59].
Chronic heart failure patients with breakthrough infections who are stable can be treated as outpatients with GDMT.
In the Post-Acute phase, exercise training should be done in these patients, considering oxygen saturation, heart rate, systolic blood pressure, and symptoms[60]. Cardiac rehabilitation includes a variety of programs such as aerobic endurance training, interval training (IT), High intensity IT and resistance training done around 2-5 times per week[60].Thoracic expansion exercises to increase lung ventilation and airway clearance are some of the recommended methods for respiratory rehabilitation in these patients. Home-based cardiac telerehabilitation- is another alternative strategy to follow for these patients. Psychological support and nutritional interventions should also be a part of rehabilitation programs[60].
Direct viral infection of the myocardium can cause myocardial injury and complications such as myocarditis and myocardial interstitial fibrosis[61,62]. System-wide inflammatory response and release of pro-inflammatory markers like Tumor necrosis factor, interleukin-6, and interleukin-1β are associated with direct myocardial injury and can cause myocardial infarction[24,63]. The prothrombotic state can result in acute coronary events[61,62]. Cardiac Arrhythmias such as atrial arrhythmias, bradyarrhythmia, and non-sustained ventricular tachycardia can occur due to inflammation of the myocardium, fibrosis, edema of interstitial tissues, medication side-effects, and myocarditis[61,62]. Atrial fibrillation can predispose patients to cardiogenic shock[62].
Patients who recover after severe COVID-19 are at high risk of Pulmonary hypertension, Diastolic dysfunction, and right heart failure[9,64]. Stress-induced cardiomyopathy or Takutsubo cardiomyopathy can develop from microvascular dysfunction and inflammatory response[65,66]. The summary of management is illustrated in Table 3.
| Management of heart failure |
| We should know that the development of heart failure in COVID-19 patients can complicate management and worsen the prognosis; Chronic heart failure patients have adverse outcomes compared to new-onset heart failure patients; GDMT guided medical therapy should be used in heart failure with individualized patient decision making based on hemodynamic status and development of complications; Avoiding over diuresis to prevent kidney injury and hypoperfusion is necessary; Watching for signs of deterioration and shock with early initiation of vasopressors in mixed shock should be practiced; Cardiac arrhythmias and acute myocardial infarction are some major complications to look out for.; Advanced hemodynamic monitoring helps to guide management in these patients; Post-recovery cardiac, pulmonary rehabilitation with psychological support and nutritional interventions is necessary |
Heart Failure can occur as a complication in patients with COVID-19 infection. It can worsen the course of COVID-19 and is associated with poor outcomes. It requires early diagnosis and appropriate management on a patient-to-patient basis. Continuing Guideline Directed medical therapy is recommended. We need to watch out for complications during its management. Post the acute phase of COVID physical, psychological and nutritional rehabilitation for these individuals is necessary to aid in recovery.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Chest Physician.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nazari N, Iran; Varshney K, Australia S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). [cited 20 April 2022]. Available from: https://coronavirus.jhu.edu/map.html. |
| 2. | Nicol M, Cacoub L, Baudet M, Nahmani Y, Cacoub P, Cohen-Solal A, Henry P, Adle-Biassette H, Logeart D. Delayed acute myocarditis and COVID-19-related multisystem inflammatory syndrome. ESC Heart Fail. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 3. | Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin. Eur Heart J. 2021;42:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 383] [Cited by in RCA: 469] [Article Influence: 117.3] [Reference Citation Analysis (0)] |
| 4. | Li Z, Shao W, Zhang J, Ma J, Huang S, Yu P, Zhu W, Liu X. Prevalence of Atrial Fibrillation and Associated Mortality Among Hospitalized Patients With COVID-19: A Systematic Review and Meta-Analysis. Front Cardiovasc Med. 2021;8:720129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Bua D, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S; Lombardia CARe Researchers. Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy. N Engl J Med. 2020;383:496-498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 436] [Cited by in RCA: 519] [Article Influence: 103.8] [Reference Citation Analysis (0)] |
| 6. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 565] [Reference Citation Analysis (1)] |
| 7. | Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA. 2020;323:1612-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1511] [Cited by in RCA: 1624] [Article Influence: 324.8] [Reference Citation Analysis (0)] |
| 8. | Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846-848. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2604] [Cited by in RCA: 3195] [Article Influence: 639.0] [Reference Citation Analysis (0)] |
| 9. | Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2428] [Cited by in RCA: 3009] [Article Influence: 601.8] [Reference Citation Analysis (1)] |
| 10. | Creel-Bulos C, Hockstein M, Amin N, Melhem S, Truong A, Sharifpour M. Acute Cor Pulmonale in Critically Ill Patients with Covid-19. N Engl J Med. 2020;382:e70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 158] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 11. | Corica B, Marra AM, Basili S, Cangemi R, Cittadini A, Proietti M, Romiti GF. Prevalence of right ventricular dysfunction and impact on all-cause death in hospitalized patients with COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11:17774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 12. | Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Ding C, Zhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2289] [Cited by in RCA: 2550] [Article Influence: 510.0] [Reference Citation Analysis (2)] |
| 13. | Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D, Italia L, Zaccone G, Tedino C, Fabbricatore D, Curnis A, Faggiano P, Gorga E, Lombardi CM, Milesi G, Vizzardi E, Volpini M, Nodari S, Specchia C, Maroldi R, Bezzi M, Metra M. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020;41:1821-1829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 332] [Cited by in RCA: 375] [Article Influence: 75.0] [Reference Citation Analysis (0)] |
| 14. | Kytömaa S, Hegde S, Claggett B, Udell JA, Rosamond W, Temte J, Nichol K, Wright JD, Solomon SD, Vardeny O. Association of Influenza-like Illness Activity With Hospitalizations for Heart Failure: The Atherosclerosis Risk in Communities Study. JAMA Cardiol. 2019;4:363-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 15. | Østergaard L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol Rep. 2021;9:e14726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 177] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 16. | Bader F, Manla Y, Atallah B, Starling RC. Heart failure and COVID-19. Heart Fail Rev. 2021;26:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 153] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 17. | Tsao CW, Strom JB, Chang JD, Manning WJ. COVID-19-Associated Stress (Takotsubo) Cardiomyopathy. Circ Cardiovasc Imaging. 2020;13:e011222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 18. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 52] [Reference Citation Analysis (0)] |
| 19. | Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, Jeanpierre E, Rauch A, Labreuche J, Susen S; Lille ICU Haemostasis COVID-19 Group. Pulmonary Embolism in Patients With COVID-19: Awareness of an Increased Prevalence. Circulation. 2020;142:184-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 724] [Cited by in RCA: 872] [Article Influence: 174.4] [Reference Citation Analysis (0)] |
| 20. | Miró Ò, Jiménez S, Mebazaa A, Freund Y, Burillo-Putze G, Martín A, Martín-Sánchez FJ, García-Lamberechts EJ, Alquézar-Arbé A, Jacob J, Llorens P, Piñera P, Gil V, Guardiola J, Cardozo C, Mòdol Deltell JM, Tost J, Aguirre Tejedo A, Palau-Vendrell A, LLauger García L, Adroher Muñoz M, Del Arco Galán C, Agudo Villa T, López-Laguna N, López Díez MP, Beddar Chaib F, Quero Motto E, González Tejera M, Ponce MC, González Del Castillo J; Spanish Investigators on Emergency Situations TeAm (SIESTA) network. Pulmonary embolism in patients with COVID-19: incidence, risk factors, clinical characteristics, and outcome. Eur Heart J. 2021;42:3127-3142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 91] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 21. | Riyahi S, Dev H, Behzadi A, Kim J, Attari H, Raza SI, Margolis DJ, Jonisch A, Megahed A, Bamashmos A, Elfatairy K, Prince MR. Pulmonary Embolism in Hospitalized Patients with COVID-19: A Multicenter Study. Radiology. 2021;301:E426-E433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 22. | Argulian E, Sud K, Vogel B, Bohra C, Garg VP, Talebi S, Lerakis S, Narula J. Right Ventricular Dilation in Hospitalized Patients With COVID-19 Infection. JACC Cardiovasc Imaging. 2020;13:2459-2461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 154] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 23. | Li Y, Li H, Zhu S, Xie Y, Wang B, He L, Zhang D, Zhang Y, Yuan H, Wu C, Sun W, Li M, Cui L, Cai Y, Wang J, Yang Y, Lv Q, Zhang L, Xie M. Prognostic Value of Right Ventricular Longitudinal Strain in Patients With COVID-19. JACC Cardiovasc Imaging. 2020;13:2287-2299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 322] [Cited by in RCA: 326] [Article Influence: 65.2] [Reference Citation Analysis (0)] |
| 24. | Italia L, Tomasoni D, Bisegna S, Pancaldi E, Stretti L, Adamo M, Metra M. COVID-19 and Heart Failure: From Epidemiology During the Pandemic to Myocardial Injury, Myocarditis, and Heart Failure Sequelae. Front Cardiovasc Med. 2021;8:713560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 77] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 25. | Arévalos V, Ortega-Paz L, Rodríguez-Arias JJ, Calvo M, Castrillo L, Salazar A, Roque M, Dantas AP, Sabaté M, Brugaletta S. Myocardial Injury in COVID-19 Patients: Association with Inflammation, Coagulopathy and In-Hospital Prognosis. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 26. | Hollenberg SM, Safi L, Parrillo JE, Fata M, Klinkhammer B, Gayed N, Glotzer T, Go RC, Gourna-Paleoudis E, Landers D, Jamal S, Shah N, Shah R, Tancredi J, Turi ZG. Hemodynamic Profiles of Shock in Patients With COVID-19. Am J Cardiol. 2021;153:135-139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Maisel A. B-type natriuretic peptide levels: diagnostic and prognostic in congestive heart failure: what's next? Circulation. 2002;105:2328-2331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 120] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Gao L, Jiang D, Wen XS, Cheng XC, Sun M, He B, You LN, Lei P, Tan XW, Qin S, Cai GQ, Zhang DY. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir Res. 2020;21:83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 192] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 29. | Qin JJ, Cheng X, Zhou F, Lei F, Akolkar G, Cai J, Zhang XJ, Blet A, Xie J, Zhang P, Liu YM, Huang Z, Zhao LP, Lin L, Xia M, Chen MM, Song X, Bai L, Chen Z, Zhang X, Xiang D, Chen J, Xu Q, Ma X, Touyz RM, Gao C, Wang H, Liu L, Mao W, Luo P, Yan Y, Ye P, Chen M, Chen G, Zhu L, She ZG, Huang X, Yuan Y, Zhang BH, Wang Y, Liu PP, Li H. Redefining Cardiac Biomarkers in Predicting Mortality of Inpatients With COVID-19. Hypertension. 2020;76:1104-1112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 30. | Stefanini GG, Chiarito M, Ferrante G, Cannata F, Azzolini E, Viggiani G, De Marco A, Briani M, Bocciolone M, Bragato R, Corrada E, Gasparini GL, Marconi M, Monti L, Pagnotta PA, Panico C, Pini D, Regazzoli D, My I, Kallikourdis M, Ciccarelli M, Badalamenti S, Aghemo A, Reimers B, Condorelli G; Humanitas COVID-19 Task Force. Early detection of elevated cardiac biomarkers to optimise risk stratification in patients with COVID-19. Heart. 2020;106:1512-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 31. | McCullough SA, Goyal P, Krishnan U, Choi JJ, Safford MM, Okin PM. Electrocardiographic Findings in Coronavirus Disease-19: Insights on Mortality and Underlying Myocardial Processes. J Card Fail. 2020;26:626-632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 32. | Bergamaschi L, D'Angelo EC, Paolisso P, Toniolo S, Fabrizio M, Angeli F, Donati F, Magnani I, Rinaldi A, Bartoli L, Chiti C, Biffi M, Pizzi C, Viale P, Galié N. The value of ECG changes in risk stratification of COVID-19 patients. Ann Noninvasive Electrocardiol. 2021;26:e12815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 33. | Szekely Y, Lichter Y, Taieb P, Banai A, Hochstadt A, Merdler I, Gal Oz A, Rothschild E, Baruch G, Peri Y, Arbel Y, Topilsky Y. Spectrum of Cardiac Manifestations in COVID-19: A Systematic Echocardiographic Study. Circulation. 2020;142:342-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 444] [Cited by in RCA: 426] [Article Influence: 85.2] [Reference Citation Analysis (0)] |
| 34. | Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, White A, Salvo GD, Sade LE, Pearce K, Newby DE, Popescu BA, Donal E, Cosyns B, Edvardsen T, Mills NL, Haugaa K. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21:949-958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 213] [Cited by in RCA: 300] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 35. | Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, Danilov T, Kukar N, Shaban N, Kini A, Camaj A, Bienstock SW, Rashed ER, Rahman K, Oates CP, Buckley S, Elbaum LS, Arkonac D, Fiter R, Singh R, Li E, Razuk V, Robinson SE, Miller M, Bier B, Donghi V, Pisaniello M, Mantovani R, Pinto G, Rota I, Baggio S, Chiarito M, Fazzari F, Cusmano I, Curzi M, Ro R, Malick W, Kamran M, Kohli-Seth R, Bassily-Marcus AM, Neibart E, Serrao G, Perk G, Mancini D, Reddy VY, Pinney SP, Dangas G, Blasi F, Sharma SK, Mehran R, Condorelli G, Stone GW, Fuster V, Lerakis S, Goldman ME. Characterization of Myocardial Injury in Patients With COVID-19. J Am Coll Cardiol. 2020;76:2043-2055. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 289] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 36. | Giustiniano E, Fazzari F, Bragato RM, Curzi M, Cecconi M. Trans-thoracic Echocardiography in Prone Positioning COVID-19 Patients: a Small Case Series. SN Compr Clin Med. 2020;2:2381-2386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1265-1273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1240] [Cited by in RCA: 1468] [Article Influence: 293.6] [Reference Citation Analysis (0)] |
| 38. | Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, Patel R, Chacko L, Brown JT, Coyle C, Leith D, Shetye A, Ariff B, Bell R, Captur G, Coleman M, Goldring J, Gopalan D, Heightman M, Hillman T, Howard L, Jacobs M, Jeetley PS, Kanagaratnam P, Kon OM, Lamb LE, Manisty CH, Mathurdas P, Mayet J, Negus R, Patel N, Pierce I, Russell G, Wolff A, Xue H, Kellman P, Moon JC, Treibel TA, Cole GD, Fontana M. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42:1866-1878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 273] [Article Influence: 68.3] [Reference Citation Analysis (0)] |
| 39. | Yonas E, Alwi I, Pranata R, Huang I, Lim MA, Gutierrez EJ, Yamin M, Siswanto BB, Virani SS. Effect of heart failure on the outcome of COVID-19 - A meta analysis and systematic review. Am J Emerg Med. 2021;46:204-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 40. | Alvarez-Garcia J, Lee S, Gupta A, Cagliostro M, Joshi AA, Rivas-Lasarte M, Contreras J, Mitter SS, LaRocca G, Tlachi P, Brunjes D, Glicksberg BS, Levin MA, Nadkarni G, Fayad Z, Fuster V, Mancini D, Lala A. Prognostic Impact of Prior Heart Failure in Patients Hospitalized With COVID-19. J Am Coll Cardiol. 2020;76:2334-2348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 151] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 41. | Tomasoni D, Inciardi RM, Lombardi CM, Tedino C, Agostoni P, Ameri P, Barbieri L, Bellasi A, Camporotondo R, Canale C, Carubelli V, Carugo S, Catagnano F, Dalla Vecchia LA, Danzi GB, Di Pasquale M, Gaudenzi M, Giovinazzo S, Gnecchi M, Iorio A, La Rovere MT, Leonardi S, Maccagni G, Mapelli M, Margonato D, Merlo M, Monzo L, Mortara A, Nuzzi V, Piepoli M, Porto I, Pozzi A, Sarullo F, Sinagra G, Volterrani M, Zaccone G, Guazzi M, Senni M, Metra M. Impact of heart failure on the clinical course and outcomes of patients hospitalized for COVID-19. Results of the Cardio-COVID-Italy multicentre study. Eur J Heart Fail. 2020;22:2238-2247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 100] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 42. | Zhang Y, Coats AJS, Zheng Z, Adamo M, Ambrosio G, Anker SD, Butler J, Xu D, Mao J, Khan MS, Bai L, Mebazaa A, Ponikowski P, Tang Q, Ruschitzka F, Seferovic P, Tschöpe C, Zhang S, Gao C, Zhou S, Senni M, Zhang J, Metra M. Management of heart failure patients with COVID-19: a joint position paper of the Chinese Heart Failure Association & National Heart Failure Committee and the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020;22:941-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 43. | Hajjar LA, Costa IBSDS, Rizk SI, Biselli B, Gomes BR, Bittar CS, de Oliveira GQ, de Almeida JP, de Oliveira Bello MV, Garzillo C, Leme AC, Elena M, Val F, de Almeida Lopes M, Lacerda MVG, Ramires JAF, Kalil Filho R, Teboul JL, Landoni G. Intensive care management of patients with COVID-19: a practical approach. Ann Intensive Care. 2021;11:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 44. | Mohamadi Yarijani Z, Najafi H. Kidney injury in COVID-19 patients, drug development and their renal complications: Review study. Biomed Pharmacother. 2021;142:111966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 45. | Fida N. Management of Heart Failure, Durable Left Ventricular Assist Device, and Heart Transplant Patients in the COVID-19 Era. Methodist Debakey Cardiovasc J. 2021;17:63-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 46. | Onohuean H, Al-Kuraishy HM, Al-Gareeb AI, Qusti S, Alshammari EM, Batiha GE. Covid-19 and development of heart failure: mystery and truth. Naunyn Schmiedebergs Arch Pharmacol. 2021;394:2013-2021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 47. | Pauschinger M, Rutschow S, Chandrasekharan K, Westermann D, Weitz A, Peter Schwimmbeck L, Zeichhardt H, Poller W, Noutsias M, Li J, Schultheiss HP, Tschope C. Carvedilol improves left ventricular function in murine coxsackievirus-induced acute myocarditis association with reduced myocardial interleukin-1beta and MMP-8 expression and a modulated immune response. Eur J Heart Fail. 2005;7:444-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 48. | Maddox TM, Januzzi JL, Jr. , Allen LA, Breathett K, Butler J, Davis LL, Fonarow GC, Ibrahim NE, Lindenfeld J, Masoudi FA, Motiwala SR, Oliveros E, Patterson JH, Walsh MN, Wasserman A, Yancy CW, Youmans QR. 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77:772-810. [RCA] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 579] [Article Influence: 144.8] [Reference Citation Analysis (0)] |
| 49. | Goligher EC, Bradbury CA, McVerry BJ, Lawler PR, Berger JS, Gong MN, Carrier M, Reynolds HR, Kumar A, Turgeon AF, Kornblith LZ, Kahn SR, Marshall JC, Kim KS, Houston BL, Derde LPG, Cushman M, Tritschler T, Angus DC, Godoy LC, McQuilten Z, Kirwan BA, Farkouh ME, Brooks MM, Lewis RJ, Berry LR, Lorenzi E, Gordon AC, Ahuja T, Al-Beidh F, Annane D, Arabi YM, Aryal D, Baumann Kreuziger L, Beane A, Bhimani Z, Bihari S, Billett HH, Bond L, Bonten M, Brunkhorst F, Buxton M, Buzgau A, Castellucci LA, Chekuri S, Chen JT, Cheng AC, Chkhikvadze T, Coiffard B, Contreras A, Costantini TW, de Brouwer S, Detry MA, Duggal A, Džavík V, Effron MB, Eng HF, Escobedo J, Estcourt LJ, Everett BM, Fergusson DA, Fitzgerald M, Fowler RA, Froess JD, Fu Z, Galanaud JP, Galen BT, Gandotra S, Girard TD, Goodman AL, Goossens H, Green C, Greenstein YY, Gross PL, Haniffa R, Hegde SM, Hendrickson CM, Higgins AM, Hindenburg AA, Hope AA, Horowitz JM, Horvat CM, Huang DT, Hudock K, Hunt BJ, Husain M, Hyzy RC, Jacobson JR, Jayakumar D, Keller NM, Khan A, Kim Y, Kindzelski A, King AJ, Knudson MM, Kornblith AE, Kutcher ME, Laffan MA, Lamontagne F, Le Gal G, Leeper CM, Leifer ES, Lim G, Gallego Lima F, Linstrum K, Litton E, Lopez-Sendon J, Lother SA, Marten N, Saud Marinez A, Martinez M, Mateos Garcia E, Mavromichalis S, McAuley DF, McDonald EG, McGlothlin A, McGuinness SP, Middeldorp S, Montgomery SK, Mouncey PR, Murthy S, Nair GB, Nair R, Nichol AD, Nicolau JC, Nunez-Garcia B, Park JJ, Park PK, Parke RL, Parker JC, Parnia S, Paul JD, Pompilio M, Quigley JG, Rosenson RS, Rost NS, Rowan K, Santos FO, Santos M, Santos MO, Satterwhite L, Saunders CT, Schreiber J, Schutgens REG, Seymour CW, Siegal DM, Silva DG, Jr. , Singhal AB, Slutsky AS, Solvason D, Stanworth SJ, Turner AM, van Bentum-Puijk W, van de Veerdonk FL, van Diepen S, Vazquez-Grande G, Wahid L, Wareham V, Widmer RJ, Wilson JG, Yuriditsky E, Zhong Y, Berry SM, McArthur CJ, Neal MD, Hochman JS, Webb SA, Zarychanski R. Therapeutic Anticoagulation with Heparin in Critically Ill Patients with Covid-19. N Engl J Med. 2021;385:777-789. [RCA] [DOI] [Full Text] [Cited by in Crossref: 636] [Cited by in RCA: 621] [Article Influence: 124.2] [Reference Citation Analysis (0)] |
| 50. | Rey JR, Caro-Codón J, Rosillo SO, Iniesta ÁM, Castrejón-Castrejón S, Marco-Clement I, Martín-Polo L, Merino-Argos C, Rodríguez-Sotelo L, García-Veas JM, Martínez-Marín LA, Martínez-Cossiani M, Buño A, Gonzalez-Valle L, Herrero A, López-Sendón JL, Merino JL; CARD-COVID Investigators. Heart failure in COVID-19 patients: prevalence, incidence and prognostic implications. Eur J Heart Fail. 2020;22:2205-2215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 170] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 51. | Fox S, Vashisht R, Siuba M, Dugar S. Evaluation and management of shock in patients with COVID-19. Cleve Clin J Med. 2020;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 52. | Ranard LS, Fried JA, Abdalla M, Anstey DE, Givens RC, Kumaraiah D, Kodali SK, Takeda K, Karmpaliotis D, Rabbani LE, Sayer G, Kirtane AJ, Leon MB, Schwartz A, Uriel N, Masoumi A. Approach to Acute Cardiovascular Complications in COVID-19 Infection. Circ Heart Fail. 2020;13:e007220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 53. | Latif F, Farr MA, Clerkin KJ, Habal MV, Takeda K, Naka Y, Restaino S, Sayer G, Uriel N. Characteristics and Outcomes of Recipients of Heart Transplant With Coronavirus Disease 2019. JAMA Cardiol. 2020;5:1165-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 151] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 54. | Genuardi MV, Moss N, Najjar SS, Houston BA, Shore S, Vorovich E, Atluri P, Molina M, Chambers S, Sharkoski T, Hsich E, Estep JD, Owens AT, Alexander KM, Chaudhry SP, Garcia-Cortes R, Molina E, Rodrigo M, Wald MJ, Margulies KB, Hanff TC, Zimmer R, Kilic A, Mclean R, Vidula H, Dodd K, Blumberg EA, Mazurek JA, Goldberg LR, Alvarez-Garcia J, Mancini D, Teuteberg JJ, Tedford RJ, Birati EY. Coronavirus disease 2019 in heart transplant recipients: Risk factors, immunosuppression, and outcomes. J Heart Lung Transplant. 2021;40:926-935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 55. | International Society of Heart and Lung Transplantation (ISHLT). Guidance from the International Society of Heart and Lung Transplantation regarding the SARS CoV-2 pandemic. [cited 20 April 2022]. Available from: https://ishlt.org/ishlt/media/documents/SARS-CoV-2_Guidance-for-Cardiothoracic-Transplant-and-VAD-center.pdf. |
| 56. | Tenforde MW, Self WH, Adams K, Gaglani M, Ginde AA, McNeal T, Ghamande S, Douin DJ, Talbot HK, Casey JD, Mohr NM, Zepeski A, Shapiro NI, Gibbs KW, Files DC, Hager DN, Shehu A, Prekker ME, Erickson HL, Exline MC, Gong MN, Mohamed A, Henning DJ, Steingrub JS, Peltan ID, Brown SM, Martin ET, Monto AS, Khan A, Hough CL, Busse LW, Ten Lohuis CC, Duggal A, Wilson JG, Gordon AJ, Qadir N, Chang SY, Mallow C, Rivas C, Babcock HM, Kwon JH, Halasa N, Chappell JD, Lauring AS, Grijalva CG, Rice TW, Jones ID, Stubblefield WB, Baughman A, Womack KN, Rhoads JP, Lindsell CJ, Hart KW, Zhu Y, Olson SM, Kobayashi M, Verani JR, Patel MM; Influenza and Other Viruses in the Acutely Ill (IVY) Network. Association Between mRNA Vaccination and COVID-19 Hospitalization and Disease Severity. JAMA. 2021;326:2043-2054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 447] [Cited by in RCA: 473] [Article Influence: 118.3] [Reference Citation Analysis (0)] |
| 57. | Wada S, Wiegand J, Markarian M, Hung V, Zhu C, Parayil M, Shim K, Serrano J, Chung W. 190. Epidemiology of COVID-19 Breakthrough Infections in Dallas County, Texas, 2021. Open Forum Infectious Diseases. 2021;8 Suppl 1:S115-S115. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 58. | Chia PY, Ong SWX, Chiew CJ, Ang LW, Chavatte JM, Mak TM, Cui L, Kalimuddin S, Chia WN, Tan CW, Chai LYA, Tan SY, Zheng S, Lin RTP, Wang L, Leo YS, Lee VJ, Lye DC, Young BE. Virological and serological kinetics of SARS-CoV-2 Delta variant vaccine breakthrough infections: a multicentre cohort study. Clin Microbiol Infect. 2022;28:612.e1-612.e7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 166] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 59. | Ke R, Martinez PP, Smith RL, Gibson LL, Achenbach CJ, McFall S, Qi C, Jacob J, Dembele E, Bundy C, Simons LM, Ozer EA, Hultquist JF, Lorenzo-Redondo R, Opdycke AK, Hawkins C, Murphy RL, Mirza A, Conte M, Gallagher N, Luo CH, Jarrett J, Conte A, Zhou R, Farjo M, Rendon G, Fields CJ, Wang L, Fredrickson R, Baughman ME, Chiu KK, Choi H, Scardina KR, Owens AN, Broach J, Barton B, Lazar P, Robinson ML, Mostafa HH, Manabe YC, Pekosz A, McManus DD, Brooke CB. Longitudinal analysis of SARS-CoV-2 vaccine breakthrough infections reveal limited infectious virus shedding and restricted tissue distribution. medRxiv 2021. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 60. | Standl E, Schnell O. Heart failure outcomes and Covid-19. Diabetes Res Clin Pract. 2021;175:108794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 61. | Samidurai A, Das A. Cardiovascular Complications Associated with COVID-19 and Potential Therapeutic~Strategies. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 62. | Farshidfar F, Koleini N, Ardehali H. Cardiovascular complications of COVID-19. JCI Insight. 2021;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 63. | Unudurthi SD, Luthra P, Bose RJC, McCarthy JR, Kontaridis MI. Cardiac inflammation in COVID-19: Lessons from heart failure. Life Sci. 2020;260:118482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 64. | Freaney PM, Shah SJ, Khan SS. COVID-19 and Heart Failure With Preserved Ejection Fraction. JAMA. 2020;324:1499-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 65. | Shah RM, Shah M, Shah S, Li A, Jauhar S. Takotsubo Syndrome and COVID-19: Associations and Implications. Curr Probl Cardiol. 2021;46:100763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 66. | Koutroumpakis E, Taylor T, Damaraju S, Badruddin Mawji S. "Covidsubo": Stress-Induced Cardiomyopathy by Novel Coronavirus Disease 2019. Cardiology. 2020;145:779-783. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |