Published online Jan 26, 2022. doi: 10.4330/wjc.v14.i1.13
Peer-review started: March 17, 2021
First decision: July 8, 2021
Revised: July 15, 2021
Accepted: December 31, 2021
Article in press: December 31, 2021
Published online: January 26, 2022
Processing time: 307 Days and 8.3 Hours
Treatment of coronary chronic total occlusion (CTO) with percutaneous coronary intervention (PCI) has rapidly increased during the past decades. Different strategies and approach were developed in the recent past years leading to an increase in CTO-PCI procedural success. The goal to achieve an extended revascularization with a high rate of completeness is now supported by strong scientific evidences and consequently, has led to an exponential increase in the number of CTO-PCI procedures, even if are still underutilized. It has been widely demon
Core Tip: The application of “contemporary” revascularization strategy in coronary chronic total occlusion percutaneous interventions, allowed a high procedural success rate and to achieve a complete or reasonable incomplete coronary revascularization. From a procedural and clinical management point of view, an improved accuracy in clinical decision making process and a state-of-the-art revascularization, led to a long-term clinical benefit, even in high-risk patients or complex coronary anatomy.
- Citation: Muraca I, Carrabba N, Virgili G, Bruscoli F, Migliorini A, Pennesi M, Pontecorboli G, Marchionni N, Valenti R. Chronic total occlusion revascularization: A complex piece to "complete" the puzzle. World J Cardiol 2022; 14(1): 13-28
- URL: https://www.wjgnet.com/1949-8462/full/v14/i1/13.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i1.13
Treatment of coronary chronic total occlusion (CTO) with percutaneous coronary intervention (PCI) has rapidly increased during the past decade, driven by technical and technological advancements involving drug-eluting stents (DES), antithrombotic drugs management, procedural strategies and interventional cardiologists’ expertise. “Contemporary” revascularization strategies include: novel and dedicated techniques, use of 2nd and 3rd generation DES and intracoronary imaging, “tailored” antithrombotic therapy management. Strategies aimed to achieve an extended revascularization with a high rate of completeness have led to an exponential increase in the number of successful CTO-PCI procedures, which translates in a long-term clinical benefit. However, CTO-PCI is still underutilized, accounting for only 5%-15% of elective PCI, despite a reported prevalence of CTO in up to one-third of patients with coronary artery disease, and 10%-18% of patients with STEMI[1,2] The presence of a CTO, compared with non-occlusive coronary lesions, greatly affects the therapeutic strategies of patients with atherosclerotic ischemic heart disease, with a more frequent referral to surgical revascularization [coronary artery bypass graft (CABG)] or medical therapy rather than percutaneous solution.
The expected benefits from the revascularization of a CTO can be summarized in: (1) Improved quality of life; (2) Improved left ventricular (LV) function; (3) Increased long-term survival; (4) Increased tolerance to potential subsequent coronary events; and (5) Reduced risk of life threatening-arrhythmias.
The available evidence in support of a favorable prognostic impact, mostly comes from observational studies (high volume single-center registries or multi-center registries), with the recognized limitations of selection and publication bias and possible residual confounders[3-6]. On the other side, such registries have the undoubted advantage to offer a view of clinical and therapeutic practice in the real world. At present, there are also extensive meta-analyses to consolidate this evidence[7-9]. Contemporary randomized clinical trials are small, and often investigate surrogate prognostic end points or non-inferiority analyses[10,11] (Table 1).
| Studies | Patients (n) | CTO-PCI success | Follow-up | PCI success vs PCI failure | ||
| MACE | Death | |||||
| Registries | OPEN-CTO 2020 (12) (Hybrid approach) | 1000 | 90% | 1 yr | 3.4% vs 3.7% | 0.9% vs 0% |
| EXPERT-CTO 2019 (2) (New generation DES) | 250 | 96.4% | 1 yr | 18.5% vs 24.4% | NR | |
| Valenti et al 2019 (3) (Elderly ≥ 75 yr) | 460 | 72% | 5 yr | 9.6% vs 17% | 84% ± 3% vs 72% ± 6% | |
| Sudhakar et al 2014 (4) | 13443 | 70.6% | 2.65 yr | NR | HR 0.72, 95%CI: 0.62-0.83 | |
| Metanalyses | Christakopoulos et al 2015 (5) | 28486 | 71% | 3.11 yr | 29.1% | 6.4% vs 9.5% |
| Hoebers et al 2015 (6) | 15459 | 71.7% | 1-10 yr | NR | 10.4% vs 14.9% | |
| Chenmin et al 2021 (7) (Elderly ≥ 75 yr) | 4693 | 70.4%-78.36% | 20 mo-5 yr | 16.8% vs 28.9% | HR: 0.51, 95%CI: 0.34-0.77 | |
| RCTs | DECISION CTO 2019 (8) | 834 | 90.6% | 4 yr | 22.3% vs 22.4% | 3.6% vs 5.3% |
| EURO CTO 2018 (9) | 396 | 86.6% | 1 yr | 5.2% vs 6.7% | 0.8% vs 0% | |
The Korean multicenter randomized DECISION-CTO trial, which was discontinued because of slow enrollment (out of 1.284 planned patients, only 834 were enrolled), showed how CTO-PCI, combined with optimal medical therapy, was not superior to medical therapy alone in reducing cardiovascular events in patients with CTO at 3-year follow-up; the primary end point, a composite of all-cause mortality, myocardial infarction, stroke, and repeat of any coronary revascularization, was 20.6% vs 19.6% (P = 0.008 for non-inferiority of optimal medical therapy). Five years follow-up data, published in 2019, confirmed no differences in term of primary end point (22.3% vs 22.4%; HR 1.03; 95%CI: 0.77 to 1.37; P = 0.86); notably, the 19.6% of the patients assigned to the no CTO-PCI strategy arm, crossed over to receive staged CTO-PCI[10]. In the Korean study, the mean age of patients was approximately 62 years, LV function 57%, and two thirds of patients had a stable coronary artery disease. It is estimated that for an adequate statistical power to detect a difference in outcome in terms of mortality between CTO-PCI and optimal medical therapy, an ideal trial would require more than 5000 patients, a figure not even remotely represented in current studies.
The multicenter randomized EURO-CTO trial enrolled 450 patients, randomized to CTO-PCI vs medical therapy with a 2:1 ratio; procedural success in the PCI arm was 86.7%; at 12 mo follow-up, CTO-PCI group showed greater improvement in the angina frequency score (P = 0.003) and the quality-of-life score (P = 0.007) compared with optimal medical therapy; causative classification system (CCS) improved considerably more in the PCI group than in the optimal medical therapy group (P < 0.001). No differences in the primary safety end points evaluated at 36 mo were found. Major cardiovascular and cerebrovascular events (MACCE) during 12 mo follow-up were similar between the two groups (P = 0.55)[11].
The lack of positive results in terms of clinical outcomes in randomized trials may be explained, at least partially, by the exclusion of patients at higher risk of events, for whom, on the basis of a perceived or demonstrated therapeutic benefit, an interventional attitude is preferred, effectively excluding the possibilities of randomization to conservative therapy for ethical reasons. Accordingly, Galassi et al[12] in their study reported how, even in the absence of statistically significant differences in MACCE at a median follow-up of 16.3 ± 8.2 mo, the group of patients with severely depressed left ventricular ejection fraction (LVEF) (< 35%), showed a significantly improvement of LVEF when a successful CTO-PCI was performed.
Convincing positive results from randomized trials are still awaited to conclusively legitimize the potential benefits of CTO-PCI in patients with indication for revascularization. The lack of unequivocal answers from randomized trials, however, does not preclude the possibility of choosing a therapeutic strategy: "evidence-based medicine" is still "the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients"[13] and the current evidence points in favor of CTO-PCI attempts.
A meta-analysis published in 2015, conducted on more than 28000 patients, showed the association of successful CTO-PCI with improved long-term survival when compared with procedural failure (OR 0.52, 95%CI: 0.43-0.63)[7]. Another meta-analysis, conducted on 2243 patients with successful CTO-PCI, found a LVEF significant increase, with 4.4 percentage points over baseline comparison in absolute terms (P < 0.01), as well as a reduction in negative ventricular remodeling[8].
