Published online Sep 26, 2021. doi: 10.4330/wjc.v13.i9.493
Peer-review started: March 24, 2021
First decision: May 5, 2021
Revised: May 27, 2021
Accepted: July 27, 2021
Article in press: July 27, 2021
Published online: September 26, 2021
Processing time: 178 Days and 6.6 Hours
Percutaneous coronary intervention (PCI) of diseased saphenous vein grafts (SVG) continues to pose a clinical challenge. Current PCI guidelines give a class III recommendation against performing PCI on chronically occluded SVG. However, contemporary outcomes after SVG intervention have incrementally improved with distal protection devices, intracoronary vasodilators, drug-eluting stents, and prolonged dual antiplatelet therapy.
To reassess the procedural and long-term outcomes of PCI for totally occluded SVG with contemporary techniques.
This was a retrospective observational study conducted at a single university hospital. The study population consisted of 35 consecutive patients undergoing PCI of totally occluded SVG. Post-procedure dual antiplatelet therapy was continued for a minimum of one year and aspirin was continued indefinitely. Clinical outcomes were assessed at a mean follow-up of 1221 ± 1038 d. The primary outcome was freedom from a major adverse cardiac event (MACE) defined as the occurrence of any of the following: death, myocardial infarction, stroke, repeat bypass surgery, repeat PCI, or graft reocclusion.
The study group included 29 men and 6 women with a mean age of 69 ± 12 years. Diabetes was present in 14 (40%) patients. All patients had Canadian Heart Classification class III or IV angina. Clinical presentation was an acute coronary syndrome in 34 (97%) patients. Mean SVG age was 12 ± 5 years. Estimated duration of occlusion was acute (< 24 h) in 34% of patients, subacute (> 24 h to 30 d) in 26%, and late (> 30 d) in 40%. PCI was initially successful in 29/35 SVG occlusions (83%). Total stent length was 52 ± 35 mm. Intraprocedural complications of distal embolization or no-reflow occurred in 6 (17%) patients. During longer term follow-up, MACE-free survival was only 30% at 3 years and 17% at 5 years.
PCI of totally occluded SVG can be performed with a high procedural success rate. However, its clinical utility remains limited by poor follow-up outcomes.
Core Tip: Cardiovascular guidelines give a Class III recommendation against performing percutaneous coronary intervention (PCI) on chronically occluded saphenous vein grafts (SVG). Given contemporary advances in SVG intervention, the goal of this study was to reassess the outcomes of PCI for totally occluded SVG in 35 consecutive patients. PCI was initially successful in 29/35 (83%) SVG occlusions. However, at 3 years only 30% of patients survived without a major cardiac event. Although PCI of totally occluded SVG can be performed with a high procedural success rate, its clinical utility remains limited by poor follow-up outcomes.
- Citation: Nardone EW, Madsen BM, McCarey MM, Fischman DL, Ruggiero NJ, Walinsky P, Vishnevsky A, Savage MP. Percutaneous coronary intervention of totally occluded coronary venous bypass grafts: An exercise in futility? World J Cardiol 2021; 13(9): 493-502
- URL: https://www.wjgnet.com/1949-8462/full/v13/i9/493.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i9.493
Percutaneous coronary intervention (PCI) of diseased saphenous vein grafts (SVG) continues to be a clinical challenge[1-4]. According to present cardiovascular guidelines, PCI of SVG with chronic total occlusions is discouraged and given a class III recommendation[5]. However, outcomes after SVG intervention have incrementally improved with distal protection devices, intracoronary vasodilators, drug-eluting stents, and prolonged dual antiplatelet therapy (DAPT). The goal of this study was to reassess the procedural and long-term outcomes of PCI for totally occluded SVG in contemporary practice.
A review of medical records and coronary angiographic films was performed to identify patients with PCI performed on totally occluded SVG. This retrospective study was approved by the Institutional Review Board of the Thomas Jefferson University Hospital. All patients had a 100% occlusion of a venous bypass graft with Thrombolysis In Myocardial Infarction (TIMI) 0 or 1 flow. Patients with subtotal occlusions and TIMI 2 or 3 flow were excluded. PCI of occluded arterial bypass grafts were also excluded.
Detailed procedural information was collected on the type of anticoagulation, use of thrombectomy and distal protection device, the number of stents implanted, total stent length, and type of stent. Procedural success was defined as restored SVG patency with > TIMI 2 flow and < 20% residual stenosis. Post-discharge, all patients with successful PCI were treated with dual antiplatelet therapy (DAPT) for at least 1 year and aspirin indefinitely.
The primary outcome was freedom from a major adverse cardiac event (MACE) during a mean follow- up period of 1121 ± 1038 d. MACE was defined as the occurrence of any of the following: Death, myocardial infarction (MI), stroke, repeat bypass surgery, repeat PCI of the target vessel, or graft reocclusion. Event rates were determined by Kaplan-Meier analysis. Event free survival was also assessed as a function of the duration of SVG occlusion classified as acute (< 24 h), subacute (> 24 h to 30 days), or late (> 30 d). Duration of occlusion was estimated on the basis of the patient’s history of symptom onset. Subgroup analyses were performed based on the duration of occlusion, clinical presentation, and stent type. Fisher’s exact test was used to evaluate the relationship of duration of occlusion and clinical presentation with initial clinical success. Between group comparison of the survival curves was performed using the Mantel-Cox log rank test. P values < 0.05 were considered significant. Descriptive statistics were used to analyze baseline patient and bypass graft characteristics. Continuous variables are reported as mean ± SD.
Baseline characteristics of the patients are presented in Table 1. The study population consisted of 29 men and 6 women. Mean age was 69 ± 12 years. Diabetes was present in 40% of patients. Twenty patients (57%) had a history of prior MI. Mean left ventricular ejection fraction was 43% ± 12%. All patients had Canadian Heart Classification III or IV angina. Clinical presentation included ST-elevation MI (STEMI) in 6 patients (17%), non-STEMI in 14 patients (40%), unstable angina in 14 patients (40%), and stable angina in 1 patient (3%).
| Characteristic | n = 35 |
| Men | 29 (83%) |
| Age (mean ± SD) | 69 ± 12 yr |
| Hypertension | 33 (94%) |
| Hyperlipidemia | 25 (71%) |
| Diabetes | 14 (40%) |
| Smoking | 14 (40%) |
| Renal insufficiency | 14 (40%) |
| History of CHF | 6 (17%) |
| Prior MI | 20 (57%) |
| Ejection fraction (mean ± SD) | 43% ± 12% |
| Clinical presentation | |
| STEMI | 6 (17%) |
| NSTEMI | 14 (40%) |
| Unstable angina | 14 (40%) |
| Stable angina | 1 (3%) |
| Canadian heart class | |
| I, II | 0 |
| III | 7 (20%) |
| IV | 28 (80%) |
Bypass graft characteristics are shown in Table 2. Mean SVG age was 12.1 ± 5.1 years. The grafted native coronary artery was the left anterior descending in 9 patients (26%), left circumflex in 13 patients (37%), right coronary artery in 10 patients (29%), and multiple vessels in 3 patients (9%). Previous PCI had been performed in 10 (29%) of the SVG. The duration of graft occlusion was acute in 12 (34%), subacute in 9 (26%), and late in 14 (40%).
| Characteristic | n (%) |
| SVG age (mean ± SD) | 12.1 ± 5.1 yr |
| Prior PCI of SVG | 10 (29) |
| Grafted native vessel | |
| LAD | 9 (26) |
| LCx | 13 (37) |
| RCA | 10 (29) |
| Multiple | 3 (9) |
| Duration of graft occlusion | |
| Acute (< 24 h) | 12 (34) |
| Subacute (> 24 h to 30 d) | 9 (26) |
| Late (> 30 d) | 14 (40) |
Procedural features and outcomes are presented in Table 3. Glycoprotein IIbIIIa inhibitors were used in 15 (43%) of cases. Thrombectomy was performed in 20 (57%). Distal protection devices were used in 9 (26%). The mean number of stents implanted was 2.1 ± 1.3 and total stent length was 52 ± 35 mm. Drug-eluting stents were used in the majority of patients.
| Feature | n (%) |
| Anticoagulation | |
| Heparin only | 12 (34) |
| Bivalirudin | 8 (23) |
| Heparin + GP IIb IIIa inhibitor | 15 (43) |
| Thrombectomy | 20 (57) |
| Distal protection device | 9 (26) |
| Number of stents (mean ± SD) | 2.1 ± 1.3 |
| Total stent length (mean ± SD) | 52 ± 35 mm |
| Stent type | |
| Drug-eluting | 19 (55) |
| Bare metal | 11 (31) |
| None | 5 (14) |
| Procedural outcome | |
| Success | 29 (83) |
| Failed | 6 (17) |
| Procedural complications | |
| Distal embolization | 1 (3) |
| No reflow | 5 (15) |
| In-hospital MACE | |
| Death | 2 (5.7) |
| Myocardial infarction | 1 (2.9) |
| Stroke | 0 |
| Repeat PCI or CABG | 0 |
| Any MACE | 3 (8.6) |
Procedural success in restoring SVG patency was achieved in 29 of the 35 patients (83%). Of the 6 unsuccessful procedures, 2 were due to the failure to cross through the occluded graft with any guidewire; in the remaining 4 cases, successful guidewire passage to the distal native vessel was accomplished but graft patency could not be restored despite balloon angioplasty and thrombectomy. Procedural success was not correlated with either clinical presentation (P = 0.99) or duration of graft occlusion (P = 0.33). Procedural complications included distal embolization or no-reflow in 6 (17%) patients. There were no instances of coronary perforation. In-hospital MACE occurred in 3 (9%) patients including 2 deaths and one nonfatal MI.
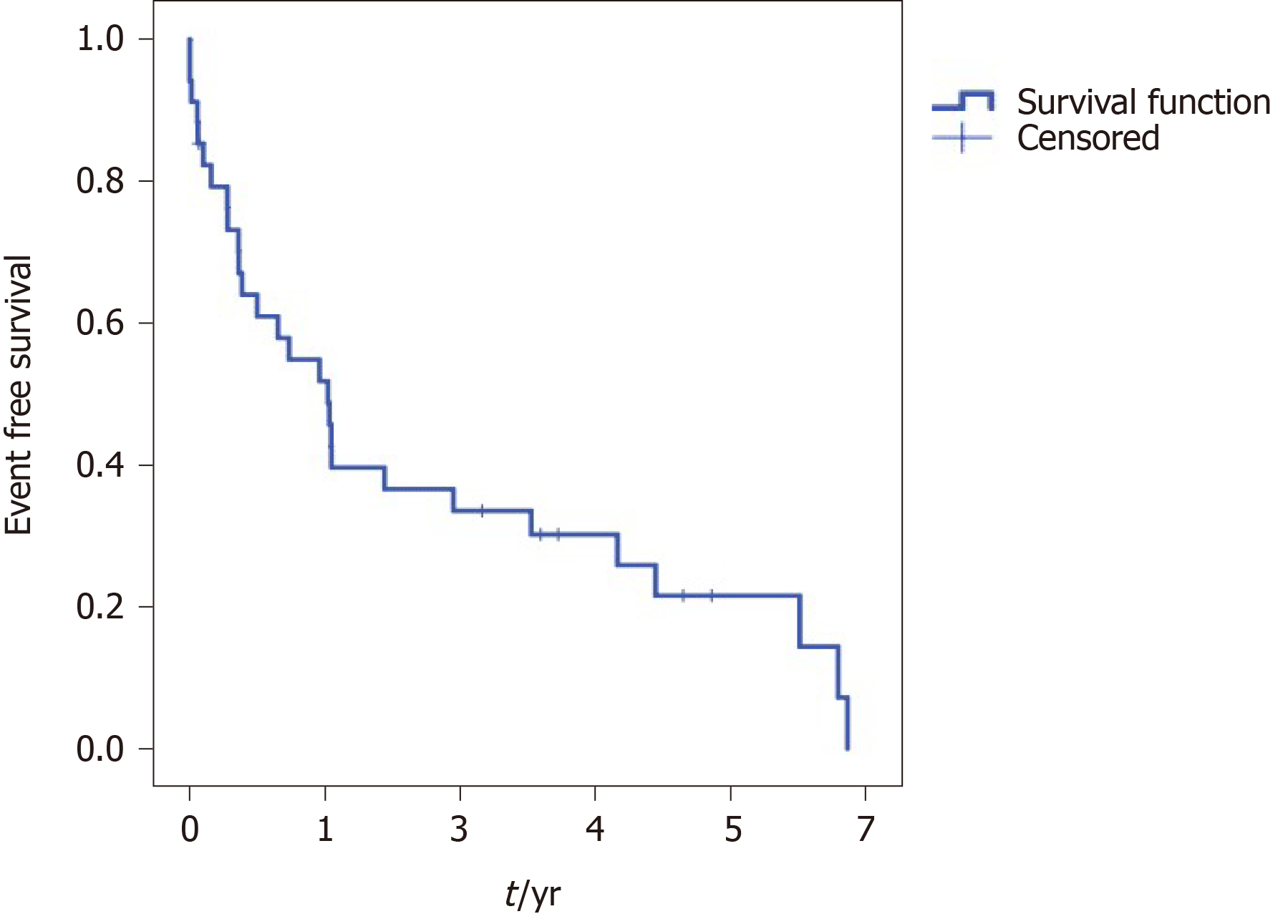
Follow-up event free survival is shown in Figure 1. MACE free survival was 58% at 1 year, 30% at 3 years, and 17% at 5 years. Distribution of specific MACE events during follow up is shown in Table 4. Longer term outcome was not related to the initial duration of SVG occlusion (Figure 2) (P = 0.60) or clinical presentation (P = 0.87). There was no difference in MACE free survival for patients with drug-eluting stents compared to bare metal stents (P = 0.97).
| MACE type | n (%) |
| Death | 5 (14) |
| Stroke | 1 (3) |
| MI | 15 (43) |
| Repeat bypass surgery | 0 |
| Repeat PCI | 6 (17) |
| Graft reocclusionAny MACE | 7 (20) 28 (80) |
The management of patients who develop bypass graft disease after previous coronary artery bypass grafting (CABG) surgery continue to pose a clinical challenge. For post-CABG patients with unstable or medically refractory symptoms, all revascularization options entail heightened complexity and procedural risk. Redo CABG carries an increased risk of morbidity and mortality compared to the initial operation[6,7]. The outcomes of PCI in SVG have been significantly improved by coronary stenting[8]. Nevertheless, compared to native coronary arteries, PCI of SVG continues to be associated with higher risk of both procedural and long-term adverse events[9]. Accordingly, if revascularization is indicated in the presence of SVG disease, it is generally preferable to intervene on the native coronary artery if technically feasible. On the other hand, native coronary arteries long after bypass surgery often have complex, heavily calcified chronic total occlusions (CTO) which result in a significantly augmented risk of PCI failure and major complications[10-12].
Historically, before the introduction of distal protection devices and drug-eluting stents, PCI of totally occluded SVG has been associated with low initial procedural success, a high rate of complications, and frequent follow-up adverse events[13,14]. More contemporary PCI studies of SVG in the setting of acute thrombosis and STEMI while demonstrating improved procedural success still report poor longer term clinical outcomes[15,16]. A few studies have evaluated the outcome of PCI in chronically occluded SVG in the DES era[17-20]. An early small study of 11 patients with chronically occluded SVG suggested a high procedural success rate and favorable longer term outcomes after PCI[17]. Subsequent studies of chronically occluded SVG involving 22 to 34 patients reported PCI procedural success in 68% to 79% of cases with relatively high rates of MACE during medium term follow-up[18-20].
Citing low success rates, high complication rates, and poor long-term patency, ACC/AHA/SCAI PCI guidelines have a Class III: Harm recommendation against PCI for chronic SVG occlusions[5]. However, it is important to note that these guidelines were published over a decade ago. Accordingly, the unanswered question is whether the cumulative advances in SVG intervention have translated into improved outcome for totally occluded grafts. Distal protection devices have been shown to reduce periprocedural MACE, can be deployed with high success rate, and are given a Class I recommendation in PCI guidelines[5,21-23]. Intracoronary vasodilators have been shown to be effective in treating no-reflow which is a common complication during SVG PCI and may have benefits if given prophylactically[24-27]. Drug-eluting stents appear to reduce restenosis in SVG early after PCI although they exhibit a catch-up phenomenon during late follow-up[28-31]. Prolonged DAPT improves outcomes following PCI in high risk patient subsets and has been suggested as a possible strategy to improve the long-term outcome after PCI of SVG[4,32,33]. In addition to these advances in SVG intervention, significant improvements in CTO outcomes have been made through continued technical and procedural innovations[34,35].
Given the aforementioned advances, the goal of the current study was to reassess the procedural and long-term outcomes of occluded SVG PCI in the context of contemporary techniques. The initial procedural success in restoring SVG patency was achieved in 83% of patients. This procedural success rate is quite favorable compared to prior reports of totally occluded SVG. On the other hand, long-term clinical outcomes remained poor even though DAPT was continued for a minimum of one year and DES were used in most patients. MACE free survival was 58% at 1 year, 30% at 3 years, and only 17% at 5 years. There was no relation between the duration of SVG occlusion prior to PCI and long-term outcome. There was also no difference in outcome with drug-eluting compared to bare metal stents. The disappointing long-term results of DES in occluded SVG is consistent with the findings of other recent studies of DES for non-occluded SVG[29-31].
Limitations of the current study should be recognized. This study was retrospective and we do not have information into why PCI of the occluded vein graft was undertaken as opposed to other treatment options. Data is not available on the number of patients who were treated by other means such as PCI of the native vessel, redo CABG, or medical therapy alone. Patients in this study who underwent PCI likely represent a small select group with totally occluded SVG. These patients were treated in the drug-eluting stent era which now spans over the past decade and a half; the study population of this report represents less than 1% of patients undergoing PCI at our institution during this time. Accordingly, the outcomes of these patients could have been affected by the selection bias of the operators.
PCI of totally occluded SVG can be performed with a relatively high rate of procedural success. However, the vast majority of patients will experience a major clinical event within a few years following the procedure. Therefore, the clinical utility of PCI for totally occluded SVG continues to be limited due to poor long-term outcome.
Percutaneous coronary intervention (PCI) of diseased saphenous vein grafts (SVG) continues to pose a clinical challenge. Given low success rates, high complication rates, and poor long term patency, current cardiovascular guidelines have a class III recommendation against PCI for chronically occluded SVG.
Contemporary outcomes of SVG intervention have incrementally improved with distal protection devices, intracoronary vasodilators, drug-eluting stents, and prolonged dual antiplatelet therapy. There is a paucity of studies on the outcome of PCI for totally occluded SVG using current techniques.
The goal of this study was to reassess the procedural and long term outcome of PCI for totally occluded SVG with contemporary techniques in the drug-eluting stent era.
This was a retrospective observational study of 35 consecutive patients undergoing PCI of totally occluded SVG. The primary outcome was freedom from a major adverse cardiac event (MACE) defined as any of the following: Death, myocardial infarction, stroke, repeat revascularization of the target vessel, or graft reocclusion. Mean follow-up was 1221 ± 1038 d.
The study group included 29 men and 6 women aged 69 ± 12 years. Mean SVG age was 12 ± 5 years. PCI was initially successful in 29/35 (83%) SVG occlusions. During long term follow-up, MACE-free survival was 30% at 3 years and 17% at 5 years.
PCI of totally occluded SVG can be performed with a relatively high rate of procedural success. However, the vast majority of patients have a major clinical event within a few years following the procedure. Thus, the clinical utility of PCI for totally occluded SVG continues to be limited by poor long term outcomes.
Although PCI of totally occluded SVG can be often initially accomplished, the long term clinical outcome remains poor. Future research is required to achieve a more sustained clinical benefit through further innovations in stent design and adjunct pharmacology.
The authors thank Scott Keith PhD, a biostatistician at the Thomas Jefferson University, for performing a statistical review.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: American College of Cardiology; Society of Cardiac Angiography and Interventions; American College of Physicians.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vermeersch P S-Editor: Ma YJ L-Editor: A P-Editor: Li JH
| 1. | Rodriguez MA, Fischman DL, Savage MP. Advances in vein graft intervention. Intervention Cardiol. 2010;2:735-754. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Lee MS, Park SJ, Kandzari DE, Kirtane AJ, Fearon WF, Brilakis ES, Vermeersch P, Kim YH, Waksman R, Mehilli J, Mauri L, Stone GW. Saphenous vein graft intervention. JACC Cardiovasc Interv. 2011;4:831-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Marmagkiolis K, Grines C, Bilodeau L. Current percutaneous treatment strategies for saphenous vein graft disease. Catheter Cardiovasc Interv. 2013;82:406-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Redfors B, Généreux P, Witzenbichler B, McAndrew T, Diamond J, Huang X, Maehara A, Weisz G, Mehran R, Kirtane AJ, Stone GW. Percutaneous Coronary Intervention of Saphenous Vein Graft. Circ Cardiovasc Interv. 2017;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1654] [Cited by in RCA: 1744] [Article Influence: 124.6] [Reference Citation Analysis (0)] |
| 6. | Loop FD, Lytle BW, Cosgrove DM, Woods EL, Stewart RW, Golding LA, Goormastic M, Taylor PC. Reoperation for coronary atherosclerosis. Changing practice in 2509 consecutive patients. Ann Surg. 1990;212:378-85; discussion 385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 109] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28:616-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 928] [Cited by in RCA: 930] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 8. | Savage MP, Douglas JS Jr, Fischman DL, Pepine CJ, King SB 3rd, Werner JA, Bailey SR, Overlie PA, Fenton SH, Brinker JA, Leon MB, Goldberg S. Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts. Saphenous Vein De Novo Trial Investigators. N Engl J Med. 1997;337:740-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 370] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 9. | Brilakis ES, O'Donnell CI, Penny W, Armstrong EJ, Tsai T, Maddox TM, Plomondon ME, Banerjee S, Rao SV, Garcia S, Nallamothu B, Shunk KA, Mavromatis K, Grunwald GK, Bhatt DL. Percutaneous Coronary Intervention in Native Coronary Arteries Versus Bypass Grafts in Patients With Prior Coronary Artery Bypass Graft Surgery: Insights From the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program. JACC Cardiovasc Interv. 2016;9:884-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 117] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 10. | Liu MJ, Chen CF, Gao XF, Liu XH, Xu YZ. In-hospital outcomes of chronic total occlusion percutaneous coronary intervention in patients with and without prior coronary artery bypass graft: A protocol for systematic review and meta analysis. Medicine (Baltimore). 2020;99:e19977. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Megaly M, Abraham B, Pershad A, Rinfret S, Alaswad K, Garcia S, Azzalini L, Gershlick A, Burke MN, Brilakis ES. Outcomes of Chronic Total Occlusion Percutaneous Coronary Intervention in Patients With Prior Bypass Surgery. JACC Cardiovasc Interv. 2020;13:900-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Shoaib A, Johnson TW, Banning A, Ludman P, Rashid M, Potts J, Kwok CS, Kontopantelis E, Azam ZA, Kinnaird T, Mamas MA. Clinical Outcomes of Percutaneous Coronary Intervention for Chronic Total Occlusion in Native Coronary Arteries vs Saphenous Vein Grafts. J Invasive Cardiol. 2020;32:350-357. [PubMed] |
| 13. | de Feyter PJ, Serruys P, van den Brand M, Meester H, Beatt K, Suryapranata H. Percutaneous transluminal angioplasty of a totally occluded venous bypass graft: a challenge that should be resisted. Am J Cardiol. 1989;64:88-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 75] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Berger PB, Bell MR, Grill DE, Simari R, Reeder G, Holmes DR Jr. Influence of procedural success on immediate and long-term clinical outcome of patients undergoing percutaneous revascularization of occluded coronary artery bypass vein grafts. J Am Coll Cardiol. 1996;28:1732-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Abdel-Karim AR, Banerjee S, Brilakis ES. Percutaneous intervention of acutely occluded saphenous vein grafts: contemporary techniques and outcomes. J Invasive Cardiol. 2010;22:253-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Nikolsky E, Mehran R, Yu J, Witzenbichler B, Brodie BR, Kornowski R, Brener S, Xu K, Dangas GD, Stone GW. Comparison of outcomes of patients with ST-segment elevation myocardial infarction with vs without previous coronary artery bypass grafting (from the Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction [HORIZONS-AMI] trial). Am J Cardiol. 2013;111:1377-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Meliga E, García-García HM, Kukreja N, Daemen J, Tanimoto S, Ramcharitar S, van Mieghem CA, Sianos G, van der Ent M, van der Giessen WJ, de Feyter P, van Domburg R, Serruys PW. Chronic total occlusion treatment in post-CABG patients: saphenous vein graft vs native vessel recanalization-long-term follow-up in the drug-eluting stent era. Catheter Cardiovasc Interv. 2007;70:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Al-Lamee R, Ielasi A, Latib A, Godino C, Ferraro M, Arioli F, Mussardo M, Piraino D, Figini F, Carlino M, Montorfano M, Chieffo A, Colombo A. Clinical and angiographic outcomes after percutaneous recanalization of chronic total saphenous vein graft occlusion using modern techniques. Am J Cardiol. 2010;106:1721-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Jim MH, Ho HH, Ko RL, Siu CW, Yiu KH, Lau CP, Chow WH. Paclitaxel-eluting stents for chronically occluded saphenous vein grafts (EOS) study. J Interv Cardiol. 2010;23:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Garg N, Hakeem A, Gobal F, Uretsky BF. Outcomes of percutaneous coronary intervention of chronic total saphenous vein graft occlusions in the contemporary era. Catheter Cardiovasc Interv. 2014;83:1025-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Baim DS, Wahr D, George B, Leon MB, Greenberg J, Cutlip DE, Kaya U, Popma JJ, Ho KK, Kuntz RE; Saphenous vein graft Angioplasty Free of Emboli Randomized (SAFER) Trial Investigators. Randomized trial of a distal embolic protection device during percutaneous intervention of saphenous vein aorto-coronary bypass grafts. Circulation. 2002;105:1285-1290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 379] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 22. | Stone GW, Rogers C, Hermiller J, Feldman R, Hall P, Haber R, Masud A, Cambier P, Caputo RP, Turco M, Kovach R, Brodie B, Herrmann HC, Kuntz RE, Popma JJ, Ramee S, Cox DA; FilterWire EX Randomized Evaluation Investigators. Randomized comparison of distal protection with a filter-based catheter and a balloon occlusion and aspiration system during percutaneous intervention of diseased saphenous vein aorto-coronary bypass grafts. Circulation. 2003;108:548-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 267] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 23. | Kaliyadan AG, Chawla H, Fischman DL, Ruggiero N 2nd, Gannon M, Walinsky P, Savage MP. Importance of Adjunct Delivery Techniques to Optimize Deployment Success of Distal Protection Filters During Vein Graft Intervention. J Invasive Cardiol. 2017;29:54-58. [PubMed] |
| 24. | Klein LW, Kern MJ, Berger P, Sanborn T, Block P, Babb J, Tommaso C, Hodgson JM, Feldman T; Interventional Cardiology Committee of the Society of Cardiac Angiography and Interventions. Society of cardiac angiography and interventions: suggested management of the no-reflow phenomenon in the cardiac catheterization laboratory. Catheter Cardiovasc Interv. 2003;60:194-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Huang RI, Patel P, Walinsky P, Fischman DL, Ogilby JD, Awar M, Frankil C, Savage MP. Efficacy of intracoronary nicardipine in the treatment of no-reflow during percutaneous coronary intervention. Catheter Cardiovasc Interv. 2006;68:671-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Michaels AD, Appleby M, Otten MH, Dauterman K, Ports TA, Chou TM, Gibson CM. Pretreatment with intragraft verapamil prior to percutaneous coronary intervention of saphenous vein graft lesions: results of the randomized, controlled vasodilator prevention on no-reflow (VAPOR) trial. J Invasive Cardiol. 2002;14:299-302. [PubMed] |
| 27. | Fischell TA, Subraya RG, Ashraf K, Perry B, Haller S. "Pharmacologic" distal protection using prophylactic, intragraft nicardipine to prevent no-reflow and non-Q-wave myocardial infarction during elective saphenous vein graft intervention. J Invasive Cardiol. 2007;19:58-62. [PubMed] |
| 28. | Mehilli J, Pache J, Abdel-Wahab M, Schulz S, Byrne RA, Tiroch K, Hausleiter J, Seyfarth M, Ott I, Ibrahim T, Fusaro M, Laugwitz KL, Massberg S, Neumann FJ, Richardt G, Schömig A, Kastrati A; Is Drug-Eluting-Stenting Associated with Improved Results in Coronary Artery Bypass Grafts? (ISAR-CABG) Investigators. Drug-eluting vs bare-metal stents in saphenous vein graft lesions (ISAR-CABG): a randomised controlled superiority trial. Lancet. 2011;378:1071-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 29. | Colleran R, Kufner S, Mehilli J, Rosenbeiger C, Schüpke S, Hoppmann P, Joner M, Mankerious N, Fusaro M, Cassese S, Abdel-Wahab M, Neumann FJ, Richardt G, Ibrahim T, Schunkert H, Laugwitz KL, Kastrati A, Byrne RA; ISAR-CABG Investigators. Efficacy Over Time With Drug-Eluting Stents in Saphenous Vein Graft Lesions. J Am Coll Cardiol. 2018;71:1973-1982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 30. | Patel NJ, Bavishi C, Atti V, Tripathi A, Nalluri N, Cohen MG, Kini AS, Sharma SK, Dangas G, Bhatt DL. Drug-Eluting Stents Versus Bare-Metal Stents in Saphenous Vein Graft Intervention. Circ Cardiovasc Interv. 2018;11:e007045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Savage MP, Fischman DL. Love in Vain? Circ Cardiovasc Interv. 2018;11:e007458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Yeh RW, Kereiakes DJ, Steg PG, Cutlip DE, Croce KJ, Massaro JM, Mauri L; DAPT Study Investigators. Lesion Complexity and Outcomes of Extended Dual Antiplatelet Therapy After Percutaneous Coronary Intervention. J Am Coll Cardiol. 2017;70:2213-2223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 33. | Sachdeva A, Bavisetty S, Beckham G, Shen AY, Aharonian V, Mansukhani P, Stone GW, Leon M, Moses J, Moore N, Hyett R, Contreras R, Brar SS. Discontinuation of long-term clopidogrel therapy is associated with death and myocardial infarction after saphenous vein graft percutaneous coronary intervention. J Am Coll Cardiol. 2012;60:2357-2363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Tajti P, Burke MN, Karmpaliotis D, Alaswad K, Werner GS, Azzalini L, Carlino M, Patel M, Mashayekhi K, Egred M, Krestyaninov O, Khelimskii D, Nicholson WJ, Ungi I, Galassi AR, Banerjee S, Brilakis ES. Update in the Percutaneous Management of Coronary Chronic Total Occlusions. JACC Cardiovasc Interv. 2018;11:615-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 35. | Brilakis ES, Mashayekhi K, Tsuchikane E, Abi Rafeh N, Alaswad K, Araya M, Avran A, Azzalini L, Babunashvili AM, Bayani B, Bhindi R, Boudou N, Boukhris M, Božinović NŽ, Bryniarski L, Bufe A, Buller CE, Burke MN, Büttner HJ, Cardoso P, Carlino M, Christiansen EH, Colombo A, Croce K, Damas de Los Santos F, De Martini T, Dens J, Di Mario C, Dou K, Egred M, ElGuindy AM, Escaned J, Furkalo S, Gagnor A, Galassi AR, Garbo R, Ge J, Goel PK, Goktekin O, Grancini L, Grantham JA, Hanratty C, Harb S, Harding SA, Henriques JPS, Hill JM, Jaffer FA, Jang Y, Jussila R, Kalnins A, Kalyanasundaram A, Kandzari DE, Kao HL, Karmpaliotis D, Kassem HH, Knaapen P, Kornowski R, Krestyaninov O, Kumar AVG, Laanmets P, Lamelas P, Lee SW, Lefevre T, Li Y, Lim ST, Lo S, Lombardi W, McEntegart M, Munawar M, Navarro Lecaro JA, Ngo HM, Nicholson W, Olivecrona GK, Padilla L, Postu M, Quadros A, Quesada FH, Prakasa Rao VS, Reifart N, Saghatelyan M, Santiago R, Sianos G, Smith E, C Spratt J, Stone GW, Strange JW, Tammam K, Ungi I, Vo M, Vu VH, Walsh S, Werner GS, Wollmuth JR, Wu EB, Wyman RM, Xu B, Yamane M, Ybarra LF, Yeh RW, Zhang Q, Rinfret S. Guiding Principles for Chronic Total Occlusion Percutaneous Coronary Intervention. Circulation. 2019;140:420-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 272] [Article Influence: 45.3] [Reference Citation Analysis (0)] |