Clinical benefit of successful CTO-PCI was found also in large registries[3-6]. In the OPEN-CTO registry (1), which enrolled 1000 patients, investigators reported in the group of successful CTO revascularization a statistically significant improvement in Seattle Angina Questionnaire (SAQ) from 49.4 ± 0.9 to 75.0 ± 0.7 (P < 0.01), and, after adjusting for baseline differences, the mean group difference in SAQ between successful and unsuccessful CTO-PCI was 10.8 (95%CI: 6.3 to 15.3; P < 0.001)[3]. At 1 year, the unadjusted MACCE rate was lower in patients with successful index CTO-PCI compared to patients with unsuccessful CTO-PCI (9.4% vs 14.6%; P = 0.04)[14].
Nowadays, despite results from perspective randomized controlled trials are conflicting, and the survival benefits are still debates, the indications to drive a CTO-PCI according to guidelines of the most important scientific societies are refractory angina symptoms despite optimal medical therapy or patients with documented large ischemic area in the territory of occluded vessel[15]. Furthermore, current evidence and guidelines support the use of viability imaging to assist decision-making in patients with ischemic heart failure and coronary artery disease[15]. Distinguishing hibernating myocardium from non-viable myocardium is particularly important to select patients that are more likely to benefit from myocardial revascularization and to reduce the risk of inappropriate treatment. Despite lack of longitudinal outcome benefit in the previous clinical trials, myocardial viability assessment plays an important role on a personalized level of clinical decision making for patients with CTO and LV dysfunction. The different noninvasive modalities available to assess myocardial viability interrogate distinct pathophysiologic myocyte and myocardial processes. The single photon emission computed tomography radionuclide tracers) examine myocyte cell membrane integrity, positron emission tomography myocardial blood flow and metabolism, cardiac magnetic resonance (CMR) with late gadolinium enhancement identifies scarred myocardium, whereas dobutamine echocardiography or CMR assesses regional ventricular contractile reserve. The imaging modality of choice needs to be individualized according to each clinical scenario, technology availability and institution expertise.
CMR is a versatile imaging modality to assess multiple interrelated features of both ischemia and viability in a single test without the use of ionizing radiation. It provides accurate and reproducible assessment of global and regional ventricular function, myocardial perfusion at rest and at stress, myocardial scar and the identification of viable but dysfunctional hibernated myocardium, being able to predict its recovery after successful revascularization[16]. Previous studies showed that the use of CMR may help to select patients who could derive significant LV reverse remodeling, ischemic burden relief, and quality of life improvement after CTO recanalization[17,18]. Nevertheless, randomized trials with larger patient numbers are warranted to explore whether CMR-guided CTO revascularization is indeed superior to other available functional imaging, and is an independent predictor of long-term improved clinical outcome. Two ongoing trials, NOBLE-CTO (the nordic-baltic randomized registry study for the evaluation of PCI in chronic total coronary occlusion; NCT03392415) and ISCHEMIA-CTO (revascularization or optimal medical therapy of CTO; NCT03564317), employing CMR and nuclear imaging are eagerly awaited. Meanwhile according to current evidences, CTO PCI should be considered in symptomatic patients despite optimal medical therapy.
Rarely, CTO presents as single vessel coronary disease. More often, the interventional cardiologist is confronted with a multivessel coronary artery disease in which CTO represents an additional element of complexity. In this scenario, it is appropriate to analyze the potential prognostic impact of percutaneous revascularization of CTO in the broader perspective of a complete or reasonable incomplete revascularization.
Pioneering studies have shown that complete coronary revascularization, achieved following PCI of at least one CTO, results in a significant reduction in long-term cardiac mortality in the setting of multivessel atherosclerotic disease[19]. Even in patients undergoing PCI for multiple CTOs, 2-year survival was significantly better in patients with a complete revascularization by PCI[20]. Further confirmation came from the publication of the subanalysis of the Synergy Between Percutaneous Coronary Intervention with Taxus And Cardiac Surgery (SYNTAX) trial, which evaluated the prognostic impact of complete revascularization achieved after PCI or CABG and its association with the presence of CTO[21]. Incomplete revascularization was found to be conditioned by the complexity of the coronary anatomy and patient comorbidities and correlated with increased mortality and MACCE at 4-year follow-up in both groups. The presence of CTO represented the strongest independent predictor of incomplete percutaneous revascularization, at a time in history still burdened by limited procedural proficiency, as demonstrated by the lower rate of successful revascularization of CTO in the group undergoing PCI, compared with the group undergoing CABG. To emphasize the importance of these results, it is worth mentioning that they derive from analyses conducted on patients in the SYNTAX trial, with stable coronary artery disease, without previous revascularizations, in whom first-generation DES were implanted, stent associated with more frequent events of restenosis and reocclusion than current second- or third-generation DES[22]. In addition, the success rate of CTO-PCI was significantly lower (approximately 49%) than the current rate, and complete revascularization was achieved in slightly more than half of the patients undergoing PCI and in only 63% of the patients undergoing CABG. Also in the study of Jang et al[23] published in 2017, data showed that in patients with CTO, achieving a complete revascularization (residual SYNTAX Score = 0) or a reasonable incomplete revascularization (residual SYNTAX Score = 12) guarantees a significantly lower risk of cardiac death and all-cause death compared with incomplete revascularization (residual SYNTAX score > 12), and these results were comparable with the CABG revascularization group at a median follow-up of 42 mo.
The favorable prognostic impact of a complete coronary revascularization has also been confirmed by large meta-analyses[5,24,25]. Among nearly 90000 patients from 35 randomized clinical trials and observational studies, completeness of revascularization, most often achieved by CABG, was found to be associated with approximately 30% reduction in long-term mortality[24]. Thus, it is not the surgical or percutaneous strategy that makes the difference, but the achievement of complete coronary revascularization. Another meta-analysis published in 2016, conducted on 156240 patients undergoing PCI for multivessel coronary artery disease, confirmed the strong prognostic benefit of the association between completeness of revascularization and reduced mortality and MACCE[25]. Notably, these benefits were maintained both in the subanalysis conducted on the cohort of 5 studies with CTO (OR 0.69; 95%CI: 0.53-0.80), and in the subanalyses that took into account the different definitions of complete revascularization[25]. Also of note, complete coronary revascularization by PCI was achieved in slightly less than half of the cases. Even in the pooled-analysis of Ahn et al[26] published in 2017, patients with incomplete revascularization by PCI had a higher risk of all-cause mortality respect to the patients treated with CABG. Conversely, no significant differences were found between patients undergoing CABG and those undergoing PCI with complete revascularization regarding the risk of death (aHR: 1.16; 95%CI: 0.83 to 1.63; P = 0.39) and the composite of death, myocardial infarction, and stroke (aHR: 1.14; 95%CI: 0.87 to 1.48; P = 0.35).
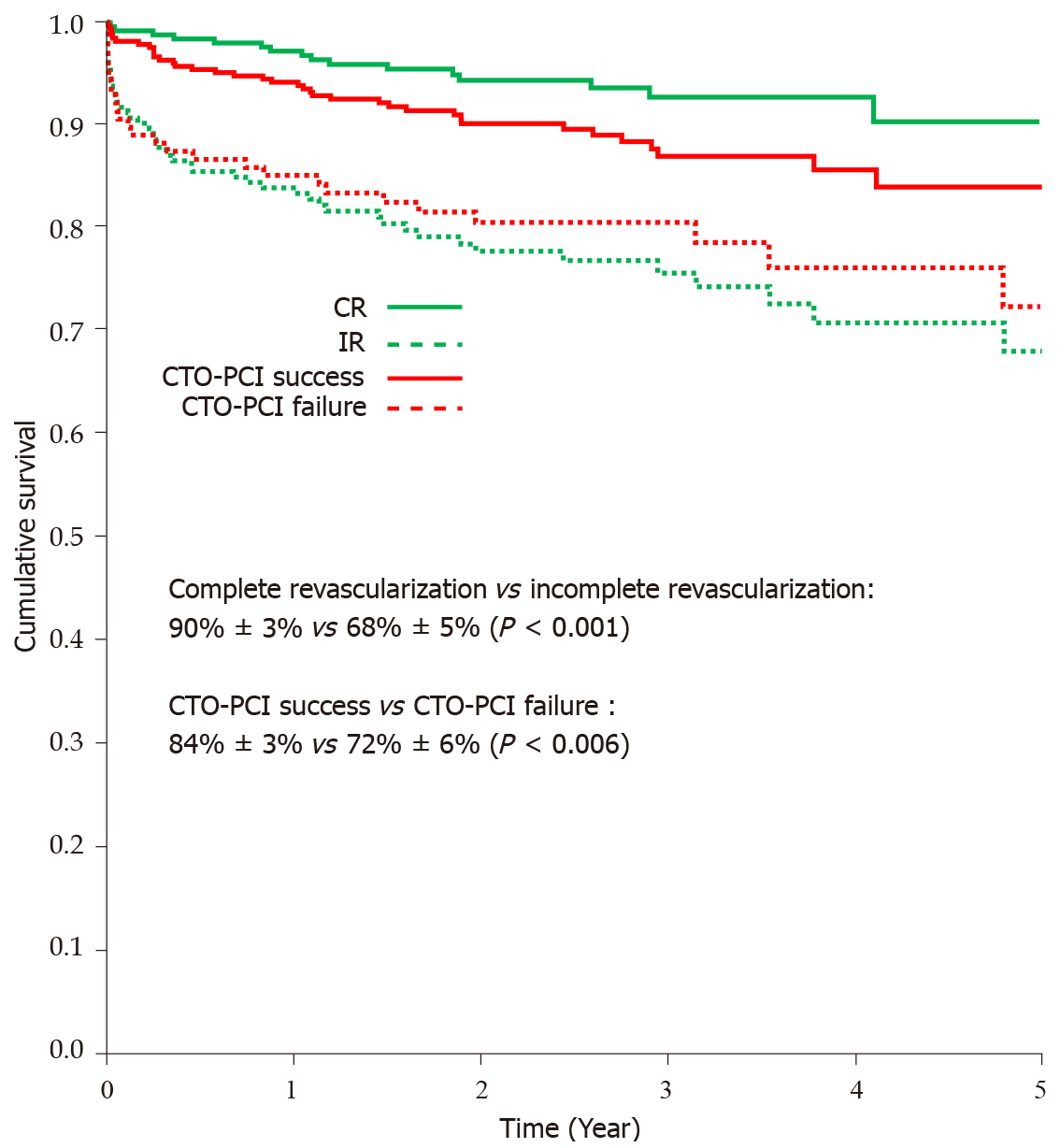
The favorable prognostic impact of successful CTO-PCI and complete revascularization on survival was also confirmed in elderly population. Valenti et al[5] collected data from 460 elderly patients (> 75 years) in the Florence real world CTO registry. Patients were stratified according to success or failure of CTO-PCI. Results showed improved five-year cardiac survival in the successful CTO-PCI group (P = 0.006) and a further improved survival benefit if complete coronary revascularization was achieved (90% ± 3% vs 68% ± 5%; P < 0.001) (Figure 1). Moreover, multivariate analysis demonstrated that increasing age, diabetes, chronic kidney disease, LVEF < 0.40 and complete revascularization resulted independently associated with long-term cardiac survival. Even in the meta-analysis of Cui et al[9] published in 2020, data derived from 8 studies showed how successful CTO-PCI was associated with reduction in long-term mortality and major adverse cardiovascular events (MACE) as compared to failed PCI in elderly.
Most of the elderly patients in these studies had high prevalence of comorbidities, complex coronary anatomy and concomitant LV dysfunction and heart failure, so they are consistent to the current setting definition of “complex higher-risk and indicated patients”[27]. In this context of patients with several comorbidities and severely reduced LV function, the execution of a percutaneous CTO revascularization is considered at very high risk, both for the technical difficulty of the procedure and for the clinical characteristics of the patient. Even if data regarding use of LV assist devices for hemodynamic support during CTO-PCI procedure are still lacking, initial experiences of small retrospective studies and case reports/series seem to show encouraging results[28].
Nowadays, the application of a “contemporary” revascularization strategy, in addition to the technical and procedural aspects, involves an optimal management of antithrombotic therapy. Patients who undergo a CTO-PCI are at high risk of clinical ischemic and thrombotic events. Antiplatelet therapy could play a leading role in reducing clinical event rates. Recent data from Valenti et al[19] has shown that a “tailored” approach based on platelet reactivity test results and clinical aspects could lead to a survival benefit. Data showed how three-year survival was significantly higher in patients with adequate responsiveness to antiplatelet drugs: the optimal platelet reactivity group compared with high platelet reactivity patients showed a lower MACE rate (95.3% ± 0.8% vs 86.2% ± 2.8%; P < 0.001). Furthermore, in high platelet reactivity cohort of patients, escalation to a more potent antiplatelet agent allowed similar survival rates to the patients with optimal platelet responsiveness. Conversely, a prolonged clopidogrel therapy in non-responders patients (when more potent antiplatelet agents were not available) was associated with a high cardiac mortality (HR: 2.37; P = 0.003)[29].
Combining the evidence from randomized trials and registries, it appears clear that, although the real benefits on prognosis have yet to be fully demonstrated, it is undeniable that the revascularization of CTO leads to an improvement in patients’ quality of life and more specifically to a reduction of angina. This evidence, in turn, raises further questions and in particular which strategy should be adopted in patients presenting CTO with a previous failed revascularization attempt or judged not amenable for CTO-PCI or in patient whose procedure would be at extremely high-risk to perform. Very interesting are the results of the retrospective multicenter study by Zivelonghi et al[30], conducted on patients with refractory angina symptoms, unsuitable for revascularization procedure or with previous revascularization failure, undergoing coronary sinus reducer (Neovasc Inc., Richmond B.C., Canada) implantation (24). In the group of patients with at least one CTO lesion, at a median follow up of 570 ± 370 d, patients experienced a statistically significant reduction in CCS class, with a significantly higher improvement respecting to the non-CTO patients’ group. One of the possible explanations of these results, according to the authors, consists in the presence of collateral coronary circulation in CTO patients; this could be the key for the device mechanism of action associated with the potential clinical benefit; nevertheless, these results need to be confirmed in perspective randomized controlled trials.
An additional complex clinical scenario is represented by acute coronary syndrome and multivessel coronary disease with the presence of a CTO.
About 50% of patients presenting with STEMI have a concomitant multivessel coronary artery disease, and about 13%-20% have a coexisting concurrent CTO; of these, only 5%-22% of cases receive an attempt percutaneous recanalization of the chronically occluded vessel, despite the current high success rate[2,31-34].
It is now recognized, from observational studies and sub-analyses of randomized trials, that the prognosis, in terms of short- and long-term survival after ST-elevation myocardial infarction (STEMI), is worse in patients with multivessel coronary artery disease and concomitant CTO. These findings have also been confirmed in a recent meta-analysis[35]. From a pathophysiological perspective, the presence of a CTO limits the possibility of providing collateral circulations to the acutely occluded vessel and, at the same time, the sudden deterioration of collaterals supplying the territory underlying the CTO may endanger a large area of myocardium.
If this intuitively explains the prognostic benefit of recanalization, which data are currently available to support this statement?
An observational study from the Florence CTO registry published in 2014[36], including patients with STEMI and concomitant CTO of the non-culprit vessel, showed a clear benefit in terms of 1- and 3-year cardiac survival in patients treated with successful CTO-PCI (performed between 7 and 30 d after primary PCI) when compared with patients with failed or non-attempted CTO-PCI; a favorable prognosis related to completeness of coronary revascularization was maintained even in very high-risk patients, such as those with cardiogenic shock, three-vessel and/or left main disease, severe LV dysfunction, and also in those patient with left anterior descending coronary artery involvement, either as culprit vessel or site of CTO (81%). In the group of patients with successful CTO-PCI, complete revascularization was achieved in 88% of cases, but even in the comparison group, extensive revascularization (non-CTO, non-infarct-related artery) was achieved in 85% of patients[36].
In 2016, the results of the randomized EXPLORE trial were published, which tested the impact of early PCI of CTO (< 7 d after the primary PCI procedure) on LV function and telediastolic ventricular volume at 4-mo follow-up[33]. Recanalization of CTO was not found to be associated with a significant improvement in LV function and telediastolic volume as assessed by magnetic resonance imaging. However, a sub-analysis of the study suggested a clinical benefit in patients undergoing PCI of the left anterior descending artery CTO[33]. Long-term follow-up (up to 5 years) showed that MACE were not significantly different in the two arms. Furthermore, no differences about the LV function were found in the two groups at 1 year[37].
The CREDO-Kyoto AMI registry analyzed 2045 patients with STEMI with or without CTO in the non-culprit vessel (18.7%). Although the presence of a CTO was independently associated with increased risk of mortality, mainly after the first 30 d after the acute event, there were no statistically significant differences in 5-year mortality between patients undergoing successful CTO-PCI and those with a failed procedure. It should be noted, however, that only 32% of cases underwent a CTO PCI, with a success rate of 64% and a low percentage of DES implantation[38].
Some evidence of MACE reduction in STEMI patients undergoing a staged CTO revascularization, compared with primary PCI and subsequent medical therapy comes from small retrospective single-center trials[39].
Although there is no clear evidence about the clinical benefit of revascularization of concurrent CTO in AMI patients, the available data are in favor of a complete coronary revascularization[40,41]. A possible explanation for the conflicting results in this setting, could be that the timing of the revascularization procedure following primary PCI must be individualized on the basis of the clinical characteristics of each patient; the application of a standardized timing in this complex clinical and procedural setting cannot be generalized.
The first reports of CTO-PCI date back to 1985, thanks to the pioneering attempts of Japanese operators who have transferred the techniques developed in the field of percutaneous revascularization of chronic femoro-popliteal occlusions to the coronary field. The first approach was antegrade, with procedural success in about 60% of attempts[42].
The observation that the distal cap of the occlusion is often less ambiguous and easier to penetrate than the proximal one, has soon created interest in a retrograde approach, first performed through vein grafts and then through septal collateral branches, leading to an increased procedural success, reaching 85%. Another technique borrowed again from the endovascular experience on the peripheral system is the "subintimal tracking and re-entry" (STAR), consisting in the recanalization of the occluded segment via a controlled subintimal dissection performed with a J-tipped wire (“knuckle”), adding a bailout strategy when failure of the "true-lumen" techniques occurs. Due to the difficulty in both navigating the guidewire and controlling the re-entry point in the true lumen, with potential loss of collateral branches, the STAR technique initially did not improve procedural success. Later, thanks to procedural refinements and devices advancements, the STAR technique has officially entered the CTO treatment option.
All these new techniques, in combination with the development of dedicated devices (among the latest the CrossBoss and Stingray system; Boston Scientific, Marlborough, MA, USA) and the use of second and third generation DES, with their improved long-term patency, have permitted a more articulated and flexible vision of CTO recanalization[22].
The indication for revascularization is conditioned by the clinical evaluation, which must take into account the patient's symptoms, LV function, comorbidities, and vitality/ischemia tests, in order to assess the expected therapeutic benefit in terms of "quality of life" and prognosis. Angiographic evaluation, on the other hand, is necessary to clarify not only the complexity of the CTO lesion, but also the probability of success and the expected risk of complications.
Indeed, only a comprehensive and integrated assessment of clinical, imaging and angiographic characteristics may define the appropriate revascularization strategy.
The goal of CTO PCI is to restore continuity between the upstream and downstream vessel segments of the occluded artery. For this purpose, two basic approaches can be used: the first one consists in penetrating the areas of loose tissue or microchannels physiologically present in part of chronic occlusions, trying to cross the thickness of the occluding plaque and proceed in the "intralesional" or “intimal” segment of the vessel; the second one aims to "bypass" the lesion, exploiting more extensively the vessel architecture and the subintimal space, proceeding within the adventitia of the vessel that, thanks to its elasticity and resistance, will constitute an operative channel.
Of note, some recently published data obtained from intracoronary imaging assessment after CTO recanalization seems to show a higher rate of all-cause mortality, post procedural myocardial infarction and target vessel revascularization in subintimal tracking techniques[43]. Subintimal recanalization was also associated with a higher prevalence of malapposed stent struts at OCT evaluation[44].
Summarizing we have two technique, intimal/intralesional and subintimal, that can be both used in antegrade and retrograde approach.
For the intimal/intralesional strategy, it’s possible to adopt a wire escalation technique according to the type of guidewires used to cross the plaque, which differ in terms of stiffness, hydrophilicity, and penetrating power; mostly with two variants: (1) "Step-up" escalation (stiff-stiff-stiffest); and (2) "Step-up-step-down" escalation (stiff-soft-stiff). Conversely, it is possible to obtain recanalization through subintimal crossing with dissection and re-entry technique by surfing in the subintimal space until the patent vessel segment is reached, bypassing the occlusion.
As mentioned above, there is also the possibility of two different approaches: (1) The antegrade approach: when the lesion is tackled by advancing guidewires along the native vessel in a proximal-distal fashion, following the bloodstream; and (2) The retrograde approach: when the lesion is tackled from the distal cap, by advancing guidewires from the donor vessel through the so called “interventional” collateral.
In some cases, different approaches can coexist in the same technique, as in the controlled antegrade and retrograde subintimal tracking (CART) or reverse CART method, where a simultaneous antegrade and retrograde approach is required.
In order to select the most appropriate approach and technique, an accurate analysis of the angiogram is a key step of the procedural strategy. The angiogram for a CTO study should preferably be performed by dual, simultaneous injection of contrast medium for better definition of vessel anatomy, effective lesion length, distal segment anatomy, and characteristics of collateral circulation, combining typical and atypical projections in order to optimize the visualization of elements of interest. "Ad hoc" CTO-PCI procedures are generally discouraged in favor of careful planning. The increased expertise in the field has allowed to identify some features of the lesions that the operator must evaluate for the choice of proper interventional strategy: morphology and localization of the proximal and distal cap, lesion length, presence of calcifications, landing zone and, finally, characteristics and quality of donor and collateral vessels.
Multiple scores have been developed over the years in order to stratify the procedures in various levels of difficulty. The effort was intended to provide a synthetic tool capable of predicting and expressing the procedural complexity of a CTO-PCI and to support the management of the procedural strategy. We will review below the main scores reported in the literature (Table 2)[45-48].
| J-CTO score | CL score | ORA score | PROGRESS score | RECHARGE score | EURO-CTO CASTLE score | |||||||
| Angiographic Features | Proximal cap blunt | 1 | Proximal cap blunt | 1 | Ostial location | 1 | Proximal cap ambiguity | 1 | Proximal cap blunt | 1 | Proximal cap blunt | 1 |
| Tortuosity > 45° | 1 | Lesion lenght > 20 mm | 1.5 | Collateral filling Rentrop 0-1 | 2 | Tortuosity | 1 | Tortuosity > 45° | 1 | Tortuosity > 45° | 1 | |
| Lenght > 20 mm | 1 | Calcification | 2 | Circumflex CTO | 1 | Lenght > 20 mm | 1 | Lenght > 20 mm | 1 | |||
| Calcification | 1 | Non-LAD CTO | 1 | Absence of interventional collaterals | 1 | Calcification | 1 | Calcification | 1 | |||
| Diseased distal landing zone | 1 | |||||||||||
| Clinical features | Prior CTO PCI failure | 1 | Previous MI | 1 | Age > 75 yr | 1 | Previous CABG on CTO target vessel | 1 | Previous CABG | 1 | ||
| Previous CABG | 1.5 | Age > 70 yr | 1 | |||||||||
The Japan-CTO (J-CTO) score[45], the progenitor of the series, was developed as a model to predict the probability of success of an antegrade wiring of the lesion within the first 30 min of the procedure. It takes into account several variables, the presence of which adds one point (+ 1) to the total score. These variables are the morphology of the proximal cap, the presence of calcifications within the occluded segment, the tortuosity of the segment, the length of the lesion (cut off > 20 mm), and the failure of a previous attempt to bridge the lesion. A score of ≥ 2 identifies a lesion that is particularly difficult to overcome.
The clinical and lesion related score was then developed[46] including some angiographic parameters already used in the J-CTO score (lesion length > 20 mm, proximal cap morphology, presence of calcifications), plus the presence of a CTO in a vessel other than the left anterior descending artery and combining them with clinical variables, such as a previous myocardial infarction and/or CABG. The score obtained identifies 4 different classes, correlated with decreasing probability of successful revascularization and increasing probability of MACCE (death, myocardial infarction, need for new revascularization with PCI or CABG, tamponade, and stroke).
The ORA (ostial location, Rentrop grade < 2, age ≥ 75) includes only 3 variables, of which one clinical (age ≥ 75 years) and two angiographic (ostial location and Rentrop collateral circulation ≥ 2)[48]. In the prospective global registry for the study of chronic total occlusion score four variables are taken into account: difficult proximal cap localization, absence of collaterals, severe tortuosity, and circumflex artery CTO[47]. These last two scores, unlike the previous ones, contemplate some variables that condition the choices in the hybrid algorithm, allowing the expansion of the field of application from only antegrade crossing techniques to retrograde and combined approaches.
The RECHARGE score was a tool developed to predict technical outcomes of CTO-PCI from patients treated by “hybrid” operators with different experience levels[49]. One point is given for a long lesion length (20 mm), visible calcification on angiography, tortuosity within the CTO segment or at CTO entry, a blunt proximal cap, a diseased distal landing zone, and the presence of a bypass graft on the CTO target vessel, respectively[49].
The more recent one the Euro-CTO CASTLE score is similar to RECHARGE score but includes among the variables, the age of the patients and previous CABG (irrespective of graft location) and discard the evaluation of the distal landing zone[50]. CASTLE Score showed similar overall discriminatory capacity compared with J-CTO score, but, for more complex procedures (J-CTO > 3 or Euro-CTO CASTLE > 4), the predictive capacity of Euro-CTO CASTLE score appeared superior[51].
Scores can be a useful tool in several aspects of CTO-PCI performance. By providing a quantitative measure of the probability of success and complications, they offer useful information to be shared with the patient and in the evaluation context of a Heart Team. Furthermore, they can guide case selection, allowing less experienced operators to confidently tackle the simplest cases, while deferring more complex challenges to more experienced operators. Nevertheless, some studies show very good success rates among experienced operators, even in case of particularly unfavorable scores[52], confirming that the scores assessment should represent a moment of reflection, but not a reason to give up before the challenge of a percutaneous revascularization.
Taking into account and keeping in mind the characteristics listed, the operator will be able to select the best interventional strategy. Historically, it is possible to identify different philosophies, or experiences to approach CTO revascularization. Currently, there are two main strategic approaches followed by practitioners: the Japanese Eastern school and the American and European Western school, evolved in the so-called "hybrid approach".
The Japanese interventional philosophy is reflected in a dedicated and thoughtful approach to CTO: extreme importance is given to the coronary study, the analysis of the angiographic picture, the availability of dedicated hemodynamic rooms. Pre-procedural tomographic techniques (to assess the anatomy of the occlusion) and intra-procedural intravascular ultrasound (to resolve ambiguities of the proximal cap and guide the return of the guides in dissection techniques) play a paramount role. The choice of the technique, obviously based on coronary anatomy, is maintained even in spite of initial procedural difficulties, favoring a careful intra-procedural choice of instrumentation and a “great mastery” in handling the available material. The use of antegrade dissection/reentry techniques, considered suboptimal for CTO recanalization, is generally discouraged, in favor of a meticulous intraluminal advancement technique or "switch" to retrograde approach. Overall, the results of the Japanese experience are extremely valid and a "driver" for international performance, with a low prevalence of clinically relevant procedural complications[52]. A potential limitation of this approach is, however, linked to the difficulty in standardizing choices and the impossibility, in different economic contexts, to use facilities and resources with the same liberality.
In an attempt to respond to this need for efficiency and uniformity, the hybrid approach of the North American school was born.
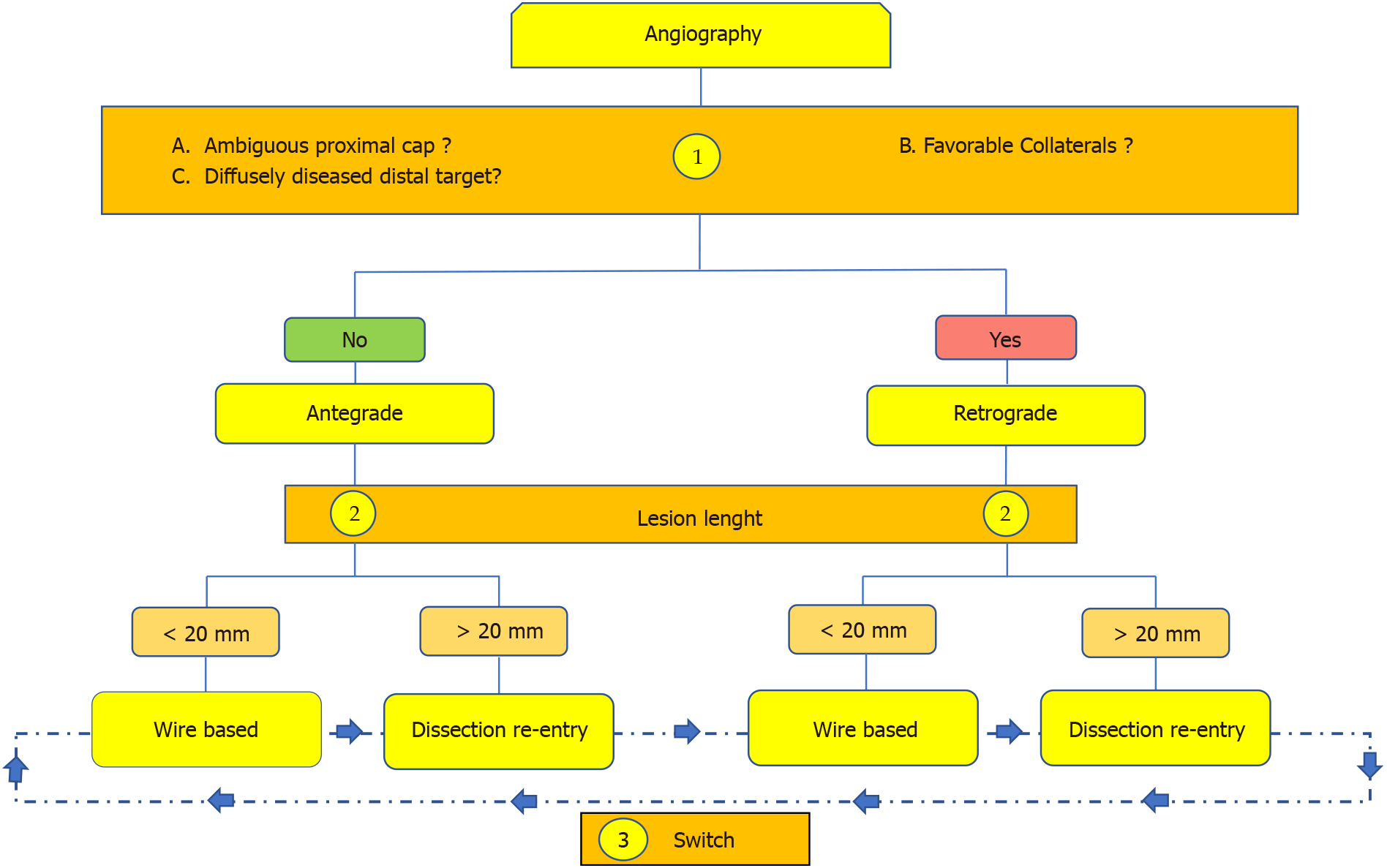
The philosophy of the hybrid approach[53] is to achieve recanalization of the occluded vessel by using all available techniques in the most effective, safe, and efficient way. It combines a limited number of anatomical information in a decision algorithm, which allows to establish the initial technique (the one with the highest probability of success in relation to the characteristics of the lesion) and the most effective bailout techniques in case of procedural failure. However, the peculiar aspect of this approach (that justifies its "hybrid" attribute) is the dynamic nature of the transition from one technique to another (Figure 2). It is recognized that excessive insistence on a single technique, in addition to being time-consuming, can even be detrimental in terms of success. Therefore, a quick "switch" is encouraged, with possible "re-cycling" among several techniques, whenever significant progress cannot be achieved within a reasonable time frame of 5-10 min. Practical benefits include shorter procedure duration, reduced radiation exposure, and potentially less use of contrast agents. Data from RECHARGE registry study evaluated the effectiveness of this approach in a "real-world" setting of European centers, finding a procedural success rate of 89%[49]. Similar results were confirmed in the recently published data from OPEN-CTO Registry: the application of hybrid approach led to a technical success rate of 86% in the index CTO-PCI[14].
A particular interesting finding was the actual application of the strategy predicted on the basis of the algorithm: in case of concordance, the success rate was higher[49]. Thanks to the algorithm, the hybrid approach leads to dissemination of learning and teaching of CTO revascularization, offering an easy guide for practitioners, particularly those with lower skills and experience level. It is worth noting that the algorithm does, however, some generalizations/limitations that are susceptible to interpretation and adaptation to individual needs.
In specialized centers, regardless of the approach strategy, safety outcomes have been shown to be very satisfactory. A meta-analysis of 65 studies, on a total of 18061 patients undergoing CTO-PCI, found an incidence of MACE (death, myocardial infarction, stroke, and CABG in emergency) of 3.1%, with a mortality of 0.2% and an incidence of cardiac tamponade of 0.3%[54]. Great care is also recommended in monitoring the amount of contrast medium used and fluoroscopy. All currently available strategies should be implemented to reduce the incidence of contrast-induced nephropathy.
Over the last years, new algorithms were developed with the aim of extending original “hybrid” approach: the Asia Pacific CTO Club algorithm[55] and the algorithm from the European CTO Club[56]. All these algorithms, the original one and his updates, are very similar. Indeed, all of them are focused on initial anatomy evaluation to guide the initial strategy choice, use of intravascular imaging is encouraged to avoid ambiguity, and criteria for failed procedure are listed. Tanaka et al[57] developed a revised algorithm, proposing a wider use of the retrograde approach, mainly in lesions with a higher J-CTO Score, highlighting how, in selected cases a primarily retrograde approach allows excellent procedural success rate with a shorter wire manipulation time.
Recently, a new revised version of “hybrid” approach was implemented, the minimalistic “hybrid” algorithm[58]. The two major points of the minimalistic “hybrid” algorithm are limiting the routine use of dual injection and encouraging the use of trans-radial access and smaller (6-7 French) guiding catheters. First results reported showed lower peri-procedural complications in the group treated according to the minimalistic approach, with similar procedural results and non-statistically significance differences in MACE[59].
Unfortunately, the multiplication of algorithms for CTO-PCI may lead to confusion rather than clarity, as also stated in a recent published editorial[60].
The ultimate challenge of coronary interventional cardiology, now fully shared by the scientific community, is to achieve a complete coronary revascularization. It has been widely demonstrated that complete coronary revascularization, achieved by either CABG or PCI, is associated with prognostic improvement, in terms of increased survival and reduction of MACE. In this scenario, the successful CTO revascularization plays a key role over the broad panorama of percutaneous coronary inter
In conclusion, the application of “contemporary” strategies aimed to obtain a state-of-the-art revascularization by PCI allows achieving long-term clinical benefit, even in high-risk patients or complex coronary anatomy with CTO. The increasing success of CTO-PCI, allowing a complete or reasonable incomplete coronary revascularization, is enabling to overcome the last great challenge of interventional cardiology, adding a “complex” piece to “complete” the puzzle.
The authors are very grateful to Fabio Torrini and Paola Baldini (A.R. Card Onlus Foundation; Florence; Italy) for their secretarial assistance.
Provenance and peer review: Invited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Teragawa H, Zhang DM S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Zhang H
| 1. | Råmunddal T, Hoebers LP, Henriques JP, Dworeck C, Angerås O, Odenstedt J, Ioanes D, Olivecrona G, Harnek J, Jensen U, Aasa M, Jussila R, James S, Lagerqvist B, Matejka G, Albertsson P, Omerovic E. Chronic total occlusions in Sweden--a report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). PLoS One. 2014;9:e103850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 110] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 2. | Claessen BE, Dangas GD, Weisz G, Witzenbichler B, Guagliumi G, Möckel M, Brener SJ, Xu K, Henriques JP, Mehran R, Stone GW. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J. 2012;33:768-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 184] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 3. | Sapontis J, Salisbury AC, Yeh RW, Cohen DJ, Hirai T, Lombardi W, McCabe JM, Karmpaliotis D, Moses J, Nicholson WJ, Pershad A, Wyman RM, Spaedy A, Cook S, Doshi P, Federici R, Thompson CR, Marso SP, Nugent K, Gosch K, Spertus JA, Grantham JA. Early Procedural and Health Status Outcomes After Chronic Total Occlusion Angioplasty: A Report From the OPEN-CTO Registry (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures). JACC Cardiovasc Interv. 2017;10:1523-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 231] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 4. | Kandzari DE, Karmpaliotis D, Kini AS, Moses JW, Tummala PE, Grantham JA, Orr C, Lombardi W, Nicholson WJ, Lembo NJ, Popma JJ, Wang J, Zhao W, McGreevy R. Late-term safety and effectiveness of everolimus-eluting stents in chronic total coronary occlusion revascularization: Final 4-year results from the evaluation of the XIENCE coronary stent, Performance, and Technique in Chronic Total Occlusions (EXPERT CTO) multicenter trial. Catheter Cardiovasc Interv. 2019;94:509-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Valenti R, Migliorini A, De Gregorio MG, Martone R, Berteotti M, Bernardini A, Carrabba N, Vergara R, Marchionni N, Antoniucci D. Impact of complete percutaneous revascularization in elderly patients with chronic total occlusion. Catheter Cardiovasc Interv. 2020;95:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | George S, Cockburn J, Clayton TC, Ludman P, Cotton J, Spratt J, Redwood S, de Belder M, de Belder A, Hill J, Hoye A, Palmer N, Rathore S, Gershlick A, Di Mario C, Hildick-Smith D; British Cardiovascular Intervention Society; National Institute for Cardiovascular Outcomes Research. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol. 2014;64:235-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 209] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 7. | Christakopoulos GE, Christopoulos G, Carlino M, Jeroudi OM, Roesle M, Rangan BV, Abdullah S, Grodin J, Kumbhani DJ, Vo M, Luna M, Alaswad K, Karmpaliotis D, Rinfret S, Garcia S, Banerjee S, Brilakis ES. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 2015;115:1367-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 189] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 8. | Hoebers LP, Claessen BE, Elias J, Dangas GD, Mehran R, Henriques JP. Meta-analysis on the impact of percutaneous coronary intervention of chronic total occlusions on left ventricular function and clinical outcome. Int J Cardiol. 2015;187:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 9. | Cui C, Sheng Z. Outcomes of percutaneous coronary intervention for chronic total occlusions in the elderly: A systematic review and meta-analysis. Clin Cardiol. 2021;44:27-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Lee SW, Lee PH, Ahn JM, Park DW, Yun SC, Han S, Kang H, Kang SJ, Kim YH, Lee CW, Park SW, Hur SH, Rha SW, Her SH, Choi SW, Lee BK, Lee NH, Lee JY, Cheong SS, Kim MH, Ahn YK, Lim SW, Lee SG, Hiremath S, Santoso T, Udayachalerm W, Cheng JJ, Cohen DJ, Muramatsu T, Tsuchikane E, Asakura Y, Park SJ. Randomized Trial Evaluating Percutaneous Coronary Intervention for the Treatment of Chronic Total Occlusion. Circulation. 2019;139:1674-1683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 272] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 11. | Werner GS, Martin-Yuste V, Hildick-Smith D, Boudou N, Sianos G, Gelev V, Rumoroso JR, Erglis A, Christiansen EH, Escaned J, di Mario C, Hovasse T, Teruel L, Bufe A, Lauer B, Bogaerts K, Goicolea J, Spratt JC, Gershlick AH, Galassi AR, Louvard Y; EUROCTO trial investigators. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39:2484-2493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 390] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 12. | Galassi AR, Boukhris M, Toma A, Elhadj Z, Laroussi L, Gaemperli O, Behnes M, Akin I, Lüscher TF, Neumann FJ, Mashayekhi K. Percutaneous Coronary Intervention of Chronic Total Occlusions in Patients With Low Left Ventricular Ejection Fraction. JACC Cardiovasc Interv. 2017;10:2158-2170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 13. | Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8991] [Cited by in RCA: 7472] [Article Influence: 257.7] [Reference Citation Analysis (0)] |
| 14. | Sapontis J, Hirai T, Patterson C, Gans B, Yeh RW, Lombardi W, Karmpaliotis D, Moses J, Nicholson WJ, Pershad A, Wyman RM, Spaedy A, Cook S, Doshi P, Federici R, Thompson CA, Nugent K, Gosch K, Grantham JA, Salisbury AC. Intermediate procedural and health status outcomes and the clinical care pathways after chronic total occlusion angioplasty: A report from the OPEN-CTO (outcomes, patient health status, and efficiency in chronic total occlusion hybrid procedures) study. Catheter Cardiovasc Interv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2722] [Cited by in RCA: 4498] [Article Influence: 899.6] [Reference Citation Analysis (0)] |
| 16. | Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445-1453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2376] [Cited by in RCA: 2212] [Article Influence: 88.5] [Reference Citation Analysis (0)] |
| 17. | Bucciarelli-Ducci C, Auger D, Di Mario C, Locca D, Petryka J, O'Hanlon R, Grasso A, Wright C, Symmonds K, Wage R, Asimacopoulos E, Del Furia F, Lyne JC, Gatehouse PD, Fox KM, Pennell DJ. CMR Guidance for Recanalization of Coronary Chronic Total Occlusion. JACC Cardiovasc Imaging. 2016;9:547-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Pica S, Di Giovine G, Bollati M, Testa L, Bedogni F, Camporeale A, Pontone G, Andreini D, Monti L, Gasparini G, Grancini L, Secco GG, Maestroni A, Ambrogi F, Milani V, Lombardi M. Cardiac magnetic resonance for ischaemia and viability detection. Guiding patient selection to revascularization in coronary chronic total occlusions: The CARISMA_CTO study design. Int J Cardiol. 2018;272:356-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Valenti R, Migliorini A, Signorini U, Vergara R, Parodi G, Carrabba N, Cerisano G, Antoniucci D. Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur Heart J. 2008;29:2336-2342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 171] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 20. | Danzi GB, Valenti R, Migliorini A, Parodi G, Vergara R, Antoniucci D. Percutaneous coronary intervention for multiple chronic total occlusions. Am J Cardiol. 2013;112:1849-1853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Farooq V, Serruys PW, Garcia-Garcia HM, Zhang Y, Bourantas CV, Holmes DR, Mack M, Feldman T, Morice MC, Ståhle E, James S, Colombo A, Diletti R, Papafaklis MI, de Vries T, Morel MA, van Es GA, Mohr FW, Dawkins KD, Kappetein AP, Sianos G, Boersma E. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol. 2013;61:282-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 228] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 22. | Valenti R, Vergara R, Migliorini A, Parodi G, Carrabba N, Cerisano G, Dovellini EV, Antoniucci D. Predictors of reocclusion after successful drug-eluting stent-supported percutaneous coronary intervention of chronic total occlusion. J Am Coll Cardiol. 2013;61:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 23. | Jang WJ, Yang JH, Song YB, Hahn JY, Choi JH, Chun WJ, Oh JH, Park YH, Kim WS, Lee YT, Gwon HC, Choi SH. Clinical implications of residual SYNTAX score after percutaneous coronary intervention in patients with chronic total occlusion and multivessel coronary artery disease: a comparison with coronary artery bypass grafting. EuroIntervention. 2017;13:97-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Garcia S, Sandoval Y, Roukoz H, Adabag S, Canoniero M, Yannopoulos D, Brilakis ES. Outcomes after complete vs incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol. 2013;62:1421-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 288] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 25. | Nagaraja V, Ooi SY, Nolan J, Large A, De Belder M, Ludman P, Bagur R, Curzen N, Matsukage T, Yoshimachi F, Kwok CS, Berry C, Mamas MA. Impact of Incomplete Percutaneous Revascularization in Patients With Multivessel Coronary Artery Disease: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2016;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Ahn JM, Park DW, Lee CW, Chang M, Cavalcante R, Sotomi Y, Onuma Y, Tenekecioglu E, Han M, Lee PH, Kang SJ, Lee SW, Kim YH, Park SW, Serruys PW, Park SJ. Comparison of Stenting Versus Bypass Surgery According to the Completeness of Revascularization in Severe Coronary Artery Disease: Patient-Level Pooled Analysis of the SYNTAX, PRECOMBAT, and BEST Trials. JACC Cardiovasc Interv. 2017;10:1415-1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 27. | Kirtane AJ, Doshi D, Leon MB, Lasala JM, Ohman EM, O'Neill WW, Shroff A, Cohen MG, Palacios IF, Beohar N, Uriel N, Kapur NK, Karmpaliotis D, Lombardi W, Dangas GD, Parikh MA, Stone GW, Moses JW. Treatment of Higher-Risk Patients With an Indication for Revascularization: Evolution Within the Field of Contemporary Percutaneous Coronary Intervention. Circulation. 2016;134:422-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 192] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 28. | Riley RF, McCabe JM, Kalra S, Lazkani M, Pershad A, Doshi D, Kirtane AJ, Nicholson W, Kearney K, Demartini T, Aaron Grantham J, Moses J, Lombardi W, Karmpaliotis D. Impella-assisted chronic total occlusion percutaneous coronary interventions: A multicenter retrospective analysis. Catheter Cardiovasc Interv. 2018;92:1261-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | De Gregorio MG, Marcucci R, Migliorini A, Gori AM, Giusti B, Vergara R, Paniccia R, Carrabba N, Marchionni N, Valenti R. Clinical Implications of "Tailored" Antiplatelet Therapy in Patients With Chronic Total Occlusion. J Am Heart Assoc. 2020;9:e014676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Zivelonghi C, Verheye S, Timmers L, van Kuijk JP, Giannini F, Dekker M, Silvis M, Abawi M, Leenders G, Kortland F, Tzanis G, Beneduce A, Benfari G, Stella P, Henriques JPS, Banai S, Agostoni P. Efficacy of Coronary Sinus Reducer in Patients With Non-revascularized Chronic Total Occlusions. Am J Cardiol. 2020;126:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 31. | Claessen BE, van der Schaaf RJ, Verouden NJ, Stegenga NK, Engstrom AE, Sjauw KD, Kikkert WJ, Vis MM, Baan J Jr, Koch KT, de Winter RJ, Tijssen JG, Piek JJ, Henriques JP. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2009;2:1128-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 179] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 32. | Park DW, Clare RM, Schulte PJ, Pieper KS, Shaw LK, Califf RM, Ohman EM, Van de Werf F, Hirji S, Harrington RA, Armstrong PW, Granger CB, Jeong MH, Patel MR. Extent, location, and clinical significance of non-infarct-related coronary artery disease among patients with ST-elevation myocardial infarction. JAMA. 2014;312:2019-2027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 285] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 33. | Henriques JP, Hoebers LP, Råmunddal T, Laanmets P, Eriksen E, Bax M, Ioanes D, Suttorp MJ, Strauss BH, Barbato E, Nijveldt R, van Rossum AC, Marques KM, Elias J, van Dongen IM, Claessen BE, Tijssen JG, van der Schaaf RJ; EXPLORE Trial Investigators. Percutaneous Intervention for Concurrent Chronic Total Occlusions in Patients With STEMI: The EXPLORE Trial. J Am Coll Cardiol. 2016;68:1622-1632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 289] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 34. | Grantham JA, Marso SP, Spertus J, House J, Holmes DR Jr, Rutherford BD. Chronic total occlusion angioplasty in the United States. JACC Cardiovasc Interv. 2009;2:479-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 218] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 35. | O'Connor SA, Garot P, Sanguineti F, Hoebers LP, Unterseeh T, Benamer H, Chevalier B, Hovasse T, Morice MC, Lefèvre T, Louvard Y. Meta-Analysis of the Impact on Mortality of Noninfarct-Related Artery Coronary Chronic Total Occlusion in Patients Presenting With ST-Segment Elevation Myocardial Infarction. Am J Cardiol. 2015;116:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 36. | Valenti R, Marrani M, Cantini G, Migliorini A, Carrabba N, Vergara R, Cerisano G, Parodi G, Antoniucci D. Impact of chronic total occlusion revascularization in patients with acute myocardial infarction treated by primary percutaneous coronary intervention. Am J Cardiol. 2014;114:1794-1800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 37. | Elias J, van Dongen IM, Råmunddal T, Laanmets P, Eriksen E, Meuwissen M, Michels HR, Bax M, Ioanes D, Suttorp MJ, Strauss BH, Barbato E, Marques KM, Claessen BEPM, Hirsch A, van der Schaaf RJ, Tijssen JGP, Henriques JPS, Hoebers LP; EXPLORE investigators. Long-term impact of chronic total occlusion recanalisation in patients with ST-elevation myocardial infarction. Heart. 2018;104:1432-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 38. | Watanabe H, Morimoto T, Shiomi H, Furukawa Y, Nakagawa Y, Ando K, Kadota K, Kimura T. Chronic total occlusion in a non-infarct-related artery is closely associated with increased five-year mortality in patients with ST-segment elevation acute myocardial infarction undergoing primary percutaneous coronary intervention (from the CREDO-Kyoto AMI registry). EuroIntervention. 2017;12:e1874-e1882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 39. | Cui KY, Yuan F, Liu H, Xu F, Zhang M, Wang W, Zhang MD, Wang YL, Zhang DF, Zhang X, Tian JF, Lyu SZ. Long-term outcomes of staged recanalization for concurrent chronic total occlusion in patients with ST-segment elevation myocardial infarction after primary percutaneous coronary intervention. J Geriatr Cardiol. 2020;17:16-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 40. | Kim SH, Behnes M, Mashayekhi K, Bufe A, Meyer-Gessner M, El-Battrawy I, Akin I. Prognostic Impact of Percutaneous Coronary Intervention of Chronic Total Occlusion in Acute and Periprocedural Myocardial Infarction. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | Ahmad Y, Howard JP, Arnold A, Prasad M, Seligman H, Cook CM, Warisawa T, Shun-Shun M, Ali Z, Parikh MA, Al-Lamee R, Sen S, Francis D, Moses JW, Leon MB, Stone GW, Karmpaliotis D. Complete Revascularization by Percutaneous Coronary Intervention for Patients With ST-Segment-Elevation Myocardial Infarction and Multivessel Coronary Artery Disease: An Updated Meta-Analysis of Randomized Trials. J Am Heart Assoc. 2020;9:e015263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 42. | Suero JA, Marso SP, Jones PG, Laster SB, Huber KC, Giorgi LV, Johnson WL, Rutherford BD. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001;38:409-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 463] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 43. | Song L, Maehara A, Finn MT, Kalra S, Moses JW, Parikh MA, Kirtane AJ, Collins MB, Nazif TM, Fall KN, Hatem R, Liao M, Kim T, Green P, Ali ZA, Batres C, Leon MB, Mintz GS, Karmpaliotis D. Intravascular Ultrasound Analysis of Intraplaque Versus Subintimal Tracking in Percutaneous Intervention for Coronary Chronic Total Occlusions and Association With Procedural Outcomes. JACC Cardiovasc Interv. 2017;10:1011-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 44. | Xhepa E, Cassese S, Rroku A, Joner M, Pinieck S, Ndrepepa G, Kastrati A, Fusaro M. Subintimal Versus Intraplaque Recanalization of Coronary Chronic Total Occlusions: Mid-Term Angiographic and OCT Findings From the ISAR-OCT-CTO Registry. JACC Cardiovasc Interv. 2019;12:1889-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 45. | Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, Kato K, Shibata Y, Hiasa Y, Doi O, Yamashita T, Hinohara T, Tanaka H, Mitsudo K; J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 660] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 46. | Alessandrino G, Chevalier B, Lefèvre T, Sanguineti F, Garot P, Unterseeh T, Hovasse T, Morice MC, Louvard Y. A Clinical and Angiographic Scoring System to Predict the Probability of Successful First-Attempt Percutaneous Coronary Intervention in Patients With Total Chronic Coronary Occlusion. JACC Cardiovasc Interv. 2015;8:1540-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 120] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 47. | Christopoulos G, Kandzari DE, Yeh RW, Jaffer FA, Karmpaliotis D, Wyman MR, Alaswad K, Lombardi W, Grantham JA, Moses J, Christakopoulos G, Tarar MNJ, Rangan BV, Lembo N, Garcia S, Cipher D, Thompson CA, Banerjee S, Brilakis ES. Development and Validation of a Novel Scoring System for Predicting Technical Success of Chronic Total Occlusion Percutaneous Coronary Interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) Score. JACC Cardiovasc Interv. 2016;9:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 270] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 48. | Galassi AR, Boukhris M, Azzarelli S, Castaing M, Marzà F, Tomasello SD. Percutaneous Coronary Revascularization for Chronic Total Occlusions: A Novel Predictive Score of Technical Failure Using Advanced Technologies. JACC Cardiovasc Interv. 2016;9:911-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 49. | Maeremans J, Walsh S, Knaapen P, Spratt JC, Avran A, Hanratty CG, Faurie B, Agostoni P, Bressollette E, Kayaert P, Bagnall AJ, Egred M, Smith D, Chase A, McEntegart MB, Smith WH, Harcombe A, Kelly P, Irving J, Smith EJ, Strange JW, Dens J. The Hybrid Algorithm for Treating Chronic Total Occlusions in Europe: The RECHARGE Registry. J Am Coll Cardiol. 2016;68:1958-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 233] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 50. | Szijgyarto Z, Rampat R, Werner GS, Ho C, Reifart N, Lefevre T, Louvard Y, Avran A, Kambis M, Buettner HJ, Di Mario C, Gershlick A, Escaned J, Sianos G, Galassi A, Garbo R, Goktekin O, Meyer-Gessner M, Lauer B, Elhadad S, Bufe A, Boudou N, Sievert H, Martin-Yuste V, Thuesen L, Erglis A, Christiansen E, Spratt J, Bryniarski L, Clayton T, Hildick-Smith D. Derivation and Validation of a Chronic Total Coronary Occlusion Intervention Procedural Success Score From the 20,000-Patient EuroCTO Registry: The EuroCTO (CASTLE) Score. JACC Cardiovasc Interv. 2019;12:335-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 105] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 51. | Kalogeropoulos AS, Alsanjari O, Keeble TR, Tang KH, Konstantinou K, Katsikis A, Jagathesan R, Aggarwal RK, Clesham GJ, Kelly PA, Werner GS, Hildick-Smith D, Davies JR, Karamasis G. CASTLE score vs J-CTO score for the prediction of technical success in chronic total occlusion percutaneous revascularisation. EuroIntervention. 2020;15:e1615-e1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 52. | Christopoulos G, Wyman RM, Alaswad K, Karmpaliotis D, Lombardi W, Grantham JA, Yeh RW, Jaffer FA, Cipher DJ, Rangan BV, Christakopoulos GE, Kypreos MA, Lembo N, Kandzari D, Garcia S, Thompson CA, Banerjee S, Brilakis ES. Clinical Utility of the Japan-Chronic Total Occlusion Score in Coronary Chronic Total Occlusion Interventions: Results from a Multicenter Registry. Circ Cardiovasc Interv. 2015;8:e002171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 53. | Brilakis ES, Grantham JA, Rinfret S, Wyman RM, Burke MN, Karmpaliotis D, Lembo N, Pershad A, Kandzari DE, Buller CE, DeMartini T, Lombardi WL, Thompson CA. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 2012;5:367-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 456] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 54. | Patel VG, Brayton KM, Tamayo A, Mogabgab O, Michael TT, Lo N, Alomar M, Shorrock D, Cipher D, Abdullah S, Banerjee S, Brilakis ES. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv. 2013;6:128-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 262] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 55. | Harding SA, Wu EB, Lo S, Lim ST, Ge L, Chen JY, Quan J, Lee SW, Kao HL, Tsuchikane E. A New Algorithm for Crossing Chronic Total Occlusions From the Asia Pacific Chronic Total Occlusion Club. JACC Cardiovasc Interv. 2017;10:2135-2143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 145] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 56. | Galassi AR, Werner GS, Boukhris M, Azzalini L, Mashayekhi K, Carlino M, Avran A, Konstantinidis NV, Grancini L, Bryniarski L, Garbo R, Bozinovic N, Gershlick AH, Rathore S, Di Mario C, Louvard Y, Reifart N, Sianos G. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention. 2019;15:198-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 113] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 57. | Tanaka H, Tsuchikane E, Muramatsu T, Kishi K, Muto M, Oikawa Y, Kawasaki T, Hamazaki Y, Fujita T, Katoh O. A Novel Algorithm for Treating Chronic Total Coronary Artery Occlusion. J Am Coll Cardiol. 2019;74:2392-2404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 58. | Vescovo GM, Zivelonghi C, Scott B, Agostoni P. Further advancement in the percutaneous revascularization of coronary chronic total occlusions: the redefined "Minimalistic Hybrid Approach" algorithm. Minerva Cardioangiol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 59. | Zivelonghi C, van Kuijk JP, Poletti E, Suttorp MJ, Eefting FD, Rensing BJ, Ten Berg JM, Colombo A, Azzalini L, Agostoni P. A "minimalistic hybrid algorithm" in coronary chronic total occlusion revascularization: Procedural and clinical outcomes. Catheter Cardiovasc Interv. 2020;95:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 60. | Rinfret S, Harding SA. A New Japanese CTO Algorithm: A Step Forward or Backward? J Am Coll Cardiol. 2019;74:2405-2409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |